Abstract
Introduction
We evaluated the impact of gender on disease severity, health-related quality of life (HRQoL), treatment management, and patient–healthcare professional (HCP) interactions from the perspectives of patients with psoriatic arthritis (PsA).
Methods
Data were collected from a global online patient survey conducted by The Harris Poll (November 2, 2017 to March 12, 2018). Eligible patients were aged ≥ 18 years, with a self-reported diagnosis of PsA for > 1 year, had visited a rheumatologist/dermatologist in the past 12 months, and had reported previously using ≥ 1 conventional synthetic or biologic disease-modifying antirheumatic drug. Data were stratified by gender and analyzed descriptively, inferentially by binomial (chi-square) tests, and by multivariate logistic regression models.
Results
Data from 1286 patients who participated were included: 52% were female, 48% were male. Varying perceptions of disease severity between males and females were indicated by differences in symptoms leading to a diagnosis of PsA, and in symptoms reported despite treatment; more females than males reported joint tenderness, skin patches/plaques, and enthesitis. More females than males reported a major/moderate impact of PsA on their physical activity and emotional/mental well-being. Reasons for switching medication differed between genders, with more females switching because they perceived their medication to not be effective enough related to their joint symptoms. More females than males were very satisfied with their communication with their rheumatologist and were more likely to discuss the impact of PsA on their daily lives, their treatment satisfaction, and treatment goals with their rheumatologist.
Conclusions
Patients’ perceptions of the impact of PsA on HRQoL, treatment management, and interactions with HCPs varied between males and females. More females than males reported major/moderate physical and emotional impacts of PsA. When treating patients, it is important for HCPs to consider the potential impact of gender on patients’ experience of PsA and its symptoms.
Graphical plain language summary available for this article.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The prevalence of psoriatic arthritis (PsA) is equal for males and females, but there are differences between genders in the burden of the disease. |
Data on the differences of the burden of PsA between genders from a patient perspective are limited. |
We evaluated the impact of gender on disease severity, health-related quality of life, satisfaction with treatment, and patient–healthcare professional (HCP) interactions from the perspectives of patients with PsA. |
What was learned from the study? |
More females than males reported major/moderate physical and emotional impacts of PsA. |
More females than males were very satisfied with their communication with their rheumatologist and were more likely to discuss the impact of PsA, and their treatment satisfaction and goals, with their rheumatologist. |
Our analysis highlights the importance for HCPs of considering a patient’s gender and how it might impact their experience of PsA. |
Digital Features
This article is published with digital features, including graphical plain language summary, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.25639593.
Introduction
Psoriatic arthritis (PsA) is a chronic inflammatory disease, characterized by psoriatic skin and nail lesions, peripheral arthritis, spondylitis, dactylitis, and enthesitis [1]. The estimated global prevalence of PsA is 0.02–0.25% in the general population and has been reported to be approximately 30% in patients with psoriasis [2, 3].
Patients with PsA experience physical dysfunction and impaired health-related quality of life (HRQoL) [4]. Furthermore, comorbidities, such as hypertension, obesity, hyperlipidemia, and type 2 diabetes mellitus are associated with PsA [5]. Of note, although the prevalence of PsA is equal in males and females [6], differences in disease burden have been observed between genders/sexes in studies of patients with PsA. Females are more likely to experience more severe disease activity, higher levels of musculoskeletal symptoms, a greater impact of PsA on their life, and are less likely to achieve minimal disease activity, compared with males [7,8,9,10]. Males are more likely to develop radiographic joint damage and have more severe psoriasis than females [9, 10].
A global online survey conducted to understand the impact of PsA on daily life from the perspective of the patient reported that while nearly all (99%) patients took prescription medication for their PsA, most still experienced musculoskeletal and skin/nail symptoms [11]. Moreover, despite treatment, patients reported that PsA impacted their physical functioning and ability to perform certain activities, as well as substantially affecting social, emotional, and work-related aspects of their lives [11].
Given the findings of previous studies suggesting differences in disease burden between females and males with PsA, we carried out an analysis of data from a global survey to further evaluate the impact of gender on patient demographics and disease characteristics, perceptions of disease severity and HRQoL, treatment management, and patient–healthcare professional (HCP) interactions from a patient’s perspective.
Methods
Survey Design and Patients
An online survey was conducted by The Harris Poll, on behalf of Pfizer Inc, between November 2, 2017 and March 12, 2018 in eight countries (Australia, Brazil, Canada, France, Spain, Taiwan, the United Kingdom, and the United States) [11]. Full details of the survey methodology have been reported previously [11]. Briefly, eligible patients, recruited from online market research panels, were aged ≥ 18 years, with a self-reported diagnosis of PsA for > 1 year prior to participation in the survey, had visited a rheumatologist or dermatologist in the past 12 months, and had reported previously ever using ≥ 1 conventional synthetic or biologic disease-modifying antirheumatic drug (DMARD) for PsA.
Analysis of Survey Data
This analysis utilized survey data from patients with PsA relating to demographics and disease characteristics, perceptions of disease severity, HRQoL (including social and work life), treatment satisfaction, and HCP interactions with patients (including communication satisfaction and discussion topics raised).
