Abstract
Introduction
Chronic cough heavily affects patients’ quality of life, and there are no effective licensed therapies available. Cough is a complication of severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) infection, asthma, and other diseases. Patients with various diseases have a different profile of tussive responses to diverse cough triggers, thereby suggesting sundry mechanisms of neuronal dysfunctions. Previously, we demonstrated that the small molecule drug XC8 shows a clinical anti-asthmatic effect. The objective of the present study was to investigate the effect of XC8 on cough.
Methods
We studied the antitussive effect of XC8 on cough induced by agonists activating human transient receptor potential (TRP) cation channels TRPA1 or TRPV1 in guinea pigs. We checked the agonistic/antagonistic activity of XC8 on the human cation channels TRPA1, TRPV1, TRPM8, P2X purinoceptor 2 (P2X2), and human acid sensing ion channel 3 (hASIC3) in Fluorescent Imaging Plate Reader (FLIPR) assay.
Results
XC8 demonstrated clear antitussive activity and dose-dependently inhibited cough in guinea pigs induced by citric acid alone (up to 67.1%) or in combination with IFN-γ (up to 76.4%). XC8 suppressed cough reflexes induced by the repeated inhalation of citric acid (up to 80%) or by cinnamaldehyde (up to 60%). No activity of XC8 against cough evoked by capsaicin was revealed. No direct agonistic/antagonistic activity of XC8 on human TRPA1, TRPV1, TRPM8, P2X2, or hASIC3 was detected.
Conclusions
XC8 acts against cough evoked by the activation of TRPA1 (citric acid/cinnamaldehyde) but not TRPV1 (capsaicin) channels. XC8 inhibits the cough reflex and suppresses the cough potentiation by IFN-γ. XC8 might be of significant therapeutic value for patients suffering from chronic cough associated with inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
XC8 acts against cough evoked by the activation of TRPA1 (citric acid/cinnamaldehyde) but not TRPV1 (capsaicin) channels. |
XC8 does not have direct agonistic/antagonistic activity on human TRPA1, TRPV1, TRPM8, P2X2, or hASIC3 channels. |
Introduction
Chronic cough (i.e., cough lasting > 8 weeks) is a common problem affecting approximately 2–18% of the general population [1, 2]. Patients with chronic cough suffer continuously, as they may experience 10–100 coughs per hour over weeks. This condition greatly affects the quality of life of patients and interferes with their daily activities, e.g., sleeping, working, and social life. In about half of cases, chronic cough is caused by other diseases such as viral infections, asthma, cystic fibrosis, bronchiectasis, and/or gastroesophageal reflux [3]. The underlying disease causes pathological processes affecting the neural pathways leading to the increased sensitivity/responsivity to coughing named cough hypersensitivity/hyperresponsivity syndrome (CHS) [4]. While the specific causes of chronic cough may vary, the underlying pathophysiologic mechanisms are quite similar. However, there are no effective licensed therapies available.
Human airways are innervated with vagal afferent Aδ- and C-fibers responsible for airway reflexes [5]. Autonomic and sensory nerve fibers in the airways express receptors for a variety of inflammatory mediators, including protons, neurotrophic factors, adenosine triphosphate (ATP), proinflammatory cytokines like interferons (IFNs), and tumor necrosis factor α (TNF-α), which can recruit nerve fibers in inflammation [6,7,8,9]. Chronic cough is often characterized by airway inflammation, which in turn induces airway remodeling and alters the plasticity of afferent vagus nerve C-fibers [10, 11]. In humans, cough can be evoked by the mechanical probing of tracheal mucosa, or by chemical stimuli, including hyper- and hypotonic solutions, acids, capsaicin, cinnamaldehyde, cigarette smoke, or others [12,13,14,15,16]. C-fibers respond to chemical stimuli by the activation of transient receptor potential (TRP) calcium permeable channels which act as sensors. In mammals, 28 TRP channels, belonging to six families are described. The most studied include TRP ankyrin (TRPA), TRP melastatin (TRPM), and TRP vanilloid (TRPV) channels. TRPV1 and TRPA1 channels are expressed at the nerve terminals and known to contribute to the pathogenesis of chronic cough [17]. Once activated, they start to release neuropeptides, such as calcitonin gene-related peptide (CGPR), substance P (SP), and neurokinin A (NKA), thereby contributing to local neurogenic inflammation characterized by cough, bronchoconstriction, vasodilation, and infiltration of immune cells [18]. The TRPV1 channel responds to high temperature, low pH, and capsaicin [19]. Capsaicin (an active component of chili pepper) is often used as a tussigenic stimulus to study the cough mechanisms [20, 21]. TRPA1 channel responds to cold temperature and a variety of irritants like acids, cigarette smoke, acrolein, and cinnamaldehyde [22]. Patients with various diseases were shown to have a divergent profile of tussive responses to stimuli such as cigarette smoke or capsaicin, thereby suggesting different mechanisms of evoked cough [23]. The response to capsaicin is known to differentiate a variety of neuronal dysfunctions [24].
Viral infections of the upper respiratory tract (URVIs) are one of the causes of chronic cough. URVIs induce inflammation accompanied by the release of such cytokines as interlukin-1 (IL-1), IL-6, IL-8, IL-11, GRO-α, TNF-α, RANTES, GM-CSF, and CCL11 (eotaxin-1) [25, 26]. An inflammatory response involving the epithelial and smooth muscle cells as well as infiltrating immune cells is associated with cough [27, 28]. Prolonged cough is one of the symptoms that many survivors of severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) infection suffer from [29].
Asthma is another condition that causes cough. This cough can be resistant to treatment with classical anti-asthmatic drugs such as inhaled corticosteroids (ICS) or long-acting beta-agonists (LABA), but sensitive to leukotriene receptor antagonist (LTRA) or anticholinergics as tiotropium [30, 31]. Biopsies from patients with chronic non-asthmatic and asthmatic cough demonstrated that many signs of airway remodeling, such as the thickening of membrane, increase in vascularity, and hyperplasia of goblet cells, were common in both groups of patients, indicating a common pathophysiological process [10]. The elevated levels of prostaglandins or histamine in the sputum of patients with cough in combination with the infiltration of mast cells indicate the neuronal activation in the airways that could stimulate cough receptors [32].
The small molecule drug XC8 (glutarimide derivative) developed by Pharmenterprises LLC was shown to affect the influx of eosinophils into bronchoalveolar lavage (BAL) in a model of lung inflammation or asthma in rats and guinea pigs [33]. We demonstrated the complete safety of XC8 in healthy probands in phase 1 clinical trial [34]. In phase 2a trial, we have shown that the treatment of asthma patients with a high levels of blood eosinophils and serum IFN-γ with XC8 led to an improvement in force expiratory volume in 1 s (FEV1) [35]. These results imply that XC8 can have the potential to affect cough. The objective of the present study was to investigate the effect of XC8 on cough induced by different stimuli in guinea pigs.
Methods
Animals
The experiments were performed on 16-week-old male Agouti guinea pigs (250–260 g), which were purchased from the Scientific Center of Biomedical Technologies (Andreevka, Moscow region). The animals were kept in cages with a controlled environment with standard pelleted food and water ad libitum. All of the animal experiments were approved by the Animal Ethics Committee of LLC Pharmenterprises (protocols No. BEC 07/2020 dated 19.05.2020, and 09/2020 dated 14.07.2020). The experimental procedures with animals were performed in accordance with the Guide for the Care and Use of Laboratory Animals [36]. All the procedures with animals were performed under anesthesia to minimize their suffering.
