Abstract
Introduction
Chronic cough is a highly problematic symptom for patients with idiopathic pulmonary fibrosis (IPF); limited therapeutic options are available. We evaluated gefapixant, a P2X3 receptor antagonist, for the treatment of chronic cough in IPF.
Methods
This randomized, double-blind, placebo-controlled, crossover study included subjects with IPF. Sequence A included gefapixant 50 mg BID (period 1; 14 days) followed by placebo (period 2; 14 days); sequence B had the opposite sequence of treatments. This regimen was specified in a protocol amendment that modified the original active treatment regimen of gefapixant 50 mg BID for 10 days and 150 mg BID for 4 days. Patients randomized to the original treatment regimen were excluded from efficacy analyses but included in safety assessments. The primary efficacy endpoint was change from baseline in awake cough frequency (coughs/hour) from periods 1 and 2 combined. Adverse events (AEs) were monitored throughout the study.
Results
A total of 51 subjects were randomized, 44 of whom were randomized to treatment sequences evaluated in the primary efficacy analysis (i.e., 22 subjects in sequence A and 22 subjects in sequence B); seven subjects received the treatment assigned before the protocol amendment and were excluded from efficacy analyses. The change from baseline in awake cough frequency from periods 1 and 2 combined (mixed model for repeated measures analysis) did not demonstrate a significant reduction versus placebo in cough at day 14 (p = 0.90); in a post hoc analysis of log-transformed data p value for reduction versus placebo at day 14 was 0.07. The most common AEs were related to taste (dysgeusia and ageusia).
Conclusions
Gefapixant was generally well tolerated but was not associated with a significant improvement in chronic cough in subjects with IPF as defined by the primary endpoint in this study.
Trial Registration
NCT02502097.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Idiopathic pulmonary fibrosis (IPF) is a condition for which adequate treatment is a significant unmet clinical need, and data for treatments from randomized controlled clinical trials for treatment of cough associated with IPF are lacking. |
Gefapixant, a P2X3 receptor antagonist, is an important, novel treatment that has demonstrated efficacy in treatment-refractory chronic cough. |
Based on results from the refractory chronic cough studies, we conducted this study with the hypothesis that gefapixant would reduce cough frequency in patients with IPF. |
What was learned from this study? |
The primary results from this study demonstrated that gefapixant was not associated with a reduction in cough frequency in patients with IPF, although post hoc analyses and secondary endpoints suggest a possible beneficial effect with gefapixant. |
Digital Features
This article is published with digital features, including summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14602344.
Introduction
Idiopathic pulmonary fibrosis (IPF) is a disorder related to dysregulated wound healing and progressive fibrosis [1]. It is clinically characterized by breathlessness, cough, worsening lung function, and impaired survival [2]. For many IPF patients, cough is the first symptom, being reported by more than 70% of patients [3]. A high cough burden has been documented in IPF patients through objective cough measurement, with a median 9.4 coughs/hour (range 1.5–39.4) [4] in one series and 14.8 (IQR 10.9, 16.8) in a second [5]. Higher cough counts have been documented during waking hours than at night [5], and a strong correlation with patient-reported measures of cough has been observed. The burden of cough in IPF patients is much higher than that observed in healthy volunteers or asthma patients, approaching that reported in patients with refractory chronic cough (RCC). Moreover, frequent coughing in IPF patients is superimposed on progressive breathlessness; the interaction between these two symptoms is likely to make the impact and unpleasantness of coughing worse in this patient group. Importantly, in IPF patients, not only does cough significantly impair quality of life, but it has been associated with disease progression [6].
Given the implications of cough for patient quality of life and possible prognosis, there have been several attempts at therapeutic targeting of this refractory symptom [3]. Although available anti-fibrotics have demonstrated amelioration of lung function in controlled trials, they have not exhibited beneficial effects on dyspnea or health status [7,8,9]. An uncontrolled, prospective study suggested improvement in cough using patient report and objective monitoring with pirfenidone therapy [10], but this may have just been due to regression to the mean, as only patients with more severe cough were recruited. Interferon-α has also shown efficacy in IPF cough in a small uncontrolled study [11], but randomized controlled data are rare. A small, placebo-controlled, crossover study demonstrated a benefit of thalidomide on patient-reported cough burden and respiratory quality of life, although a significant burden of adverse effects was reported during thalidomide therapy [12]. A second placebo-controlled crossover study demonstrated reduced objective daytime cough frequency from inhaled cromoglycate in patients with IPF but not RCC, suggesting that mechanisms underlying cough and its susceptibility to treatment in these conditions may differ. Importantly, despite a 31.1% improvement in cough frequency, cromoglycate therapy was not associated with improvements in cough-specific quality of life or reported cough severity in that study [13]; a phase 2b study is currently further assessing the value of this therapy. With scant published research and a lack of licensed treatments for IPF cough, there is a considerable unmet medical need for antitussive treatments in this population.
