Abstract
Purpose of Review
Despite no general conclusions regarding the therapeutic effect of MSCs on virus-induced acute lung injury in pre-clinical studies, a significant number of clinical trials using MSC-based treatment for COVID-19-associated ARDS were initiated during the global pandemic. Here, we aimed to discuss differences and similarities in clinical trials using MSC-based treatments for classical ARDS and COVID-19-associated ARDS and to raise some future perspectives.
Recent Findings
Several pre-clinical studies have demonstrated that MSC treatment may not be a good treatment option for virus infections because MSCs themselves are susceptible to the virus. However, MSCs lack expression of the angiotensin-converting enzyme 2 (ACE2) receptor, suggesting that MSCs are not likely to be infected by the COVID-19 virus. Interestingly, recent meta-analyses demonstrated that an improved survival rate in patients with COVID-19-associated ARDS treated with MSCs was obtained in 24 out of 26 completed clinical trials.
Summary
This review provides comparative perspectives on MSC-based therapy for COVID-19-associated ARDS and classical ARDS.
Similar content being viewed by others
Introduction
The classical acute respiratory distress syndrome (ARDS) was described for the first time in 1967 by Ashbaugh et al. as a destructive lung injury with an uncontrolled inflammatory process [1]. This acute inflammatory process causes severe alveolar damage and capillary basement membrane leakage leading to a progressive respiratory failure with high morbidity and mortality burden (Reviewed in [2, 3]). Classical ARDS can result from different causes including sepsis, pneumonia, and trauma (Reviewed in [2]). During the last years, more and more studies point towards that classical ARDS is an umbrella term that includes several different ARDS phenotypes [2, 4, 5••, 6, 7]. For example, Calfee et al. described in 2014 the two subgroups hyper- and hypo-inflammatory ARDS. The hyper-inflammatory group, with hallmarks such as high plasma levels of inflammatory markers including interleukin (IL)-6, IL-8, and plasminogen activator inhibitor-1 (PAI-1), was associated with more severe disease progression and lower survival rate [4]. These two phenotypes have also been identified in other cohorts and clinical trials including for example the SAILS trial and the HARP-2 trial [8, 9] with similar findings.
During the last decades, much effort has been put into understanding the pathogenesis and pathophysiology of ARDS, and many clinical trials have been completed in the search for an effective treatment. In particular, recent clinical trials have investigated mesenchymal stromal cell (MSC)-based therapies, based on the results from very successful pre-clinical studies utilizing bacteria, endotoxin, smoke inhalation, and other models of acute lung injury. These clinical studies have all demonstrated safety but unfortunately failed to uniformly prove significantly increased clinical outcomes [10,11,12,13].
In 2019, the coronavirus disease 2019 (COVID-19)-associated ARDS was described for the first time [14, 15]. Although there are similarities between the classical ARDS and the COVID-19-associated ARDS pathology, an increasing number of studies demonstrate that there are also differences between the syndromes [2, 16,17,18], which will be summarized in the section below (Fig. 1). The first clinical investigation using MSC-based therapy to treat COVID-19-associated ARDS was initiated very early in the pandemic outbreak, and the numbers of completed studies are currently increasing (Table 1) [19••]. Similar to the results from the MSC trials on patients with classical ARDS, MSC infusions were shown to be safe for the patients. Interestingly, a pooled analysis of the clinical trials using MSCs to treat COVID-19-associated ARDS completed between January 2020 and the end of July 2022 demonstrated a relative risk reduction for all-cause COVID-19 mortality (RR = 0.63) [19••]. However, the number of studies is still fairly small, and results derived from the different studies are difficult to compare to each other since the standard clinical treatment strategies changed during the pandemic, and sometimes also during an ongoing study [19••, 20, 21].
