Abstract
Introduction
Dry powder inhalers (DPIs), a commonly prescribed inhaler type for respiratory diseases, require patients to generate sufficient peak inspiratory flow (PIF) to ensure optimal drug delivery to the airways. Effectiveness of therapy also requires a good inhalation technique and adequate medication adherence. For patients with chronic obstructive pulmonary disease (COPD), recent studies conducted in tertiary care suggest that DPI users with suboptimal PIF have poorer COPD-related health status and increased exacerbation risk versus those with optimal PIF. The PIFotal study will investigate the impact of PIF, inhalation technique and medication adherence on patient-reported outcomes in patients with COPD in primary care using a DPI for their maintenance therapy.
Methods and Analysis
This cross-sectional observational study will assess 1200 patients (aged ≥ 40 years, diagnosed with COPD and using a DPI for COPD maintenance therapy for ≥ 3 months) from the Netherlands, Spain, Portugal, Poland, Greece and Australia. Assessments will consist of (1) PIF measurements (usual patient inhalation manoeuvre, maximal PIF against resistance of own inhaler, and maximal PIF against low resistance); (2) Clinical COPD Questionnaire (CCQ), COPD Assessment Test and Test of Adherence to Inhalers scores; and (3) video recordings of patient inhalation technique. Dependent variables include health status (CCQ score), number of self-reported exacerbations in previous 12 months, and healthcare resource utilisation in previous 6 months. Independent variables include PIF values, inhalation technique errors, medication adherence, and demographic and clinical characteristics. In the primary analysis, the mean difference in CCQ score between patients (1) with optimal/suboptimal PIF, (2) exhibiting/not exhibiting inhalation technique errors, and (3) adhering/not adhering to medication will be examined in a multivariable linear mixed model.
Ethics
The study protocol was approved by ethics committees/institutional review boards of all participating sites prior to enrolment; written informed consent was obtained from all study participants.
Trial Registration Number
ClinicalTrials.gov: NCT04532853.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In COPD, effectiveness of inhaled therapy delivered via dry powder inhalers (DPIs) requires generation of sufficient peak inspiratory flow (PIF), as well as good inhalation technique and medication adherence. |
PIFotal is a cross-sectional observational study that will investigate the effects of PIF, inhalation technique and medication adherence on patient-reported outcomes in patients with COPD within a primary care setting. |
Here, we report the methodology of the PIFotal COPD study. |
What will be learned from the study? |
Results from this study will enable better understanding of the relationship between PIF, inhalation technique, medication adherence and health status in DPI users. |
In contrast to previous studies, the assessment of PIF and inhalation manoeuvre will be measured objectively for a given inhaler using the In-Check DIAL device. |
In contrast to previous large studies, PIFotal will use video recordings with multiple assessors to objectify inhalation technique errors. |
Patients manifesting inhalation errors during their visit will receive tailored instruction in correct inhaler technique. |
Limitations include the cross-sectional study design, which does not allow the assessment of causality; recall bias associated with self-reported instruments; and no comparison of DPIs versus other inhaler types. |
In addition, the study only includes patients with stable COPD and not current exacerbations. |
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive lung condition that requires maintenance therapy for symptom control and prevention of exacerbations [1]. The dominant therapeutic strategy for COPD consists of inhaled therapy, which is most commonly delivered via dry powder inhalers (DPIs) [1, 2]. Indeed, in a large-scale analysis of real-world data from Europe, the USA, Japan and China, 89% of 3326 COPD patients were prescribed a DPI versus 19% prescribed a pressurised metered dose inhaler (pMDI) (some patients used more than one inhaler type for maintenance therapy) [3]. Furthermore, around 45% of inhaler-delivered medications listed as commonly used by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) can be delivered by DPIs [4]. More than 20 different DPIs are currently available, demonstrating varying performance levels dependent on the mechanism of disaggregation, aerosolisation, dose metering accuracy and inter-patient variability in the use of DPIs [4]. DPIs act as breath-actuated devices, many of which require the patient to generate sufficient peak inspiratory flow (PIF) to disaggregate the powder into particles with a diameter < 5 μm, which can then be inhaled into the lower respiratory tract [5–8]. The internal resistance of a device, and hence the flow required to overcome this resistance, varies with different DPI designs [5].
Prevalence data on suboptimal PIF are scarce in patients with COPD, particularly in primary care. Findings from observational studies suggest that 32–47% of inpatients admitted for exacerbations of COPD demonstrated a suboptimal PIF (< 60 L/min) prior to discharge; suboptimal PIF was also reported in 19–78% of stable outpatients with COPD [9]. In a small observational study of outpatients with COPD, suboptimal PIF (defined as PIF < 60 L/min for a low–medium-resistance device and PIF < 30 L/min for a high-resistance device) was seen in 40% of participants, suggesting that many patients do not generate sufficient inspiratory force to overcome the resistance of prescribed DPIs [6]. Several independent predictors for suboptimal PIF have been identified, including patient effort, female gender, shorter height and older age [6, 10, 11]. In order to judge whether a patient will be able to use and benefit from a DPI device, PIF should be measured in the clinical setting.
A limited number of studies have assessed the effect of PIF on clinical outcomes in patients with COPD. Recent studies have found that reduced PIF predicts both all-cause and COPD-related hospital readmission in patients with COPD [7]. In a retrospective analysis by Loh et al. [7], patients hospitalised with a COPD exacerbation and with PIF ≤ 60 L/min prior to discharge had significantly fewer days until the next all-cause and COPD readmission compared with those with a PIF > 60 L/min. Moreover, in patients discharged from the hospital, poor PIF is a predictor of readmission for COPD [7].