The pathophysiology of chronic cough in IPF is unclear. However, the chronic cough experienced in IPF has aspects that are similar to those observed with RCC and unexplained chronic cough. Cough in IPF is not clearly related to pulmonary function [4]. Additionally, evidence of increased cough reflex sensitivity in this patient population and reduced cough frequency upon sleep suggest a neurological role in IPF chronic cough [14, 15]. Gefapixant, a P2X3 receptor antagonist, has been studied in patients with treatment-refractory and unexplained chronic cough and has demonstrated efficacy in reducing objective cough counts and improving patient-reported outcomes [16,17,18]. P2X3 receptors are ATP-gated ion channels found on vagal afferent fibers innervating the airways, thought to be important in activating the cough reflex [19, 20]. Two studies have suggested that ATP levels are elevated in the airways of patients with IPF [21, 22], raising the possibility that a similar mechanism drives cough in these patients. We therefore hypothesized that gefapixant would ameliorate cough burden in IPF patients with chronic cough.
Methods
Study Design
This study (Sponsor Protocol 016; NCT02502097) was a randomized, double-blind, placebo-controlled, crossover study of gefapixant in subjects with IPF that was conducted in accordance with principles of good clinical practice at 19 centers with extensive expertise in therapeutic trials of patients with diffuse parenchymal lung disease (Table E1). The study was approved by investigational review boards/ethical review committees, and patients provided informed consent prior to being enrolled in the study (Supplementary Material). This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
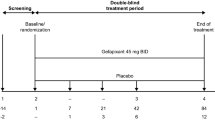
Subjects were screened during a period of up to 14 days followed by two 14-day treatment periods, with a 14–21-day washout period between each treatment period. Randomization was done using a centralized interactive voice response system/interactive web response system (IVRS/IWRS). Subjects and all personnel involved in the conduct and interpretation of the study were blinded to treatment codes; unblinding was done through the IVRS/IWRS. Subjects were assigned randomly in a 1:1 ratio to a treatment sequence (A: 22 subjects) of gefapixant 50 mg BID (one 50 mg tablet) during period 1 followed by placebo BID (one matching tablet) during period 2, or a treatment sequence (B: 22 subjects) of placebo BID during period 1 followed by gefapixant 50 mg BID during period 2. Subjects returned 14 days (± 3 days) after completing the second treatment period for a follow-up visit.
Protocol Amendment and Randomization Error
The study was originally designed to randomize subjects to the following two treatment sequences: placebo BID for 14 days followed by gefapixant 50 mg BID for 10 days and 150 mg BID (three 50 mg tablets) for 4 days (three subjects), or gefapixant 50 mg BID for 10 days and 150 mg BID for 4 days followed by placebo BID for 14 days (four subjects). Data subsequently demonstrated similar pharmacologic effects and improved tolerability with gefapixant 50 mg BID compared with higher doses in patients with RCC [17]. The protocol was therefore amended to randomize subjects to 50 mg BID for the full 14-day active treatment sequences for the rest of the recruitment period; primary analyses were done using this post-amendment subject population. Seven subjects were randomized prior to the amendment and followed the original dosing regimen; data from these subjects are not included in the primary analyses.
Additionally, a programming error in the IWRS system led to eight subjects not being crossed over to the alternate treatment group as planned. The error was identified, and, of the eight subjects, six subjects had already completed the study and the other two subjects were returned to their assigned treatment. The administration of the incorrect dosing in the second period of the crossover study design resulted in an additional 10 days of treatment with gefapixant 50 mg BID or placebo and an additional 4 days of treatment with gefapixant 150 mg BID or placebo. Due to the error, the modified intention-to-treat (mITT) analysis population (population used for primary and secondary efficacy analyses) was redefined to include all randomized subjects who were enrolled into study under the aforementioned protocol amendment, had baseline and at least one post-baseline cough frequency values, and had otherwise complied with the protocol without any other major protocol deviation.