Important pathological similarities and differences between classical ARDS and COVID-19-associated ARDS. Classical ARDS and COVID-19-associated ARDS share several similarities in their pathology including significant lung inflammation with fluid accumulation in the alveoli, respiratory failure, and excessive immune response, but there are also important differences between the two syndromes which have been summarized in this figure. Understanding these differences is important for the clinical management and the development of therapeutic strategies for both classical ARDS and COVID-19-associated ARDS. Abbreviations: ARDS, acute respiratory distress syndrome; COVID-19, coronavirus disease 2019; SARS-CoV-2 virus, severe acute respiratory distress syndrome coronavirus 2. This figure was illustrated using Biorender.com
In the first part of this review, we will discuss the differences and similarities between ARDS and COVID-19-associated ARDS pathology. In the second part, we will summarize, discuss, and compare the results from the clinical trials using MSC-based treatment for ARDS and COVID-19-associated ARDS.
Differences in Classical ARDS and COVID-19-Associated ARDS Pathophysiology
Classical ARDS and COVID-19-associated ARDS share several similarities in their pathology including significant lung inflammation with fluid accumulation in the alveoli, respiratory failure, and excessive immune response, but there are also important differences between the two syndromes (Fig. 1) [2, 16,17,18, 22]. The most obvious difference is that COVID-19-associated ARDS is exclusively caused by the SARS-CoV-2 virus, while the classical ARDS can have different etiologies including for example trauma, sepsis, and aspiration [2, 3, 14, 15, 22]. Moreover, other significant differences include differences in respiratory mechanics where higher respiratory system compliance and increased dead space fractions have been reported in patients with COVID-19-associated ARDS compared to patients with the classical ARDS [16, 23••, 24]. Moreover, increased levels of thrombotic mediators and lower expression of interferons have been reported in COVID-19-associated ARDS compared to the classical ARDS [25, 26]. A reduction of neutrophil-to-lymphocyte ratio with an impaired or delayed lymphocyte activation has also been observed in COVID-19-associated ARDS compared to classical ARDS, where the reduced neutrophil-to-lymphocyte ratio has been correlated to an increased disease severity [25, 26]. There is also evidence that patients with COVID-19-associated ARDS have elevated levels of circulating D-dimer [23••]. Understanding these differences is important for the clinical management and the development of therapeutic strategies for both classical ARDS and COVID-19-associated ARDS.
MSC-Based Therapies for Classical ARDS and COVID-19-Associated ARDS
What Is Known from Pre-clinical Experiments on MSC Treatment for Virus-Induced Acute Lung Injury?
There is a large body of literature demonstrating the efficacy of MSC administration in pre-clinical models of acute lung injury; however, most of them have focused on endotoxin- or bacterial-induced lung injury [27, 28] and not so much focus, so far, has been on virus-induced lung disease. Nevertheless, a few papers on MSC-based treatment for virus-induced acute lung injury have been published with contradictory results. For example, in a recent paper, Tan et al. investigated the effect of MSC treatment in H1N1 influenza virus-induced acute lung injury. Here, the authors reported that MSC treatment decreased the total cell count in bronchoalveolar lavage fluid and increased the number of infiltrating CD4+, CD8+, B-cells, T-cells, and monocyte in the alveolar space, but did not result in an improved survival rate or reduced viral load compared to untreated control cells [29••]. Similar results, i.e., no improved survival rate and no reduction in viral load, have also been reported by other groups [30, 31]. In contrast, Qin et al. demonstrated that MSC treatment reduced herpesvirus-68-induced pneumonia with decreased lung damage, decreased levels of inflammatory markers, and inhibition of viral replication compared to untreated control mice [32]. Similar results were reported by Chan et al., where they reported that mice infected with influenza A/H5N1 treated with MSCs had an increased survival rate compared to controls treated with control fibroblasts [33]. As such, there is no general conclusion regarding the therapeutic effect of MSCs on virus-induced acute lung injury. One potential explanation for this could be that MSCs are effective against specific viruses. For example, Tan et al. demonstrated that the majority of MSCs in their study expressed α-2,6-linked SA (influenza A/H1N1 virus binding receptors) and were highly susceptible to infection of the virus. Interestingly, it has been reported that human MSCs do not express the angiotensin-converting enzyme 2 (ACE2) receptor [34••], suggesting that MSCs might not be susceptible to infection of the COVID-19 virus.