Cough Induced by Citric Acid
To study the effect of XC8 on cough induced by the inhalation of citric acid, guinea pigs were treated with XC8 intragastrically (p.o.) at doses of 0.7, 1.4, 2.8, 4.2, 5.6, 7.0, and 14.0 mg/kg diluted in distilled water with 1% Tween-80. In 7 h, all of the animals inhaled the citric acid solution (0.3 M in saline) for 8 min using an Omron compAIR NE-C28 compression nebulizer. The group of control animals received the vehicle (distilled water with 1% Tween-80) instead of XC8. Antitussive activity of XC8 was assessed manually by counting the number of coughs by trained personnel within 8 min after the start of citric acid inhalation and expressed as percentage of inhibition in comparison to control group of animals.
In order to assess the effect of IFN-γ on cough, animals inhaled IFN-γ at a dose of 10 μg/kg using an Omron compAIR NE-C28 compression nebulizer for 3 min. Then, after 7 h, all of the animals inhaled the citric acid solution (0.3 M in saline) for 8 min using an Omron compAIR NE-C28 compression nebulizer. XC8 was administered p.o., immediately after the inhalation of IFN-γ at doses of 0.7, 1.4, 2.8, 4.2, 5.6, 7.0, and 14.0 mg/kg. The group of control animals received the vehicle. Antitussive activity was assessed by counting the number of coughs within 8 min after the start of citric acid inhalation and expressed as percentage of inhibition in comparison to control group.
Chronic Cough Induced by Citric Acid
Guinea pigs inhaled a citric acid solution (0.4 M in saline) for 10 min daily from the 0th to 6th days. XC8 was given p.o. daily, 1 h before the inhalation of citric acid. Control animals received distilled water with 1% Tween-80 instead of XC8. Butamirate (Codelac Neo®, OTCPharm, Russia)—powerful centrally acting cough suppressant was used as a reference drug. Butamirate at a dose of 5 mg/kg was administered p.o. in the same regimen. Antitussive activity was evaluated by counting the number of coughs within 10 min after each inhalation of citric acid and expressed as percentage of inhibition in comparison to control group of animals. The results of the most representative experiment with XC8 (at doses of 1.4, 7.0, and 14 mg/kg) are presented.
Cough Induced by Cinnamaldehyde
Guinea pigs were treated p.o. with XC8 (at doses of 0.14, 1.4, or 14 mg/kg) 1, 3, 6, 8, and 12 h before the inhalation of cinnamaldehyde solution. Then, animals inhaled a solution of cinnamaldehyde (50 mM in saline with 3.5% Tween-80) for 10 min using an Omron compAIR NE-C28 compression nebulizer. The comparator drug butamirate was given p.o. at a dose of 5 mg/kg according to the same regimen. The evaluation of antitussive activity was carried out by counting the number of coughs within 20 min and expressed as percentage of inhibition in comparison to control group of animals, which received the vehicle instead of XC8.
Cough Induced by Capsaicin
Cough challenge with capsaicin (30 µM) was performed by inhalation for 5 min using an Omron compAIR NE-C28 compression nebulizer with subsequent measurements of coughs within 15 min. The treatment of guinea pigs with XC8 (at doses 0.14, 1.4, and 14 mg/kg) was done before the challenge at 0.5, 1, 3, 6, 12, or 24 h. Control animals received distilled water with 1% Tween-80 instead of XC8. Butamirate was used as a comparator drug at a dose of 5 mg/kg according to the same regimen. The evaluation of antitussive activity was carried out manually by counting the number of coughs within 15 min from the start of inhalation and expressed as percentage of inhibition in comparison to control group of animals.
Ion Channel Activity
P2X2 Receptor
The interaction of XC8 with the P2X2 ion channel was studied using the Fluorescent Imaging Plate Reader (FLIPR) assay by SB Drug Discovery (UK). Human P2X2 cells were trypsinized, counted, and seeded in black, clear-bottomed 96 well plates at a density of 50,000 cells per well in 100 µl volume and incubated overnight. Next day, media (DMEM containing 10% FBS, and 2 mM l-glutamine) was removed from cell plates and assay buffer (1.26 mM CaCl2, 0.49 mM MgCl2 0.6H2O, 0.41 mM MgSO4 0.7H2O, 5.63 mM KCl, 0.44 mM KH2 PO4, 138 mM NaCl, 0.34 mM Na2 HPO4, 5.5 mM d-glucose, 20 mM HEPES) was added. Calcium 5 dye (Molecular Devices, USA, R8185) solution was then added to the wells and incubated at room temperature for 50 min. Calcium 5 Dye solution was prepared in assay buffer according to the manufacturer’s instructions. For agonist testing: the plates were placed in the FLIPR, after incubation with dye, and fluorescence monitored every 1 s. After 20 s, test compound XC8 or reference agonist was added to the wells and the fluorescence monitored for 5 min at ex/emm: 488 nm/510–570 nm. For antagonist testing: the test compound XC8 and reference inhibitors were added to the wells and incubated at room temperature for 10 min. The plates were then placed in the FLIPR and fluorescence monitored every 1 s. After 20 s, the reference agonist, BzATP, was added and the fluorescence monitored for 5 min at ex/emm: 488 nm/510–570 nm.
hTRPA1 and hASIC3 Receptors
The interaction of XC8 with hTRPA1 and hASIC3 ion channels was studied using the FLIPRTETRA and Ion Flux platform, respectively, by Eurofins (France).
For the hTPRA1 FLIPR assay, the compound XC8 was prepared in assay buffer to the final concentration 50 µM. The compound wells, reference agonist allyl isothiocyanate (AITC), reference antagonist Ruthenium Red, and background vehicle controls were prepared in DMSO (0.3%). All wells were prepared using FLIPR assay buffer. The reference agonist for each ion channel assay was prepared in a similar manner to serve as assay control. The reference agonist for each ion channel was included at Emax (the concentration where the reference agonist elicited a maximal response). The agonist assay was conducted on a FLIPRTETRA instrument where the test compound XC8, vehicle controls, and reference agonist were added to the assay plate after a fluorescence baseline was established. The agonist assay was a total of 180 s and was used to assess the compound’s ability to activate each ion channel assayed.
For the antagonist assay, compound XC8 was added on the FLIPRTETRA and pre-incubated for 5 min at room temperature. Using historic EC80 potency values, all the pre-incubated sample compound wells were challenged with an EC80 concentration of reference agonist after the establishment of a fluorescence baseline. The antagonist assay was conducted on a FLIPRTETRA instrument where vehicle controls and an EC80 concentration of reference agonist were added to the appropriate wells. The antagonist assay (total of 180 s) was used to assess the compound’s ability to inhibit each ion channel assayed.
For the hASIC3 IonFlux HT Agonist Assay, all recordings were obtained from a holding potential of − 60 mV. Cells were exposed to a pH 7.4 external assay solution to establish a baseline response. One addition of the pH 5.5 external assay solution was added for 2 s to establish an ASIC3 peak current response and test concentration of compound XC8 in pH 7.4 was applied for 2 s to detect the agonist response. Results showing an inhibition or stimulation higher than 50% are considered to represent significant effects of the test compounds.
TRPM8 and TRPV1 Channels
The activity of XC8 was studied in cellular and nuclear receptor functional assays in a concentration of 50 µM according to Phelps et al. and Behrendt et al. [37, 38]. The study was performed by Eurofins. The cellular agonist effect was calculated as a percentage of the control response to a known reference agonist for each target, and the cellular antagonist effect was calculated as a percentage of the inhibition of control reference agonist response for each target. In each experiment, if applicable, the respective reference compound was tested concurrently with the test compounds, and the data were compared with historical values determined at Eurofins. The experiment was made in accordance with validation Standard Operating Procedure of Eurofins.