Patient responses were stratified by gender and analyzed descriptively, and also inferentially by binomial (chi-square) tests [11, 12]. All percentages and binomial tests were calculated and analyzed based on weighted global data [13], which adjusted for the relative size of each country’s adult population within the total adult population of all eight countries. Relative differences between genders were measured using multivariate logistic regression models based on unweighted data. Odds ratios (ORs) and 95% confidence intervals (CIs) were determined, and results were adjusted for the following covariates (as potential confounders): age, country, current PsA medication (biologic DMARD), diagnosed conditions (comorbid arthritis/anxiety/depression), education level (low/high), employment status (not available for Brazil and Taiwan), income (low/medium/high; not available for Brazil and Taiwan), marital status, PsA medication ever taken (steroids), and time since PsA diagnosis. Differences were considered to be statistically significant if p < 0.05; only statistically significant differences are presented for ORs.
Ethical Approval
All patients provided informed consent before participating in the survey. As this was a non-interventional survey and personal data from the surveys were not identifiable, ethical approval was not required.
Results
Patients
This analysis included data from 1286 patients who participated in the survey and met eligibility criteria. Of these, 674 (52%) were female and 612 (48%) were male. Patient demographics and disease characteristics were generally similar for females and males, with some exceptions (Table 1). Females had a longer time between symptoms and diagnosis, compared with males (mean [standard deviation]: 5.2 [9.8] vs. 3.4 [7.2], respectively, p < 0.05; Table 1). A greater proportion of females than males were from the United States (47 vs. 33%, respectively, p < 0.05). More females than males reported having ever taken a steroid (57 vs. 43%, p < 0.05) and another prescription medication for PsA (12 vs. 8%, p < 0.05), other than a biologic, DMARD, non-steroidal anti-inflammatory drug (NSAID), or steroid (Table 1). More females than males were currently taking a biologic DMARD and oral conventional synthetic or targeted synthetic DMARD (20 vs. 15%, respectively, p < 0.05; Table 1). In addition, a greater proportion of females vs. males had ever been diagnosed with other conditions, including anxiety (32 vs. 24%, respectively), depression (27 vs. 19%), and osteoarthritis (17 vs. 9%; all p < 0.05).
Patient-Reported Symptoms Related to PsA
For both females and males, starting to experience pain (62 and 61%, respectively) was the most commonly reported reason for visiting an HCP that led to a diagnosis of PsA. More females than males reported experiencing musculoskeletal symptoms (59 vs. 42%, p < 0.05) or stiffness (48 vs. 39%, p < 0.05) and having to cover up their skin when around others (31 vs. 23%, p < 0.05), as reasons for visiting an HCP that led to a diagnosis of PsA. In contrast, more males than females stated difficulty participating in sports or recreational activities (33 vs. 26%, p < 0.05) as a reason for visiting an HCP that led to a diagnosis of PsA (Fig. 1).
Patient-reported reasons for visiting an HCP that led to a PsA diagnosis, with ORs and relative differences for males vs. females. Percentages are based on weighted data (adjusted for size of each country’s adult population); data reported are in response to the question: ‘What caused you to visit a healthcare profession that ultimately led to your PsA diagnosis? Please select all that apply’. ORs (adjusted for confounders) and relative differences (defined as OR minus 1) are based on unweighted data and are only reported for responses determined to be statistically significant by multivariate logistic regression models. *p < 0.05 for males vs. females without adjustment for confounders; ††p < 0.01, †††p < 0.001 for males vs. females with adjustment for confounders (ORs). CI confidence interval, HCP healthcare professional, N number of patients who answered the question (weighted), OR odds ratio, PsA psoriatic arthritis
Compared with females, males were 45.9% (OR 0.54 [95% CI 0.43–0.68]) and 29.2% (OR 0.71 [95% CI 0.55–0.91]) less likely to report experiencing musculoskeletal symptoms and having to cover up skin when around others, respectively, as reasons for visiting an HCP that led to a diagnosis of PsA. In contrast, males were 43.0% more likely than females (OR 1.43 [95% CI 1.12–1.83]) to report difficulty participating in sports or recreational activities as a reason for visiting an HCP that led to a diagnosis of PsA (Fig. 1).
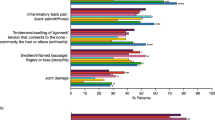
Both females and males stated that they experienced a range of PsA-related symptoms in the 12 months prior to their participation in the survey (Fig. 2a). The most commonly reported musculoskeletal symptom in both females and males was joint pain (80 and 77%, respectively). Generally, more females than males reported that they experienced musculoskeletal symptoms, such as joint swelling, joint tenderness, stiffness, inflammatory back pain/stiffness, tenderness or swelling of the ligaments/tendons that connect to bones (commonly the heel or elbow) and swollen or inflamed (“sausage”) fingers or toes (all p < 0.05). The most frequent skin/nail symptoms for both genders were skin patches/plaques, which were experienced by a greater proportion of females than males (63 vs. 53%, respectively), as were skin discomfort and nail changes (all p < 0.05). In addition, unusual fatigue was reported by 56% of females vs. 48% of males (p < 0.05; Fig. 2a).
