Abstract
Background
In Japan, workers receive a health checkup annually, and based on the results, a follow-up health guidance or intervention is provided when deemed necessary. However, it remains unclear whether the current real-world health checkup and guidance programs in Japan successfully lead to behavioral changes or improvement of clinical outcomes in individuals who require cardiovascular (CV) risk management.
Objective
This study aimed to explore the association between health checkup and the subsequent behavior change in CV risk management in subjects with uncontrolled blood pressure (BP) without antihypertensive drug prescription, who can have increased risk of CV events.
Patients and Methods
This was a retrospective cohort study that used health-checkup and claims data from a Japanese healthcare database managed by MinaCare Co., Ltd. Of those aged 20–74 years with available data on systolic and diastolic BP from 2015 to 2017, data from individuals with uncontrolled BP who were not prescribed antihypertensive drugs within 6 months before their baseline health checkup in 2015 were extracted and analyzed. The primary outcome measures were changes in antihypertensive drug prescription and BP control status based on health-checkup results from the baseline year (2015) to 2017. CV risk-management behavior was also assessed using body mass index (BMI) and smoking status, as these are the major modifiable CV risk factors.
Results
Among 39,242 subjects with uncontrolled BP without antihypertensive drug prescription at baseline, 88.9% remained without prescription in 2016. Of the subjects without prescription, 62.9% continued to have uncontrolled BP. Both statuses of the major modifiable CV risk factors remained unchanged in 2016: 92.1% of obese subjects (BMI ≥ 25 kg/m2) at baseline remained obese, and 93.8% of smokers at baseline aged ≥ 40 years continued to smoke. Logistic regression analysis revealed that age 60–69 years (vs. 40–49 years), hypertension (HT) stage II (vs. stage I), HT stage III (vs. stage I), and BMI ≥ 25.0 kg/m2 (vs. < 25.0 kg/m2) were factors associated with uncontrolled BP in 2016 (subsequent year), regardless of antihypertensive drug prescription.
Conclusions
Untreated HT for years increases the risk of CV events. These results suggest that current health-checkup and guidance programs are inadequately effective for behavioral change. Further practices for committing to lifestyle modifications and seeking medical advice based on their health-checkup results need to be undertaken to improve health behavior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A substantial number of Japanese employees and their dependents who had had uncontrolled BP and had not received antihypertensive drug prescription in 2015 continued not to receive a prescription and to have uncontrolled BP in 2016 and 2017. |
A BMI ≥ 25.0 kg/m2 was associated with uncontrolled BP in the subsequent year, irrespective of antihypertensive drug prescription status, highlighting the importance of lifestyle modification such as BMI management. |
Our study findings suggest that current health-checkup and guidance programs may leave individuals untreated and be inadequately effective for behavioral change. |
1 Introduction
Globally, hypertension (HT) is a common pathological condition and considered the leading cause of premature death [1, 2]. Furthermore, high blood pressure (BP) has been reported as a major risk factor of adult mortality from noncommunicable diseases (NCDs) and injuries in Japan [3]. The reason is that HT is a major factor associated with cardiovascular disease (CVD) and cerebrovascular disease [4,5,6], which are the second and fourth causes of death, respectively, in Japan [7]. With the growing super-aging society and increasing healthcare expenses in Japan, the NCD burden on the socioeconomic system arising from CVD is a topical issue [8, 9]. Although the prevention of CVD requires comprehensive management of primary clinical conditions, such as HT, hyperlipidemia, diabetes mellitus (DM), and metabolic syndrome, monitoring and control of HT is the foundation of CVD prevention.
Blood pressure is often not well controlled in real-world settings. In a previous study using health-checkup data extracted from the Japanese employment-based health-insurance database, a substantial proportion of subjects failed to achieve target BP and lipid parameters recommended by the Japanese Society of Hypertension Guidelines for the Management of Hypertension and the Japan Atherosclerosis Society Guidelines for the Management of Hyperlipidemia (e.g., proportion of subjects with systolic BP (SBP) ≥ 140 mmHg was 19.0%/12.2% (males/females) in the 55- to 59-year age group) [10]. Similar results were obtained from two national databases of the Specific Health Checkups and Specific Health Guidance (MHLW-SH) issued in 2010 [11] and the National Health and Nutrition Survey (MHLW-H&N) issued in 2011 [12]. Other previous studies also reported low achievement rates for treatment goals of BP in patients with DM (30.5%) and chronic kidney disease (33.4%) [13] and a lower BP control rate in Japan than in other high-income countries, such as Canada, Germany, South Korea, and the USA [14].