Subjects
This study enrolled male and female subjects aged 40 years or older with a diagnosis of IPF according to guideline-recommended criteria at the time of the trial [23]. Study subjects also experienced self-reported history of troublesome, daily cough for more than 8 weeks, stable cough frequency for at least 4 weeks, and a score of ≥ 40 mm on the cough severity VAS at screening. Cough Severity Diary (CSD) and daily cough scores were collected using the IVRS/IWRS system and reviewed at screening. Subjects were excluded if they were current smokers (within the previous 30 days), had a history of opioid use within 1 week of the baseline visit, had experienced an upper respiratory tract infection or initiation of treatment with an angiotensin-converting enzyme inhibitor within 4 weeks prior to the baseline visit, treatment with an investigational drug or biologic within 30 days of the first dose of study treatment, malignancy within 2 years of screening, cutaneous adverse drug reaction to sulfonamides, or symptoms of renal disease or renal obstructive disease. Full inclusion and exclusion criteria are enumerated in the supplementary material (Table E2).
Efficacy Measurements
Cough monitoring was conducted for 24 h during period 1 and period 2 at baseline (day 0) and at day 7 and day 14 after administration of the study treatment using an ambulatory cough recording device (VitaloJAK™, Vitalograph, UK). The resulting data from the device recording were processed by validated, custom-written software that reduced the length of the file by cutting out the majority of speech and background noise, but retained cough data [24]. Cough sounds were tagged manually at an independent cough monitoring core lab, who provided documentation of the time of each cough event over the 24-h period as well as the time the subject went to asleep and awakened.
The primary efficacy endpoint was change from baseline in awake objective cough frequency (coughs/hour) from periods 1 and 2 combined. Secondary endpoints included the following: change from baseline in awake objective cough frequency from each period separately; change from baseline in 24-h objective cough frequency from periods 1 and 2 combined; change from baseline in 24-h objective cough frequency from each period separately; change from baseline in sleep cough frequency from periods 1 and 2 combined; cough frequency responder endpoints (30% reduction, 50% reduction, and 70% reduction); cough severity visual analog scale (VAS), Cough Quality-of-Life Questionnaire (CQLQ), CSD and daily cough score; University of California, San Diego Shortness of Breath Questionnaire (UCSD SOBQ); and Borg CR10 Scale.
Safety Assessments
Subjects were queried regarding adverse events (AEs) at every visit starting with day 1. All subjects who were randomized and received at least one dose of study treatment were assessed for safety, which included monitoring of AEs, physical examination, vital signs, 12-lead electrocardiogram, and clinical laboratory tests. Additional safety assessments were performed to monitor renal and urological safety, taste-related AEs, and oral paresthesia/hypoesthesia. If the subject reported a taste-related AE, a structured taste questionnaire was administered.
Statistical Methods
A sample size of 42 subjects (21 subjects per treatment sequence) was estimated to provide 80% statistical power for the two-period crossover analysis of variance to be statistically significant at α = 0.05 when the average treatment effect was 50% and the within-subject period standard deviation was 110%. To allow for up to a 15% study attrition rate, a total of 50 subjects (25 per treatment sequence) were to be enrolled.
The primary and secondary analyses of efficacy were conducted on the mITT set, which included subjects who sufficiently complied with the protocol without any other major protocol deviation and had baseline and at least one post-baseline cough frequency value (see aforementioned randomization error details). A mixed model for repeated measures (MMRM) analysis of variance was used to evaluate results in this study and included fixed effects for period, treatment group, visit, and all interaction terms, and the period-specific baseline value as a covariate. The derived percent change in daytime cough frequency measured at each dose was the repeated measure. The primary efficacy analysis was the dose (the repeated measure) by treatment interaction. Model contrasts were constructed to compare the active treatment results to the placebo treatment results for each individual dose. The least-squares (LS) mean change from baseline with associated standard errors for each treatment group and estimated treatment differences along with 90% confidence intervals (CI) and p values were generated.
An exploratory post hoc analysis was used to analyze the primary endpoint on the log10 scale, as cough frequency data tend to be positively skewed and normalize with log transformation. The changes from baseline for log10-transformed variables were analyzed using a mixed effects model, fitting terms for treatment sequence, subject within sequence, treatment, and period. The following baseline covariates were included: average of the log10 baseline measurements for the subject and the period-specific baseline. Summaries of geometric mean of awake cough frequency were generated by treatment and by study visit. The percent difference change between gefapixant and placebo was estimated by 100 (10diff − 1), where diff is the difference provided by the analysis of the log-transformed variable.
For cough frequency responder analyses, comparison of gefapixant and placebo was done using Fisher’s exact test. The analysis methods for other secondary endpoints were consistent with the method for the primary analysis. The post hoc and secondary analyses were not adjusted for multiplicity; p values for secondary endpoints are therefore nominal.
