Abstract
Background
Japanese employers are obligated to offer employees annual health checkups and guidance programs for their health promotion and maintenance to prevent cardiovascular (CV) and lifestyle-related diseases. Under these programs, checkup recipients are notified of the checkup results, and in case of abnormal findings, employers are expected to provide employees with follow-up encouragement to change their behavior; for example, with medical consultations or lifestyle modifications. However, the effect of these programs on behavioral changes and their subsequent clinical outcomes has not been clearly assessed.
Objective
The aim of this study was to investigate changes in CV risk management behaviors after receiving unfavorable health checkup results on serum lipid levels among subjects without antidyslipidemic drug prescription and uncontrolled lipid levels and at elevated risk of CV events in a real-world setting.
Patients and Methods
This retrospective cohort study used a Japanese employment-based health insurance database managed by MinaCare Co., Ltd. This study analyzed the data from the annual health checkups of recipients aged 20–74 years with data on their low-density lipoprotein-cholesterol (LDL-c), high-density lipoprotein-cholesterol (HDL-c), and triglyceride (TG) values from 2015 to 2017, who had uncontrolled lipid levels based on their checkup results at baseline in 2015, and without prescription records of antidyslipidemic drugs. Lipid status was considered uncontrolled if any of the following were detected: LDL-c ≥ 140 mg/dL, HDL-c < 40 mg/dL, or TG ≥ 150 mg/dL. Changes in antidyslipidemic drug prescription, as a primary CV risk management behavior measure, and in lipid control status in 2016 and 2017 were investigated. Potential factors associated with lipid control were also explored using logistic regression analysis.
Results
Among 154,421 subjects without antidyslipidemic drug prescription and with uncontrolled lipid levels in 2015, 93.6% remained without antidyslipidemic drug prescription in both 2016 and 2017. Of these subjects, 76.8% and 76.4% continued having uncontrolled lipid levels in 2016 and 2017, respectively. Fewer subjects without prescription achieved lipid control than those with prescription. Various factors were associated with lipid control, with high LDL-c as the greatest risk factor for uncontrolled lipid levels.
Conclusions
These results suggest that most health checkup recipients may not have changed their behaviors; that is, they may have not sought medical treatment and continued having uncontrolled lipid levels in the years following the unfavorable health checkup results. To encourage subjects to initiate desirable behavioral changes, more practical support may be essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Of the health checkup recipients who were not prescribed antidyslipidemic drugs and had uncontrolled lipid levels as reported in previous health checkup results in 2015, non-prescription status did not change in 96.3% in 2016 and in 97.1% in 2017 and uncontrolled lipid status did not change from 2015 to 2017 in > 75%. |
These results suggest the importance of pharmacological treatment in lipid control and that more approaches are essential to encourage desirable behavioral changes for maintaining and promoting workers’ health and eventually for cardiovascular disease prevention in Japan. |
Lipid parameter values as well as body mass index and smoking status in 2015 were found to be associated with uncontrolled lipid status in 2016, suggesting the importance of cardiovascular event prevention through comprehensive approaches including pharmacological treatment for dyslipidemia and modifying cardiovascular-related lifestyle behaviors. |
1 Introduction
Once considered as diseases in high-income countries, non-communicable diseases (NCDs) have become a universal health concern [1]. NCDs accounted for 73.4% of deaths globally in 2017, and cardiovascular diseases (CVDs) were primary contributors to NCD deaths [2]. CVDs are the leading causes of mortality worldwide [2] and in Japan [3], and the global death toll due to CVDs has been increasing in recent years [4]. With the devastating impact of NCDs, including CVDs, on patients and society [5, 6], it is necessary to reduce the burden of NCDs by preventing and controlling CVDs as well as other NCDs for global health and sustainable development [7].
Dyslipidemia is a globally common condition. Along with other metabolic factors including hypertension and obesity, and lifestyle-related factors including smoking, dyslipidemia is a risk factor for atherosclerosis, which is a major underlying pathogenesis of CVDs [8]. Elevated serum lipid levels are associated with an increased risk of cardiovascular (CV) events [9,10,11,12]. Meanwhile, CVDs are largely preventable and treatable by modifying risk factors. Lowering lipid levels, especially low-density lipoprotein-cholesterol (LDL-c) levels, can contribute to CV risk reduction [13, 14]. Lipid monitoring and control play a pivotal role in CVD prevention [15, 16].
However, lipid parameters are often not well controlled in real-world settings. A previous study using health checkup data extracted from the Japanese employment-based health insurance database demonstrated a trend of suboptimal lipid control in Japan [17]. Similar results were reported in two national databases of the Specific Health Checkups and Specific Health Guidance (MHLW-SH) issued in 2010 [18] and the National Health and Nutrition Survey (MHLW-H&N) issued in 2015 [19].