Patient-reported symptoms related to PsA a experienced in the 12 months prior to participation in the survey and b experienced despite PsA treatment, with ORs and relative differences for males vs. females. Percentages are based on weighted data (adjusted for size of each country’s adult population); a Data reported are in response to the question: ‘Which of the following symptoms, if any, have you experienced in the past 12 months related to psoriatic arthritis? Please select all that apply’; b Data reported are in response to the question: ‘Which of the following symptoms do you still experience despite psoriatic arthritis treatment? Please select all that apply. I still experience…’. ORs (adjusted for confounders) and relative differences (defined as OR minus 1) are based on unweighted data and are only reported for responses determined to be statistically significant by multivariate logistic regression models. *p < 0.05 for males vs. females without adjustment for confounders; †p < 0.05 for males vs. females with adjustment for confounders (ORs). CI confidence interval, N for a number of patients who answered the question (weighted) and for b, number of patients who were taking Rx medications for their psoriatic arthritis, who answered the question (weighted), Net the net percentages of the individual responses for the musculoskeletal and skin/nail symptoms categories, OR odds ratio, PsA psoriatic arthritis, Rx doctor’s prescription
Overall, most (91% of females and males) patients taking medication at the time of the survey responded that, despite treatment for PsA, they still experienced symptoms; most symptoms were experienced by a similar proportion of females and males (Fig. 2b). Despite treatment, the most common musculoskeletal symptom in both females and males was joint pain (54 and 51%, respectively). The most common skin/nail symptoms in both genders were skin patches or plaques and they were also experienced by more females vs. males (43 vs. 36%, respectively, p < 0.05). More females than males experienced joint tenderness (43 vs. 36%, respectively, p < 0.05) and similarly, despite treatment, enthesitis was still experienced by 30% of females, compared with 24% of males (p < 0.05; Fig. 2b). Compared with females, males were 35.0% more likely (OR 1.35 [95% CI 1.01–1.81]) to report experiencing joint damage despite PsA treatment (Fig. 2b).
Patients’ Perceptions and Concerns of the Impact of PsA
For patients of both genders, the most commonly reported aspect of their lives that PsA had a major or moderate negative impact on was the level of physical activity, which was reported by a greater proportion of females vs. males (81 vs. 75%, respectively, p < 0.05). In addition, a major or moderate negative impact on their emotional/mental well-being was reported by more females than males (73 vs. 65%, respectively, p < 0.05; Fig. 3a).
Patient-reported perceptions on a major/moderate negative impact of PsA on aspects of life, b social impact and work impact of PsA, and c patient-reported concerns about the impact of PsA, with ORs and relative differences for males vs. females. Percentages are based on weighted data (adjusted for size of each country’s adult population); a Data reported are a summary of major/moderate life impact of PsA in response to the question: ‘How much of a negative impact if any, has psoriatic arthritis had on each of the following aspects of your life?’ (data not shown for no/slight impact). b Data reported are in response to the question: ‘Have you done any of the following as a result of psoriatic arthritis? Please select all that apply’; c Data reported are in response to the question: ‘What do you worry about the most because of psoriatic arthritis? Please select all that apply’. ORs (adjusted for confounders) and relative differences (defined as OR minus 1) are based on unweighted data and are only reported for responses determined to be statistically significant by multivariate logistic regression models. *p < 0.05 for males vs. females without adjustment for confounders; †††p < 0.001 for males vs. females with adjustment for confounders (ORs). ‡Not shown in United Kingdom; §Only shown in United Kingdom. CI confidence interval, N number of patients who answered the question (weighted), OR odds ratio, PsA psoriatic arthritis
Compared with females, males were 37.9% less likely (OR 0.62 [95% CI 0.49–0.78]) to report an impact to their emotional/mental well-being as an aspect of their lives that PsA had a major or moderate negative impact on (Fig. 3a). The impact of PsA on other aspects of patients’ lives, including education, ability to perform and progress at work, and relationships with family, friends, and romantic partners, was similar between genders (Fig. 3a).
To further explore the impact of PsA, patients were asked about their perceptions of the impact of PsA on their social and work lives. A similar proportion of females and males reported that they stopped participating in sports or recreational activities (56 vs. 55%, respectively) and experienced social shame (34 vs. 31%; Fig. 3b). However, more females than males experienced emotional distress (65 vs. 50%, respectively, p < 0.05) and stopped participating in social activities (49 vs. 41%, p < 0.05; Fig. 3b). Relating to impact of PsA on work life, more females than males went on permanent disability (14 vs. 9%, respectively, p < 0.05), whereas fewer females vs. males reported lower work productivity due to PsA (38 vs. 47%, p < 0.05; Fig. 3b). A similar proportion of females and males took a sick day (47 vs. 51%, respectively), medical leave (32 vs. 36%), quit or were let go from their jobs (14 vs. 11%), or switched jobs because of PsA (11 vs. 13%; Fig. 3b). When asked what they worry about most because of their PsA, more females than males expressed concern that their life expectancy may be shortened by PsA and/or other health conditions that typically accompany PsA (36 vs. 27%, respectively, p < 0.05), whereas more males than females were concerned that PsA would affect their ability to work (42 vs. 31%, respectively, p < 0.05; Fig. 3c).