Inhalation technique is often suboptimal in patients with COPD [12, 13] and this can reduce the effectiveness of an inhaled therapy, regardless of inhaler type [14–17]. DPIs, for example, require patients to exhale fully before inhaling the medication, followed by a strong, deep inhalation [8]. In a prospective observational study by Sulaiman et al., low PIF (< 35 L/min) was found to be the most common inhaler technique error with DPIs, with 48% of COPD patients studied inhaling with insufficient effort from a DPI. [18] Other inhalers can also be associated with inhalation errors. For example, in a meta-analysis of 10 studies, the three most common errors associated with use of pMDIs in 1105 patients with COPD were failure to exhale fully and away from the inhaler before inhalation (66% of patients), failure to hold breath for 5–10 s (42%) and failure to inhale slowly and deeply (39%) [19]. Similar errors were identified in a meta-analysis of 12 studies (n = 1288) investigating device use errors with soft mist inhalers: those occurring in more than one in four patients were failure to exhale fully and away from the device before inhalation, failure to hold breath for up to 10 s, and failure to take a slow, deep breath while pressing the dose release button [20]. As such, while suboptimal PIF appears to be the most common inhalation technique error for DPI users, the reverse (‘supra-optimal’ PIF) is common among pMDI and soft mist inhaler users.
Both GOLD and the Global Initiative for Asthma advise checking inhalation technique at every visit and before changing medication [1, 21]. However, inhalation technique is often not assessed when selecting an inhaler device and treatment [12, 16, 17, 22, 23]. If patients are not educated on the correct use of their inhalers, clinical outcomes may be compromised [24, 25]. The CRITIKAL study examined the use of inhalers in patients with asthma to identify errors that impact most negatively on clinical outcomes. It found that insufficient inspiratory effort was common in DPI users (32–38%) and was associated with uncontrolled asthma and increased exacerbation rates [23]. Other factors associated with an increased rate of exacerbations in this study included not sealing the lips around the mouthpiece, the dose being compromised because of shaking or tipping the device, and not removing the cap from the device [23]. In the same study, actuation before inhalation was found to have a significant association with uncontrolled asthma for pMDI users, whereas insufficient inspiratory flow was not, suggesting that problems with coordination are more critical for adequate disease control with pMDIs [23]. Another disadvantage of pMDIs over other classes of inhaler is the environmental impact, with an estimated 20–30 times higher carbon footprint of selected pMDIs versus DPIs [26]. This should be taken into account alongside other factors when choosing an inhaler.
Non-adherence to medication represents another significant barrier to optimal disease management [27]. Non-adherence can be ‘conscious’, and is often due to patient doubts about the necessity of using an inhaler, economic concerns (medication-sparing) or perceived concerns around safety [28, 29]. It can also be ‘unwitting’, such as not following instructions to prepare the dose, inappropriate handling of the inhaler device, not holding one’s breath after inhaling the medication, or incorrect posture (e.g. not tilting the head slightly) [16, 17, 23]. Note that unwitting non-adherence may overlap with inhalation technique errors. Finally, non-adherence may be ‘erratic’, meaning the patient forgets to take their medication [30].
A better understanding of the relationship between PIF, inhalation technique and medication adherence, and their impact on health status will help physicians in selecting the most suitable inhaler device for each patient. Optimising these factors has the potential to improve the effectiveness of maintenance therapy, including long-term disease control and quality of life [31] (Fig. 1). Here, we report the methodology of the PIFotal COPD study, which will investigate the effects of PIF, inhalation technique and medication adherence on patient-reported outcomes in patients with COPD in primary care who are using a DPI for their maintenance therapy. For further information, the study protocol is available on request (version 3; date: 31 July 2020).
Objectives
Primary Objectives
The primary objectives of this cross-sectional observational study are to determine the association of (1) PIF; (2) inhalation technique errors; and (3) medication adherence with health status in COPD patients who receive maintenance therapy (i.e. long-acting bronchodilators either with or without inhaled corticosteroids [ICS]) delivered through a DPI.
Secondary Objectives
Secondary objectives are (1) to determine the association of PIF, inhalation technique errors and medication adherence with history of exacerbations and historical healthcare resource utilisation (HCRU; i.e. relevant consultations of healthcare providers, hospitalisations and clinical parameters); (2) to identify critical inhalation technique errors based on the relationship of these errors with health status and prior exacerbations; (3) to determine the prevalence of suboptimal PIF and different inhalation technique errors (critical and non-critical) for the different inhaler resistance clusters; (4) to examine associations of inhalation technique errors with maximal PIF (against resistance of own inhaler); and (5) to examine associations between patient-specific factors and maximal PIF (against low resistance).
Methods
Study Design
The PIFotal COPD study (registered on 31 August 2020) is a cross-sectional observational study that will be conducted in six countries: the Netherlands, Spain, Portugal, Poland, Greece and Australia. A list of study sites can be found at https://clinicaltrials.gov/ct2/show/study/NCT04532853. Details of the PIFotal study design can be found in Fig. 2.