Statistics
Comparison of the data obtained from several experimental groups with one control group was performed by a one-way ANOVA or two-way ANOVA with Dunnett’s multiple comparison test. Data are presented as mean (M) ± standard deviation (SD). The software GrafPadPrism version 8.0 was used for calculations.
Results
The Effect of XC8 on Cough Induced by a Single Inhalation of Citric Acid with or Without IFN-γ
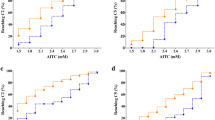
In humans, cough can be initiated by different irritants, such as cigarette smoke, acids, hyper- and hypotonic solutions, capsaicin, or prostanoids [13,14,15]. Patients exhibit a divergent response to various tussive stimuli suggesting the existence of several neurophenotypes of airway diseases evoked by distinct mechanisms [23]. We investigated the effect of XC8 on cough induced by several agonists activating various receptors in male guinea pigs. First, we estimated the effect of XC8 on cough induced by the inhalation of citric acid. Acid is known to activate the TRPV1 and TRPA1 channels, but the activation of the airway sensory nerve depends on the magnitude and rate of pH change [14]. Before we found that the most pronounced anti-asthmatic effect of XC8 on guinea pigs was observed in the dose range of 1.4–7.0 mg/ kg, which corresponds to 20–100 mg per day for humans [33]. In phase 2a clinical trial, the highest anti-asthmatic effect of XC8 was observed for a dose of 100 mg per day [35]. Therefore, we chose the dose range of XC8 from 0.7 to 14.0 mg/kg for oral administration to animals. Control animals received the vehicle. In 7 h of XC8 dosing, all of the animals were inhaled with a 0.3 M citric acid and antitussive activity was assessed by counting the number of coughs (see experiment scheme, Fig. 1a). XC8 showed the pronounced dose-dependent effect on cough with the maximal inhibition of 67.1% at a dose of 5.6 mg/kg (Fig. 1b, d).
The effect of XC8 treatment on cough induced in guinea pigs by a single inhalation of citric acid alone or in combination with IFN-γ. a Experimental scheme. Animals (ten per group) were treated with XC8 at doses from 0.7 to 14 mg/kg p.o., or with vehicle (control group) 7 h before the inhalation of citric acid (0.3 M in PBS) alone (b), or in combination with IFN-γ (10 mg/kg) (c). The number of coughs was recorded from the start of inhalation and presented in absolute numbers (b, c) or as a percentage of inhibition (d, e). The data are presented as M ± SD. The stars (****) indicate the significant difference when compared to the control group determined by a one-way ANOVA followed by Dunnett’s multiple comparison test, p < 0.0001; ns not significant
The IFN-γ was shown to enhance the cough response to citric acid in guinea pigs by the depolarization of membranes [6]. We were interested whether XC8 can inhibit the cough induced by citric acid and enhanced by IFN-γ. IFN-γ was administered to the animals just before the administration of XC8. As shown in Fig. 1b, the addition of IFN-γ to the citric acid increased the cough frequency by 42% (from 22.1 to 31.6 coughs/8 min). The maximal inhibition effect of XC8 on cough evoked by citric acid in combination with IFN-γ comprised 76.4% observed for the dose of XC8 4.2 mg/kg. The effect of XC8 on cough induced by citric acid combined with IFN-γ was more pronounced than on cough induced by citric acid alone, indicating that IFN-γ cough potentiation was successfully resolved by XC8.
The Effect of XC8 on Chronic Cough Induced by Multiple Inhalations of Citric Acid
Chronic cough in guinea pigs can be modeled by repeated inhalation of citric acid [39]. We aimed to assess the effect of tachyphylaxis by the tested drug XC8. To do this, the animals received XC8 (at doses of 1.4, 7.0, and 14 mg/kg p.o.), 1 h before the inhalation of the citric acid solution within 6 days every day (Fig. 2). The control animals received the vehicle instead of XC8. Butamirate was used as a comparator drug.
The effect of XC8 on the cough induced by the repeated inhalation of citric acid to guinea pigs. a Experimental scheme. Groups of 15 animals were treated with XC8 at doses of 1.4, 7, or 14 mg/kg p.o. before the inhalation (0, 1, 2, 3, 4, 5, or 6 days) with citric acid (0.3 M in PBS). Control animals received the vehicle. Butamirate was administered in the same way at a dose of 5 mg/kg. b The number of coughs was measured from the start of inhalation and expressed as percentage of inhibition. Data are presented as M ± SD. The stars indicate the significant difference compared to the control group determined by two-way ANOVA followed by Dunnett’s multiple comparison test, (****) indicates p < 0.0001, (*) indicates p < 0.05; ns not significant
The results showed that the administration of XC8 at doses of 7.0 and 14 mg/kg resulted in a statistically significant reduction of coughs induced by the repeated inhalation of citric acid from 1 to 5 consecutive days. The observed cough suppression ranged from 22 to 80%. The effect of XC8 observed after treatment at doses of 7.0 and 14 mg/kg was comparable to the reference antitussive drug butamirate. At lower dose (1.4, mg/kg), the effect of XC8 was less pronounced.
The Effect of XC8 on Cough Induced by the Inhalation of Cinnamaldehyde
Next, we assessed the effect of XC8 on cough induced by cinnamaldehyde, activator of TRPA1 channel. The TRPA1 channel is co-expressed with TRPV1 and is present on airway-innervating C-fibers [40]. TRPA1 is a chemo-sensitive receptor activated by cinnamaldehyde [41], nicotine [42], ozone, menthol [43], formalin, tear gases, and mustard oil. In addition, TRPA1 serves as a sensor for the cold temperature and early detection of bacterial lipopolysaccharide (LPS) [44, 45].
Animals were treated with XC8 (0.14, 1.4, or 14 mg/kg, p.o.) 1, 3, 6, 8, 12 h before the inhalation of 50 mM cinnamaldehyde solution. The group of control animals received the vehicle instead of XC8 (Fig. 3a). The results of the study show that XC8 significantly reduced the coughs in guinea pigs caused by the inhalation of cinnamaldehyde (Fig. 3b). The most pronounced effect of the XC8 was observed when it was administered 3 and 6 h before the inhalation at doses of 1.4 and 14 mg/kg, achieving up to 60% inhibition of the coughs. The comparator drug butamirate showed a similar effect on cough inhibition (up to 60%) with a maximal difference to control observed when administered 6 h before the inhalation of cinnamaldehyde.
The effect of XC8 on the of cough hypersensitivity induced by inhalation of cinnamaldehyde to guinea pigs. a Experimental scheme. Animals (ten per group) were treated with XC8 (0.14, 1.4 or 14 mg/kg p.o.) on 1, 3, 6, 8, or 12 h before inhalation of cinnamaldehyde (50 mM) for 10 min. Group of control animals received the vehicle. b The number of coughs was measured from the start of inhalation and expressed as percentage of inhibition. Data are presented as M ± SD. The stars indicate the significant difference in comparison to the control group (treated with vehicle) determined by two-way ANOVA followed by Dunnett’s multiple comparison test, (****) indicates p < 0.0001, (***) indicates p < 0.001, (**) indicates p < 0.01, (*) indicates p < 0.05; ns not significant
The Effect of XC8 on Cough Induced by the Inhalation of Capsaicin
Next, we investigated the effect of XC8 on cough induced by capsaicin. Capsaicin is known to activate the TRPV1 channel, which also can be activated by heat and low pH. Activation of TRPV1 induces calcium influx and membrane depolarization, which in turn leads to neurogenic inflammation [46]. Cough challenge was performed with capsaicin. Animals were treated with XC8 (0, 14, 1.4, and 14 mg/kg p.o.) before the challenge at 0.5, 1, 3, 6, 12, or 24 h. Group of control animals received the vehicle. Butamirate was used as a comparator drug (Fig. 4a). XC8 demonstrated very limited activity against cough evoked by capsaicin (Fig. 4b). Statistically significant reduction of coughs was shown only on late time point 12 h at 14 mg/kg of XC8. No statistically significant effect was shown for butamirate.