What Is Known from Clinical Trials?
MSC-Based Clinical Trials in Patients with Classical ARDS
Since the two first phase I trials on MSC-based treatments for classical ARDS in 2014–2015 [10, 11], several other trials have been completed which all demonstrated that MSCs were well-tolerated in this patient group, but no significant improved lung function or other clinical relevant outcomes were consistently observed [12, 35, 36••, 37]. The data obtained in the clinical trials mentioned above, except the two latest publications, have been extensively summarized by us and others [38,39,40] and will therefore not be covered here. In the more recent study by Wick et al., the authors measured potential biomarkers in the airspace and in circulation in ARDS patients included in the START trial study 48 h after treatment with MSC or placebo. Here, they found that there was a decrease in the airspace proteins Ang-2, IL-6, and sTNFR1 in patients treated with MSC compared to patients in the placebo group. Interestingly, the levels of measured biomarkers in the circulation differed very much from those measured in the mini-bronchoalveolar lavage fluid samples. This is important information to consider when collecting samples for treatment evaluation and biological understanding, as biomarkers isolated from the plasma versus the airspace most likely reflect different biological processes [37]. The most recent completed clinical trial in classical ARDS was published in 2022; here, the authors used multipotent adult progenitor cells to treat classical ARDS (moderate-to-severe) in a multicenter, randomized, double-blind, dose-escalation, placebo-controlled phase 1/2 trial. The patients were given either 300 × 106 or 900 × 106 cells diluted in 300 ml PlasmaLyte-A or placebo through a 200-µm blood filter tubing set as a single peripheral or central venous infusion. Similar to the other completed trials, the cells were demonstrated to be well-tolerated, and no acute safety concerns were observed. There was one death that occurred in the cell-treated group; however, it was determined by the data and safety monitoring board (DSMB) to be unrelated to the cell therapy. At day 28 after treatment, there was an increased number of treatment-emergent adverse events in the group that received the cells compared to the placebo group (91.3% in patients receiving 900 × 106 cells vs. 60% for placebo); however, there was a lower mortality rate in the cell-treated group both at day 28 (25% in patients receiving 900 × 106 cells vs. 40% for placebo) and at day 365 (40% in patients receiving 900 × 106 cells vs. 50% for placebo) compared to placebo [36••].
MSC-Based Clinical Trials in Patients with COVID-19-Associated ARDS
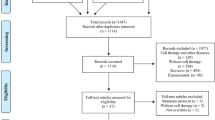
After the COVID-19 outbreak, the enthusiasm for using MSCs as cell-based therapy was once again raised leading to a dramatic increase in clinical trials using MSCs as therapy for COVID-19-associated ARDS. Searching on the PubMed database for published clinical trials through October 2, 2023, using the keywords “COVID-19” and “mesenchymal stromal cells,” we identified 24 published studies (summarized in Table 1). In this section, we will briefly summarize and discuss the more recent papers and highlight some interesting lessons that can be learned from these trials as well as discuss differences and similarities with completed MSC-based trials on patients with classical ARDS.
