Abstract
Introduction
Gout is an inflammatory, metabolic disease associated with a high comorbidity burden including cardiovascular disease, hypertension, type 2 diabetes, hyperlipidemia, renal disease, and metabolic syndrome. Approximately 9.2 million Americans have gout, making prognosis and treatment outcome predictors highly important. About 600,000 Americans have early-onset gout (EOG), generally defined as first gout attack at ≤ 40 years of age. However, data on EOG clinical features, comorbidity profile, and treatment response are sparse; this systematic literature review provides insight.
Methods
PubMed and American College of Rheumatology (ACR)/European Alliance of the Associations for Rheumatology (EULAR) abstract archives were searched for early-onset gout, “early onset gout,” and (“gout” AND “age of onset”). Duplicate, foreign language, single case report, older (before 2016), and irrelevant/data insufficient publications were excluded. The age of diagnosis categorized patients as having common gout (CG, generally > 40 years) or EOG (generally ≤ 40 years). Applicable publications were extensively reviewed/discussed among authors for inclusion/exclusion consensus.
Results
A total of 283 publications were identified, with 46 (35 articles, 10 abstracts) reviewed and 17 (12 articles, 5 abstracts) ultimately included. Eleven reported clinical characteristics, with 6 EOG-CG retrospective/cross-sectional comparisons. Gout diagnosis preceded cardiometabolic comorbidity and renal comorbidities were less prevalent in EOG than CG patients. EOG patients had more severe disease (more gout flares, polyarticular disease), higher pre-therapy serum urate (SU), and worse oral urate-lowering therapy response. Genetics-focused publications reported higher incidences of dysfunctional urate transporter mutations in EOG patients.
Conclusions
This review suggests that EOG is more recalcitrant to urate-lowering therapy, is associated with urate transporter defects, and carries heavy disease burden. Therefore, early rheumatology referral and urate-lowering in a treat-to-target fashion may benefit EOG patients. Interestingly, EOG patients had fewer cardiometabolic comorbidities at diagnosis than CG patients, presenting a potential “window of opportunity” to attenuate cardiometabolic comorbidity development with SU control. Preventing gout-related suffering and health burden is particularly important in these young EOG patients who will live with gout and its sequelae for decades.
Plain Language Summary
Gout, an inflammatory arthritis caused by high urate levels in the blood (SU), is associated with medical issues, including heart disease, high blood pressure, type 2 diabetes, and kidney disease. Millions of Americans have gout, with some having early-onset gout (EOG), generally the first gout attack at or before 40 years of age. Little information on EOG has been published; this literature review provides insight. More recent articles and major rheumatology meeting presentations (2016 to August 2022) on EOG were reviewed. Publications that were duplicates, not in English, on a single patient, or were not relevant/did contain enough information were excluded. The age at gout diagnosis determined if patients had common gout (CG) or EOG. Of the 283 publications identified, 17 were included in this review. Gout-associated medical issues (heart, metabolic, and kidney-related) were less common in EOG than CG patients and occurred after gout diagnosis in EOG patients. Compared to CG patients, EOG patients more often had severe gout (more gout attacks and affected joints), higher SU, and worse response to oral SU-lowering medications. Genetics-focused publications showed that mutations affecting how urate is removed from the body are more common in EOG patients. Overall, the literature suggests that EOG may be difficult to treat, has a genetic component, and has a heavy disease burden. Therefore, early rheumatology referral and gout management may benefit EOG patients due to a potential “window of opportunity” where proper SU control may prevent gout-related suffering and health burden in young EOG patients who will live with gout and its consequences for decades.