Safety analyses were done on the safety set, which included all randomized subjects who had received at least one dose of study drug. Safety data were summarized by treatment group using frequencies and incidence rates.
Results
Subjects
A total of 51 subjects were randomized into this study: 22 subjects were randomized to receive the placebo to gefapixant sequence, and 22 subjects were randomized to receive the gefapixant to placebo sequence. An additional three subjects were randomized to receive placebo (14 days BID) and then gefapixant 50 mg BID for 10 days followed by 150 mg BID for 4 days; four subjects were randomized to receive gefapixant 50 mg BID for 10 days followed by 150 mg BID for 4 days then placebo (14 days BID) (Fig. 1). Of the 51 randomized subjects, 46 (90.2%) completed the study and five (9.8%) discontinued. All five discontinuations were due to AEs (Fig. 1).
Study design and patient accounting. *Subjects in the mITT analysis included those who had at least one post-baseline cough frequency value and were to have complied with the protocol without major deviation; subjects who completed the study after a protocol amendment that changed dosing from 10 days of gefapixant 50 mg followed by 4 days of 150 mg to 14 days of 50 mg were excluded. Subjects included in the safety analysis were to have received at least one dose of study treatment (subjects completing before the protocol amendment changing the dose of gefapixant are included)
Over 75% of subjects were male and 95% were white. The mean age was 69.6 years. The mean duration of cough was 7 years, mean forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio was 83.6 (± 10.60)%, and 53% of subjects had a prior diagnosis of rhinitis, gastroesophageal reflux disease (GERD), asthma, or postnasal drainage. Baseline characteristics were relatively similar across treatment sequences (Table 1). Despite a screening VAS cough requirement, there was significant variability in baseline VAS and recorded cough frequency (Figure E1).
Efficacy
The change from baseline in awake objective cough frequency from periods 1 and 2 combined (MMRM analysis) did not demonstrate a significant reduction versus placebo in cough at either day 7 or day 14; on day 7, LS mean treatment difference was −2.5 (−10.1, 5.1), p = 0.5096 (a 4.1% difference from placebo) and on day 14, LS mean treatment difference was −0.8 (−13.4, 11.8), p = 0.8983 (a 5.3% difference from placebo) (Table 2; Fig. 2). The exploratory post hoc analysis of log-transformed awake cough frequency for periods 1 and 2 combined showed that the percent change adjusted by placebo was −9.52% (95% CI: −28.86%, 15.07%) (nominal p = 0.41) on day 7 and −24.61% (95% CI: −44.55%, 2.50%) (nominal p = 0.07) on day 14 for periods 1 and 2 combined (Table 2; Fig. 2).
Responder analyses demonstrated that gefapixant 50 mg had a greater response rate of ≥ 30% reduction compared with placebo on day 7 and day 14 for periods 1 and 2 combined. On day 7, 52.8% of subjects on gefapixant versus 29.7% of subjects on placebo had a 30% reduction (nominal p = 0.06), and on day 14, 50% of subjects on gefapixant versus 26.3% of subjects on placebo had a 30% reduction (nominal p = 0.06). The response rates for ≥ 50% and ≥ 70% reduction were greater for gefapixant than for placebo (Fig. 3). A post hoc analysis suggested that the proportion of patients experiencing a > 30% reduction in awake cough frequency was greater in patients with greater baseline cough burden as defined by ≥ 50 coughs/hour (Figure E2) or VAS ≥ 40 (Figure E3).
Secondary endpoints demonstrated that scores for cough severity VAS (Figure E4A), CSD total score, daily cough scores, Borg CR10, CQLQ (Figure E4B), and UCSD SOBQ scores were all numerically higher (i.e., worse) for the placebo group than for the gefapixant group, although nominal p values were < 0.05 for only the daily CSD endpoint (Table 3).
Safety
A majority of subjects reported at least one AE while on gefapixant, and approximately half of subjects reported at least one AE while on placebo. The most common AEs were taste-related (dysgeusia, ageusia, and hypogeusia) (Table 4). There were four subjects who discontinued treatment due to an AE (two subjects on placebo and two subjects on gefapixant); one subject discontinued during the washout period after period 1 placebo treatment (Table 4). Subjects reported the following AEs leading to discontinuations: on placebo, sinusitis and pneumonia, and on gefapixant 50 mg, dizziness, fatigue, dysphonia, myalgia, productive cough, oral paresthesia, decreased oxygen saturation, and lower respiratory tract infection (some individual patients who discontinued reported multiple AEs).