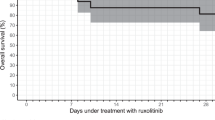
In 2022, Kirkham et al. published a meta-analysis of controlled trials of MSC-based treatment for patients with COVID-19-associated ARDS. This was a systematic search of the literature conducted on studies published until November 15, 2021. Based on the results from the reviewed studies, the authors concluded that MSCs likely can reduce mortality in patients with critical or severe COVID-19 because they found evidence that MSC-based treatment reduced the relative and absolute risk of death at the study endpoint [41•]. All studies included in this meta-analysis were however very small and different investigational protocols were used [41•]. Earlier this year, 2023, Soetjahjo et al. published a double-blind, randomized, placebo-controlled, multicenter trial (NCT04333368) involving severe COVID-19 patients in which they gave three injections of umbilical cord-derived MSCs with 1 × 106 cells/kg body weight per time point. The study enrolled 42 patients who were randomly assigned into two equal groups and aimed to investigate the safety and effectiveness of MSC-based treatment. No decrease in the length of hospitalization was seen in the MSC-treated group compared to the control group. However, the MSC-treated group had a significant increase in oxygenation index and a smaller increase in procalcitonin values compared to the control group [42•]. In the trial by Zarrabi and colleagues (IRCT20200217046526N2), MSC treatment was combined with a dose of extracellular vesicles (EVs) derived from MSCs. In this randomized, multicentric, phase II clinical trial, 43 patients with severe COVID-19 were enrolled (MSC alone, n = 11; MSC combined with EVs, n = 8; control group, n = 24), and the study aimed to assess safety and efficacy of two doses of perinatal tissue-derived MSC or one dose of MSCs followed by a dose of MSC-derived EVs. The authors reported the treatments to be safe with minimal adverse events, and a decreased serum level of inflammatory markers was seen in all study groups; however, there was a more prominent change in the MSC alone and MSC combined with EVs compared to controls [43•]. Li et al. published their 2-year follow-up results from a randomized, double-blind, placebo-controlled trial (NCT04288102) [44], in which 100 patients with severe COVID-19 were included. The patients received either 3 MSC infusions (n = 65, 4 × 107 cells per infusion) or placebo (n = 35) on days 0, 3, and 6 in combination with standard of care. The authors observed that MSC administration was safe 2 years after treatment; however, the efficacy of MSC treatment reported at the 1-year follow-up [45] was not significantly sustained at the 2-year follow-up according to 6-min walking distance data, quality of life, and extent of lung damage. There were no significant differences in pulmonary fibrosis based on the CT images between the MSC group and the placebo group at 24-month follow-up [44]. Taken together, it is very difficult to draw any conclusions from these different studies on COVID-19-associated ARDS because since they were performed during the pandemic, they are small studies, the standard of care changed between different trials, and sometimes within one trial, different MSC sources, doses, and criteria were used. However, there are several clinical trials that report at least some beneficial effects, and similar to the MSC trials on classical ARDS, they demonstrate that MSC-based therapy is safe also for COVID-19-associated ARDS. As suggested by Kirkham et al., one option would be to develop a “master protocol” to ensure consistency of cell product production and manufacturing and dosing strategies to simplify the ability to compare results between different clinical trials [41•]. However, creating a “master protocol” for ensuring consistent product manufacturing among the clinical trials would entail several difficulties including for example intellectual patent rights associated with each pharmaceutical industry and differences in regional laws and regulations.
So far, only first-generation MSC products have been used in all MSC therapy for classical and COVID-19-associated ARDS; however, a large body of literature indicates that pre-activating MSCs with appropriate cues prior to infusion could enhance their therapeutic potency [46,47,48]. For example, IFN-γ pre-treated MSCs have been demonstrated to inhibit T-cell proliferation as well as inhibit T-cell production of IFN-γ, TNF-α, and IL-2 in vitro [46]. However, contradictory results have been published on the actual in vivo effect of IFN-γ pre-treated MSCs in experimental graft versus host disease models [48, 49]. In another study, Bustos et al. pre-treated MSCs with serum obtained from ARDS patients and found that pre-treated MSCs produced increased levels of anti-inflammatory cytokines such as IL-10 and IL-11RN and decreased levels of pro-inflammatory cytokines such as IL-6, IL-8, IFN-γ, and IL-1β [47]. An altered secretome profile has also been demonstrated by MSCs treated with bronchoalveolar lavage fluid samples obtained from ARDS patients [50]. An increasing number of publications suggest that the MSC therapeutic function depends on the microenvironment they encounter [47, 50,51,52,53]. Therefore, it is essential to understand how MSC function is altered after entering a COVID-19 infectious environment containing large concentrations of pro-inflammatory cytokines (cytokine storm) and neutralizing antibodies and B-cell responses. In a recently published study, it was demonstrated that MSCs inhibit B-cell differentiation and block pan-antibody secretion, findings that may have implications for B-cell-mediated anti-viral responses [54]. Another important factor is the increased levels of D-Dimer observed in COVID-19 patients [23••]. In a few case reports, elevation levels of D-dimer have been observed after MSC treatment and linked with serious side effects such as pulmonary embolisms and venous clots [55, 56]. However, the pooled analysis on the clinical trials using MSCs to treat COVID-19-associated ARDS found that MSC-based treatment was safe for patients with COVID-19-associated ARDS [19••]. However, further studies are warranted before we can understand the exact impact of the COVID-19-associated ARDS environment on infused MSCs.