Similar content being viewed by others
Why carry out this study? |
About 600,000 Americans have early-onset gout (EOG, generally the first gout attack at ≤ 40 years of age), but data on its clinical features, comorbidity profile, and treatment response are sparse. |
This systematic literature review was performed to examine EOG literature as a whole and provide some insight on these young patients who will live with gout for decades. |
What was learned from this study? |
A gout diagnosis frequently preceded the onset of cardiometabolic and renal comorbidities in EOG patients and these comorbidities were less prevalent at diagnosis than in their older common gout counterparts. |
EOG patients had more severe gout (more gout flares, polyarticular disease), higher pre-therapy serum urate, worse oral urate-lowering therapy response, and higher incidence of urate transporter genetic mutations than common gout patients. |
Early rheumatology referral and gout management may benefit EOG patients due to a potential “window of opportunity” where proper SU control may prevent gout-related suffering and health burden in young EOG patients who will live with gout and its consequences for decades. |
Introduction
Gout is the most common inflammatory arthritis in adults, affecting approximately 9.2 million adults in the United States [1] (prevalence of 3.9%) and 41.2 million adults worldwide [2]. The risk of gout increases with age [3], but an estimated 600,000–700,000 patients in the United States develop early-onset gout (EOG), generally thought of as first gout attack before the age of 40 years [1, 4]. Although the 2020 American College of Rheumatology (ACR) gout management guidelines [5] do not specifically make recommendations for managing EOG, both the European Alliance of Associations for Rheumatology (EULAR) [6] and British Society of Rheumatology [7] guidelines recommend rapid initiation of urate lowering therapy (ULT) in patients diagnosed with gout before the age of 40 years.
There is a clear relationship between gout and metabolic syndrome [8, 9], defined by the World Health Organization as the presence of insulin resistance (impaired glucose tolerance, impaired fasting glucose, or type 2 diabetes) with ≥ 2 of the following: obesity, dyslipidemia, hypertension, and microalbuminuria [10]. The prevalences of individual metabolic syndrome components have also been associated with gout and/or hyperuricemia, including hypertension [9, 11,12,13,14,15], insulin resistance/diabetes [15,16,17,18,19], obesity [9, 19, 20], and dyslipidemia [9, 21]. The high prevalence of metabolic syndrome and its components likely contribute to the higher risk of cardiovascular disease [15, 19, 22], events [19, 23,24,25], and mortality [26,27,28,29,30] in gout patients. Further, chronic inflammation secondary to monosodium urate (MSU) crystal deposition has been shown to increase cardiovascular risk [31,32,33,34,35]. Gout patients also have a higher risk of developing renal insufficiency and end-stage renal disease than their non-gout counterparts [12, 15, 36,37,38,39,40], particularly those with crystalluria [41].
Unfortunately, there is a paucity of data related to the clinical features, comorbidity profile, and treatment response of patients with EOG. Given that EOG patients will live with this progressive, painful, inflammatory arthritis for decades, and the gout-imposed risk of renal [19, 38, 42], cardiovascular [19, 23, 26, 43, 44], and cerebrovascular [19, 25] disease, EOG could have a major and lasting impact on long-term patient health. Further, compared to non-gouty populations, gout patients have decreased quality of life [45, 46], increased disability [2, 47], and higher rates of all-cause death [26, 28]. This systematic literature review was conducted to better understand and characterize patients with EOG.
Methods
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Literature Review
A systematic search was conducted using PubMed to identify full publications and the ACR and EULAR abstract archives to identify published abstracts that were not yet available in full manuscript form. Articles and abstracts focusing on EOG were identified using the following search terms: early onset gout, “early onset gout”, and “(gout AND age of onset).” All literature searches were performed in August 2022.
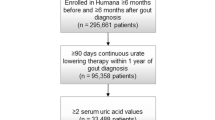
In an effort to review the most contemporary literature focusing on EOG, only publications from 2016–2022 were included. All publication titles were screened by two authors (AA, LPS) for possible inclusion in this literature review. Items possibly containing data of interest were thoroughly reviewed, and publications meeting any of the following criteria were excluded: not available in English, duplicate publication or data set (e.g., subset of a larger identified data set, meeting abstract of a full publication, literature review), single patient case report, or insufficient/irrelevant data. Publications satisfying inclusion/exclusion criteria were extensively reviewed and discussed by all authors. Unanimous consensus was reached regarding the final included publication list. The PRISMA flowchart showing literature identification is shown in the Fig. 1.
Data Analysis
Available data were collated using an Excel spreadsheet for qualitative and quantitative analysis. Studies of similar type (e.g., claims-based, medical record data) were separately examined to avoid potential confounding of results. Patient demographics, comorbidity burden, and gout characteristics were examined and compared between EOG and CG populations. Because this systematic literature review was exploratory in nature and meant to be hypothesis generating, statistical analyses were not performed. Continuous parameters are presented as means and categorical data are presented as n (%). In some publications, continuous data were presented as median (Q1, Q3). In these cases, the mean was estimated as (median + Q1 + Q3)/3, as has been shown to be appropriate for systematic literature reviews and meta-analyses [48].