Treatment Management
Patients who responded that they had goals for managing PsA were asked which of their goals were most important to them. More females than males answered that putting PsA into remission was most important (21 vs. 16%, respectively, p < 0.05), whereas for more males than females, increasing their levels of physical activity (7 vs. 4%, respectively, p < 0.05), reducing stiffness (5 vs. 2%, p < 0.05), and switching from injections or infusions to oral medications (3 vs. 1%, p < 0.05) were most important (Fig. 4a).
a Most important goal for managing PsA, b reasons for switching PsA medication, and c most desired changes to PsA medication, with ORs and relative differences for males vs. females. Percentages are based on weighted data (adjusted for size of each country’s adult population); a Data reported are in response to the question: ‘You mentioned that you have goals related to managing psoriatic arthritis. Which of these goals is most important to you right now?’; b Data reported are in response to the question: ‘Thinking of the most recent time you switched your psoriatic arthritis medication(s), which of the following, if any, are reasons why you switched? Please select all that apply’; c) Data reported are in response to the question: ‘Ideally, what would you most like to change, if anything, about your current prescription medication(s)? Please select all that apply’. ORs (adjusted for confounders) and relative differences (defined as OR minus 1) are based on unweighted data and are only reported for responses determined to be statistically significant by multivariate logistic regression models. *p < 0.05 for males vs. females without adjustment for confounders; †p < 0.05, ††p < 0.01, †††p < 0.001 for males vs. females with adjustment for confounders (ORs); ‡Not shown in the United Kingdom; §Only shown in the United Kingdom. CI confidence interval, N number of patients who a had goals for managing PsA, b switched medications in the past 2 years, c were currently taking prescription medications for PsA, who answered the question (weighted), Net the net percentages of the individual responses for patients’ most desired changes to their PsA medication categories, OR odds ratio, PsA psoriatic arthritis
For goals related to managing PsA, males were 37.8% (OR 0.62 [95% CI 0.49–0.79]) and 28.3% (OR 0.72 [95% CI 0.57–0.90]) less likely to report putting PsA into remission and improving their emotional well-being, respectively, compared with females. Similarly, males were 27.5% (OR 0.73 [95% CI 0.57–0.92]) and 21.8% (OR 0.78 [95% CI 0.61–1.00]) less likely than females to report preventing disability and reduction of general swelling or dactylitis, respectively, as goals related to managing PsA (Fig. 4a).
Overall, 37% of patients reported that they switched their PsA medication in the 2 years prior to participating in the survey, with females less likely to switch (34%) vs. males (41%). Of these patients, more females than males reported that switching PsA treatment was due to joint symptoms not improving or getting worse (41 vs. 28%, respectively, p < 0.05) and side effects being difficult to manage (35 vs. 22%, p < 0.05; Fig. 4b). By contrast, more males than females reported switching medication due to potential serious side effect concerns (29 vs. 16%, respectively), symptoms being under control (18 vs. 9%), because the medication interrupted their daily routine (16 vs. 8%), or because they did not like taking pills (15 vs. 5%) (all p < 0.05; Fig. 4b).
Males were 86.5% (OR 1.87 [95% CI 1.18–2.95]), 81.1% (OR 1.81 [95% CI 1.13–2.91]) and 104.5% (OR 2.05 [95% CI 1.16–3.60]) more likely than females to report concerns about potential serious effects, dactylitis not improving or getting worse, and not liking needles or injections, respectively, as reasons for switching PsA medication. Additionally, compared with females, males were 104.8% (OR 2.05 [95% CI 1.18–3.56]), 273.9% (OR 3.74 [95% CI 1.75–7.98]) and 435.6% (OR 5.36 [95% CI 1.86–15.43]) more likely to report their symptoms being under control, not liking taking pills and needing surgery as reasons for switching PsA medication (Fig. 4b).
Of patients taking medication for PsA at the time of the survey, more females than males reported that the change they most wanted from their PsA prescription medication was better relief of musculoskeletal symptoms (43 vs. 35%, respectively, p < 0.05), and more males than females most wanted to change how often they had to take their medication (37 vs. 28%, respectively, p < 0.05; Fig. 4c).
Satisfaction with HCP Communication
When asked about their satisfaction with the communication they had with their HCPs (rheumatologist or dermatologist) that they had seen during the 12 months prior to the survey, most patients (88% for dermatologist and 89% for rheumatologist) were ‘very’ or ‘somewhat’ satisfied. More females than males (60 vs. 51%, respectively, p < 0.05) were ‘very satisfied’ with the communication with their rheumatologist, whereas fewer females than males were ‘somewhat satisfied’ (28 vs. 39%, p < 0.05; Fig. 5a). For patients who had seen a dermatologist in the previous 12 months, there were no differences between males and females in terms of their satisfaction in their communication with their dermatologist (Fig. 5b).