Japanese corporate employers are obligated to offer their employees and their dependents annual regular health checkups and guidance programs to enable them to be aware of their own health conditions and to promote and maintain their health to prevent CVD and lifestyle-related diseases. Additionally, a new statutory health checkup program commenced in 2008 with the aim of specifically preventing metabolic syndrome in insured individuals and dependents aged ≥ 40 years. As a part of these programs, employers are stipulated to notify their employees of the health checkup results and adopt follow-up measures, including encouragement for medical consultation and/or lifestyle modifications in case of abnormal findings. It is expected that health checkup recipients who were notified of their elevated CV risk and received follow-up encouragement would positively change their behaviors; for example, seek treatment from healthcare professionals and/or quit smoking and focus on body mass index (BMI) management. These changes would reduce the risk of CVD, and eventually, NCDs. However, the effect of these programs on behavioral changes and subsequent clinical outcomes has not been clearly assessed.
Therefore, the objective of this study was to investigate the changes in CV risk management behaviors after receiving unfavorable health checkup results on serum lipids among subjects without antidyslipidemic drug prescription and uncontrolled lipid levels who can be at an elevated risk of CV events in a real-world setting. Additionally, we exploratorily investigated the potential factors associated with lipid control to gain an insight into the improvement of lipid control in Japan.
2 Methods
2.1 Study Design
This was a retrospective cohort study using a Japanese healthcare database managed by MinaCare Co., Ltd (Tokyo, Japan).
2.2 Data Source
The MinaCare database is an employment-based health insurance database that includes periodically updated health checkup data and medical/pharmaceutical claims data of the employees and their dependent family members since 2010. The MinaCare database covers a wide range of age groups up to 74 years of employees that work in large-scale nationwide retailers and manufacturers, and those in food, information, transportation, and energy industries. Individuals aged ≥ 75 years are not included in this database because they are included in a different insurance program. The database contains approximately 6.1 million individuals’ data with medical and pharmaceutical claims and approximately 2.3 million individuals’ data with health checkups (as of February 2020).
During a health checkup, a recipient undergoes physical examination, including body weight measurement, blood pressure, and blood tests as well as physicians’ examinations. In addition, at the time of the checkup, individuals must complete a questionnaire about their lifestyle, such as smoking. Health checkup data include data on individuals’ demographics, smoking status, and various examination results and self-reported lifestyle habits.
2.3 Ethics Statement
This study involves data that exist in an anonymized structured format and contains no personal information. Therefore, obtaining informed consent from subjects and approval for this study from the ethical review committee was not required because studies using only un-linkable anonymized data are outside the scope of the “Ethical Guidelines for Medical and Health Research Involving Human Subjects” set by the Japanese government. The study was conducted in accordance with legal and regulatory requirements (e.g., privacy protection laws) as well as with scientific purpose, value, and rigor. MinaCare manages such anonymized data under the data transfer contract with client health insurers.
2.4 Data Extraction and Management
Health checkup data between 2015 and 2017 (the latest available 3-year period at the time of planning) and prescription claims data between 2014 and 2017 were extracted from the MinaCare dataset based on Japan’s fiscal year of April through March. Health checkups are usually conducted annually; in case of multiple records in any given year, the first record was used to render three records for each subject corresponding to 2015, 2016, and 2017.
From the checkup data, we used data on lipid parameter values as well as demographic and clinical characteristics, including self-reported smoking status.
2.5 Study Population
Subjects were included if they (1) were aged 20–74 years at the time of their health checkup in the baseline year (2015); (2) had health checkup data on LDL-c, high-density lipoprotein-cholesterol (HDL-c), and triglyceride (TG) values for 3 consecutive years from 2015 to 2017 in the MinaCare database; and (3) did not have prescription records of antidyslipidemic drugs and had uncontrolled lipid levels based on checkup results at baseline. Antidyslipidemic drugs and lipid control status are defined in detail in Sect. 2.6.
2.6 Outcome Measures and Definitions
The primary outcome measures were antidyslipidemic drug prescription and lipid control status in the subsequent year in 2016. CV risk management behavior was primarily measured using antidyslipidemic drug prescriptions.
Antidyslipidemic drugs were defined by the prescription record of the drugs listed in Supplementary Table 1 (see electronic supplementary material [ESM]), within 6 months prior to the health checkup. There was a 99.5% agreement between antidyslipidemic drug prescriptions within 6 months and 12 months prior to the health checkup. Thus, antidyslipidemic drug prescription within 6 months prior to the health checkup was consistently used in the analyses.
Lipid control status was classified as controlled or uncontrolled, based on the diagnostic criteria used for dyslipidemia screening [16, 20]. An uncontrolled lipid status was defined as the presence of any one of the following: LDL-c ≥ 140 mg/dL, HDL-c < 40 mg/dL, or TG ≥ 150 mg/dL; and a controlled lipid status as LDL-c < 140 mg/dL, HDL-c ≥ 40 mg/dL, and TG < 150 mg/dL [16, 20].