PIFotal study design. Figure produced by the General Practitioners’ Research Institute. Step 1: clinical examination; Step 2: verification of eligibility; Step 3: written informed consent; Step 4: PIF assessment; Step 5: maximal PIF against the resistance of patient’s own device; Step 6: maximal PIF at low resistance; Step 7: fill in three questionnaires (Clinical COPD Questionnaire, COPD Assessment Test and Test of Adherence to Inhalers); Step 8: inhalation technique will be video-recorded using usual medication; Step 9: patients receive tailored inhalation instructions based on the inhalation errors. PIF peak inspiratory flow
Between October 2020 and May 2021 (first participant enrolled on 21 October 2020), patients were invited to participate in the study through the following sites in both urban and rural areas: general practitioner (GP) practices, community pharmacies, outpatient clinics (both public and private) and patient organisations. Visits at home are also permissible during the COVID pandemic. Overall inclusion and data collection will be overseen by the General Practitioners’ Research Institute (GPRI) and boosted by ‘local champions’ (i.e. colleagues in the professional GPRI network who have agreed to lead the PIFotal study in a specific country). The PIFotal COPD study will be conducted in a manner that is consistent with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria [32]. Selection bias will be avoided by visiting older people who have mobility impairment in their homes and by helping patients who have low literacy to fill out the study questionnaires. All study sites will be trained on how to assist patients in the completion of questionnaires without influencing the results (e.g. reading out the questions with all possible answers, but not interpreting the answers). Furthermore, careful monitoring will be carried out to ensure correct assessment of PIF measures. The video recordings of inhalation technique will be scored by two independent assessors using the checklist of the Netherlands Lung Alliance [33]. In case of disagreement, two assessors will try to reach consensus. If unsuccessful, a third experienced assessor will be invited to reconcile the disagreement.
Sample Size Calculation (Based on Analysis of Primary Outcome)
A power analysis was conducted based on the Clinical COPD Questionnaire (CCQ). Patients with optimal PIF are expected to have a CCQ score that is on average 0.2 points lower (i.e. better health status) (standard deviation = 1, Cohen’s d = 0.2) than patients with suboptimal PIF for their specific device resistance. This difference corresponds to 50% of the minimal clinically important difference for a CCQ of 0.4 points [34]. Furthermore, to take a clustering effect into account (patients from the same GP practice or site may be more alike than those from different GP practices), we estimate the intraclass correlation to be 0.03 (based on data from 1022 COPD and asthma-COPD overlap patients from a data registry of an asthma/COPD outpatient clinic) [35]. Thus, expecting a Cohen’s d of 0.2, taking into account a cluster size of 12 patients per GP practice and a 2:1 ratio of optimal to suboptimal patients, and adopting 5% significance (α) and 80% power (1 – β), a total of 1176 patients need to be included. Hence, a sample size of ~ 1200 patients is deemed a suitable population size.
Patient Population
Two measures will be put in place to promote the real-world nature of the study. First, diagnosis of COPD may be made by a physician without the requirement to conduct additional confirmatory and ancillary testing. Second, only a limited number of inclusion and exclusion criteria will be adopted.
In order to be eligible to participate in the PIFotal COPD study, a patient must meet the following inclusion criteria: (1) a diagnosis of COPD; (2) aged ≥ 40 years; (3) current use of maintenance therapy (i.e. long-acting bronchodilator(s) either with or without inhaled ICS delivered through a DPI) for at least 3 months; and (4) sufficient investigator-assessed decision-making capacity to provide informed consent (e.g. absence of acute psychotic disorders, severe pervasive developmental disorders/severe intellectual disability or advanced neurodegenerative disease).
Exclusion criteria include (1) an exacerbation requiring oral corticosteroids and/or antibiotics in the past 6 weeks; (2) life-threatening disease and life expectancy < 6 months; and (3) current participation in a randomised controlled trial of COPD medication.
To make sure that the results of the study are generalisable, we aim to have representative rates of all DPIs used by the patients. This is likely to be achieved without adopting stratified sampling. However, after inclusion of 800 participants, we will check the distribution of DPI devices with varying resistance. If it is apparent that one specific device is used by more than 50% of the participants (400 participants), patients using this device will no longer be invited to participate in the study.
Main Study Parameters
The PIFotal study will collect data on health status (measured with CCQ and COPD Assessment Test) and number of self-reported COPD exacerbations in the previous 12 months. Since exacerbations may exhibit seasonal effects [36], collecting data for ≤ 12 months prior to the visit reduces the risk of seasonal factors such as weather influencing exacerbation results.
PIF will be assessed using the In-Check DIAL G16 device [37,38,39], a disposable, single-patient mouthpiece with a one-way valve that prevents patients from exhaling into the device. The resistance of the In-Check DIAL G16 will be set to match the resistance of the patient’s own inhaler. If a patient uses multiple inhalers, the assessment priority list of inhalers (Table 1) will outline the inhaler PIF cut-off measurements. The list is calculated based on the prevalence of inhalers in participating countries, prioritising the more common inhalers in order to obtain the most representative and generalisable data. PIF will be assessed in three different ways: (1) PIF for the usual patient inhalation manoeuvre at the resistance of own inhaler; (2) maximal PIF at the resistance of own inhaler (Max PIF [Rx]); and (3) maximal PIF at low resistance (Max PIF [R1]) of the In-Check DIAL device.
For assessment of inhalation technique, patients will inhale their usual medication, and the inhalation procedure will be video-recorded for later assessment of successive inhalation steps by two independent raters, based on standard inhaler technique guidelines [33]. Self-reported medication adherence will be assessed using the 12-item version of the Test of Adherence to Inhalers (TAI-12) [30, 44], which measures ‘unwitting’, ‘erratic’ and ‘conscious’ non-adherence.