Summary and Final Remarks
The completed clinical trials have all demonstrated that MSC-based treatment is safe to be used as treatment for patients with classical ARDS and COVID-19-associated ARDS, despite the different etiologies and differences in pathophysiology. Some of the clinical trials published during the last years and recent meta-analyses suggest that MSCs could potentially reduce mortality in patients with severe COVID-19-associated ARDS.
After several decades of progression in the field of MSC-based therapies for respiratory diseases with good pre-clinical outcomes and very stimulating results, we have now reached a plateau phase without a well-defined track forward. After several years with many completed clinical trials reporting no significant improved outcomes, it is easy to be critical and question if MSC-based therapies would be a likely future treatment option for patients with respiratory failure or severe acute lung disorders. However, we strongly believe that MSC-based therapy will be a future therapeutic option for at least subgroups of patients within specific inflammatory lung disorders such as ARDS and COVID-19-associated ARDS. But to advance to the next step, it is important to take a step back. We need to return to do some bench work and to repeat many of the in vitro and pre-clinical experiments with all the advanced techniques and instruments that are now available to us, because we believe that it is crucial that we understand (i) the MSC biology, (ii) the MSC–host environment interaction, (iii) the plasticity of in vivo MSCs, and (iv) which subgroups of patients that truly have a chance of benefit from this type of treatment before we can obtain significantly improved outcomes in future MSC-based clinical trials for acute inflammatory lung disorders.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967;2(7511):319–23.
Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers. 2019;5(1):18.
Yadav H, Thompson BT, Gajic O. Fifty years of research in ARDS. Is acute respiratory distress syndrome a preventable disease? Am J Respir Crit Care Med. 2017;195(6):725–36.
Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA, et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2(8):611–20.
•• Wilson JG, Calfee CS. ARDS subphenotypes: understanding a heterogeneous syndrome. Crit Care. 2020;24(1):102. This study summarizes the current knowledge of ARDS subphenotypes.
Reilly JP, Calfee CS, Christie JD. Acute respiratory distress syndrome phenotypes. Semin Respir Crit Care Med. 2019;40(1):19–30.
Grasselli G, Calfee CS, Camporota L, Poole D, Amato MBP, Antonelli M, et al. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 2023;49(7):727–59.
Sinha P, Kerchberger VE, Willmore A, Chambers J, Zhuo H, Abbott J, et al. Identifying molecular phenotypes in sepsis: an analysis of two prospective observational cohorts and secondary analysis of two randomised controlled trials. Lancet Respir Med. 2023.
Moore AR, Pienkos SM, Sinha P, Guan J, O’Kane CM, Levitt JE, et al. Elevated plasma interleukin-18 identifies high-risk acute respiratory distress syndrome patients not distinguished by prior latent class analyses using traditional inflammatory cytokines: a retrospective analysis of two randomized clinical trials. Crit Care Med. 2023.
Zheng G, Huang L, Tong H, Shu Q, Hu Y, Ge M, et al. Treatment of acute respiratory distress syndrome with allogeneic adipose-derived mesenchymal stem cells: a randomized, placebo-controlled pilot study. Respir Res. 2014;15:39.
Wilson JG, Liu KD, Zhuo H, Caballero L, McMillan M, Fang X, et al. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir Med. 2015;3(1):24–32.
Matthay MA, Calfee CS, Zhuo H, Thompson BT, Wilson JG, Levitt JE, et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir Med. 2019;7(2):154–62.