To supplement the assessment of changes in CV risk management behaviors after the health checkup and guidance program at baseline, data on self-modifiable CV risk management behaviors (i.e., BMI and smoking status) collected at health checkups in the following year (2016) were assessed as secondary outcome measures. BMI was based on the data obtained during the health checkup examination. Smoking status was based on the recipient’s response to the question about their current smoking habit (yes or no) in a questionnaire administered during the checkup; ex-smokers or those who never smoked were considered non-smokers.
In addition to BMI and self-reported smoking status, demographic and clinical characteristics, such as sex, age, antihypertensive and diabetes mellitus (DM) drug prescription, and metabolic syndrome were assessed as potential factors associated with lipid control. The same 6-month period as for antidyslipidemic drugs was applied to antihypertensive and DM drug prescriptions. Metabolic syndrome was defined as waist circumference ≥ 85 cm (males) or ≥ 90 cm (females) and the presence of at least two of the following: (1) antihypertensive drug prescription and/or systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg; (2) antidyslipidemic drug prescription and/or TG ≥ 150 mg/dL and/or HDL-c < 40 mg/dL; and (3) DM drug prescription and/or fasting blood glucose ≥ 110 mg/dL [21].
As a baseline characteristic, the cutoff level for blood pressure (BP) and hypertension stages was based on the Japanese Society of Hypertension Guidelines for the Management of Hypertension in 2014 that were in place at the time of baseline health checkups [22].
2.7 Statistical Analysis
Demographic and clinical characteristics and primary and secondary outcome measures were descriptively summarized. To investigate changes in CV risk management behavior after receiving unfavorable health checkup results, the main focus of this study was to describe changes in the primary outcomes from the study baseline (2015) to the following year (2016). To further analyze the changes in these primary outcomes, we followed up and summarized the changes in primary outcomes for another year to 2017. We calculated the proportion of subjects with and without antidyslipidemic drug prescription in 2016 and 2017 based on the prescription status in the previous year. By the prescription status each year, the proportion of subjects with controlled and uncontrolled lipid status in 2016 and 2017 was calculated. Lipid control in 2016 was also summarized, considering the effects of sex, age, baseline lipid measures, and antidyslipidemic drug prescription in 2016. Mean values, changes from the baseline, and the proportion of subjects achieving the target values for each lipid parameter were also summarized.
As for secondary outcome measures, the BMI status in 2016 of the subjects with baseline BMI ≥ 25 kg/m2 and self-reported smoking status in 2016 of ≥ 40-year-old smokers at baseline were descriptively summarized. The analyses for BMI excluded missing values, which were rare (< 0.1%). For smoking, the analysis was restricted to individuals aged ≥ 40 years because many responses were missing for those aged < 40 years.
A multivariate logistic regression analysis was performed to explore the association of potential factors with the outcome variable of an uncontrolled lipid status in 2016. The following baseline explanatory variables from 2015 were included in the analysis: sex, age category, lipid parameter values, obesity status (BMI < 25/≥ 25 kg/m2), smoking status (yes/no/missing or not reported), antihypertensive drug prescription (yes/no), DM drug prescription (yes/no), and metabolic syndrome status (yes/no). The cutoff point for obesity was BMI ≥ 25 kg/m2 [22]. The analysis was conducted separately for those with and without antidyslipidemic drug prescription in 2016 and excluded subjects with missing BMI values. For each factor, the odds ratio (OR) and 95% confidence interval (CI) were calculated.
No formal hypothesis testing was used owing to the exploratory nature of the study. The 95% CI for OR that excluded 1 was sometimes referred to as ‘statistically significant’.
SAS version 9.4 and R 3.5.0 were used for statistical analysis.
3 Results
3.1 Subject Flow and Baseline Characteristics
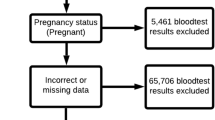
Figure 1 shows the flow of the subjects in this study. A total of 154,421 subjects had no prescription record of antidyslipidemic drugs and had an uncontrolled lipid status at baseline (2015); thus, they were considered as the study population.
Table 1 summarizes the demographic and clinical characteristics of the subjects at baseline. Of the subjects included, 31.2% were females and 68.8% were males. The most common age group was 50–59 years and 40–49 years for female and male subjects, respectively. Of the three lipid parameters, based on which lipid control status was defined, the LDL-c target was not achieved by the largest proportion of both female and male subjects (85.8% and 64.0%, respectively), followed by TG (25.1% and 53.2%, respectively) and HDL-c (3.9% and 16.5%, respectively).