Patients’ satisfaction with their communication with their a rheumatologist and b dermatologist. Percentages are based on weighted data (adjusted for size of each country’s adult population); a Data reported are in response to the question: ‘How satisfied are you with the communication you currently have with your healthcare professionals regarding psoriatic arthritis? 1. Rheumatologist’; b Data reported are in response to the question: ‘How satisfied are you with the communication you currently have with your healthcare professionals regarding psoriatic arthritis? 2. Dermatologist’; *p < 0.05 for females vs. males. N number of patients who had seen a a rheumatologist or b a dermatologist in the past 12 months, who answered the question (weighted)
The most common topic that females discussed with their rheumatologist and dermatologist, was treatment goals (83 and 80%, respectively), whereas males most frequently discussed their overall health (80 and 75%; Fig. 6a, b). More females than males discussed treatment goals (83 vs. 78%, respectively, p < 0.05), the impact of PsA on their ability to conduct daily activities (82 vs. 73%, p < 0.05), and response to and/or satisfaction with their treatment regimen (81 vs. 72%, p < 0.05) with their rheumatologist (Fig. 6a). Treatment goals was the only topic that more females than males (80 vs. 72%, respectively, p < 0.05) discussed with their dermatologist (Fig. 6b).
Patients’ topics of discussion with their a rheumatologist and b dermatologist, with ORs and relative differences for males vs. females. Percentages are based on weighted data (adjusted for size of each country’s adult population); a Data reported are ‘yes’ responses to the question: ‘In the last 12 months, have you discussed/conducted each of the following with your rheumatologist regarding psoriatic arthritis?’; b Data reported are ‘yes’ responses to the question: ‘In the last 12 months, have you discussed/conducted each of the following with your dermatologist regarding psoriatic arthritis?’. ORs (adjusted for confounders) and relative differences (defined as OR minus 1) are based on unweighted data and are only reported for responses determined to be statistically significant by multivariate logistic regression models. *p < 0.05 for males vs. females without adjustment for confounders; †p < 0.05, ††p < 0.01 for males vs. females with adjustment for confounders (ORs); ‡Including how my current medication may help reach my treatment goals; §Including diet, exercise, and/or natural remedies. CI confidence interval, N number of patients who had seen a a rheumatologist or b a dermatologist in the past 12 months, who answered the question (weighted), OR odds ratio
Compared with females, males were less likely to discuss treatment goals, impact on ability to conduct daily activities and response to and/or satisfaction with treatment regimen with their rheumatologist; for instance, 39.7% (OR 1.40 [95% CI 1.04–1.87]), 40.5% (OR 1.41 [95% CI 1.06–1.86]) and 62.0% (OR 1.62 [95% CI 1.22–2.15]) of males, respectively, were more likely to say they did not discuss these topics with their rheumatologist (Fig. 6a).
Discussion
Although the prevalence of PsA is similar in males and females, the burden of disease is known to differ between genders/sexes [6,7,8, 10]. However, studies describing gender differences in the burden of PsA from patients’ perspectives are limited. In this analysis of data from a global survey of patients with PsA, variations between genders were observed not only for patients’ perceptions of disease severity and the impact of PsA on patient HRQoL, but also in patient satisfaction with treatment and interactions with HCPs. Biological factors, such as sex hormones and genetic mechanisms, environmental factors, and differences in patient-reported perceptions of pain may all play a role in gender/sex differences in patients’ experience of PsA [14]. Indeed, rates of fibromyalgia, a central sensitization phenomenon, are higher in females than males with PsA, which may conflate patient-reported outcomes of PsA disease, such as pain [15]. This is supported by results from randomized controlled trials and an observational study that have shown that females tend to have more severe “pain-sensitive” PsA disease characteristics than males (e.g., higher tender joint counts and tender entheseal counts) [7, 16].
In this analysis, patient demographics and disease characteristics were generally similar between the genders; however, a greater proportion of females than males had been previously diagnosed with other conditions (such as anxiety, depression, and osteoarthritis), had ever taken steroids or prescription medications other than biologics, DMARDs, NSAIDs, or steroids for PsA, and were currently taking biologic/oral DMARDS. These data are consistent with the greater burden of PsA experienced by females than by males [6,7,8, 10]. Interestingly, an impact of gender on time to diagnosis of PsA was observed in this analysis; females reported a significantly greater delay in being diagnosed than males, with the time between symptoms and diagnosis being on average 5.2 years for females vs. 3.4 years for males. This is consistent with findings from a population-based study showing that female patients require more visits for musculoskeletal reasons to rheumatologists before a diagnosis of PsA is confirmed [17]; this may be due to misunderstanding of more subjective symptoms such as pain [18], potentially delaying diagnosis. It has previously been shown that a PsA diagnosis delay may contribute to poorer radiographic outcomes and physical function [19,20,21], which, given the greater delays in diagnosis in this study, could impact females to a greater extent than males.