Major statutory health-checkup and guidance programs for Japanese workers are designed to prevent CVD and lifestyle disease by promoting the implementation of health behaviors through health monitoring. In Japan, it is well recognized that merely providing the checkup results to individuals is insufficient to cause behavioral changes. These programs mandate that the companies offer not only health checkups but also follow-ups (e.g., they encourage medical consultation attendance or provide health guidance) for their employees with checkup results indicative of a requirement of such help. Additionally, a new statutory national program, Specific Health Checkups and Specific Health Guidance, was commenced in 2008 with the aim of preventing metabolic syndrome. In this program, medical insurers provide an annual health checkup to insured individuals and their dependents aged ≥ 40 years, and based on the results, specific health guidance for lifestyle modifications is provided to those who require such support. The expected outcome of these current programs is that regular health monitoring, feedback, and further guidance promote health behaviors, such as medical consultation for the treatment of disease, smoking cessation, and body mass index (BMI) management, which reduce the risk of CVD. However, the real-world effectiveness of these current programs on individual behavioral changes and their subsequent clinical outcomes remain unclear.
Therefore, this study aimed to explore the association between health checkups and the subsequent prescription of antihypertensive drugs and BP control status among individuals who have uncontrolled BP and are not on antihypertensives, who can have an increased risk of CV events, with the intention of inferring the effectiveness of the full health-checkup and guidance programs in the real world. Additionally, we explored potential factors associated with antihypertensive drug prescription and BP control. As behaviors for CV risk management, changes in smoking and BMI status were also assessed because these are major modifiable CV risk factors.
2 Methods
2.1 Study Design
This was a retrospective cohort study that used a Japanese healthcare database managed by MinaCare Co., Ltd. (Tokyo, Japan).
2.2 Data Source
The MinaCare database is an employment-based health-insurance database that includes periodically updated health-checkup data (e.g., individuals’ demographics, smoking status, and vital signs) and medical/pharmaceutical claims data of employees and their dependent family members since 2010. The MinaCare database covers a wide range of age groups up to 74 years who work in large-scale nationwide retailing industries, manufacturers, and food, information, transportation, and energy industries. The database contains data of approximately 6.1 million individuals with medical and pharmaceutical claims and approximately 2.3 million individuals with health checkups (as of February 2020). Subjects aged ≥ 75 years are not included in this database because they are to be included in a different insurance program other than employment-based health-insurance program.
During the health checkup, a recipient undergoes physical examination, such as BP, body-weight measurement, blood test for lipid metabolism and others, and physicians’ examination. Additionally, at the time of the checkup, a questionnaire on one’s lifestyle, such as smoking, and current and past medical treatment is completed. Data regarding follow-ups after checkups (e.g., access to health guidance, contents of health guidance, and other types of follow-ups provided) were not available in this database.
In the present analysis, we used data on BP and demographic and clinical characteristics, such as sex, age, BMI, and self-reported smoking status, in addition to prescription data on antihypertensive drugs.
2.3 Ethics Statement
This study involved data that exist in an anonymized structured format and contained no personal information. Therefore, obtaining informed consent from subjects and approval from the ethical review committee were not required because studies using only unlinkable anonymized data are outside the scope of the “Ethical Guidelines for Medical and Health Research Involving Human Subjects” set by the Japanese government. The study was conducted in accordance with legal and regulatory requirements (e.g., privacy protection laws) and scientific purpose, value, and rigor. MinaCare manages such anonymized data under the data transfer contract with the client health insurers.
2.4 Study Population
Subjects were included if they (1) were aged between 20 and 74 years at the time of the health checkup in 2015, (2) had systolic (SBP) and diastolic BP (DBP) data for 3 consecutive years from 2015 to 2017, and (3) had uncontrolled BP and were not prescribed antihypertensive drugs within 6 months before the health checkup in 2015.
2.5 Data Extraction and Management
Health checkup data between 2015 and 2017 (the latest 3 consecutive years available at the time of planning) and prescription claims data between 2014 and 2017 were extracted from the MinaCare database based on Japan’s fiscal year of April through March. Health checkups are usually conducted annually; in case of multiple records in any given year, the first record was used to render three records for each subject corresponding to 2015, 2016, and 2017.
2.6 Outcome Measures and Definitions
The primary outcome measures were changes in antihypertensive drug prescription and BP control status based on health-checkup results from 2015 to 2017.