3.2 Change in Antidyslipidemic Drug Prescription Status
Among those included, 96.3% (148,783/154,421) in 2016 and 97.1% (144,516/148,783) in 2017 continued without the prescription (Fig. 2). Even when the prescription was started in 2016, 27.1% (1,527/5,638) of the subjects were no longer prescribed antidyslipidemic drugs in 2017. Overall, the prescription status did not change from ‘no’ for most subjects from 2015 to 2017 (93.6% [144,516/154,421]). The prescription proportion in 2016 increased with age; from 0.9% in < 30-year-olds to 9.5% in ≥ 70-year-olds (Supplementary Figure 1, see ESM).
3.3 Changes in Lipid Control Status
In line with the unchanged prescription status, most subjects had an uncontrolled lipid status in 2016 (118,037/154,421 [76.4%]) and 2017 (115,925/154,421 [75.1%]). Fig. 3 summarizes the lipid control status in 2016 and 2017 by the antidyslipidemic drug prescription status each year. Fewer subjects without prescription achieved lipid control than those with prescription. Among those who had no prescription in 2016 and 2017 as the most common prescription pattern, 76.8% and 76.4% did not achieve lipid control, respectively (Fig. 3b). In contrast, when the prescription continued for 2 years (2016 and 2017), approximately 50% had an uncontrolled lipid status each year.
Lipid control status by antidyslipidemic drug prescription in 2016 and 2017. Prescription records made within 6 months prior to the health checkup are included. Proportion of subjects who did and did not achieve a lipid control status by antidyslipidemic drug prescription pattern in 2016: a no or yes; b from 2016 to 2017: no/no (remained without prescription), no/yes (started prescription in 2017), yes/no (started in 2016 but discontinued prescription in 2017), and yes/yes (continued prescription)
As observed in the whole study population, a smaller proportion of subjects achieved lipid control without antidyslipidemic drug prescription than those with the prescription, regardless of sex and age, but only in the subgroups with LDL-c ≥ 140 mg/dL (Fig. 4a), HDL-c ≥ 40 mg/dL (Fig. 4b), and TG < 150 mg/dL at baseline (Fig. 4c).
Lipid control status by sex, lipid parameter values at baseline (2015), and age at baseline (x-axis). Proportion of lipid control achievers (blue) and non-achievers (red) in subgroups stratified by multiple factors (i.e., age, sex, antidyslipidemic drug prescription in 2016, and three lipid parameter targets (a LDL-c < 140 or ≥ 140 mg/dL, b HDL-c < 40 or ≥ 40 mg/dL, c TG < 150 or ≥ 150 mg/dL). HDL-c high-density lipoprotein-cholesterol, LDL-c low-density lipoprotein-cholesterol, TG triglyceride
Supplementary Table 2 (see ESM) shows the change in each lipid parameter value and the proportion of each target achieved by antidyslipidemic drug prescription from 2015 to 2017. Based on the mean LDL-c values and proportion of the target achievers, LDL-c was better controlled in subjects with antidyslipidemic drug prescription than in those without, particularly in the first year of the prescription, yielding a reduction of approximately 40 mg/dL. TG was decreased more in those with a prescription than in those without. In contrast, HDL-c control did not change greatly over the years, regardless of prescription patterns.
3.4 Factors Associated with an Uncontrolled Lipid Status in the Subsequent Year
A logistic regression analysis was performed to explore the factors associated with an uncontrolled lipid status in 2016 with 2015 as the baseline year (Fig. 5).
Factors associated with uncontrolled lipid status in 2016. Odds ratios for the status of “uncontrolled lipid status in 2016” as an outcome variable were calculated using a multivariate logistic regression model. The following variables at baseline (2015) were included as explanatory variables: sex; age; LDL-c, HDL-c, and TG levels; obesity status; smoking status; antihypertensive drug prescription within 6 months; DM drug prescription within 6 months; and metabolic syndrome. The analysis was conducted separately for a those without antidyslipidemic drug prescriptions in 2016 and b those with antidyslipidemic drug prescriptions in 2016, where drug prescription status in 2016 was based on claims prescription records within 6 months prior to the health checkup in 2016. Subjects with missing BMI values were excluded. BMI body mass index, CL confidence limit, DM diabetes mellitus, HDL-c high-density lipoprotein-cholesterol, LDL-c low-density lipoprotein-cholesterol, MS/NR missing or no response, TG triglyceride
Most of the baseline factors were found to be either positively (more likely to have) or negatively (less likely to have) associated with uncontrolled lipid status in 2016. LDL-c ≥ 140 mg/dL in 2015 was positively associated with uncontrolled lipid status in 2016 for those who were not prescribed antidyslipidemic drugs in 2016 (OR 5.784 [95% CI 5.523–6.056]) (Fig. 5a) and negatively associated with uncontrolled lipid status in 2016 for those who were prescribed antidyslipidemic drugs in 2016 (OR 0.755 [95% CI 0.627–0.909]) (Fig. 5b). Abnormal values for the other lipid parameters, HDL-c < 40 mg/dL and TG ≥ 150 mg/dL, as well as the other self-modifiable factors, BMI ≥ 25.0 kg/m2 and smoking status in 2015, remained risk factors for uncontrolled lipid status in 2016, regardless of whether the subjects were prescribed antidyslipidemic drugs in 2016 or not.