As reasons for visiting an HCP leading to their diagnosis, different symptoms of PsA were more commonly reported by females and males, which could reflect varying perceptions in disease severity. Furthermore, greater proportions of females than males stated specific symptoms they had experienced, whereas males focused more on their difficulty participating in activities. Overall, in the 12 months prior to participating in the study, females and males experienced similar symptoms of PsA, but there were certain symptoms that were reported by a greater proportion of females than males. Specifically, despite treatment, most patients continued to experience symptoms, with more females than males reporting joint tenderness, skin patches/plaques, and enthesitis. These findings are consistent with studies showing that enthesitis was worse in females than males, as were tender joint counts [6, 7]. However, some studies demonstrated that both tender joint counts and swollen joint counts were comparable between sexes [6, 7]. Interestingly, after adjustment for confounding factors (particularly country and steroid use), males were more likely than females to report experiencing joint damage despite PsA treatment. While outcomes such as tender joint counts and enthesis are typically objectively assessed by a physician, it should be noted that, as this was a patient survey, all symptoms, including joint damage, were self-reported. Nevertheless, gender differences in reported symptoms may inform physicians in their clinical assessment of disease through bespoke disease investigation and subsequent decision-making.
This analysis found that females were more likely to report a major/moderate impact of PsA on their level of physical activity and emotional/mental well-being than males. Furthermore, females were more likely to experience a negative impact of PsA on aspects of their social life and to go on permanent disability from work, than males. These findings are aligned with those from other studies, in which females experienced lower functional capacity/physical functioning and lower HRQoL compared with males with PsA [6, 8, 10, 22]. A real-world study in PsA showed a greater level of impairment of activity related to work as well as life impact for females, compared with males [22]. There were also differences between genders regarding what they were most concerned about because of their PsA, with more females being worried about a negative impact on their life expectancy and males being more worried about PsA affecting their ability to work. These results support that together with disease activity measures, life impacts of PsA should be carefully considered when implementing disease management strategies, where decision-making should be aligned with patient preferences.
The patient-reported goals relating to PsA management were all regarding what their disease management could help them achieve, or the convenience of taking their medication. Although a similar proportion of females and males reported preventing disability and reduction of general swelling as goals for managing PsA, after adjustment for confounding factors (particularly biologic DMARD/steroid use and arthritis diagnosis), males were less likely than females to report these as goals. As most patients in this analysis continued to experience symptoms despite receiving treatment for PsA, it is understandable that some patients sought to switch their medication. Interestingly, females were less likely to report switching medication than males, and certain specific reasons for switching were more commonly reported by females and males. This finding is in contrast to real-world registry data, showing lower persistence on biologic DMARDs in female vs. male patients with PsA [23, 24]. More females than males switched their medication because they thought that it was not being effective enough at improving their joint symptoms, or that the side effects were difficult to manage. The change that more females than males wanted the most from their medication was better relief of musculoskeletal symptoms. More males than females reported switching medication due to concerns surrounding the impact of taking the medication on their daily routine, and males most wanted to change how often they had to take their medication. In a post hoc analysis of real-world data assessing the effectiveness of biologic medication for PsA, females switched their biologic medication more frequently than males, and were less satisfied with treatment than males [25].
To optimize PsA treatment outcomes, effective communication and shared decision-making between patients and HCPs is key [26, 27]. There can be misalignment between patients’ perspectives of their PsA disease activity and satisfaction with control of the disease, and the perspectives of their HCPs [28, 29]. Misalignment in patient-HCP satisfaction regarding control of PsA has been shown to contribute to a greater negative life impact of PsA for patients, compared with patients whose perception is aligned with that of their HCP [29]. Furthermore, a previous analysis using data from the global survey found that, although most patients were satisfied with communication with their HCP, those who had suboptimal communication were more likely to experience negative impacts of PsA [26]. Consistent with this, in our analysis, the majority of patients were ‘very/somewhat satisfied’ with their communication with their rheumatologist and dermatologist; however, more females than males reported being very satisfied with their communication with their rheumatologist. Females were also more likely to discuss how PsA impacted their daily lives and their treatment satisfaction and goals with their HCPs than males, indicating that they may be more comfortable interacting with their HCP, or more motivated to optimize their treatment.
This analysis is subject to some limitations, which should be considered when interpreting the findings. The major limitation is the self-reported nature of the data obtained from the global survey, which relied on patients’ ability to understand the survey questions, accurately describe their PsA diagnosis, and correctly recall their symptoms and medications. Information on PsA disease features, such as joint damage, tender joints, swollen joints, enthesitis (defined in the survey as tenderness or swelling of the ligaments/tendons that connect to bones – commonly the heel or elbow), and dactylitis (defined in the survey as swollen or inflamed [“sausage”] fingers or toes) was self-reported and not verified by patient medical records or their physicians. A higher proportion of females than males had anxiety and depression, which may have impacted patient perception of pain-related outcomes and responses to therapy, and vice versa. However, the prevalence of chronic pain conditions (e.g., fibromyalgia) was not assessed. In addition, females may be more likely to report their symptoms than males, which may have influenced the results. The data were collected from an online survey, therefore, patients without access to the Internet or membership in online panels are not represented in the results. Furthermore, of the patients who were included in the analysis, 45% were from North America and 24% from Europe, which could prevent the generalizability of the results to other parts of the world.