The effect of XC8 on the cough induced by the inhalation of capsaicin in guinea pigs. a Experimental scheme. Animals (10 per group) were treated with XC8 at doses of 0.14, 1.4, or 14 mg/kg at 0.5, 1, 3, 6, 12, or 24 h before the inhalation of capsaicin (30 µM in PBS) within 5 min. Group of control animals received the vehicle. b The number of coughs measured within 15 min from the start of inhalation and expressed as percentage of inhibition. Data are presented as M ± SD. The stars indicate the significant difference in comparison to the control group (treated with vehicle) determined by two-way ANOVA followed by Dunnett’s multiple comparison test, (*) indicates p < 0.05; ns not significant
Effect of XC8 on the P2X2, hTRPA1, hASIC3, TRPV1, and TRPM8 Channels In Vitro
To determine the mechanism of action of XC8 in cough model in guinea pigs we evaluated the activity of XC8 on P2X2, hTRPA1, hASIC3, TRPV1, and TRPM8 ion channels in Fluorescent Imaging Plate Reader (FLIPR) assay by SB Drug Discovery (UK) and by Eurofins (France). No agonistic/antagonistic activity of XC8 on any of these receptors (at a concentration of 50 µM) was revealed.
Discussion
XC8 has demonstrated a pronounced therapeutic effect on cough induced by the inhalation of citric acid or cinnamaldehyde, but not by capsaicin. It is believed that citric acid evokes a multimodal challenge affecting both TRPA1 and TRPV1 channels, expressed in the airway nerve endings of vagal C-fibers. However, Wang et al. have shown that weak organic acids activate the TRPA1 channel [47] because they diffuse into the cell causing intracellular acidification and changing the pH of the cytosol. In contrast, the TRPV1 channel reacts to extracellular protons from strong acids. Mukhopadhyay et al. demonstrated that the TRPA1 channel is a direct sensor for citric acid in three types of cells [48]. This observation was confirmed in experiments with the selective antagonist of the TRPV1 channel GRC 6211, which did not inhibit an increased Ca2+ influx induced by citric acid [49]. The effect of XC8 on cough caused by the single inhalations of citric acid was similar to that induced by the repeated inhalation of citric acid during 7 days. Moreover, XC8 reduced the cough caused by citric acid in combination with IFN-γ, which is known to enhance the cough reflex sensitivity [6]. The effect was even more pronounced (76.4%) than that induced by citric acid alone (67.1%). Another agonist of TRPA1 is cinnamaldehyde, which was shown to activate it specifically [40] while the activation can be inhibited by the HC030031 antagonist of TRPA1 [50]. The effect of XC8 on cough induced by cinnamaldehyde was comparable to that induced by the licensed drug butamirate.
Capsaicin acts specifically on TRPV1 channels. The effect of XC8 on cough induced by the inhalation of capsaicin did not show statistically significant difference compared to treatment with the vehicle. Therefore, XC8 acts exclusively against cough evoked by the activation of TRPA1, but not TRPV1 channels.
The TRPA1 ion channel is highly expressed on the C fibers innervating the entire respiratory tract as well as on the non-neuronal cells of respiratory tract including fibroblasts, epithelial cells (tracheal, bronchial, and alveolar), smooth muscle cells (SMC), and lymphocytes [51,52,53,54,55,56]. In addition to citric acid and cinnamaldehyde potential agonists of TRPA1 channel include cigarette smoke, reactive oxygen species (ROS), and hypochlorite, which are all known as asthma triggers. The increase in some of these stimuli has been observed in the lungs of asthma patients [57,58,59,60]. Neuronal ion channel TRPA1 plays a tremendous role in the induction of allergen-induced airway inflammation. The activation of the TRPA1 channel by different chemical irritants triggers the release of CGRP, SP, or NKA, known as mediators of neurogenic inflammation, and induce an inflammatory response with mucus production, local release of cytokines IL-5, IL-13, TNF-α, CCL11, and finally airway hyperreactivity (AHR) [61]. The blockade of TRPA1 channel by specific antagonist was shown to reduce the released neuropeptides and subsequent infiltration of airway eosinophils, mucus production, and AHR [61]. These data indicate that the TRPA1 channel is involved in the interaction of nervous and immune systems in the airways, causing asthmatic inflammation of airways after an exposure to an inhaled allergen.
The TRPV1 ion channel, which is activated by capsaicin is not involved in allergic airway inflammation in ovalbumin-induced asthma [61], but plays a role in the induction of chronic cough when stimulated by TRPV1-specific stimuli [62]. Non-asthmatic coughers were shown to have an increased expression of TRPV1 in epithelial nerves when compared to normal volunteers [20]. The inflammation induced by the activation of the TRPV1 channel was shown to be histamine-dependent, while the TRPA1 channel mediates a histamine-independent response [63]. The effect of XC8 on coughs induced by TRPA1 agonists suggests that pathological allergy resulting from neuro-immune interactions of TRPA1 with inflammatory factors may be a target for XC8 treatment.
Respiratory viruses such as human rhinovirus (HRV) and respiratory syncytial virus (RSV) infect human respiratory epithelial cells and cause about 75% of all asthma exacerbations in adults [64]. The infection of epithelial cells with viruses is known to induce the up-regulation of mRNA of both TRPV1 and TPRA1 channels. The upregulation of the TRPA1 channels in neuronal cells was demonstrated for HRV-16 [65, 66]. The expression of TRPA1 in the membrane of peripheral nerves does not require the virus replication and can be induced by released IL-6 and IL-8 proinflammatory cytokines [65]. The neutralization of IL-6 and IL-8 blocks the upregulation of both TRRV1 and TPRA1 channels [67]. These data indicate that TRPA1 ion channel activation could be involved in asthma exacerbations induced by respiratory viruses. Cough is also the most common symptom (79%) in COVID-19 patients [68]. It was shown that 34% of recovering patients have persistent cough [69]. Therefore, XC8 can have a beneficial effect in treating persistent cough and asthma exacerbations caused by respiratory viruses including SARS-CoV-2.
The exact mechanism of action of XC8 in the treatment of asthma and cough is not clear. The cough reflex is a complex biological process that involves multiple steps, including airway receptors, vagal nerve, CNS, muscles, and antitussive agents may interfere at any step of this process [70]. We’ve evaluated the activity of XC8 across most commonly affected cough targets and did not find any agonistic or antagonistic activity of XC8 on TRPV1, TRPA1, hASIC3, TRPM8, or P2X2 ion channels. This result suggests that the effect of XC8 is other than direct blocking of these channels.
One of the discovered actions of XC8 is the inhibition of the Golgi resident human glutamyl cyclase (gQC), the enzyme that catalyzes the pyroglutamination of chemokines of C– C motif family involved in many inflammatory disorders including asthma (unpublished data). Pyroglutamination is required for the potent chemotactic activity of CCL2, CCL7, CCL8, and CCL13 chemokines. Being released at the site of allergic inflammation, these chemokines act as chemoattractants and activators of eosinophils [71,72,73,74]. Binding of these chemokines to CCR receptors present on human eosinophils can induce their degranulation with the subsequent release of inflammatory mediators from specific granules, which are involved in tissue remodeling [75,76,77]. The CCR3 receptor was shown to play the major role in eosinophil chemotaxis [77]. By inhibiting gQC, XC8 can reduce the activity of CCL2, CCL7, CCL8, and CCL13 chemokines and finally suppresses the eosinophil-driven inflammation.