BP control status and HT classification were defined according to the Japanese Society of Hypertension Guidelines for the Management of Hypertension in 2014 that were used in the clinical settings at the time of baseline health checkups in 2015 [15]. “Controlled BP” was defined as SBP < 140 mmHg and DBP < 90 mmHg, and “Uncontrolled BP” was defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg (Supplementary Table 1). HT was classified as HT grade I (SBP 140–159 and/or DBP 90–99 mmHg), HT grade II (SBP 160–179 and/or DBP 100–109), or HT grade III (SBP ≥ 180 and/or DBP ≥ 110) (Supplementary Table 1).
CV risk-management behavior was evaluated by antihypertensive drug prescription, BMI, and smoking habit. BMI and smoking, considered as secondary outcome measures, were assessed as behaviors for CV risk management because these are major risk factors of CV, and can be potentially changed by the subjects themselves. Antihypertensive drug prescription was defined by prescription records of antihypertensive medications within 6 months before the health checkup. Regarding antihypertensive drugs, all drugs indicated for hypertension and available at the time of this study were included in this study (Supplementary Table 2). There was 99.6% agreement between antihypertensive drug prescription within 6 and 12 months before the health checkup. Thus, antihypertensive drug prescription within 6 months before the health checkup was consistently used in the analyses. For self-reported smoking status, those who reported “yes” were considered current smokers, while those who reported “no” were considered past smokers and nonsmokers.
Metabolic syndrome was defined as waist circumference ≥ 85 cm (males) or ≥ 90 cm (females) and the presence of at least two of the following risk factors: (1) use of antihypertensive medication and/or SBP ≥ 130 mmHg and/or DBP ≥ 85 mmHg; (2) use of antihyperlipidemic medication and/or hypertriglyceridemia (triglyceride level ≥ 150 mg/dL) and/or hypo-HDL-cholesterolemia (HDL-c level < 40 mg/dL); and (3) use of DM medication and/or fasting blood glucose level ≥ 110 mg/dL [16].
2.7 Statistical Analysis
Demographic and clinical characteristics and primary outcome measures were descriptively summarized. Antihypertensive drug prescription (yes/no) in 2016 was summarized, considering the effect of sex, age, and HT stage at baseline (in 2015). Similarly, BP control status (controlled/uncontrolled) in 2016 was summarized, considering the effect of sex, age, baseline HT stage, and antihypertensive drug prescription in 2016.
BMI status in 2016 of the subjects with BMI ≥ 25 kg/m2 at baseline and self-reported smoking status in 2016 of subjects aged ≥ 40 years who reported to smoke at baseline were descriptively summarized. Additionally, to explore the association between changes in BMI and BP control status, the mean changes in BMI (± standard error) were plotted against baseline BMI for each of the three categories of BP changes from 2015 to 2016 (worsened, unchanged, and improved) in subjects aged 40–59 years. The analyses of BMI excluded missing values, which were rare (0.2%). The analysis of BMI and BP control status was performed for subjects aged 40–59 years because (1) there were relatively few subjects aged < 40 and ≥ 60 years, leading to a large variation of mean changes in BMI in these age groups, and (2) individuals aged ≥ 40 years were targeted for a new Japanese national program for lifestyle disease prevention, Specific Health Checkups and Specific Health Guidance, due to the increasing number of individuals strongly suspected of having metabolic syndrome or pre-metabolic syndrome [17, 18]. For smoking, the results were restricted to age ≥ 40 years because a large number of responses were missing for ages < 40 years.
Logistic regression was used to explore factors associated with antihypertensive drug prescription in 2016 and BP control status in 2016. The following variables at baseline were included as explanatory variables: sex, age (categorized by decade), HT stage (I/II/III), obesity status (BMI < 25 or ≥ 25 kg/m2), smoking status (yes/no/missing or not reported), antihyperlipidemic drug prescription within 6 months (yes/no), DM drug prescription within 6 months (yes/no), and metabolic syndrome (yes/no). The cutoff point for obesity (BMI ≥ 25 kg/m2) was based on the Japanese Society of Hypertension Guidelines for the Management of Hypertension in 2014 [15]. For each factor, the odds ratio (OR) and its 95% confidence interval (CI) were calculated. For BP control status in 2016, the analysis was conducted separately for those prescribed and not prescribed antihypertensive drugs in 2016.
No formal hypothesis test was used due to the exploratory nature of the study. Moreover, 95% CI for OR that excluded 1 was sometimes referred to as “statistically significant.”
SAS version 9.4 and R 3.5.0 were used in the statistical analysis.
3 Results
3.1 Subject Flow and Baseline Characteristics
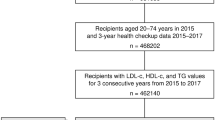
Figure 1 shows the subject flow of this study. Of the 931,038 subjects with health-checkup data in the MinaCare database in 2015, a total of 39,242 subjects with uncontrolled BP without antihypertensive drug prescription in 2015 were identified as the study population.