Of the factors found to be positively associated with an uncontrolled lipid status in the logistic regression analysis, we further explored the lipid control status by self-modifiable factors, BMI, and self-reported smoking status at baseline (Table 2). Regardless of antidyslipidemic drug prescriptions, more non-obese than obese (lipid control without/with prescription: 25.9%/51.8% and 17.5%/37.5%, respectively) and more non-smokers than smokers (lipid controlled without/with prescription: 23.4%/50.0% and 20.7%/34.6%, respectively) achieved lipid control.
3.5 Changes in BMI and Smoking Status
We additionally explored changes in CV risk management behaviors in terms of the secondary outcome measures of BMI and smoking status in 2016. Consistent with the primary outcome measure of antidyslipidemic drug prescription, in most subjects, BMI and smoking status did not change from baseline. Of a subset of obese subjects (BMI ≥ 25.0 kg/m2) at baseline, 91.0% continued to be categorized as obese in 2016, and 94.2% of ≥ 40-year-old self-reported smokers at baseline continued smoking in 2016.
4 Discussion
Although subjects had not been prescribed antidyslipidemic drugs and had health checkup results indicating an uncontrolled lipid status in the baseline year (2015), most subjects remained untreated with antidyslipidemic drugs, and more than 75% continued to have uncontrolled lipid levels in 2016 and 2017 in this study.
Theoretically, all residents in Japan are covered by public medical insurance and have the freedom to receive treatment at any of the healthcare institutions, generally with a small out-of-pocket expense. Even under this condition, our results describe a ‘real-world’ situation wherein approximately 95% of subjects were not prescribed antidyslipidemic drugs, despite checkup results suggesting dyslipidemia. Furthermore, our analysis revealed a gap between accumulated evidence of antidyslipidemic medication benefits and the reality of controlling lipid parameters. A meta-analysis of 27 randomized controlled trials of statin treatment reported that lowering LDL-c by approximately 1 mmol/L (~ 39 mg/dL) yielded a 21% reduction in major vascular events, irrespective of baseline risks of major vascular events [14]. In the present study, in subjects who started antidyslipidemic drugs in 2016 and 2017, LDL-c was reduced by approximately 40 mg/dL in the same year. However, 27.1% of the patients discontinued the treatment in 2017. Overall, most subjects did not receive antidyslipidemic drug prescriptions, and more than three quarters of subjects without the prescription failed to achieve lipid control, as substantiated in the poor lipid control status in previous studies [17,18,19]. Although nearly half of the subjects prescribed antidyslipidemic drugs for 2 years remained with an uncontrolled lipid status, our analysis, coupled with previous findings, may underscore the importance of pharmacological treatment for lipid control.
Difficulty in changing the checkup recipient’s behavior was also supported by the lack of change in secondary measures (BMI and smoking status) as in previous studies. Another report on blood pressure control, utilizing the same MinaCare database, showed a substantial proportion, albeit smaller than dyslipidemia, of subjects who did not receive proper treatment despite the checkup results indicating hypertension ([23], in press). In another Japanese statutory health checkup targeting metabolic syndrome, recipients with an increase in visceral fat with one or more additional risks are recommended to participate in the subsequent health guidance program to support behavioral modification. A database study of this checkup program revealed that most recipients eligible did not attend these programs, despite the results and recommendations calling for change [24, 25]. One possible scenario for the lack of change in antidyslipidemic drug prescription status in the present study population is that even though the subjects sought treatment, some physicians may have prioritized lifestyle improvement over medication according to therapeutic guidelines for dyslipidemia [16], particularly for subjects who had uncontrolled HDL-c levels. However, this may have been the case for only a certain proportion of subjects, considering that only about 12.5% of the subjects had abnormal findings in HDL-c levels alone or with the other parameters at baseline, and thus might not affect the overall trend of the drug prescription status observed in this study. The absence of subjective symptoms, particularly in the earlier stages of dyslipidemia, may also serve as a barrier to initiate behavioral changes. This may be particularly the case for younger checkup recipients, marked with a smaller antidyslipidemic drug prescription proportion. Moreover, considering the lower awareness of dyslipidemia (compared with hypertension) suggested in a previous study in Japan [26] and in comparison with the aforementioned report on BP [23], the fact that lipid parameter values are measured only on blood examinations, in contrast to the wide availability of BP self-monitoring devices, may also contribute to forming a barrier.