According to O’Connell et al. asthma resistance to treatment with glucocorticoids (GC) is caused by IFN-γ induced JAK/STAT signaling [78]. We have demonstrated that patients with an increased level of IFN-γ are sensitive to treatment with XC8, resulting in an improvement in FEV1 [35]. IFN-γ is known as a non-specific inducer of cough [79], which enhances the cough response when administered together with citric acid [6]. In our experiments, cough induced by citric acid combined with IFN-γ was sensitive to treatment with XC8, as XC8 completely abolished the IFN-γ enhancement effect and reduced cough frequency to the same level as without IFN- γ. We can assume that one mechanism by which XC8 suppresses cough is inhibition of IFN-γ induced signaling pathways. Such a mechanism could be relevant for cough conditions like asthma, COPD, and post-viral cough in patients with severe COVID-19 [67].
It is currently believed that TRPV1 and TRPA1 channels play a complex regulatory role in airway function and inflammatory diseases [80, 81]. The TRPV1 channel is likely involved in the pathophysiological condition of cough hypersensitivity [82]. However, the treatment of patients having refractory chronic cough with TRPV1 antagonists did not show a promising result, indicating more complex mechanism of this disease [83, 84]. The TRPA1 channel is considered as a more promising target for the treatment of cough or asthma with TRPA1-dependent neuronal inflammation [85]. Besides asthma, the upregulation of TRPA1 channel is implicated in the pathogenesis of such respiratory diseases as COPD, allergic rhinitis, and cystic fibrosis [52]. The TRPA1 channel is shown to be a major neuronal sensor of oxidative stress, present in patients with COPD [86]. The activation of TRPA1 channel on nerve endings in the skin causes local inflammation leading to dermatitis or psoriasis [87]. XC8 being effective in the treatment of cough induced by the activation of the TRPA1 channel can have significant potential in the treatment of other diseases mediated by this mechanism.
References
Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, Kim S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J. 2015;45(5):1479–81. https://doi.org/10.1183/09031936.00218714 (Epub 2015/02/07).
Satia I, Mayhew AJ, Sohel N, Kurmi O, Killian KJ, O'Byrne PM, Raina P. Prevalence, incidence and characteristics of chronic cough among adults from the Canadian Longitudinal Study on Aging. ERJ Open Res. 202;7(2):00160–2021. https://doi.org/10.1183/23120541.00160-2021
Chamberlain SA, Garrod R, Douiri A, Masefield S, Powell P, Bucher C, et al. The impact of chronic cough: a cross-sectional European survey. Lung. 2015;193(3):401–8. https://doi.org/10.1007/s00408-015-9701-2 (Epub 2015/03/20).
Morice AH, Millqvist E, Belvisi MG, Bieksiene K, Birring SS, Chung KF, et al. Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J. 2014;44(5):1132–48. https://doi.org/10.1183/09031936.00218613 (Epub 2014/08/22).
West PW, Canning BJ, Merlo-Pich E, Woodcock AA, Smith JA. Morphologic characterization of nerves in whole-mount airway biopsies. Am J Respir Crit Care Med. 2015;192(1):30–9. https://doi.org/10.1164/rccm.201412-2293OC (Epub 2015/04/24).
Deng Z, Zhou W, Sun J, Li C, Zhong B, Lai K. IFN-gamma enhances the cough reflex sensitivity via calcium influx in vagal sensory neurons. Am J Respir Crit Care Med. 2018;198(7):868–79.
Clarke R, Monaghan K, About I, Griffin CS, Sergeant GP, El Karim I, et al. TRPA1 activation in a human sensory neuronal model: relevance to cough hypersensitivity? Eur Respir J. 2017. https://doi.org/10.1183/13993003.00995-2017 (Epub 2017/09/22).
McGovern AE, Mazzone SB. Neural regulation of inflammation in the airways and lungs. Auton Neurosci. 2014;182:95–101. https://doi.org/10.1016/j.autneu.2013.12.008 (Epub 2014/01/15).
Lin RL, Gu Q, Khosravi M, Lee LY. Sustained sensitizing effects of tumor necrosis factor alpha on sensory nerves in lung and airways. Pulm Pharmacol Ther. 2017;47:29–37. https://doi.org/10.1016/j.pupt.2017.06.001 (Epub 2017/06/08).
Niimi A, Torrego A, Nicholson AG, Cosio BG, Oates TB, Chung KF. Nature of airway inflammation and remodeling in chronic cough. J Allergy Clin Immunol. 2005;116(3):565–70. https://doi.org/10.1016/j.jaci.2005.07.010 (Epub 2005/09/15).
Lieu T, Undem BJ. Neuroplasticity in vagal afferent neurons involved in cough. Pulm Pharmacol Ther. 2011;24(3):276–9. https://doi.org/10.1016/j.pupt.2011.02.003 (Epub 2011/03/08).
Widdicombe JG. Respiratory reflexes from the trachea and bronchi of the cat. J Physiol. 1954;123(1):55–70. https://doi.org/10.1113/jphysiol.1954.sp005033 (Epub 1954/01/01).
Gravenstein JS, Devloo RA, Beecher HK. Effect of antitussive agents on experimental and pathological cough in man. J Appl Physiol. 1954;7(2):119–39. https://doi.org/10.1152/jappl.1954.7.2.119 (Epub 1954/09/01).
Lalloo UG, Fox AJ, Belvisi MG, Chung KF, Barnes PJ. Capsazepine inhibits cough induced by capsaicin and citric acid but not by hypertonic saline in guinea pigs. J Appl Physiol (1985). 1995;79(4):1082–7. https://doi.org/10.1152/jappl.1995.79.4.1082 (Epub 1995/10/01).
Karlsson JA, Fuller RW. Pharmacological regulation of the cough reflex–from experimental models to antitussive effects in man. Pulm Pharmacol Ther. 1999;12(4):215–28. https://doi.org/10.1006/pupt.1999.0207 (Epub 1999/09/29).
Nishino T, Tagaito Y, Isono S. Cough and other reflexes on irritation of airway mucosa in man. Pulm Pharmacol. 1996;9(5–6):285–92. https://doi.org/10.1006/pulp.1996.0037 (Epub 1996/10/01).
Brooks SM. Irritant-induced chronic cough: irritant-induced TRPpathy. Lung. 2008;186(Suppl 1):S88-93. https://doi.org/10.1007/s00408-007-9068-0 (Epub 2008/02/02).
Weller K, Reeh PW, Sauer SK. TRPV1, TRPA1, and CB1 in the isolated vagus nerve–axonal chemosensitivity and control of neuropeptide release. Neuropeptides. 2011;45(6):391–400. https://doi.org/10.1016/j.npep.2011.07.011 (Epub 2011/08/27).
Morice AH, Geppetti P. Cough. 5: the type 1 vanilloid receptor: a sensory receptor for cough. Thorax. 2004;59(3):257–8. https://doi.org/10.1136/thx.2003.013482 (Epub 2004/02/27).
Groneberg DA, Niimi A, Dinh QT, Cosio B, Hew M, Fischer A, et al. Increased expression of transient receptor potential vanilloid-1 in airway nerves of chronic cough. Am J Respir Crit Care Med. 2004;170(12):1276–80. https://doi.org/10.1164/rccm.200402-174OC (Epub 2004/09/28).