Table 1 summarizes the baseline characteristics of the study population. The proportion of females was 27.7%, and the mean ages at baseline were 46.9 years and 50.4 years in males and females, respectively. The proportions of subjects with BMI ≥ 25.0 kg/m2 in males and females were 48.8 and 37.6%, respectively. The proportions of smokers in males and females were 31.8 and 13.9%, respectively.
3.2 Antihypertensive Drug Prescription
In 2016, 88.9% (34,898/39,242) of subjects continued to have no antihypertensive drug prescription (Supplementary Figure 1). Of those subjects without prescription in 2015 and 2016, 90.9% (31,720/34,898) remained with no antihypertensive drug prescription in 2017. In contrast, 11.1% (4344/39,242) of subjects were prescribed antihypertensive drugs in 2016; of these, 86.8% (3769/4344) continued their prescription in 2017.
The proportions of subjects who were prescribed antihypertensive drugs in 2016 differed in HT stages and age but were generally similar between the sexes (Supplementary Figure 2).
3.3 Changes in Blood Pressure (BP) Control Status
Of the entire study population (n = 39,242), 61.2% (24,034/39,242) and 58.4% (22,927/39,242) had uncontrolled BP in 2016 and 2017, respectively.
Of the subjects without antihypertensive drug prescription in 2016, 62.9% (21,952/34,898) had uncontrolled BP in 2016 (Fig. 2a). Conversely, of the subjects with antihypertensive drug prescription in 2016, 47.9% (2082/4344) had uncontrolled BP (Fig. 2a).
BP control status by antihypertensive drug prescription status in 2016 and 2017. aNo/No = Subjects without antihypertensive drug prescription in both 2016 and 2017. bNo/Yes = Subjects without antihypertensive drug prescription in 2016 but with prescription in 2017. cYes/No = Subjects with antihypertensive drug prescription in 2016 but discontinued prescription in 2017. dYes/Yes = Subjects with antihypertensive drug prescription in both 2016 and 2017. BP blood pressure
When checking the prescription status in 2016 and 2017, 80.8% (31,720/39,242) of subjects continued to have no antihypertensive drug prescription. Of these, 60.5% (19,179/31,720) in 2016 and 61.5% (19,513/31,720) in 2017 remained with uncontrolled BP (Fig. 2b).
Subjects without antihypertensive drug prescription showed a greater tendency for uncontrolled BP in 2016 than those with drug prescription, regardless of sex, age, and HT stage at baseline (Supplementary Figure 3).
3.4 Changes in Body Mass Index (BMI) and Smoking Status
Because BMI and smoking status can be potentially changed by the subjects themselves, we examined these as measures of subjects’ behaviors for CV risk management. Among subjects with BMI ≥ 25 kg/m2 at baseline and non-missing BMI in 2016 (n = 17,940), 92.1% (n = 16,526) continued to have BMI ≥ 25 kg/m2, and 7.9% (n = 1414) had BMI < 25 kg/m2 in 2016. Among subjects aged ≥ 40 years who reported smoking at baseline (n = 9053), 93.8% (n = 8489) continued to smoke, 6.1% (n = 551) quit smoking, and 0.1% (n = 13) had missing data or no response in 2016. These trends for BMI and smoking were consistent irrespective of sex and age category (data not shown).
3.5 Factors Associated with Antihypertensive Drug Prescription in the Subsequent Year (Logistic Regression Analysis)
Logistic regression was conducted to identify factors associated with antihypertensive drug prescription in 2016 (Fig. 3). Factors positively associated with antihypertensive drug prescription with statistical significance were female sex (vs. male), age 50–59 years (vs. 40–49 years), age 60–69 years (vs. 40–49 years), age 70–74 years (vs. 40–49 years), HT stage II (vs. stage I), HT stage III (vs. stage I), baseline BMI ≥ 25.0 kg/m2 (vs. < 25.0 kg/m2), smoking at baseline (vs. no), antihyperlipidemic drug prescription at baseline (vs. no), DM drug prescription at baseline (vs. no), and metabolic syndrome at baseline (vs. no).
Factors associated with antihypertensive drug prescription in 2016. Odds ratios for “prescription of antihypertensive drug in 2016” as an outcome variable were calculated using the logistic regression model. The following variables at baseline were included as explanatory variables: sex, age, HT stage, obesity status, smoking status, antihyperlipidemic drug prescription within 6 months, DM drug prescription within 6 months, and metabolic syndrome. Subjects with missing BMIs were excluded. BMI body mass index, CL confidence limit, DM diabetes mellitus, HT hypertension, MS/NR missing or no response
Sensitivity analysis with a subgroup of subjects aged ≥ 40 years indicated no large difference in results (data not shown).