HCRU will be assessed over the last 6 months, including primary and secondary care, care provided by other healthcare providers, hospitalisations, laboratory assessments and medication use. HCRU data are usually collected in the 6 months prior to study visit, because these data rely on patient reports, and evidence suggests that recall of patients over periods ≥ 6 months is not reliable [45].
The names (generic and brand), anatomic therapeutic chemical code of the World Health Organization [46], dose, frequency, number of puffs, type of device, duration of device use and other medications prescribed to a patient will be recorded.
Demographic and clinical characteristics, including sex, age, height, weight, COPD duration (years), COPD severity (collected at GP examination or through patient report), smoking behaviour and previous asthma will be recorded.
Assessment of safety is described in the Supplementary Material.
SARS-CoV-2
To prevent contamination and thereby the risk of a viral infection with SARS-CoV-2 for a successive participant, the In-Check DIAL will be cleaned after each use. Furthermore, it is important to note that the In-Check DIAL G16 uses one-way valves and requires an inspiratory manoeuvre that does not produce aerosols through which viruses can spread. However, in the unlikely event of serious adverse events, the sponsor will report these to the accredited ethics committee that approved the study protocol.
The possibility of virtual visits was investigated in a short pilot but was deemed to be unfeasible within the current population. Therefore, no virtual visits will be performed. Visits at home will be identical to those at the GP’s office or pharmacy. As described above, extensive safety measures will be in place to prevent COVID infection, independent of where the visit is performed.
Statistical Analysis
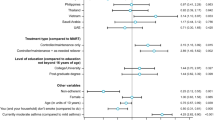
Participants’ clinical and demographic characteristics will be summarised using descriptive statistics. In the primary analysis, the mean difference in CCQ score between (1) patients with optimal/suboptimal PIF, (2) patients who do/do not exhibit inhalation technique errors, and (3) patients who do/do not adhere to medication will be examined in a multivariable linear mixed model. Adjustment will be made for covariates and the possible confounding effect of COPD severity (e.g. effect of device choice on PIF and CCQ score). Secondary objectives will be examined in two multivariable Poisson (or negative binomial) mixed models for quantitative variables. To facilitate a clinical interpretation of the magnitude of associations of PIF, inhalation technique errors and medication adherence with CCQ score, the unstandardised regression coefficients of these independent variables will be compared with those between the CCQ score and the unstandardised regression coefficients of other characteristics (e.g. sex, age, smoking pack-years). Mixed model analysis will be used to account for potential dependence of observations (i.e. patients from the same GP practice or site may be more alike than those from different GP practices or sites, possibly due to the inhalation training provided within the GP practice). Model assumptions (e.g. normality, linearity and homoscedasticity) will be examined. Additionally, the following sensitivity and subgroup analyses will be conducted by repeating the primary analysis to assess (1) COPD Assessment Test as the dependent variable; (2) repeating the main analysis using propensity score matching rather than adjustment for covariates; (3) patients with a PIF below and above the minimal PIF according to the Summary of Product Characteristics of the device that a patient uses; and (4) subgroups excluding patients with a history of asthma, current use of pMDIs, diagnosis of COPD as confirmed through spirometry (COPD severity according to GOLD stages 1–4), prior exacerbations before switching over to a new medication or use of multiple inhalers. Missing data will be imputed using multiple imputation. The imputation model will comprise all variables included in the analyses, and all variables that predicted missingness of a variable or its value. Imputed values will be obtained in three rounds. Parameters and test statistics will be calculated. To control for an undesired inflation of the type I error rate, the alpha value will be adjusted using the false discovery rate [41]. Missing or ambiguous CCQ scores will be calculated using the individual domains where possible.
Scientific Advisory Board
A scientific advisory board has been set up to provide advice on the study protocol, the conduct of the study, data to be collected (including time windows, e.g. which time period to consider for HCRU), statistical analyses and interpretation of the results. All members of the scientific advisory board are distinguished researchers and/or clinicians in the field of respiratory medicine and care for patients with COPD (Supplementary Table 1).
The study sponsor is GPRI, who will undertake data collection and analysis for the study and facilitate and coordinate participation across the study sites. A data governance committee has been set up to decide on the data use for new projects, and consists of the chair of the scientific advisory board (Ioanna Tsiligianni), the principal investigator (Janwillem Kocks) and a representative from the funder (Alberto de la Hoz).
Data Collection and Management
Personal data will be handled confidentially. During the analysis phase, all data will be pseudonymised. All participants will receive a unique study identification number. This number will not be linked to the participant’s personal information (e.g. initials and birth date). Instead, a participant identification code list will be used to link data to a participant, and the key to the code will be safeguarded by the coordinating investigator. Data will be entered into an electronic case report form (eCRF). Castor [47], a data collection software, will be used to ensure the adequate entry, management and storage of the collected data. All inhalation technique videos will be recorded on centrally managed iPads and uploaded directly into Castor. The videos will be removed from the iPad after uploading, and all data on iPads will be encrypted by Castor servers. Only those researchers who are responsible for the assessment of the inhalation technique can decrypt the video files and see the patients’ images. All other researchers who can access the eCRF will not be able to view the video recordings.