Satia I, Tsamandouras N, Holt K, Badri H, Woodhead M, Ogungbenro K, et al. Capsaicin-evoked cough responses in asthmatic patients: evidence for airway neuronal dysfunction. J Allergy Clin Immunol. 2017;139(3):771 e10-779 e10. https://doi.org/10.1016/j.jaci.2016.04.045 (Epub 2016/07/23).
Birrell MA, Belvisi MG, Grace M, Sadofsky L, Faruqi S, Hele DJ, et al. TRPA1 agonists evoke coughing in guinea pig and human volunteers. Am J Respir Crit Care Med. 2009;180(11):1042–7. https://doi.org/10.1164/rccm.200905-0665OC (Epub 2009/09/05).
Belvisi MG, Birrell MA, Khalid S, Wortley MA, Dockry R, Coote J, et al. Neurophenotypes in airway diseases. Insights from translational cough studies. Am J Respir Crit Care Med. 2016;193(12):1364–72. https://doi.org/10.1164/rccm.201508-1602OC (Epub 2016/01/08).
Satia I, Watson R, Scime T, Dockry RJ, Sen S, Ford JW, et al. Allergen challenge increases capsaicin-evoked cough responses in patients with allergic asthma. J Allergy Clin Immunol. 2019;144(3):788 e1-795 e1. https://doi.org/10.1016/j.jaci.2018.11.050 (Epub 2019/01/21).
Morice AH. The cough hypersensitivity syndrome: a novel paradigm for understanding cough. Lung. 2010;188(Suppl 1):S87-90. https://doi.org/10.1007/s00408-009-9185-z (Epub 2009/10/08).
Chung KF. Chronic ‘cough hypersensitivity syndrome’: a more precise label for chronic cough. Pulm Pharmacol Ther. 2011;24(3):267–71. https://doi.org/10.1016/j.pupt.2011.01.012 (Epub 2011/02/05).
Takahara N, Ito S, Furuya K, Naruse K, Aso H, Kondo M, et al. Real-time imaging of ATP release induced by mechanical stretch in human airway smooth muscle cells. Am J Respir Cell Mol Biol. 2014;51(6):772–82. https://doi.org/10.1165/rcmb.2014-0008OC (Epub 2014/06/03).
Srisomboon Y, Squillace DL, Maniak PJ, Kita H, O’Grady SM. Fungal allergen-induced IL-33 secretion involves cholesterol-dependent, VDAC-1-mediated ATP release from the airway epithelium. J Physiol. 2020;598(10):1829–45. https://doi.org/10.1113/JP279379 (Epub 2020/02/28).
Sher L. Post-COVID syndrome and suicide risk. QJM. 2021;114(2):95–8. https://doi.org/10.1093/qjmed/hcab007 (Epub 2021/01/25).
Niimi A, Fukumitsu K, Takeda N, Kanemitsu Y. Interfering with airway nerves in cough associated with asthma. Pulm Pharmacol Ther. 2019;59:101854. https://doi.org/10.1016/j.pupt.2019.101854 (Epub 2019/11/05).
Niimi A, Matsumoto H, Mishima M. Eosinophilic airway disorders associated with chronic cough. Pulm Pharmacol Ther. 2009;22(2):114–20. https://doi.org/10.1016/j.pupt.2008.12.001 (Epub 2009/01/06).
Choudry NB, Fuller RW, Pride NB. Sensitivity of the human cough reflex: effect of inflammatory mediators prostaglandin E2, bradykinin, and histamine. Am Rev Respir Dis. 1989;140(1):137–41. https://doi.org/10.1164/ajrccm/140.1.137 (Epub 1989/07/01).
Ferko B, Romanova J, Rydlovskaya AV, Kromova TA, Proskurina OV, Amelina AN, et al. A novel oral glutarimide derivative XC8 suppresses sephadex-induced lung inflammation in rats and ovalbumin-induced acute and chronic asthma in guinea PIGS. Curr Pharm Biotechnol. 2019;20(2):146–56. https://doi.org/10.2174/1389201020666190215103505 (Epub 2019/02/16).
Renner A, Romanova J, Ferko B, Schmutz H, Nebolsin V, Muller M, et al. Safety, pharmacokinetics and pharmacodynamics of a novel anti-asthmatic drug, XC8, in healthy probands. Pulm Pharmacol Ther. 2019;59:101852. https://doi.org/10.1016/j.pupt.2019.101852 (Epub 2019/10/10).
Romanova J, Chikina E, Rydlovskaya A, Pohl W, Renner A, Zeifman A, et al. New anti-chemokine oral drug XC8 in the treatment of asthma patients with poor response to corticosteroids: results of a phase 2A randomized controlled clinical trial. Pulm Ther. 2020;6(2):351–69. https://doi.org/10.1007/s41030-020-00134-5 (Epub 2020/10/24).
In Guide for the Care and Use of Laboratory Animals, th, Ed. Washington (DC), 2011. https://www.ncbi.nlm.nih.gov/pubmed/?term=Mojtabavi%2C+N.%3B+Dekan%2C+G.+2002. Accessed 18 October
Phelps PT, Anthes JC, Correll CC. Cloning and functional characterization of dog transient receptor potential vanilloid receptor-1 (TRPV1). Eur J Pharmacol. 2005;513(1–2):57–66. https://doi.org/10.1016/j.ejphar.2005.02.045 (Epub 2005/05/10).
Behrendt HJ, Germann T, Gillen C, Hatt H, Jostock R. Characterization of the mouse cold-menthol receptor TRPM8 and vanilloid receptor type-1 VR1 using a fluorometric imaging plate reader (FLIPR) assay. Br J Pharmacol. 2004;141(4):737–45. https://doi.org/10.1038/sj.bjp.0705652 (Epub 2004/02/06).
Xu X, Chen Q, Qiu Z, Shi C, Ding H, Wang L, et al. Association of cough hypersensitivity with tracheal TRPV1 activation and neurogenic inflammation in a novel guinea pig model of citric acid-induced chronic cough. J Int Med Res. 2018;46(7):2913–24. https://doi.org/10.1177/0300060518778951 (Epub 2018/06/08).
Nassenstein C, Kwong K, Taylor-Clark T, Kollarik M, Macglashan DM, Braun A, et al. Expression and function of the ion channel TRPA1 in vagal afferent nerves innervating mouse lungs. J Physiol. 2008;586(6):1595–604. https://doi.org/10.1113/jphysiol.2007.148379 (Epub 2008/01/26).
Bandell M, Story GM, Hwang SW, Viswanath V, Eid SR, Petrus MJ, et al. Noxious cold ion channel TRPA1 is activated by pungent compounds and bradykinin. Neuron. 2004;41(6):849–57. https://doi.org/10.1016/s0896-6273(04)00150-3 (Epub 2004/03/30).
Talavera K, Gees M, Karashima Y, Meseguer VM, Vanoirbeek JA, Damann N, et al. Nicotine activates the chemosensory cation channel TRPA1. Nat Neurosci. 2009;12(10):1293–9. https://doi.org/10.1038/nn.2379 (Epub 2009/09/15).
Ryckmans T, Aubdool AA, Bodkin JV, Cox P, Brain SD, Dupont T, et al. Design and pharmacological evaluation of PF-4840154, a non-electrophilic reference agonist of the TrpA1 channel. Bioorg Med Chem Lett. 2011;21(16):4857–9. https://doi.org/10.1016/j.bmcl.2011.06.035 (Epub 2011/07/12).
Meseguer V, Alpizar YA, Luis E, Tajada S, Denlinger B, Fajardo O, et al. TRPA1 channels mediate acute neurogenic inflammation and pain produced by bacterial endotoxins. Nat Commun. 2014;5:3125. https://doi.org/10.1038/ncomms4125 (Epub 2014/01/22).