Simonson OE, Mougiakakos D, Heldring N, Bassi G, Johansson HJ, Dalen M, et al. In vivo effects of mesenchymal stromal cells in two patients with severe acute respiratory distress syndrome. Stem Cells Transl Med. 2015;4(10):1199–213.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506.
Beloncle FM. Is COVID-19 different from other causes of acute respiratory distress syndrome? J Intensive Med. 2023;3(3):212–9.
Zhu Y, Sharma L, Chang D. Pathophysiology and clinical management of coronavirus disease (COVID-19): a mini-review. Front Immunol. 2023;14:1116131.
Leisman DE, Deutschman CS, Legrand M. Facing COVID-19 in the ICU: vascular dysfunction, thrombosis, and dysregulated inflammation. Intensive Care Med. 2020;46(6):1105–8.
•• Couto PS, Al-Arawe N, Filgueiras IS, Fonseca DLM, Hinterseher I, Catar RA, et al. Systematic review and meta-analysis of cell therapy for COVID-19: global clinical trial landscape, published safety/efficacy outcomes, cell product manufacturing and clinical delivery. Front Immunol. 2023;14:1200180. This systematic review and meta-analysis of cell therapy for COVID-19 provides the most comprehensive and up-to-date summary.
Moll G, Drzeniek N, Kamhieh-Milz J, Geissler S, Volk HD, Reinke P. MSC Therapies for COVID-19: importance of patient coagulopathy, thromboprophylaxis, cell product quality and mode of delivery for treatment safety and efficacy. Front Immunol. 2020;11:1091.
Ringden O, Moll G, Gustafsson B, Sadeghi B. Mesenchymal stromal cells for enhancing hematopoietic engraftment and treatment of graft-versus-host disease, hemorrhages and acute respiratory distress syndrome. Front Immunol. 2022;13: 839844.
Huppert LA, Matthay MA, Ware LB. Pathogenesis of acute respiratory distress syndrome. Semin Respir Crit Care Med. 2019;40(1):31–9.
•• Grasselli G, Tonetti T, Protti A, Langer T, Girardis M, Bellani G, et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: a multicentre prospective observational study. Lancet Respir Med. 2020;8(12):1201–8. This prospective observational study on COVID-19 patients reports that there are clinical differences between classical ARDS and COVID-19-associated ARDS.
Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201(10):1299–300.
Hue S, Beldi-Ferchiou A, Bendib I, Surenaud M, Fourati S, Frapard T, et al. Uncontrolled innate and impaired adaptive immune responses in patients with COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;202(11):1509–19.
Matthay MA, Leligdowicz A, Liu KD. Biological mechanisms of COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;202(11):1489–91.
Cruz FF, Weiss DJ, Rocco PR. Prospects and progress in cell therapy for acute respiratory distress syndrome. Expert Opin Biol Ther. 2016;16(11):1353–60.
Walter J, Ware LB, Matthay MA. Mesenchymal stem cells: mechanisms of potential therapeutic benefit in ARDS and sepsis. Lancet Respir Med. 2014;2(12):1016–26.
•• Tan Y, Wang Y, Souza-Moreira L, Wang C, Murray ABP, Salkhordeh M, et al. Mesenchymal stem cells induce dynamic immunomodulation of airway and systemic immune cells in vivo but do not improve survival for mice with H1N1 virus-induced acute lung injury. Front Bioeng Biotechnol. 2023;11:1203387. In this study, they demonstrate that MSC-based treatment has no survival benefit in influenza A virus-induced lung injury.
Gotts JE, Abbott J, Matthay MA. Influenza causes prolonged disruption of the alveolar-capillary barrier in mice unresponsive to mesenchymal stem cell therapy. Am J Physiol Lung Cell Mol Physiol. 2014;307(5):L395-406.
Darwish I, Banner D, Mubareka S, Kim H, Besla R, Kelvin DJ, et al. Mesenchymal stromal (stem) cell therapy fails to improve outcomes in experimental severe influenza. PLoS ONE. 2013;8(8): e71761.