Conclusions
This analysis of data from a global online survey suggests that the burden of PsA is greater for females than males, with more females reporting a major/moderate impact on their physical activity and emotional/mental well-being. There were also differences in the impact of PsA on the social and work lives of males and females. Of note, more females were very satisfied with their communication with their rheumatologist, and discussed treatment goals, the impact of PsA on their daily activities, and their response to/satisfaction with their treatment. Together, these data highlight the importance of considering how patients' gender impacts their experience with PsA when treating them.
Data Availability
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
References
Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376:957–70.
Mease PJ, Gladman DD, Papp KA, et al. Prevalence of rheumatologist-diagnosed psoriatic arthritis in patients with psoriasis in European/North American dermatology clinics. J Am Acad Dermatol. 2013;69:729–35.
Ogdie A, Weiss P. The epidemiology of psoriatic arthritis. Rheum Dis Clin North Am. 2015;41:545–68.
Taylor WJ. Impact of psoriatic arthritis on the patient: through the lens of the WHO international classification of functioning, health, and disability. Curr Rheumatol Rep. 2012;14:369–74.
Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken). 2011;63:1729–35.
Passia E, Vis M, Coates LC, et al. Sex-specific differences and how to handle them in early psoriatic arthritis. Arthritis Res Ther. 2022;24:22.
Orbai A-M, Perin J, Gorlier C, et al. Determinants of patient-reported psoriatic arthritis impact of disease: an analysis of the association with sex in 458 patients from fourteen countries. Arthritis Care Res (Hoboken). 2020;72:1772–9.
Duruoz MT, Gezer HH, Nas K, et al. Gender-related differences in disease activity and clinical features in patients with peripheral psoriatic arthritis: a multi-center study. Joint Bone Spine. 2021;88: 105177.
Coates LC, van der Horst-Bruinsma IE, Lubrano E, et al. Sex-specific differences in patients with psoriatic arthritis: a systematic review. J Rheumatol. 2023;50:488–96.
Eder L, Thavaneswaran A, Chandran V, Gladman DD. Gender difference in disease expression, radiographic damage and disability among patients with psoriatic arthritis. Ann Rheum Dis. 2013;72:578–82.
Coates LC, Orbai A-M, Azevedo VF, et al. Results of a global, patient-based survey assessing the impact of psoriatic arthritis discussed in the context of the Psoriatic Arthritis Impact of Disease (PsAID) questionnaire. Health Qual Life Outcomes. 2020;18:173.
Rosner B. Fundamentals of biostatistics. 8th ed. Boston: Cengage Learning; 2015.
Kish L. Survey sampling. New York: John Wiley & Sons; 1965.
Eder L, Chandran V, Gladman DD. Gender-related differences in patients with psoriatic arthritis. Int J Clin Rheumatol. 2012;7:641–9.
Mease PJ. Fibromyalgia, a missed comorbidity in spondyloarthritis: prevalence and impact on assessment and treatment. Curr Opin Rheumatol. 2017;29:304–10.
Eder L, Gladman DD, Mease P, et al. Sex differences in the efficacy, safety and persistence of patients with psoriatic arthritis treated with tofacitinib: a post-hoc analysis of phase 3 trials and long-term extension. RMD Open. 2023;9: e002718.
Tarannum S, Widdifield J, Wu CF, Johnson SR, Rochon P, Eder L. Understanding sex-related differences in healthcare utilisation among patients with inflammatory arthritis: a population-based study. Ann Rheum Dis. 2023;82:283–91.
Zhang L, Losin EAR, Ashar YK, Koban L, Wager TD. Gender biases in estimation of others’ pain. J Pain. 2021;22:1048–59.
Haroon M, Gallagher P, FitzGerald O. Diagnostic delay of more than 6 months contributes to poor radiographic and functional outcome in psoriatic arthritis. Ann Rheum Dis. 2015;74:1045–50.
Tillett W, Jadon D, Shaddick G, et al. Smoking and delay to diagnosis are associated with poorer functional outcome in psoriatic arthritis. Ann Rheum Dis. 2013;72:1358–61.
Theander E, Husmark T, Alenius GM, et al. Early psoriatic arthritis: short symptom duration, male gender and preserved physical functioning at presentation predict favourable outcome at 5-year follow-up. Results from the Swedish Early Psoriatic Arthritis Register (SwePsA). Ann Rheum Dis. 2014;73:407–13.
Gossec L, Walsh JA, Michaud K, et al. Women with psoriatic arthritis experience higher disease burden than men: findings from a real-world survey in the United States and Europe. J Rheumatol. 2023;50:192–6.
Ribeiro da Silva MR, Ribeiro Dos Santos JB, Maciel Almeida A, et al. Medication persistence for psoriatic arthritis in a Brazilian real-world setting. Future Sci OA. 2019;5:FSO369.