Ethics and Dissemination
The PIFotal COPD study will be conducted in accordance with the principles of the Declaration of Helsinki (version October 2013) [48] and in accordance with ethical legislation of all participating countries. The study protocol has received approvals from the following institutional ethics committees/institutional review boards: Australia: Human Research Ethics Committee (HREC 3) University of Sydney; Greece: Research Ethics Committee University of Crete; Poland: Komisja Bioetyczna przy Beskidziej Izble Lekarskiej–Bielsko Biala; Komisji Bioetycznej przy Śląskiej Izbie Lekarskiej; Silesian Medical Society (Śląska Izba Lekarska); Bioethics Committee at Lower Silesian Medical Association; Bioethics Committee at the Medical University of Białystok; Portugal: North Health Regional Administration (ARS Norte); Matosinhos Local Health Unit (ULS Matosinhos); Guimarães Hospital; Center Health Regional Administration (ARS Centro); Regional Health Administration of Lisbon and Tagus Valley (ARS LVT); Spain: Comité de Ética de la Investigación (CEI) Islas Baleares; CEI Hospital Universitario de Gran Canaria; the Netherlands: Medisch Ethische Toetsingscommissie (METC) Assen. Written informed consent will be obtained by the site investigator from all study participants before questionnaire completion, PIF assessment and audio-visual recording of their inhalation technique. Specifically, with regard to the audio-visual recording, participants will be asked for informed consent (1) to share the audio-visual recordings with raters (who will rate the inhalation techniques) and (2) for using the video for medical education purposes. Further information on confidentiality is detailed in the informed consent form (Supplementary Material).
The study findings will be reported in due course at research conferences and in peer-reviewed journals. The study protocol and clinical study data will be made available after publication of the primary manuscript in a peer-reviewed journal. These data will be available upon reasonable request. Further details will be provided in the primary manuscript.
Monitoring and Quality Assurance
The PIFotal COPD study will be conducted in accordance with internationally accepted STROBE quality criteria [32]. Monitoring will be carried out by an independent study monitor contracted by GPRI. All data will be entered in the eCRF by the investigator using the study-specific iPad directly into Castor. Castor has an audit trail that enables the tracking of changes and the application of validation rules. This will minimise errors and missing values on questionnaires. If data are completed on paper (for instance, as a fail-safe system in case of technical issues during a visit), double data entry will be performed afterwards.
End of Study Notification
If required by local regulations, the investigator/sponsor will notify the accredited medical ethical committee of the end of the study within a period of 8 weeks, and will submit a final report with the results of the study, including any publications/abstracts of the study, to the accredited medical ethical committee.
Discussion
The PIFotal COPD study is the first to examine the real-world prevalence and implications of PIF, as well as inhalation technique and medication adherence, on patient behaviour and disease outcomes in patients with COPD who are receiving maintenance treatment with DPIs. The unique design of this study will also enable us to better understand the relationship between demographic and clinical characteristics and PIF.
Following hospitalisation for an acute exacerbation of COPD, patients are commonly discharged on DPIs if they have been using them during their hospital stay, possibly because they require fewer steps to use than pMDIs [7]. However, sufficient inspiratory flow is needed to overcome the internal resistance of a DPI device and ensure delivery of the medication to the lungs [49]. Suboptimal PIF is common among COPD patients at hospital discharge, with female gender being the only factor consistently associated with reduced PIF [6, 38]. However, little is known about the association of suboptimal PIF with clinical and demographic factors, which has contributed to the development of this real-world observational study.
Strengths and Limitations
A major strength of the PIFotal study is that, unlike in previous studies, the assessment of PIF and inhalation manoeuvre will be measured objectively for a given inhaler using the In-Check DIAL device. An additional strength is that it will measure maximal PIF as well as the typical patient inhalation manoeuvre, which will provide insights into the reasons for poor inspiratory effort. This may help to differentiate patients who cannot achieve optimal PIF due to lack of muscle strength or other physiological factors (e.g. hyperinflation) and thus cannot be trained, versus patients who do not achieve optimal PIF but can be trained. Real-time feedback will be used to improve inhaler technique. Studies investigating the benefits of real-time feedback on inhaler technique have demonstrated significant improvements [50,51,52]. Another novel element of this study is the use of a video recording, allowing a thorough assessment of any errors in inhalation technique. The assessment is challenging as the inhalation manoeuvre is performed very quickly (within a few seconds), with almost 20 possible errors that can occur. In previous studies, inhalation technique was not recorded but rated on the spot by a number of different observers, resulting in potentially subjective observations and the possibility of inter-rater variability [23]. The video recordings used in this study will allow the manoeuvre to be replayed by two trained researchers, increasing the inter-rater reliability of the assessment.
The PIFotal study is associated with a number of potential limitations. The first is the focus on DPIs; however, as DPIs are the most commonly prescribed inhaler type for COPD, data from the PIFotal study should be well representative of primary care prescribing patterns and therefore highly generalisable. Furthermore, previously published data indicate that insufficient inspiratory flow is less of a critical inhalation technique error for other inhaler types, such as pMDIs [23]. Even though DPI use is a prerequisite for entry into the PIFotal study, concomitant use of other inhaler types is, in fact, permitted and will be accounted for in the sensitivity analyses. Other potential limitations include the inability to assess causality, owing to the data collection at a single point in time. In addition, questionnaire-based studies are subject to potential recall bias, and there is the potential that patients may alter their inhalation technique in order to conform to expectations while being videoed.
Conclusion
This large multinational observational study will help healthcare professionals to understand the importance of optimal PIF, inhalation technique and medication adherence in DPI users, and the possible clinical consequences in terms of patient-reported outcomes. This will assist primary care physicians with selecting the most appropriate device for each patient, with a resistance that better matches their inhalation ability.