Qin A, Wang XJ, Fu J, Shen A, Huang X, Chen Z, et al. hMSCs treatment attenuates murine herpesvirus-68 (MHV-68) pneumonia through altering innate immune response via ROS/NLRP3 signaling pathway. Mol Biomed. 2023;4(1):27.
Chan MC, Kuok DI, Leung CY, Hui KP, Valkenburg SA, Lau EH, et al. Human mesenchymal stromal cells reduce influenza A H5N1-associated acute lung injury in vitro and in vivo. Proc Natl Acad Sci U S A. 2016;113(13):3621–6.
•• Avanzini MA, Mura M, Percivalle E, Bastaroli F, Croce S, Valsecchi C, et al. Human mesenchymal stromal cells do not express ACE2 and TMPRSS2 and are not permissive to SARS-CoV-2 infection. Stem Cells Transl Med. 2021;10(4):636–42. In this study, they report that MSCs isolated from human tissues are not permissive to COVID-19 virus.
Simonson OE, Mougiakakos D, Heldring N, Bassi G, Johansson HJ, Dalen M, et al. In vivo effects of mesenchymal stromal cells in two patients with severe acute respiratory distress syndrome. Stem Cells Transl Med. 2016;5(6):845.
•• Bellingan G, Jacono F, Bannard-Smith J, Brealey D, Meyer N, Thickett D, et al. Safety and efficacy of multipotent adult progenitor cells in acute respiratory distress syndrome (MUST-ARDS): a multicentre, randomised, double-blind, placebo-controlled phase 1/2 trial. Intensive Care Med. 2022;48(1):36–4. In this phase 1/2 trial, it was demonstrated that intravenous multipotent adult progenitor cells given to patients with moderate-to-severe ARDS had a lower mortality rate at day 28 and day 365 compared to the placebo group.
Wick KD, Leligdowicz A, Zhuo H, Ware LB, Matthay MA. Mesenchymal stromal cells reduce evidence of lung injury in patients with ARDS. JCI Insight. 2021;6(12).
Rolandsson Enes S, Weiss DJ. Cell therapy for lung disease: current status and future prospects. Curr Stem Cell Rep. 2020;6:30–9.
Emanuele Rezoagli EJM, John Laffey,, O’Toole aD. The safety and efficiency of addressing ARDS using stem cell therapies in clinical trials. In: J. K. Burgess IHH, editor. Stem Cell-Based Therapy for Lung Disease. Switzerland: Springer Nature 2019. 219–38.
Dunbar H, Weiss DJ, Rolandsson Enes S, Laffey JG, English K. The inflammatory lung microenvironment; a key mediator in MSC licensing. Cells. 2021;10(11).
• Kirkham AM, Bailey AJM, Monaghan M, Shorr R, Lalu MM, Fergusson DA, et al. Updated living systematic review and meta-analysis of controlled trials of mesenchymal stromal cells to treat COVID-19: a framework for accelerated synthesis of trial evidence for Rapid Approval-FASTER Approval. Stem Cells Transl Med. 2022;11(7):675–87. This is a metastudy in which they compare the results from 11 clinical trials examining MSCs to treat COVID-19.
• Soetjahjo B, Malueka RG, Nurudhin A, Purwoko, Sumardi, Wisaksana R, et al. Effectiveness and safety of normoxic allogenic umbilical cord mesenchymal stem cells administered as adjunctive treatment in patients with severe COVID-19. Sci Rep. 2023;13(1):12520. Clinical trial investigating the safety and effectiveness of umbilical cord-derived MSCs as an adjunctive treatment for severe COVID-19. They reported no adverse effects and improved oxygenation profile in MSC group compared to control group.
• Zarrabi M, Shahrbaf MA, Nouri M, Shekari F, Hosseini SE, Hashemian SR, et al. Allogenic mesenchymal stromal cells and their extracellular vesicles in COVID-19 induced ARDS: a randomized controlled trial. Stem Cell Res Ther. 2023;14(1):169. In this clinical trial, they combined MSC treatment with extracellular vesicles in patients with COVID-19-associated ARDS.