A total of seven subjects reported a serious AE (8.5% in the gefapixant group and 6.7% in the placebo group). There were two deaths: one subject following gefapixant (a terminal IPF patient who reported respiratory failure considered possibly related to study drug 11 days after the last dose of gefapixant 50 mg during period 2) and one subject following placebo (due to pneumonia considered unrelated to study drug reported 3 days after ending placebo treatment in period 2 and 24 days after the last dose of gefapixant 50 mg during period 1).
Discussion
This study represents the first time that P2X3 antagonism has been tested as a treatment to decrease cough burden in IPF patients with chronic cough. Our findings demonstrate that there was no statistical significance between the P2X3 receptor antagonist, gefapixant, and placebo in the primary endpoint of awake cough frequency. Importantly, several methodological/procedural issues occurred in this study that may have confounded our ability to draw definitive conclusions on the effect of P2X3 antagonism in this patient population. Of note, given the skewed nature of the cough frequency data, log transformation is commonly used in cough studies; a post hoc analysis using log-transformed data showed greater numerical improvement in cough frequency with gefapixant versus placebo. A responder analysis also suggested that improvements in cough frequency and a response to gefapixant compared with placebo were more evident in IPF patients with greater cough burden. All patient-reported outcomes were numerically lower (better or less severe) for gefapixant compared with placebo, although only the CSD showed statistically significant improvement. The safety profile of gefapixant was similar to that reported in prior work in patients with RCC [16]. Thus, although the primary endpoint did not show statistically significant improvement with gefapixant versus placebo, several endpoints/analyses hint at a possible treatment effect that will be informative in the design of future research.
In this study, gefapixant 50 mg BID did not achieve the pre-specified primary endpoint of demonstrating a significant reduction in awake cough frequency versus placebo over 2 weeks of treatment in patients with IPF; this contrasts with studies of gefapixant in patients with RCC, where robust effects have been observed [16,17,18]. There are several potential explanations for this finding. Firstly, our study highlights the importance of considering the variability of cough frequency between patients. Both awake and 24-h cough frequency endpoints generally exhibit a positively skewed distribution, which can be normalized for analysis by log transformation. The analysis of log-transformed data, therefore, has greater statistical power for detecting potential treatment effects compared with the analysis of the raw data. Thus, the planned analysis of the primary endpoint of awake cough frequency in this study was not optimal for demonstrating efficacy. Indeed, the post hoc analysis of the log-transformed data provides some evidence of a treatment effect, a 25% reduction in cough frequency over placebo with a nominal p value close to statistical significance (p = 0.07). We also note that a higher proportion of gefapixant patients achieved at least 30% reduction in cough frequency in this study. Reductions in cough frequency of 20–30% are considered clinically meaningful in RCC [25]. Together with the significant improvement in the CSD and numerical improvements in the majority of patient-reported outcomes, these data are consistent with effects of potential clinical relevance in IPF. However, this study was underpowered to adequately assess the benefit of gefapixant versus placebo using patient-reported outcomes. Only the cough-specific quality-of-life questionnaire suggested no effect of gefapixant. Although some evidence supports the validity of the CQLQ in IPF patients [26], such questionnaires were developed in patients with RCC and may not capture or be responsive to the impacts of coughing most important to patients with IPF.
Despite the possible antitussive effect of gefapixant in IPF suggested by our data, this was clearly not as marked or robust as the effects seem in patients with RCC [16,17,18]. This may reflect differences in the biological mechanisms of cough in different disease populations, with ATP/P2X3 interactions important for cough only in a subgroup of IPF patients. Recent data support significant heterogeneity of chronic cough with likely different endotypes [27,28,29]. This notion is also supported by differing therapeutic responses to inhaled sodium cromoglycate seen in a recent study comparing IPF patients with RCC [13]. Another consideration is that the effective doses of gefapixant in RCC might be insufficient to treat cough in IPF. Much higher doses of gefapixant (up to 600 mg BID) were evaluated in the initial RCC studies and are known to be safe although they resulted in all patients experiencing a taste-related AE [17, 18]. It is unknown whether differences in the biological mechanisms underpinning cough in IPF might necessitate higher doses of P2X3 antagonism to achieve more substantial improvements in cough.