Geale K, Lindberg I, Paulsson EC, et al. Persistence of biologic treatments in psoriatic arthritis: a population-based study in Sweden. Rheumatol Adv Pract. 2020;4: rkaa070.
Colombo D, Frassi M, Mariano GP, et al. The CHRONOS real-world evidence of biologic treatments in psoriatic arthritis in Italy: a post hoc gender analysis. Womens Health Rep (New Rochelle). 2022;3:162–71.
Coates LC, Azevedo VF, Cappelleri JC, et al. Exploring the quality of communication between patients with psoriatic arthritis and physicians: results of a global online survey. Rheumatol Ther. 2021;8:1741–58.
Gossec L, Baraliakos X, Kerschbaumer A, et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis. 2020;79:700–12.
Eder L, Thavaneswaran A, Chandran V, Cook R, Gladman DD. Factors explaining the discrepancy between physician and patient global assessment of joint and skin disease activity in psoriatic arthritis patients. Arthritis Care Res (Hoboken). 2015;67:264–72.
Furst DE, Tran M, Sullivan E, et al. Misalignment between physicians and patient satisfaction with psoriatic arthritis disease control. Clin Rheumatol. 2017;36:2045–54.
Acknowledgments
We thank the participants of the study. We would also like to thank Kathy Steinberg from the Harris Poll, USA, for their input into the manuscript.
Medical Writing, Editorial, and Other Assistance
Medical writing support, under the direction of the authors, was provided by Sharon Gill, PhD, and Lewis C Rodgers, PhD, CMC Connect, a division of IPG Health Medical Communications, and was funded by Pfizer, New York, NY, USA, in accordance with Good Publication Practice (GPP 2022) guidelines (Ann Intern Med. 2022;175:1298–304).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
This study was sponsored by Pfizer. Medical writing support and Rapid Service Fee were funded by Pfizer.
Author information
Authors and Affiliations
Contributions
Conceptualization of study and design: Lihi Eder, Pascal Richette, Valderilio F Azevedo, Joseph C Cappelleri, Megan Hoang and Jade Moser. Patient recruitment and data acquisition: Jade Moser. All authors were involved in the analysis of the data, drafting the article or revising it critically for important intellectual content, and all authors (Lihi Eder, Pascal Richette, Laura C Coates, Valderilio F Azevedo, Joseph C Cappelleri, Edward P Johnson, Megan Hoang, Jade Moser and Meriem Kessouri) approved the final version to be submitted for publication.
Corresponding author
Ethics declarations
Conflict of Interest
Lihi Eder has received research and educational grants from AbbVie, Eli Lilly, Fresenius Kabi, Janssen, Novartis, Pfizer Inc, Sandoz, and UCB, and has received consulting fees from AbbVie, Bristol Myers Squibb, Eli Lilly, Janssen, Novartis, Pfizer Inc, and UCB. Pascal Richette has received consulting fees from AbbVie, Celgene, Eli Lilly, Janssen, MSD, Novartis, Pfizer Inc, and UCB. Laura C Coates is an Editorial Board member of Rheumatology and Therapy. Laura C Coates was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions. Laura C Coates has received research funding from AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Novartis, Pfizer Inc, and UCB, has received consulting fees from AbbVie, Amgen, Bristol Myers Squibb, Celgene, Eli Lilly, Gilead, Galapagos, Janssen, MoonLake, Novartis, Pfizer Inc, and UCB, and has received speaker fees from AbbVie, Amgen, Biogen, Celgene, Eli Lilly, Galapagos, Gilead, GSK, Janssen, Medac, Novartis, Pfizer Inc, and UCB. Valderilio F Azevedo has received research funding from AbbVie, Bristol Myers Squibb, Eli Lilly, Genentech, GSK, Pfizer Inc, and UCB, and has received consulting and speaker fees from AbbVie, Celltrion, Eli Lilly, Janssen, Pfizer Inc, and Roche. Joseph C Cappelleri and Meriem Kessouri are employees and shareholders of Pfizer Inc. Edward P Johnson and Jade Moser are employees of The Harris Poll, which was a paid contractor to Pfizer to conduct the initial research and related statistical analysis. Megan Hoang was an intern of Pfizer Inc at the time of the analysis.
Ethical Approval
All patients provided informed consent before participating in the survey. As this was a non-interventional survey and personal data from the surveys were not identifiable, ethical approval was not required.
Additional information
Prior presentation: Selected data in this manuscript were previously presented at the 23rd Annual Congress of the European Alliance of Associations for Rheumatology in 2023 held on May 31–June 3 as an oral presentation, and at the American College of Rheumatology Convergence in 2023 held on November 10–15 as a poster presentation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Eder, L., Richette, P., Coates, L.C. et al. Gender Differences in Perceptions of Psoriatic Arthritis Disease Impact, Management, and Physician Interactions: Results from a Global Patient Survey. Rheumatol Ther (2024). https://doi.org/10.1007/s40744-024-00678-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40744-024-00678-x