3.6 Factors Associated with Uncontrolled BP in the Subsequent Year (Logistic Regression Analysis)
Logistic regression was performed to explore factors associated with uncontrolled BP in 2016 among subjects with and without antihypertensive drug prescription in 2016 (Fig. 4). For the subjects treated with antihypertensive drugs in 2016 (Fig. 4a), factors associated with uncontrolled BP with statistical significance were age 60–69 years (vs. 40–49 years; OR 1.314; 95% CI 1.080‒1.600), HT stage II (vs. stage I; OR 1.722; 95% CI 1.506‒1.970), HT stage III (vs. stage I; OR 2.528; 95% CI 2.103‒3.038), baseline BMI ≥ 25.0 kg/m2 (vs. < 25.0 kg/m2; OR 1.273; 95% CI 1.109‒1.462), and DM drug prescription at baseline (vs. no; OR 1.898; 95% CI 1.315‒2.740).
Factors associated with uncontrolled BP in 2016. Odds ratios for the status of “uncontrolled BP in 2016” as an outcome variable were calculated using the logistic regression model. The following variables at baseline were included as explanatory variables: sex, age, HT stage, obesity status, smoking status, antihyperlipidemic drug prescription within 6 months, DM drug prescription within 6 months, and metabolic syndrome. The analysis was conducted separately for a those with antihypertensive drug prescription in 2016 and b those without antihypertensive drug prescription in 2016. Subjects with missing BMIs were excluded. BMI body mass index, BP blood pressure, CL confidence limit, DM diabetes mellitus, HT hypertension, MS/NR missing data or no response
For subjects without antihypertensive drug prescription in 2016 (Fig. 4b), factors positively associated with uncontrolled BP with statistical significance were age 60–69 years (vs. 40–49 years; OR 1.092; 95% CI 1.005‒1.186), HT stage II (vs. stage I; OR 4.551; 95% CI 4.207‒4.923), HT stage III (vs. stage I; OR 11.98; 95% CI 9.362‒15.32), and BMI ≥ 25.0 kg/m2 (vs. < 25.0 kg/m2; OR 1.239; 95% CI 1.177‒1.304). Factors negatively associated with uncontrolled BP were age 20–29 years (vs. 40–49 years; OR 0.548; 95% CI 0.484‒0.620), age 30–39 years (vs. 40–49 years; OR 0.741; 95% CI 0.688‒0.798), smoking at baseline (vs. no; OR 0.932; 95% CI 0.884–0.982), and antihyperlipidemic drug prescription at baseline (vs. no; OR 0.812; 95% CI 0.727‒0.906).
Sensitivity analysis with a subgroup of subjects aged ≥ 40 years indicated no large difference in results (data not shown).
3.7 BMI and BP Control
Because BMI is potentially modifiable by the subjects themselves and BMI ≥ 25 kg/m2 was identified as a significant factor associated with uncontrolled BP in the logistic regression analyses, additional exploratory analysis on BMI and BP was performed. The mean changes in BMI of subjects aged 40–59 years at baseline were plotted against baseline BMI for each of the three categories of BP stage changes (e.g., worsened, unchanged, and improved) from 2015 to 2016 (Fig. 5). Subjects with “improved” BP status tended to have a negative mean change in BMI. In contrast, subjects with “worsened” BP status tended to have a positive mean change in BMI. These trends were more prominent in males and those with a higher baseline BMI.
Mean change (± standard error) in BMI from 2015 to 2016 by baseline BMI. The lines indicate changes in BP stage from 2015 to 2016 (blue, worsened; red, unchanged; green, improved). The figures are shown by sex and baseline age category. Subjects aged between 40 and 60 years at baseline and with available BMI values in 2015‒2017 were analyzed. BMI body mass index, BP blood pressure
4 Discussion
To assess behavioral changes and the improvement of clinical outcomes in individuals after they participated in real-world health-checkup and guidance programs in Japan, we specifically examined the changes in antihypertensive drug prescription and BP control status in individuals with checkup results indicating the need for CV risk management, using real-world data. We found that among the subjects without antihypertensive drug prescription with uncontrolled BP at baseline (in 2015), 88.9% remained to have no antihypertensive drug prescription in 2016. Of these subjects without prescription, 62.9% continued to have uncontrolled BP in 2016, which contrasted with 47.9% of those who started antihypertensive drug prescription in 2016. Similarly, of those who continued to have no antihypertensive drug prescription in 2016 and 2017 (80.8%), 60.5% in 2016 and 61.5% in 2017 continued to have uncontrolled BP. Uncontrolled BP in the subsequent year was statistically significantly associated with age 60–69 years (vs. 40–49 years), HT stage II (vs. stage I), HT stage III (vs. stage I), and BMI ≥ 25.0 kg/m2 (vs. < 25.0 kg/m2), regardless of antihypertensive drug prescription in 2016.