Karashima Y, Talavera K, Everaerts W, Janssens A, Kwan KY, Vennekens R, et al. TRPA1 acts as a cold sensor in vitro and in vivo. Proc Natl Acad Sci USA. 2009;106(4):1273–8. https://doi.org/10.1073/pnas.0808487106 (Epub 2009/01/16).
Kollarik M, Undem BJ. Sensory transduction in cough-associated nerves. Respir Physiol Neurobiol. 2006;152(3):243–54. https://doi.org/10.1016/j.resp.2005.12.008 (Epub 2006/01/31).
Wang YY, Chang RB, Allgood SD, Silver WL, Liman ER. A TRPA1-dependent mechanism for the pungent sensation of weak acids. J Gen Physiol. 2011;137(6):493–505. https://doi.org/10.1085/jgp.201110615 (Epub 2011/05/18).
Mukhopadhyay I, Kulkarni A, Aranake S, Karnik P, Shetty M, Thorat S, et al. Transient receptor potential ankyrin 1 receptor activation in vitro and in vivo by pro-tussive agents: GRC 17536 as a promising anti-tussive therapeutic. PLoS ONE. 2014;9(5):e97005. https://doi.org/10.1371/journal.pone.0097005 (Epub 2014/05/14).
Xia R, Dekermendjian K, Lullau E, Dekker N. TRPV1: a therapy target that attracts the pharmaceutical interests. Adv Exp Med Biol. 2011;704:637–65. https://doi.org/10.1007/978-94-007-0265-3_34 (Epub 2011/02/04).
Andre E, Gatti R, Trevisani M, Preti D, Baraldi PG, Patacchini R, et al. Transient receptor potential ankyrin receptor 1 is a novel target for pro-tussive agents. Br J Pharmacol. 2009;158(6):1621–8. https://doi.org/10.1111/j.1476-5381.2009.00438.x (Epub 2009/10/23).
Jaquemar D, Schenker T, Trueb B. An ankyrin-like protein with transmembrane domains is specifically lost after oncogenic transformation of human fibroblasts. J Biol Chem. 1999;274(11):7325–33. https://doi.org/10.1074/jbc.274.11.7325 (Epub 1999/03/06).
Mukhopadhyay I, Kulkarni A, Khairatkar-Joshi N. Blocking TRPA1 in respiratory disorders: does it hold a promise? Pharmaceuticals (Basel). 2016. https://doi.org/10.3390/ph9040070 (Epub 2016/11/10).
Nassini R, Pedretti P, Moretto N, Fusi C, Carnini C, Facchinetti F, et al. Transient receptor potential ankyrin 1 channel localized to non-neuronal airway cells promotes non-neurogenic inflammation. PLoS ONE. 2012;7(8):e42454. https://doi.org/10.1371/journal.pone.0042454 (Epub 2012/08/21).
Kannler M, Luling R, Yildirim AO, Gudermann T, Steinritz D, Dietrich A. TRPA1 channels: expression in non-neuronal murine lung tissues and dispensability for hyperoxia-induced alveolar epithelial hyperplasia. Pflugers Arch. 2018;470(8):1231–41. https://doi.org/10.1007/s00424-018-2148-6 (Epub 2018/05/14).
Wang M, Zhang Y, Xu M, Zhang H, Chen Y, Chung KF, et al. Roles of TRPA1 and TRPV1 in cigarette smoke-induced airway epithelial cell injury model. Free Radic Biol Med. 2019;134:229–38. https://doi.org/10.1016/j.freeradbiomed.2019.01.004 (Epub 2019/01/15).
Yap JMG, Ueda T, Takeda N, Fukumitsu K, Fukuda S, Uemura T, et al. An inflammatory stimulus sensitizes TRPA1 channel to increase cytokine release in human lung fibroblasts. Cytokine. 2020;129:155027. https://doi.org/10.1016/j.cyto.2020.155027 (Epub 2020/02/13).
Bautista DM, Jordt SE, Nikai T, Tsuruda PR, Read AJ, Poblete J, et al. TRPA1 mediates the inflammatory actions of environmental irritants and proalgesic agents. Cell. 2006;124(6):1269–82. https://doi.org/10.1016/j.cell.2006.02.023 (Epub 2006/03/28).
Jordt SE, Bautista DM, Chuang HH, McKemy DD, Zygmunt PM, Hogestatt ED, et al. Mustard oils and cannabinoids excite sensory nerve fibres through the TRP channel ANKTM1. Nature. 2004;427(6971):260–5. https://doi.org/10.1038/nature02282 (Epub 2004/01/09).
McNamara CR, Mandel-Brehm J, Bautista DM, Siemens J, Deranian KL, Zhao M, et al. TRPA1 mediates formalin-induced pain. Proc Natl Acad Sci USA. 2007;104(33):13525–30. https://doi.org/10.1073/pnas.0705924104 (Epub 2007/08/10).
Dai Y, Wang S, Tominaga M, Yamamoto S, Fukuoka T, Higashi T, et al. Sensitization of TRPA1 by PAR2 contributes to the sensation of inflammatory pain. J Clin Investig. 2007;117(7):1979–87. https://doi.org/10.1172/JCI30951 (Epub 2007/06/16).
Caceres AI, Brackmann M, Elia MD, Bessac BF, del Camino D, D’Amours M, et al. A sensory neuronal ion channel essential for airway inflammation and hyperreactivity in asthma. Proc Natl Acad Sci USA. 2009;106(22):9099–104. https://doi.org/10.1073/pnas.0900591106 (Epub 2009/05/22).
McLeod RL, Fernandez X, Correll CC, Phelps TP, Jia Y, Wang X, et al. TRPV1 antagonists attenuate antigen-provoked cough in ovalbumin sensitized guinea pigs. Cough. 2006;2:10. https://doi.org/10.1186/1745-9974-2-10 (Epub 2006/12/19).
Voisin T, Bouvier A, Chiu IM. Neuro-immune interactions in allergic diseases: novel targets for therapeutics. Int Immunol. 2017;29(6):247–61. https://doi.org/10.1093/intimm/dxx040 (Epub 2017/08/18).
Johnston SL, Pattemore PK, Sanderson G, Smith S, Lampe F, Josephs L, et al. Community study of role of viral infections in exacerbations of asthma in 9–11 year old children. BMJ. 1995;310(6989):1225–9. https://doi.org/10.1136/bmj.310.6989.1225 (Epub 1995/05/13).
Abdullah H, Heaney LG, Cosby SL, McGarvey LP. Rhinovirus upregulates transient receptor potential channels in a human neuronal cell line: implications for respiratory virus-induced cough reflex sensitivity. Thorax. 2014;69(1):46–54. https://doi.org/10.1136/thoraxjnl-2013-203894 (Epub 2013/09/05).
Omar S, Clarke R, Abdullah H, Brady C, Corry J, Winter H, et al. Respiratory virus infection up-regulates TRPV1, TRPA1 and ASICS3 receptors on airway cells. PLoS ONE. 2017;12(2):e0171681. https://doi.org/10.1371/journal.pone.0171681 (Epub 2017/02/12).
Wang Z, Yang Y, Yang H, Capo-Aponte JE, Tachado SD, Wolosin JM, et al. NF-kappaB feedback control of JNK1 activation modulates TRPV1-induced increases in IL-6 and IL-8 release by human corneal epithelial cells. Mol Vis. 2011;17:3137–46 (Epub 2011/12/16).