Li TT, Zhang B, Fang H, Shi M, Yao WQ, Li Y, et al. Human mesenchymal stem cell therapy in severe COVID-19 patients: 2-year follow-up results of a randomized, double-blind, placebo-controlled trial. EBioMedicine. 2023;92: 104600.
Shi L, Yuan X, Yao W, Wang S, Zhang C, Zhang B, et al. Human mesenchymal stem cells treatment for severe COVID-19: 1-year follow-up results of a randomized, double-blind, placebo-controlled trial. EBioMedicine. 2022;75: 103789.
Chinnadurai R, Copland IB, Patel SR, Galipeau J. IDO-independent suppression of T cell effector function by IFN-gamma-licensed human mesenchymal stromal cells. J Immunol. 2014;192(4):1491–501.
Bustos ML, Huleihel L, Meyer EM, Donnenberg AD, Donnenberg VS, Sciurba JD, et al. Activation of human mesenchymal stem cells impacts their therapeutic abilities in lung injury by increasing interleukin (IL)-10 and IL-1RN levels. Stem Cells Transl Med. 2013;2(11):884–95.
Polchert D, Sobinsky J, Douglas G, Kidd M, Moadsiri A, Reina E, et al. IFN-gamma activation of mesenchymal stem cells for treatment and prevention of graft versus host disease. Eur J Immunol. 2008;38(6):1745–55.
Chinnadurai R, Bates PD, Kunugi KA, Nickel KP, DeWerd LA, Capitini CM, et al. Dichotomic potency of IFNgamma licensed allogeneic mesenchymal stromal cells in animal models of acute radiation syndrome and graft versus host disease. Front Immunol. 2021;12: 708950.
Rolandsson Enes S, Hampton TH, Barua J, McKenna DH, Dos Santos CC, Amiel E, et al. Healthy versus inflamed lung environments differentially affect mesenchymal stromal cells. Eur Respir J. 2021;58(4).
Abreu SC, Enes SR, Dearborn J, Goodwin M, Coffey A, Borg ZD, et al. Lung inflammatory environments differentially alter mesenchymal stromal cell behavior. Am J Physiol Lung Cell Mol Physiol. 2019.
Morrison TJ, Jackson MV, Cunningham EK, Kissenpfennig A, McAuley DF, O’Kane CM, et al. Mesenchymal stromal cells modulate macrophages in clinically relevant lung injury models by extracellular vesicle mitochondrial transfer. Am J Respir Crit Care Med. 2017;196(10):1275–86.
Abreu SC, Hampton TH, Hoffman E, Dearborn J, Ashare A, Singh Sidhu K, et al. Differential effects of the cystic fibrosis lung inflammatory environment on mesenchymal stromal cells. Am J Physiol Lung Cell Mol Physiol. 2020;319(6):L908–25.
Porter AP, Pirlot BM, Dyer K, Uwazie CC, Nguyen J, Turner C, et al. Conglomeration of T- and B-cell matrix responses determines the potency of human bone marrow mesenchymal stromal cells. Stem Cells. 2022;40(12):1134–48.
Jung JW, Kwon M, Choi JC, Shin JW, Park IW, Choi BW, et al. Familial occurrence of pulmonary embolism after intravenous, adipose tissue-derived stem cell therapy. Yonsei Med J. 2013;54(5):1293–6.
Wu Z, Zhang S, Zhou L, Cai J, Tan J, Gao X, et al. Thromboembolism induced by umbilical cord mesenchymal stem cell infusion: a report of two cases and literature review. Transplant Proc. 2017;49(7):1656–8.
Funding
Open access funding provided by Lund University. This work was supported by the Swedish Heart Lung Foundation, the Medical Faculty at Lund University, and the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
SRE and DJW conceived the design and concept, performed the literature search, and wrote the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weiss, D.J., Rolandsson Enes, S. MSC-Based Cell Therapy for COVID-19-Associated ARDS and Classical ARDS: Comparative Perspectives. Curr Stem Cell Rep (2023). https://doi.org/10.1007/s40778-023-00231-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s40778-023-00231-6