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2021 report). 2020 [cited February 2 2021]. https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf.
Levy ML, Carroll W, Izquierdo Alonso JL, Keller C, Lavorini F, Lehtimäki L. Understanding dry powder inhalers: Key technical and patient preference attributes. Adv Ther. 2019;36(10):2547–57.
Ding B, Small M, Scheffel G, Holmgren U. Maintenance inhaler preference, attribute importance, and satisfaction in prescribing physicians and patients with asthma, COPD, or asthma–COPD overlap syndrome consulting for routine care. Int J Chron Obstruct Pulmon Dis. 2018;13:927–37.
Berkenfeld K, Lamprecht A, McConville JT. Devices for dry powder drug delivery to the lung. AAPS PharmSciTech. 2015;16(3):479–90.
Ghosh S, Ohar JA, Drummond MB. Peak inspiratory flow rate in chronic obstructive pulmonary disease: Implications for dry powder inhalers. J Aerosol Med Pulm Drug Deliv. 2017;30(6):381–7.
Ghosh S, Pleasants RA, Ohar JA, Donohue JF, Drummond MB. Prevalence and factors associated with suboptimal peak inspiratory flow rates in COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:585–95.
Loh CH, Peters SP, Lovings TM, Ohar JA. Suboptimal inspiratory flow rates are associated with chronic obstructive pulmonary disease and all cause readmissions. Ann Am Thorac Soc. 2017;14(8):1305–11.
Laube BL, Janssens HM, de Jongh FH, et al. What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J. 2011;37(6):1308–31.
Mahler DA. Peak inspiratory flow rate as a criterion for dry powder inhaler use in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2017;14(7):1103–7.
Duarte AG, Tung L, Zhang W, Hsu ES, Kuo Y-F, Sharma G. Spirometry measurement of peak inspiratory flow identifies suboptimal use of dry powder inhalers in ambulatory patients with COPD. Chronic Obstr Pulm Dis. 2019;6(3):246–55.
Malmberg LP, Rytila P, Happonen P, Haahtela T. Inspiratory flows through dry powder inhaler in chronic obstructive pulmonary disease: age and gender rather than severity matters. Int J Chron Obstruct Pulmon Dis. 2010;5:257–62.
Chapman KR, Voshaar TH, Virchow JC. Inhaler choice in primary practice. Eur Respir Rev. 2005;14(96):117–22.
Hesso I, Kayyali R, Nabhani-Gebara S. Supporting respiratory patients in primary care: a qualitative insight from independent community pharmacists in London. BMC Health Serv Res. 2019;19(1):5.
Capstick TG, Clifton IJ. Inhaler technique and training in people with chronic obstructive pulmonary disease and asthma. Expert Rev Respir Med. 2012;6(1):91–101.
Sanchis J, Gich I, Pedersen S, Aerosol Drug Management Improvement Team. Systematic review of errors in inhaler use: Has patient technique improved over time? Chest. 2016;150(2):394–406.
Kocks JWH, Chrystyn H, van der Palen J, et al. Systematic review of association between critical errors in inhalation and health outcomes in asthma and COPD. NPJ Prim Care Respir Med. 2018;28(1):43.
Molimard M, Raherison C, Lignot S, et al. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: real-life assessment of 2935 patients. Eur Respir J. 2017;49(2):1601794.
Sulaiman I, Cushen B, Greene G, et al. Objective assessment of adherence to inhalers by patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;195(10):1333–43.
Cho-Reyes S, Celli BR, Dembek C, Yeh K, Navaie M. Inhalation technique errors with metered-dose inhalers among patients with obstructive lung diseases: a systematic review and meta-analysis of US studies. Chronic Obstruct. Pulm. Dis. J. 2019;6(3):267–80.
Navaie M, Dembek C, Cho-Reyes S, Yeh K, Celli BR. Device use errors with soft mist inhalers: a global systematic literature review and meta-analysis. Chron Respir Dis. 2020;17:1479973119901234.
Global Initiative for Asthma. Pocket guide to asthma management and prevention—a pocket guide for health professionals. 2019 [cited 19 Dec 2019]. https://ginasthma.org/wp-content/uploads/2019/04/GINA-2019-main-Pocket-Guide-wms.pdf.
Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19(1):10.
Price DB, Roman-Rodriguez M, McQueen RB, et al. Inhaler errors in the CRITIKAL study: type, frequency, and association with asthma outcomes. J Allergy Clin Immunol Pract. 2017;5(4):1071–81.
Roggeri A, Micheletto C, Roggeri DP. Inhalation errors due to device switch in patients with chronic obstructive pulmonary disease and asthma: critical health and economic issues. Int J Chron Obstruct Pulmon Dis. 2016;11:597–602.
Bosnic-Anticevich SZ, Cvetkovski B, Azzi EA, Srour P, Tan R, Kritikos V. Identifying critical errors: addressing inhaler technique in the context of asthma management. Pulm Ther. 2018;4(1):1–12.
Janson C, Henderson R, Lofdahl M, Hedberg M, Sharma R, Wilkinson AJK. Carbon footprint impact of the choice of inhalers for asthma and COPD. Thorax. 2020;75(1):82–4.