Despite the reminder of abnormal findings, further guidance, and encouragement in health-checkup and guidance programs, > 80% of the subjects remained to have no antihypertensive drug prescription in the subsequent years (2016 and 2017), and ≥ 90% of the subjects did not change their CV risk-related lifestyle, that is, those who had a baseline BMI ≥ 25 kg/m2 and smokers at baseline aged ≥ 40 years maintained their statuses in the subsequent year. These results indicated that subjects with abnormal health-checkup records were left untreated and uncontrolled. The Japanese national program for lifestyle disease prevention, Specific Health Checkups and Specific Health Guidance, offers lifestyle modification consultation and/or education programs according to health-checkup results. However, it was reported that most subjects eligible for the guidance/intervention program did not attend the program [19, 20], and only approximately 10% of the eligible subjects completed the program [21]. Furthermore, although the intervention program itself was shown to be sufficiently effective in eliciting behavioral modifications and improving abdominal obesity [19], a recent study reported that this intervention program was not associated with clinically meaningful weight loss or improvement of other CV risk factors [22]. Although the present study did not evaluate this particular program, our real-world results would add to these previous findings. Taken together, it is suggested that current health-checkup and guidance programs in Japan may be inadequate for driving personal behavioral changes and motivating individuals into action. Greater effort and better strategies to drive behavioral changes are required.
These results possibly reflect some types of barriers to antihypertensive drug treatment or CV risk-management behaviors in health-checkup recipients. A previous study suggested a low awareness of HT management among Japanese workers [23]. Furthermore, a recent study reported that Japan is among the countries with the lowest rates of HT awareness, treatment, and control [14]. Thus, in individuals who need to improve their condition, further efforts may be needed to change their habits, such as endeavoring to alter lifestyles and seeking medical advice. As a basis for new approaches specific to Japan, there may be a need to bring to light patients’ awareness and understanding of BP management methods because previous surveys on awareness of HT management were mainly conducted among physicians [24,25,26]. Some patient-centered surveys may contribute to the identification of such barriers, which would provide useful information for the development of more effective strategies for motivating individual behavioral changes for CVD risk management.
The need for lifestyle modification may be supported by the finding that a high BMI (≥ 25 kg/m2) in subjects with and without antihypertensive drug prescription was associated with uncontrolled BP. Indeed, as shown in Fig. 5, subjects who showed improvement in BMI from 2015 to 2016 generally presented greater improvements in BP stages than those who did not show a reduction in BMI, indicating that those who succeeded in controlling BMI were likely to improve their BP or vice versa. In contrast, in the logistic regression analysis, there was an apparent small “protective” effect of smoking in those who continued without antihypertensive drug prescription in 2016 (OR 0.932). With some reports negating the adverse effect of smoking on BP [27,28,29], the effect of smoking on BP control may not yet have reached a consistent conclusion. Nevertheless, our study results suggest the importance of primary prevention for HT and CVD management with a comprehensive approach—that is, pharmacological treatment with lifestyle modification.
This study has several limitations. First, the database was limited to Japanese employees and their dependents who work in specific sectors, which may not fully represent the general population of Japan. For instance, the database does not include individuals in the primary industries (e.g., agriculture, fishery, and forestry), self-employed individuals, and older-age individuals (i.e., individuals aged ≥ 75 years). However, with a large population size covering a wide range of ages, the MinaCare database reflects the individuals insured by employment-based health insurance and is of great use in studying such a population. Indeed, based on a previous study that used the MinaCare database reporting consistent data with two national data reports [10], the generalizability of this study is not considered low. Second, antihypertensive drug prescription, BMI, and smoking were used to indirectly assess the subjects’ behavioral changes in CV management in this database. Prospective cohort studies would allow a wider range of methods and outcomes to assess “behaviors” more directly. Lastly, it should be noted that although some individuals included in this study may have received some form of follow-up activities such as health guidance, the effect of these activities was not evaluated in this study. The aim of this study was to obtain a real-world view of the full checkup and guidance programs. Thus, assessment of a particular effort or intervention was outside the scope of this study. However, such assessments would be worthwhile and should be conducted in future studies in order to develop better and more effective programs. Although the abovementioned limitations of this study should be noted, to the best of our knowledge, this is the first study to explore the association between health checkup and the subsequent CVD risk-management behaviors in workers in Japan, analyzing a large number of individuals (39,242 subjects). Another strength of our study is that the prescription status was obtained from prescription data instead of self-reported data. Thus, recall bias was prevented as the data obtained did not depend on subjects’ memory.