Although the barriers to behavioral change among subjects who received unfavorable health checkup results are still unclear, warranting further studies, our results suggest that additional approaches are required to encourage the recipients to change their behavior. Employers are required to strive to provide employees who have abnormal findings during checkups with health instructions and recommendations for secondary examinations. In reality, however, more than 30% of employers did not encourage their employees to undergo a secondary work-up or provide health instructions, according to the national survey [27]. Theoretically, all Japanese employees and their dependents undergo regular health checkups annually. Therefore, maximizing this opportunity with a more intensive approach, including education and regular reminders, may elicit behavioral change and ultimately prevent CVD and other NCDs at a population level.
Our results suggest the importance of pharmacological LDL-c management in lipid control. Among the various factors found to be associated with uncontrolled lipid status using logistic regression, high LDL-c (LDL-c ≥ 140 mg/dL) was the greatest risk, increasing the odds of lipid control failure without antidyslipidemic drug prescription by five-fold. Meanwhile, in subjects who started antidyslipidemic drugs, LDL-c levels ≥ 140 mg/dL decreased the odds of lipid control failure. In contrast, abnormal TG and HDL-c levels remained as risk factors for uncontrolled lipid status regardless of the presence or absence of antidyslipidemic drug prescription. Moreover, when the lipid control status was stratified based on the target achievement of each lipid parameter as well as sex and age, more subjects with antidyslipidemic drug prescription achieved lipid control than those without the prescription, regardless of sex and age, but only in the subgroups with LDL-c ≥ 140 mg/dL, HDL ≥ 40 mg/dL, or TG < 150 mg/dL. Based on the definition of lipid control as abnormal values in at least one of the lipid parameters (LDL-c, HDL-c, and TG), all three subgroups (LDL-c ≥ 140 mg/dL, HDL ≥ 40 mg/dL, and TG < 150 mg/dL) commonly included subjects with LDL-c ≥ 140 mg/dL at baseline. It is inferred that more patients who had elevated LDL-c levels may have achieved lipid control with antidyslipidemic drug prescription than those without, and this may not always be applicable to those who had normal LDL-c but abnormal HDL-c and/or TG values. These results may reflect the actual situation in which most subjects with dyslipidemia had abnormal LDL-c levels (70.8% at baseline), while smaller proportions had abnormal HDL-c or TG levels (12.5% and 44.5%, respectively, at baseline). In addition, considering the predominance of LDL-c-lowering agents in antidyslipidemic drugs marketed in Japan, many subjects are considered to have received pharmacological treatment targeted at lowering LDL-c levels and regaining lipid control, leading to an apparent negative association between uncontrolled lipid levels and baseline LDL-c ≥ 140 mg/dL. However, those with normal LDL-c but abnormal HDL-c or TG values may not benefit from LDL-c-lowering agents or, for some reason, antidyslipidemic drugs prescribed to improve HDL-c or TG levels may have failed to exert the expected effects.
Nevertheless, the results also suggest the importance of comprehensive lipid management that encompasses other risks of lipid control failure, that is, BMI ≥ 25.0 kg/m2 and smoking status, albeit with relatively small OR, as well as HDL-c < 40 mg/dL and TG ≥ 150 mg/dL. The Japan Atherosclerosis Society guidelines recommend lifestyle modification first for those without a history of coronary artery disease, and in cases where lifestyle management only cannot control the lipid status, pharmacological treatment and lifestyle management are recommended [16]. However, in most subjects with obesity and a smoking habit at baseline, these states did not change the next year, suggesting that they did not engage in necessary lifestyle modifications. Recently, total cholesterol levels have been reported to be surging in Japan, possibly as a consequence of the westernization of lifestyles [28]. Furthermore, amid the demographic shift to a highly aging population, which is associated with more CV events, CVD, and the ensuing burden, over 30% of the Japanese population is projected to be over 65 years in 2025 [29]. For the aging population to live healthy and independent lives, there is an imminent need for comprehensive CVD prevention and management as well as boosting the motivation for behavioral alteration from the bottom up, starting with the younger generations.
This study has several limitations. First, the database was limited to Japanese employees and their dependents covered by employment-based insurance and therefore may not fully represent the entire population in Japan. The database includes a relatively small proportion of elderly people over 70 years and excludes workers of specific sectors (e.g., self-employment) that were not covered by the employment-based insurance. However, the proportion of checkup recipients in these populations are smaller than working generations (25–64 years) and corporate employees [30], all of whom are supposed to receive compulsory checkups under the obligation imposed on their employers. However, with a large sample size and relatively wide age distribution, the database is considered to reflect the individuals insured by employment-based health insurance. Indeed, a previous study using the MinaCare database reported data consistent with two national data reports [17]. This may rationalize the use of this database for the present study. Second, the definition of antidyslipidemic drugs included all antidyslipidemic drugs, not classified by the indication for each parameter. That is, LDL-c-lowering agents and TG-lowering agents were both defined as ‘antidyslipidemic drugs’ (Supplementary Table 1, see ESM). Finally, the nature of the database study was such that antidyslipidemic drug prescriptions were the main means of the subjects’ behavioral changes for CV management as well as BMI and smoking status. Checkup recipients who consulted health care professionals and were instructed and engaged in lifestyle modification without drug prescription were not explicitly captured in the data, although most included subjects failed to achieve lipid control without the prescription. Prospective cohort studies would allow a wider range of methods/outcomes to assess subjects’ ‘behaviors’ more directly. These limitations should be noted upon interpretation. Nevertheless, prescription data allowed us to accurately capture the pharmacological dyslipidemia management in Japan, as it was not dependent on self-report data, which is more prone to recall bias. Furthermore, to the best of our knowledge, this study is important to gain insight into the effectiveness of health checkup and guidance programs on CV risk management behaviors in workers in Japan, the main supporters of the economy and super-aging society, and may warrant further studies on this issue.