Importantly, the safety profile of gefapixant in this patient group was similar to that previously reported. Urological and renal AEs were infrequent and similar between placebo and active treatment, although there was a numerically higher incidence on gefapixant. Urological or renal AEs have not been observed in previous studies of gefapixant in patients with RCC or unexplained chronic cough [16,17,18, 20]. Despite a patient population with severe lung disease, the overall incidence of serious AEs was similar between active therapy and placebo. One death was deemed possibly related to study medication by the investigator, although respiratory failure and pneumonia are known complications of the underlying lung disease [2, 30]. Although AE monitoring did not reveal any specific safety concerns, tolerability was affected by gefapixant, with taste-related AEs and oral paresthesia/hypoesthesia comparable to that seen in previous studies at this dose level [16].
In addition to issues noted above, this study was also limited by its relatively small sample size, a protocol amendment where the dose regimen was altered (leading to exclusion of some patients who completed the original dose regimen from the primary mITT analysis population), and a randomization error resulting in eight subjects not receiving crossover medication as planned (leading to additional exclusions from the mITT population). Additionally, the study of cough treatments for IPF patients is complicated by multiple comorbidities that are not well understood with regard to their association with chronic cough and likely not optimally accounted for in this exploratory study. These limitations did not have an impact on the interpretation of safety data in this trial. Although some subjects received more study medication than originally planned due to the randomization error, previous studies have evaluated higher dosing regimens, and safety of subjects was not compromised; these patients were retained in the analysis of safety data.
Conclusion
In summary, this study demonstrates that gefapixant did not meet the pre-specified primary objective of reduction in awake cough frequency in patients with IPF complicated by cough. Gefapixant was well tolerated, with the most commonly reported AEs to be related to taste effects known to be associated with this therapy. Although they must be interpreted with caution, post hoc analyses and secondary endpoints suggest a potential therapeutic effect and the need for further research in patient populations that may be particularly amenable to therapeutic treatment of cough complicating IPF.
References
Martinez FJ, Collard HR, Pardo A, Raghu G, Richeldi L, Selman M, Swigris JJ, Taniguchi H, Wells AU. Idiopathic pulmonary fibrosis. Nat Rev Dis Primers. 2017;3:17074.
Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med. 2018;378:1811–23.
Vigeland CL, Hughes AH, Horton MR. Etiology and treatment of cough in idiopathic pulmonary fibrosis. Respir Med. 2017;123:98–104.
Key AL, Holt K, Hamilton A, Smith JA, Earis JE. Objective cough frequency in idiopathic pulmonary fibrosis. Cough. 2010;6:4.
Schertel A, Funke-Chambour M, Geiser T, Brill AK. Novel insights in cough and breathing patterns of patients with idiopathic pulmonary fibrosis performing repeated 24-hour-respiratory polygraphies. Respir Res. 2017;18:190.
Ryerson CJ, Abbritti M, Ley B, Elicker BM, Jones KD, Collard HR. Cough predicts prognosis in idiopathic pulmonary fibrosis. Respirology. 2011;16:969–75.
Noble PW, Albera C, Bradford WZ, Costabel U, du Bois RM, Fagan EA, Fishman RS, Glaspole I, Glassberg MK, Lancaster L, et al. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Eur Respir J. 2016;47:243–53.
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, Cottin V, Flaherty KR, Hansell DM, Inoue Y, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2071–82.
King TE Jr, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, Gorina E, Hopkins PM, Kardatzke D, Lancaster L, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2083–92.
van Manen MJG, Birring SS, Vancheri C, Vindigni V, Renzoni E, Russell AM, Wapenaar M, Cottin V, Wijsenbeek MS. Effect of pirfenidone on cough in patients with idiopathic pulmonary fibrosis. Eur Respir J. 2017;2017:50.
Lutherer LO, Nugent KM, Schoettle BW, Cummins MJ, Raj R, Birring SS, Jumper CA. Low-dose oral interferon α possibly retards the progression of idiopathic pulmonary fibrosis and alleviates associated cough in some patients. Thorax. 2011;66:446–7.
Horton MR, Santopietro V, Mathew L, Horton KM, Polito AJ, Liu MC, Danoff SK, Lechtzin N. Thalidomide for the treatment of cough in idiopathic pulmonary fibrosis: a randomized trial. Ann Intern Med. 2012;157:398–406.
Birring SS, Wijsenbeek MS, Agrawal S, van den Berg JWK, Stone H, Maher TM, Tutuncu A, Morice AH. A novel formulation of inhaled sodium cromoglicate (PA101) in idiopathic pulmonary fibrosis and chronic cough: a randomised, double-blind, proof-of-concept, phase 2 trial. Lancet Respir Med. 2017;5:806–15.
Doherty MJ, Mister R, Pearson MG, Calverley PM. Capsaicin induced cough in cryptogenic fibrosing alveolitis. Thorax. 2000;55:1028–32.