Price D, Keininger DL, Viswanad B, Gasser M, Walda S, Gutzwiller FS. Factors associated with appropriate inhaler use in patients with COPD—lessons from the REAL survey. Int J Chron Obstruct Pulmon Dis. 2018;13:695–702.
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–67.
Duarte-de-Araújo A, Teixeira P, Hespanhol V, Correia-de-Sousa J. COPD: understanding patients’ adherence to inhaled medications. Int J Chron Obstruct Pulmon Dis. 2018;13:2767–73.
Plaza V, Fernández-Rodríguez C, Melero C, et al. Validation of the “Test of the Adherence to Inhalers” (TAI) for asthma and COPD patients. J Aerosol Med Pulm Drug Deliv. 2016;29(2):142–52.
Dudvarski Ilic A, Zugic V, Zvezdin B, et al. Influence of inhaler technique on asthma and COPD control: a multicenter experience. Int J Chron Obstruct Pulmon Dis. 2016;11:2509–17.
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
Lung Alliance Netherlands. Correct use of inhaled medication—Asthma and COPD. 2011 [cited 25 March 2021]. http://longalliantie.nl/files/9613/6752/1352/03a_Goed_gebruik_Inhalatiemedicatie_astma_en_COPD_december_2011_en-GB_28_feb._2012.pdf.
Kocks JW, Tuinenga MG, Uil SM, van den Berg JW, Stahl E, van der Molen T. Health status measurement in COPD: the minimal clinically important difference of the clinical COPD questionnaire. Respir Res. 2006;7(1):62.
Baron AJ, Flokstra-de Blok BMJ, van Heijst E, et al. Prevalence of asthma characteristics in COPD patients in a Dutch well-established asthma/COPD service for primary care. Int J Chron Obstruct Pulmon Dis. 2020;15:1601–11.
Hicks A, Healy E, Sandeman N, Feelisch M, Wilkinson T. A time for everything and everything in its time - exploring the mechanisms underlying seasonality of COPD exacerbations. Int J Chron Obstruct Pulmon Dis. 2018;13:2739–49.
Sanders MJ. Guiding inspiratory flow: development of the In-Check DIAL G16, a tool for improving inhaler technique. Pulm Med. 2017;2017:1495867.
Harb HS, Laz NI, Rabea H, Abdelrahim MEA. Prevalence and predictors of suboptimal peak inspiratory flow rate in COPD patients. Eur J Pharm Sci. 2020;147:105298.
Barnes CN, Mahler DA, Ohar JA, Lombardi DA, Crater GD. Peak inspiratory flows: defining repeatability limits and a predictive equation for different inhalers. Chest. 2020;158(4):1413–9.
Haidl P, Heindl S, Siemon K, Bernacka M, Cloes RM. Inhalation device requirements for patients’ inhalation maneuvers. Respir Med. 2016;118:65–75.
Virchow JC, Weuthen T, Harmer QJ, Jones S. Identifying the features of an easy-to-use and intuitive dry powder inhaler for asthma and chronic obstructive pulmonary disease therapy: results from a 28-day device handling study, and an airflow resistance study. Expert Opin Drug Deliv. 2014;11(12):1849–57.
De Boer AH, Gjaltema D, Hagedoorn P, Frijlink HW. Can ‘extrafine’dry powder aerosols improve lung deposition? Eur J Pharm Biopharm. 2015;96:143–51.
Newhouse MT, Nantel NP, Chambers CB, Pratt B, Parry-Billings M. Clickhaler (a novel dry powder inhaler) provides similar bronchodilation to pressurized metered-dose inhaler, even at low flow rates. Chest. 1999;115(4):952–6.
Chiesi, S.A.U. TAI: Test of Adherence to Inhalers. 2021 [cited March 5 2021]. https://taitest.com/.
Frei A, Siebeling L, Wolters C, et al. The inaccuracy of patient recall for COPD exacerbation rate estimation and its implications: results from central adjudication. Chest. 2016;150(4):860–8.
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2021. 2021 [cited 2 March 2021]. https://www.whocc.no/atc_ddd_index/.
Castor EDC. Home. 2021 [cited March 25 2021]. https://www.castoredc.com/.
World Medical Association. WMA Declaration of Helsinki – ethical principles for medical research involving human subjects. 2013 [cited 2 March 2021]. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
Price DB, Yang S, Ming SWY, et al. Physiological predictors Of peak inspiRatory flow using Observed lung function resultS (POROS): evaluation at discharge among patients hospitalized for a COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2018;13:3937–46.
Chan DS, Callahan CW, Sheets SJ, Moreno CN, Malone FJ. An Internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm. 2003;60(19):1976–81.
Sulaiman I, Greene G, MacHale E, et al. A randomised clinical trial of feedback on inhaler adherence and technique in patients with severe uncontrolled asthma. Eur Respir J. 2018;51(1):1701126.
Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47(3):251–6.
Acknowledgements
The authors thank Evgeni Dvortsin for his valuable contribution in the initial development of the project.
Funding
This study was co-funded by Boehringer Ingelheim and GPRI. The study sponsor is GPRI, who will also be performing the data collection and analysis. Boehringer Ingelheim is the funding and scientific partner, and is funding the journal’s Rapid Service fee.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Olive Denneny, MSc, of MediTech Media and was funded by Boehringer Ingelheim.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
ML, HW, AdlH, AG, SB-A, RD, FL, JM, DP, MRR, IT, OU, BW and JK contributed towards the overall concept and methodology. ML, HW, AG, SB-A, RD, FL, JM, DP, MRR, IT, OU, BW and JK contributed towards the supervision and data curation of the study protocol. JM and JK were involved in software support. HW, AdlH, JM and JK contributed to acquisition of funding and resources for the study. ML and HW conducted the project administration. ML and JK contributed to writing the original draft of the protocol. All authors have contributed towards the development of the manuscript, and have reviewed and approved the final manuscript.