5 Conclusion
Our results suggest that most health checkup recipients with unfavorable serum lipid results without antidyslipidemic drug treatment may not have sought medical treatment and continued to have uncontrolled lipid levels in the following years. Difficulty in behavioral change after health checkup and guidance programs are also suggested by the results showing other self-modifiable CV risk factors such as BMI and smoking status, which were unchanged in approximately 90% of obese subjects and smokers. To avoid leaving the recipients untreated and unsupported and to encourage them to initiate desirable behavioral changes, more practical support may be essential to maintain and promote workers’ health and eventually for CVD prevention in Japan.
References
World Health Organization. Global status report on noncommunicable diseases 2010. 2011. https://www.who.int/nmh/publications/ncd_report2010/en/. Accessed 13 May 2020.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Lond Engl. 2018;392:1736–88 ([published correction appears in Lancet. 2019 Jun 22;393(10190):e44] [published correction appears in Lancet. 2018 Nov 17;392(10160):2170]).
Ministry of Health, Labour and Welfare. Report of vital statistics in 2018. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/geppo/nengai18/dl/gaikyou30.pdf. Accessed 13 Dec 2019.
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25.
Nomura S, Sakamoto H, Glenn S, Tsugawa Y, Abe SK, Rahman MM, et al. Population health and regional variations of disease burden in Japan, 1990–2015: a systematic subnational analysis for the Global Burden of Disease Study 2015. Lancet Lond Engl. 2017;390:1521–38 (published correction appears in Lancet. 2017 Sep 23;390(10101):1488).
Muka T, Imo D, Jaspers L, Colpani V, Chaker L, van der Lee SJ, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015;30:251–77.
World Health Organization. Global action plan for the prevention and control of NCDs 2013–2020. https://www.who.int/nmh/events/ncd_action_plan/en/. Accessed 13 May 2020.
Mendis S, Puska P, Norrving B, World Health Organization. Global atlas on cardiovascular disease prevention and control. Geneva: World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/44701/9789241564373_eng.pdf?sequence=1&isAllowed=y. Accessed 8 July 2019.
Tanabe N, Iso H, Okada K, Nakamura Y, Harada A, Ohashi Y, et al. Serum total and non-high-density lipoprotein cholesterol and the risk prediction of cardiovascular events - the JALS-ECC. Circ J. 2010;74:1346–56.
Imano H, Noda H, Kitamura A, Sato S, Kiyama M, Sankai T, et al. Low-density lipoprotein cholesterol and risk of coronary heart disease among Japanese men and women: the Circulatory Risk in Communities Study (CIRCS). Prev Med. 2011;52:381–6.
Langsted A, Freiberg JJ, Nordestgaard BG. Fasting and nonfasting lipid levels: influence of normal food intake on lipids, lipoproteins, apolipoproteins, and cardiovascular risk prediction. Circulation. 2008;118:2047–56.
Benfante R, Yano K, Hwang LJ, Curb JD, Kagan A, Ross W. Elevated serum cholesterol is a risk factor for both coronary heart disease and thromboembolic stroke in Hawaiian Japanese men. Implications of shared risk. Stroke. 1994;25:814–20.
Cholesterol Treatment Trialists’ (CTT) Collaboration, Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet Lond Engl. 2010;376:1670–81.
Cholesterol Treatment Trialists’ (CTT) Collaborators, Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet Lond Engl. 2012;380:581–90.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–143. ([published correction appears Circulation. 2019 Jun 18;139(25):e1182-e1186]).
Japan Atherosclerosis Society. Dyslipidemia medical treatment guide 2018 (Shishitsuijosho shinryo gaido) in Japanese. 1st ed. Tokyo: Japan Atherosclerosis Society; 2018 (in Japanese).
Shima D, Ii Y, Yamamoto Y, Nagayasu S, Ikeda Y, Fujimoto Y. A retrospective, cross-sectional study of real-world values of cardiovascular risk factors using a healthcare database in Japan. BMC Cardiovasc Disord. 2014;14:120.