Hope-Gill BD, Hilldrup S, Davies C, Newton RP, Harrison NK. A study of the cough reflex in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2003;168:995–1002.
Smith JAKMM, Morice AH, Birring SS, McGarvey LP, Sher MR, Li YP, Wu WC, Xu ZJ, Muccino DR, Ford AP. Gefapixant, a P2X3 receptor antagonist, for the treatment of refractory or unexplained chronic cough in a phase 2b randomised controlled trial. Lancet Resp Med 2020;8:775–785.
Smith JAKMM, Butera P, Smith SA, Li YP, Xu ZJ, Holt K, Sen S, Sher MR, Ford AP. Gefapixant in two randomized dose-escalation studies in chronic cough. Eur Respir J 2020; 55:1901615.
Abdulqawi R, Dockry R, Holt K, Layton G, McCarthy BG, Ford AP, Smith JA. P2X3 receptor antagonist (AF-219) in refractory chronic cough: a randomised, double-blind, placebo-controlled phase 2 study. Lancet. 2015;385:1198–205.
Kwong K, Kollarik M, Nassenstein C, Ru F, Undem BJ. P2X2 receptors differentiate placodal vs. neural crest C-fiber phenotypes innervating guinea pig lungs and esophagus. Am J Physiol Lung Cell Mol Physiol 2008;295:L858–865.
Morice AH, Kitt MM, Ford AP, Tershakovec AM, Wu WC, Brindle K, Thompson R, Thackray-Nocera S, Wright C. The effect of gefapixant, a P2X3 antagonist, on cough reflex sensitivity: a randomised placebo-controlled study. Eur Respir J 2019;2019:54.
Muller T, Fay S, Vieira RP, Karmouty-Quintana H, Cicko S, Ayata K, Zissel G, Goldmann T, Lungarella G, Ferrari D, et al. The purinergic receptor subtype P2Y2 mediates chemotaxis of neutrophils and fibroblasts in fibrotic lung disease. Oncotarget. 2017;8:35962–72.
Riteau N, Gasse P, Fauconnier L, Gombault A, Couegnat M, Fick L, Kanellopoulos J, Quesniaux VF, Marchand-Adam S, Crestani B, et al. Extracellular ATP is a danger signal activating P2X7 receptor in lung inflammation and fibrosis. Am J Respir Crit Care Med. 2010;182:774–83.
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
McGuinness K, Kelsall A, Lowe J, Woodcock A, Smith J. Automated cough detection: a novel approach [abstract]. Am J Respir Crit Care Med. 2007;175:A381.
Nguyen AM, Muccino D, Birring S, Bacci ED, Vernon MK, Mines D, Smith JA. Defining minimal clinically important differences (MCID) in chronic cough: analyses of objective cough counts from a phase 2 randomized controlled trial. J Allergy Clin Immunol 2019;143:AB169.
Lechtzin N, Hilliard ME, Horton MR. Validation of the Cough Quality-of-Life Questionnaire in patients with idiopathic pulmonary fibrosis. Chest. 2013;143:1745–9.
Belvisi MG, Birrell MA, Khalid S, Wortley MA, Dockry R, Coote J, Holt K, Dubuis E, Kelsall A, Maher SA, et al. Neurophenotypes in airway diseases. insights from translational cough studies. Am J Respir Crit Care Med 2016;193:1364–72.
Long L, Yao H, Tian J, Luo W, Yu X, Yi F, Chen Q, Xie J, Zhong N, Chung KF, Lai K. Heterogeneity of cough hypersensitivity mediated by TRPV1 and TRPA1 in patients with chronic refractory cough. Respir Res. 2019;20:112.
Mazzone SB, Chung KF, McGarvey L. The heterogeneity of chronic cough: a case for endotypes of cough hypersensitivity. Lancet Respir Med. 2018;6:636–46.
Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med. 2018;379:797–8.
Acknowledgements
The authors thank the investigators and the participants of this trial.
The Chronic Cough in IPF Study Group included the following investigators Iftikhar Hussain; Mandel Sher; Selwyn Spangenthal; Faisal Fakih; Mark Gotfried; Kevin Flaherty; Lisa Lancaster; Maureen Horton; Robert Kaner; Kapil Patel; Mary Beth Scholand ; Robert Sussman; Ganesh Raghu; Imre Noth; Michael Denenberg; Shahzad Ahmad; Neil Ettinger; Vivek Iyer; Murali Ramaswamy.