In conclusion, our study results suggest that current health-checkup and guidance programs leave most individuals untreated and are insufficiently effective for behavioral change. Based on individuals’ health-checkup results, further practices for committing to lifestyle modification and seeking medical advice need to be undertaken to improve health behavior.
References
Mendis S, Puska P, Norrving B, World Health Organization. Global atlas on cardiovascular disease prevention and control. Geneva: World Health Organization. 2011. https://apps.who.int/iris/bitstream/handle/10665/44701/9789241564373_eng.pdf?sequence=1&isAllowed=y. Accessed 8 July 2019.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50.
Ikeda N, Inoue M, Iso H, Ikeda S, Satoh T, Noda M, et al. Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLoS Med. 2012;9:e1001160.
Lawes CM, Rodgers A, Bennett DA, Parag V, Suh I, Ueshima H, et al. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003;21:707–16.
Kitamura A, Yamagishi K, Imano H, Kiyama M, Cui R, Ohira T, et al. Impact of hypertension and subclinical organ damage on the incidence of cardiovascular disease among Japanese residents at the population and individual levels—the Circulatory Risk in Communities Study (CIRCS). Circ J. 2017;81:1022–8.
World Health Organization. Global status report on noncommunicable diseases 2014 (No. WHO/NMH/NVI/15.1). World Health Organization. 2014. https://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf. Accessed 8 July 2019.
Ministry of Health, Labour and Welfare [Internet]. Tokyo: report of vital statistics in 2018. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/geppo/nengai18/dl/gaikyou30.pdf(Japanese). Accessed 13 December 2019.
Muka T, Imo D, Jaspers L, Colpani V, Chaker L, van der Lee SJ, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015;30:251–77.
Nomura S, Sakamoto H, Glenn S, Tsugawa Y, Abe SK, Rahman MM, et al. Population health and regional variations of disease burden in Japan, 1990–2015: a systematic subnational analysis for the Global Burden of Disease Study 2015. Lancet. 2017;390:1521–38.
Shima D, Ii Y, Yamamoto Y, Nagayasu S, Ikeda Y, Fujimoto Y. A retrospective, cross-sectional study of real-world values of cardiovascular risk factors using a healthcare database in Japan. BMC Cardiovasc Disord. 2014;14:120.
Ministry of Health, Labour and Welfare [Internet]. Tokyo: data source of the specific health checkups and specific health guidance. http://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/info02a-2.html(Japanese). Accessed 11 June 2019.
Ministry of Health, Labour and Welfare [Internet]. Tokyo: data source of the national health and nutrition survey. http://www.mhlw.go.jp/bunya/kenkou/kenkou_eiyou_chousa.html(Japanese). Accessed 11 June 2019.
Kudo N, Yokokawa H, Fukuda H, Sanada H, Miwa Y, Hisaoka T, Isonuma H. Achievement of target blood pressure levels among Japanese workers with hypertension and healthy lifestyle characteristics associated with therapeutic failure. PLoS One. 2015;10:e0133641.
NCD Risk Factor Collaboration (NCD-RisC). Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394:639–51.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–392.
Teramoto T, Sasaki J, Ueshima H, Egusa G, Kinoshita M, Shimamoto K, et al. Metabolic syndrome. J Atheroscler Thromb. 2008;15:1–5.
Ministry of Health, Labour and Welfare [Internet]. Tokyo: specific health checkups and specific health guidance. https://www.mhlw.go.jp/seisaku/2009/09/02.html(Japanese). Accessed 13 July 2020.
Ministry of Health, Labour and Welfare [Internet]. Tokyo: the national health and nutrition survey in Japan, 2018. https://www.mhlw.go.jp/content/000681200.pdf (Japanese). Accessed 13 July 2020.
Nakao YM, Miyamoto Y, Ueshima K, Nakao K, Nakai M, Nishimura K, et al. Effectiveness of nationwide screening and lifestyle intervention for abdominal obesity and cardiometabolic risks in Japan: The metabolic syndrome and comprehensive lifestyle intervention study on nationwide database in Japan (MetS ACTION-J study). PLoS One. 2018;13:e0190862.