Ministry of Health, Labour and Welfare. Data source of the specific health checkups and specific health guidance. http://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/info02a-2.html. Accessed 11 June (in Japanese).
Ministry of Health, Labour and Welfare. Data source of the National Health and Nutrition Survey. http://www.mhlw.go.jp/bunya/kenkou/kenkou_eiyou_chousa.html. Accessed 11 June 2019 (in Japanese).
Japan Atherosclerosis Society. Essence for dyslipidemia treatment for preventing atherosclerotic diseases. http://dl.med.or.jp/dl-med/jma/region/dyslipi/ess_dyslipi2014.pdf. Accessed 8 July 2019 (in Japanese).
Teramoto T, Sasaki J, Ueshima H, Egusa G, Kinoshita M, Shimamoto K, et al. Metabolic syndrome. J Atheroscler Thromb. 2008;15:1–5.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–392.
Higa S, et al. Relationship of annual health checkups with the subject’s subsequent behavior of cardiovascular risk management in a real-world setting in Japan: a retrospective cohort study on changes in antihypertensive drug prescription and blood pressure from 2015 to 2017. Drugs - Real World Outcomes. 2021. https://doi.org/10.1007/s40801-020-00224-5
Nakao YM, Miyamoto Y, Ueshima K, Nakao K, Nakai M, Nishimura K, et al. Effectiveness of nationwide screening and lifestyle intervention for abdominal obesity and cardiometabolic risks in Japan: The metabolic syndrome and comprehensive lifestyle intervention study on nationwide database in Japan (MetS ACTION-J study). PLoS ONE. 2018;13:e0190862.
Tsushita K, Hosler SA, Miura K, Ito Y, Fukuda T, Kitamura A, et al. Rationale and descriptive analysis of specific health guidance: the Nationwide Lifestyle Intervention Program Targeting Metabolic Syndrome in Japan. J Atheroscler Thromb. 2018;25:308–22.
Tanaka T, Okamura T, Yamagata Z, Takebayashi T, Tamura U, Kusaka Y, et al. Awareness and treatment of hypertension and hypercholesterolemia in Japanese workers: the High-risk and Population Strategy for Occupational Health Promotion (HIPOP-OHP) study. Hypertens Res Off J Jpn Soc Hypertens. 2007;30:921–8.
Ministry of Health, Labour and Welfare. Survey on state of employees’ health. https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450095&tstat=000001020508&cycle=0&tclass1=000001064060&tclass2=000001064061. Accessed 13 May 2020.
Kitamura A, Sato S, Kiyama M, Imano H, Iso H, Okada T, et al. Trends in the incidence of coronary heart disease and stroke and their risk factors in Japan, 1964 to 2003: the Akita-Osaka study. J Am Coll Cardiol. 2008;52:71–9.
Cabinet Office Japan. Annual Report on the Ageing Society [Summary] FY. 2019. https://www8.cao.go.jp/kourei/english/annualreport/2019/pdf/2019.pdf. Accessed 25 Dec 2019.
Ministry of Health, Labour and Welfare. Status of medical checkups. https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa07/3-8.html. Accessed 1 June 2020.
Acknowledgements
Medical writing support was provided by Emiko Sato at Clinical Study Support, Inc. (Nagoya, Japan) and funded by Pfizer Japan Inc.
Author information
Authors and Affiliations
Contributions
KN, SH, and YI were involved in the development of the protocol. YY developed the database and YI analyzed the data. All authors contributed to conceptualizing and designing the study, interpreting the results, and drafting and revising the manuscript. All authors approved the final manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Funding
This research was sponsored and funded by Pfizer Japan Inc.
Conflict of interest
KN, SH, and YA are full-time employees of Pfizer Japan Inc., and hold Pfizer stock. YI is a full-time employee of Pfizer R&D Japan and holds Pfizer stock. YY has no conflicts of interest to declare.
Ethics approval and consent to participate
This study involved data that exist in an anonymized structured format and contained no personal information. Studies exclusively using unlinkable anonymized data are outside the scope of the “Ethical Guidelines for Medical and Health Research Involving Human Subjects” by the Japanese government. Therefore, obtaining informed consent and approval from the ethical review committee was not required for this study.
Consent for publication
Not applicable.
Code availability
Not applicable.
Availability of data and material
The data that support the findings of this study are available from the database maintained by MinaCare Co., Ltd. (Tokyo, Japan), independent of Pfizer Japan Inc. Pfizer Japan Inc. is not involved in validating or storing the data included in the database. Restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from MinaCare Co., Ltd.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nozawa, K., Higa, S., Ii, Y. et al. Antidyslipidemic Drug Prescriptions and Lipid Control Status After Unfavorable Annual Health Checkup Results: A Retrospective Cohort Study Using a Health Insurance Database. Drugs - Real World Outcomes 8, 227–240 (2021). https://doi.org/10.1007/s40801-021-00231-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-021-00231-0