Funding
This study was funded by Afferent Pharmaceuticals, which was acquired by Merck & Co., Inc., Kenilworth, NJ, USA. Jaclyn A. Smith is additionally funded by the NIHR Manchester Biomedical Research Centre, a Wellcome Investigator Award and is an NIHR Senior Investigator. Journal fees have been funded by Merck Sharp & Dohme, a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA .
Medical Writing and/or Editorial Assistance
Medical writing support was provided by Anish Mehta (Merck & Co., Inc., Kenilworth, NJ, USA) and additional publication and editorial support was provided by Jennifer Pawlowski (Merck & Co., Inc, Kenilworth, NJ, USA). This support was funded by Merck Sharp & Dohme, a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
FJM: Conception/design/planning of the study, acquisition of data, analysis of data, interpretation of results, drafting the manuscript, and critical review/revision of the manuscript. ASA: Interpretation of results, acquisition of data, and critical review/revision of the manuscript. JAS: Analysis of data, interpretation of results, drafting the manuscript, and critical review/revision of the manuscript. MK: Conception/design/planning of the study, acquisition of data, analysis of data, interpretation of results, and critical review/revision of the manuscript. AF: Conception/design/planning of the study, acquisition of data, interpretation of results, and critical review/revision of the manuscript. JJL: Analysis of data, interpretation of results, and critical review/revision of the manuscript. YL: Analysis of data, interpretation of results, and critical review/revision of the manuscript.
Prior Presentation
This study was presented at the American Thoracic Society 2019 International Conference, May 17-22, 2019 in Dallas, TX, USA (Martinez FJ, Afzal A, Kitt MM, Ford A, Li JJ, Li YP, Smith J. The Treatment of Chronic Cough in Idiopathic Pulmonary Fibrosis Patients with Gefapixant, a P2x3 Receptor Antagonist. Am J Resp Crit Care Med 2019;199:A2638).
Disclosures
Fernando J. Martinez discloses fees from Abbvie, Boehringer Ingelheim, Bristol Myers Squibb, Csl Behring, DevPro, Genentech, IQVIA, Sanofi, Shionogi, and Veracyte. He has been a participant in ILD trials sponsored by Afferent/MSD, Bayer, Biogen, National Heart, Lung and Blood Institute, Patara/Respivant, ProMedior/Roche, and Veracyte. Amna Sadaf Afzal is an employee of Merck & Co., Inc., Kenilworth, NJ, USA and reports receiving a salary and stock. Jaclyn A. Smith has received grants and personal fees from Afferent Pharmaceuticals/Merck & Co., Inc., Kenilworth, NJ (related to submitted work) as well as grants and personal fees from Ario Pharma, GlaxoSmithKline, NeRRe Pharmaceuticals, Menlo, and Bayer; personal fees from Boehringer Ingelheim, Genentech, and NeoMed; nonfinancial support from Vitalograph; and personal fees from Cheisi. Additionally, JAS is a named inventor on a patent describing detection of cough from sound recordings. The patent is owned by University Hospital of South Manchester and licensed to Vitalograph Ltd. MMK was an employee of Afferent Pharmaceuticals/Merck & Co., Inc., Kenilworth, NJ. Anthony P. Ford was the founder of Afferent Pharmaceuticals and a former employee of Merck & Co., Inc., Kenilworth, NJ. APF subsequently co-founded and is currently employed by CuraSen Therapeutics. Jerry Jing Li is an employee of Merck & Co., Inc., Kenilworth, NJ, USA and reports receiving a salary and stock. Yuping Li received personal fees from Afferent Pharmaceuticals/Merck & Co., Inc., Kenilworth, NJ. MMK was an employee of Afferent Pharmaceuticals/Merck & Co., Inc., Kenilworth, NJ. MMK is currently an employee of Axalbion SA.
Compliance with Ethics Guidelines
The study was approved by Investigational Review Boards/Ethical Review Committees and patient provided informed consent prior to being enrolled in the study (Appendix). This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA’s data sharing policy, including restrictions, is available at http://engagezone.msd.com/ds_documentation.php. Requests for access to the clinical study data can be submitted through the EngageZone site or via email to dataaccess@merck.com.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The members of the Chronic Cough in IPF Study Group are processed under the acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Martinez, F.J., Afzal, A.S., Smith, J.A. et al. Treatment of Persistent Cough in Subjects with Idiopathic Pulmonary Fibrosis (IPF) with Gefapixant, a P2X3 Antagonist, in a Randomized, Placebo-Controlled Clinical Trial. Pulm Ther 7, 471–486 (2021). https://doi.org/10.1007/s41030-021-00162-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-021-00162-9