Disclosures
ML is a co-principal investigator for the PIFotal study and has received grants from Boehringer Ingelheim, which is the financial and scientific partner of GPRI for the submitted study, and from AstraZeneca for scientific projects in the area of COPD/asthma. HW has received grants from Boehringer Ingelheim, which is the financial and scientific partner of GPRI for the submitted study, and from AstraZeneca, Novartis and Chiesi for scientific projects in the area of COPD/asthma. AdlH and AG are employees of Boehringer Ingelheim. SB-A has received grants from TEVA, and personal fees from TEVA, Boehringer Ingelheim, AstraZeneca, GSK, Sanofi and Mylan. RD has received grants and personal fees from TEVA, Boehringer Ingelheim, AstraZeneca, GSK, Chiesi, Focus Care and Glenmark. FL has received grants and personal fees from GSK, personal fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Menarini International, Novartis, Orion and Trudell International, outside the submitted work. JM received grants from Boehringer Ingelheim during the conduct of the study and grants from AstraZeneca, Chiesi, Novartis and GSK, outside the submitted work. DP reports grants and personal fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Mylan, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, Theravance and Zentiva (Sanofi Generics); grants from the British Lung Foundation, Respiratory Effectiveness Group, UK National Health Service and AKL Research and Development Ltd; personal fees from Cipla, GlaxoSmithKline, Kyorin, Merck, Mundipharma, Airway Vista Secretariat, EPG Communication Holdings Ltd, FIECON Ltd, Fieldwork International, OM Pharma SA, PeerVoice, Phadia AB, Spirosure Inc, Strategic North Limited, Synapse Research Management Partners S.L., Talos Health Solutions, and WebMD Global LLC; non-financial support from Efficacy and Mechanism Evaluation programme and Health Technology Assessment; stock/stock options from AKL Research and Development Ltd, which produces phytopharmaceuticals; owns 74% of the social enterprise Optimum Patient Care Ltd (Australia and UK) and 92.61% of Observational and Pragmatic Research Institute Pte Ltd (Singapore); and 5% shareholding in Timestamp, which develops adherence monitoring technology. MR-R receives grants and personal fees from AstraZeneca and GSK, and personal fees from Boehringer Ingelheim, Chiesi, Menarini, Mundipharma, Novartis, Pfizer, TEVA and BIAL. IT reports grants and personal fees from GSK, AstraZeneca and Boehringer Ingelheim; grants from Hellas and ELPEN; and personal fees from Novartis, Menarini and MSD. OU reports grants and personal fees from AstraZeneca, Boehringer Ingelheim, Edmond Pharma, Chiesi and GSK; grants from Edmond Pharma; and personal fees from Napp, Mundipharma, Sandoz, Takeda, Cipla, COVIS, Novartis, Mereobiopharma, Orion and Menarini. JK reports grants, personal fees and non-financial support from AstraZeneca, GSK and Boehringer Ingelheim; grants and personal fees from Chiesi Pharmaceuticals and TEVA; grants from Mundipharma; personal fees from MSD and COVIS Pharma; and also holds 72.5% of shares in the General Practitioners Research Institute.
Compliance with Ethics Guidelines
The PIFotal COPD study will be conducted in accordance with the principles of the Declaration of Helsinki (version October 2013) [48] and in accordance with ethical legislation of all participating countries. Written informed consent will be obtained from all study participants. The study protocol has received approvals from the following institutional ethics committees/institutional review boards: Australia: Human Research Ethics Committee (HREC 3) University of Sydney; Greece: Research Ethics Committee University of Crete; Poland: Komisja Bioetyczna przy Beskidziej Izble Lekarskiej–Bielsko Biala; Komisji Bioetycznej przy Śląskiej Izbie Lekarskiej; Silesian Medical Society (Śląska Izba Lekarska); Bioethics Committee at Lower Silesian Medical Association; Bioethics Committee at the Medical University of Białystok; Portugal: North Health Regional Administration (ARS Norte); Matosinhos Local Health Unit (ULS Matosinhos); Guimarães Hospital; Center Health Regional Administration (ARS Centro); Regional Health Administration of Lisbon and Tagus Valley (ARS LVT); Spain: Comité de Ética de la Investigación (CEI) Islas Baleares; CEI Hospital Universitario de Gran Canaria; the Netherlands: Medisch Ethische Toetsingscommissie (METC) Assen. Written informed consent will be obtained by the site investigator from all study participants before questionnaire completion, PIF assessment and audio-visual recording of their inhalation technique. Specifically, with regard to the audio-visual recording, participants will be asked for informed consent (1) to share the audio-visual recordings with raters (who will rate the inhalation techniques) and (2) for using the video for medical education purposes. Further information on confidentiality is detailed in the informed consent form (Supplementary Material).
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Leving, M., Wouters, H., de la Hoz, A. et al. Impact of PIF, Inhalation Technique and Medication Adherence on Health Status and Exacerbations in COPD: Protocol of a Real-World Observational Study (PIFotal COPD Study). Pulm Ther 7, 591–606 (2021). https://doi.org/10.1007/s41030-021-00172-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-021-00172-7