Tsushita K, Hosler AS, Miura K, Ito Y, Fukuda T, Kitamura A, Tatara K. Rationale and descriptive analysis of specific health guidance: the nationwide lifestyle intervention program targeting metabolic syndrome in Japan. J Atheroscler Thromb. 2018;25:308–22.
Ministry of Health, Labour and Welfare [Internet]. Tokyo: Tokutei kenkoushinsa tokutei hokenshidoni kansuru data. https://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/info02a-2.html(Japanese). Accessed 7 August 2020.
Fukuma S, Iizuka T, Ikenoue T, Tsugawa Y. Association of the National Health Guidance Intervention for obesity and cardiovascular risks with health outcomes among Japanese men. JAMA Intern Med. 2020;180:1630–7. https://doi.org/10.1001/jamainternmed.2020.4334.
Tanaka T, Okamura T, Yamagata Z, Takebayashi T, Tamura U, Kusaka Y, et al. Awareness and treatment of hypertension and hypercholesterolemia in Japanese workers: the High-risk and Population Strategy for Occupational Health Promotion (HIPOP-OHP) study. Hypertens Res. 2007;300:921–8.
Ikeda N, Hasegawa T, Hasegawa T, Saito I, Saruta T. Awareness of the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2000) and compliance to its recommendations: surveys in 2000 and 2004. J Hum Hypertens. 2006;20:263–6.
Obara T, Ubeda SR, Ohkubo T, Matsuura H, Ishimitsu T, Takata M, et al. Awareness of the Japanese Society of Hypertension Guidelines for the Management of Hypertension and their use in clinical practices: 2009 survey results. Hypertens Res. 2015;38:400–4.
Mogi M, Hasebe N, Horiuchi M, Shimamoto K, Umemura S. The results of a survey of physicians about the Japanese Society of Hypertension Guidelines for the Management of Hypertension 2014 and its clinical use. Hypertens Res. 2016;39:660–3.
Mikkelsen KL, Wiinberg N, Høegholm A, Christensen HR, Bang LE, Nielsen PE, et al. Smoking related to 24-h ambulatory blood pressure and heart rate: a study in 352 normotensive Danish subjects. Am J Hypertens. 1997;10:483–91.
Imamura H, Miyamoto N, Uchida K, Teshima K, Masuda Y, Kobata D. Cigarette smoking, blood pressure and serum lipids and lipoproteins in middle-aged women. J Physiol Anthropol Appl Hum Sci. 2001;20:1–6.
John U, Meyer C, Hanke M, Völzke H, Schumann A. Smoking status, obesity and hypertension in a general population sample: a cross-sectional study. QJM. 2006;99:407–15.
Acknowledgements
Medical writing support was provided by Ayumi Hamaguchi at Clinical Study Support, Inc. (Nagoya, Japan) and funded by Pfizer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was sponsored and funded by Pfizer.
Conflict of interest
SH, KN, and YA are full-time employees of Pfizer Japan, Inc. and hold Pfizer stock. YI is a full-time employee of Pfizer R&D Japan and holds Pfizer stock. YY and KO have no conflicts of interest to declare.
Ethical approval and consent to participate
This study involved data that exist in an anonymized structured format and contained no personal information. Studies exclusively using unlinkable anonymized data are outside the scope of the “Ethical Guidelines for Medical and Health Research Involving Human Subjects” by the Japanese government. Therefore, obtaining informed consent and approval from the ethical review committee were not required for this study.
Consent for publication
Not applicable.
Availability of data and materials
The data that support the findings of this study are available from the database maintained by MinaCare Co. Ltd. (Tokyo, Japan), independent of Pfizer. Pfizer is not involved in validating or storing the data included in the database. Restrictions apply to the availability of these data, which were used under license for the current study, and are not publicly available. However, data are available from the authors upon reasonable request and with permission from MinaCare Co. Ltd.
Code availability
Not applicable.
Author contributions
SH, YI, and KN were involved in the development of the protocol. YY developed the database, and YI analyzed the data. All authors, including KO and YA, contributed to conceptualizing and designing the study, interpreting the results, and drafting and revising the manuscript. All authors approved the final manuscript and agreed to be accountable for all aspects of the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Higa, S., Ii, Y., Nozawa, K. et al. Relationship of Annual Health Checkups with the Subject’s Subsequent Behavior of Cardiovascular Risk Management in a Real-World Setting in Japan: A Retrospective Cohort Study on Changes in Antihypertensive Drug Prescription and Blood Pressure from 2015 to 2017. Drugs - Real World Outcomes 8, 215–225 (2021). https://doi.org/10.1007/s40801-020-00224-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-020-00224-5