Chen HJ, Qiu J, Wu B, Huang T, Gao Y, Wang ZP, et al. Early chest CT features of patients with 2019 novel coronavirus (COVID-19) pneumonia: relationship to diagnosis and prognosis. Eur Radiol. 2020;30(11):6178–85. https://doi.org/10.1007/s00330-020-06978-4 (Epub 2020/06/11).
Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, et al. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2021;76(4):396–8. https://doi.org/10.1136/thoraxjnl-2020-215818 (Epub 2020/11/12).
Reynolds SM, Mackenzie AJ, Spina D, Page CP. The pharmacology of cough. Trends Pharmacol Sci. 2004;25(11):569–76. https://doi.org/10.1016/j.tips.2004.09.009 (Epub 2004/10/20).
Cynis H, Hoffmann T, Friedrich D, Kehlen A, Gans K, Kleinschmidt M, et al. The isoenzyme of glutaminyl cyclase is an important regulator of monocyte infiltration under inflammatory conditions. EMBO Mol Med. 2011;3(9):545–58. https://doi.org/10.1002/emmm.201100158 (Epub 2011/07/21, PubMed PMID: 21774078).
Proudfoot AE. Chemokine receptors: multifaceted therapeutic targets. Nat Rev Immunol. 2002;2(2):106–15. https://doi.org/10.1038/nri722 (Epub 2002/03/26).
Dunzendorfer S, Kaneider NC, Kaser A, Woell E, Frade JM, Mellado M, et al. Functional expression of chemokine receptor 2 by normal human eosinophils. J Allergy Clin Immunol. 2001;108(4):581–7. https://doi.org/10.1067/mai.2001.118518 (Epub 2001/10/09).
Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res. 2009;29(6):313–26. https://doi.org/10.1089/jir.2008.0027 (Epub 2009/05/16).
Gleich GJ, Adolphson CR, Leiferman KM. The biology of the eosinophilic leukocyte. Annu Rev Med. 1993;44:85–101. https://doi.org/10.1146/annurev.me.44.020193.000505 (Epub 1993/01/01).
Nagase H, Yamaguchi M, Jibiki S, Yamada H, Ohta K, Kawasaki H, et al. Eosinophil chemotaxis by chemokines: a study by a simple photometric assay. Allergy. 1999;54(9):944–50. https://doi.org/10.1034/j.1398-9995.1999.00184.x (Epub 1999/10/03).
Fujisawa T, Kato Y, Nagase H, Atsuta J, Terada A, Iguchi K, et al. Chemokines induce eosinophil degranulation through CCR-3. J Allergy Clin Immunol. 2000;106(3):507–13. https://doi.org/10.1067/mai.2000.108311 (Epub 2000/09/13).
O’Connell D, Bouazza B, Kokalari B, Amrani Y, Khatib A, Ganther JD, et al. IFN-gamma-induced JAK/STAT, but not NF-kappaB, signaling pathway is insensitive to glucocorticoid in airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2015;309(4):L348–59. https://doi.org/10.1152/ajplung.00099.2015 (Epub 2015/06/21).
Londino JD, Gulick DL, Lear TB, Suber TL, Weathington NM, Masa LS, et al. Post-translational modification of the interferon-gamma receptor alters its stability and signaling. Biochem J. 2017;474(20):3543–57. https://doi.org/10.1042/BCJ20170548 (Epub 2017/09/09).
Hajna Z, Cseko K, Kemeny A, Kereskai L, Kiss T, Perkecz A, et al. Complex regulatory role of the TRPA1 receptor in acute and chronic airway inflammation mouse models. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21114109 (Epub 2020/06/13).
Gu Q, Lee LY. TRP channels in airway sensory nerves. Neurosci Lett. 2021;748:135719. https://doi.org/10.1016/j.neulet.2021.135719 (Epub 2021/02/16).
Materazzi S, Nassini R, Gatti R, Trevisani M, Geppetti P. Cough sensors. II. Transient receptor potential membrane receptors on cough sensors. Handb Exp Pharmacol. 2009;187:49–61. https://doi.org/10.1007/978-3-540-79842-2_3 (Epub 2008/10/01).
Khalid S, Murdoch R, Newlands A, Smart K, Kelsall A, Holt K, et al. Transient receptor potential vanilloid 1 (TRPV1) antagonism in patients with refractory chronic cough: a double-blind randomized controlled trial. J Allergy Clin Immunol. 2014;134(1):56–62. https://doi.org/10.1016/j.jaci.2014.01.038 (Epub 2014/03/29).
Belvisi MG, Birrell MA, Wortley MA, Maher SA, Satia I, Badri H, et al. XEN-D0501, a novel transient receptor potential vanilloid 1 antagonist, does not reduce cough in patients with refractory cough. Am J Respir Crit Care Med. 2017;196(10):1255–63. https://doi.org/10.1164/rccm.201704-0769OC (Epub 2017/06/27).
Nassini R, Materazzi S, Andre E, Sartiani L, Aldini G, Trevisani M, et al. Acetaminophen, via its reactive metabolite N-acetyl-p-benzo-quinoneimine and transient receptor potential ankyrin-1 stimulation, causes neurogenic inflammation in the airways and other tissues in rodents. FASEB J. 2010;24(12):4904–16. https://doi.org/10.1096/fj.10-162438 (Epub 2010/08/20).
Taylor-Clark TE. Role of reactive oxygen species and TRP channels in the cough reflex. Cell Calcium. 2016;60(3):155–62. https://doi.org/10.1016/j.ceca.2016.03.007 (Epub 2016/03/27).
Kodji X, Arkless KL, Kee Z, Cleary SJ, Aubdool AA, Evans E, et al. Sensory nerves mediate spontaneous behaviors in addition to inflammation in a murine model of psoriasis. FASEB J. 2019;33(2):1578–94. https://doi.org/10.1096/fj.201800395RR (Epub 2018/09/12).
Acknowledgements
Funding
All of the experimental work and the journal’s Rapid Service Fee were financed by the Pharmenterprises LLC (Moscow, Russia).
Authorship
All of the listed authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, had full access to experimental data, and approved the current version of the manuscript.
Author Contributions
Dr. VN is the founder and CEO of the Pharmenterprises LLC, which develops new drugs. Dr. VN is the author of the XC8 molecule, the author of the idea, the initiator and the head of the project. Dr. AR is responsible for the development of the XC8 concept, design, planning, and analyzes of all animal experiments. Dr. OP is responsible for the performance of animal experiments. Dr. SM analyzed animal experiments and performed statistical analysis of the data. YG took part in analysis and interpretation of the results. Dr. JR analyzed all preclinical data, selected data for publication, and wrote the manuscript.
Disclosures
Vladimir Nebolsin is the author of the project, the founder, and the CEO of the company Pharmenterprises LLC. Julia Romanova, Anastasia Rydlovskaya, Stepan Mochalov, Oxana Proskurina, and Yulia Gorokh are employees of Pharmenterprises LLC and have nothing to disclose.
Compliance with Ethics Guidelines
All of the animal experiments were approved by the Animal Ethics Committee of LLC Pharmenterprises (protocols No. BEC 07/2020 dated 19.05.2020, and 09/2020 dated 14.07.2020). The experimental procedures with animals were performed in accordance with the Guide for the Care and Use of Laboratory Animals [36]. All the procedures with animals were performed under anesthesia to minimize their suffering.
Data Availability
All data are available from the corresponding author upon request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Romanova, J., Rydlovskaya, A., Mochalov, S. et al. The Effect of Anti-Chemokine Oral Drug XC8 on Cough Triggered by The Agonists of TRPA1 But Not TRPV1 Channels in Guinea Pigs. Pulm Ther 8, 105–122 (2022). https://doi.org/10.1007/s41030-022-00183-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-022-00183-y