Results
Literature Search
The literature search identified a total of 283 references (Fig. 1). After removing 66 duplicate publications, 1 review article, 16 single patient case reports, eight publications not available in English, and 147 categorized as inapplicable/lacking sufficient information, a total of 35 articles and ten abstracts were extensively reviewed for eligibility and discussed by the authors. Ultimately, 12 full-length publications and five abstracts were included in the final systematic review. Unanimous consensus among the authors to include all articles was reached. Of the 17 included publications, six focused on the genetic component of EOG [49,50,51,52,53,54], ten focused on the clinical aspects of EOG [55,56,57,58,59,60,61,62,63,64], and one had aspects of both [65]. Of the clinically focused publications, six were retrospective, cross-sectional comparisons between EOG and CG cohorts [57,58,59,60,61,62], three were prospective comparisons between EOG and CG patients [55, 56, 65], and two were claims-based analyses comparing EOG and CG populations [63, 64].
Clinical Characteristics of Early-Onset Gout and Common Gout Patients
Eleven publications made comparisons between patients with EOG and patients with CG, with patients deriving from France, China, Korea, Taiwan, and the United States. Six studies were retrospective in nature and examined existing data sets, three studies were prospective in nature and had accompanying dietary investigations, and two studies were insurance claims-based analyses. EOG was defined as gout diagnosis/first acute gout flare before the age of 40 years in seven studies and before the age of 30 years in four studies. Of the nine studies with medical record data, gout was defined using ACR/EULAR criteria in five [57, 58, 60, 61, 65].
Patient Characteristics
Mean patient age at first gout flare/gout diagnosis ranged from 23.5–32.8 years in EOG patients and 47.8–61.0 years in CG patients (Table 1). The proportion of male patients was high in both EOG (96.7–100%) and CG (71.0–97.3%) cohorts, but was consistently higher in EOG patients. However, a similar proportion of male patients was noted in one Chinese population (EOG: 98.7 vs. CG: 97.3%; Table 1) [65].
Comorbidity burden was consistently lower in patients with EOG than in those with CG. In studies with medical record data, hypertension, diabetes, hyperlipidemia/dyslipidemia, coronary artery disease, and chronic kidney disease (CKD) were all less prevalent in patients with EOG (Table 2). Of note, CKD prevalence was markedly lower in EOG patients across all studies, as reflected in available eGFR data. Average mean eGFR across studies was 93.4 ml/min/1.73 m2 in EOG cohorts and 74.2 ml/min/1.73 m2 in CG cohorts. The identified claims-based analysis that examined cardiometabolic and renal comorbidities showed lower cardiorenal comorbidity prevalence in EOG than CG patients in the United States, with lower rates of hypertension (34 vs. 77%), cardiovascular disease (% not provided), type 2 diabetes (13 vs. 39%), and CKD (5 vs. 20%) at the time of first gout diagnosis code [63]. Similar trends were observed here in studies with medical record data in US, Chinese, and French populations. Amatucci et al. [63] also showed that, in both EOG and CG patients, comorbidity prevalence at first gout diagnosis code was higher and comorbidity prevalence following gout diagnosis grew faster than in the general US population of similar age. Similar observations were made in a Chinese EOG cohort included in the current analysis for hypertension (EOG: 59.9% vs. Chinese population of similar age: 20.0%), diabetes (6.7 vs. 3.2%), and metabolic syndrome (31.7 vs. 6.1%) [65]. In contrast, obesity rates were higher in patients with EOG than in patients with CG, except in France where the rate was consistent between groups [59]. Mean body mass index was similar between EOG and CG populations, with the exception of the US, where BMI was higher in patients with CG.
The remaining claims-based study examined new-onset glaucoma risk in Taiwanese patients with and without gout. Gout patients who were 20–39 years of age had the highest risk of developing glaucoma among gout patients and compared to their non-gout counterparts [64].
Gout Characteristics
In eight of nine studies (88.9%) with medical record data, authors reported more severe disease in EOG patients than in CG patients [55, 57,58,59,60,61,62, 65]. This conclusion was based on SU at diagnosis, gout duration, and the proportion of patients with acute gout flare, polyarticular disease, tophi, and target SU with oral ULT therapy (Table 3). In EOG and CG patients, gout duration (EOG: 6.9 vs. CG: 6.5 years) and proportion of patients with tophi (29.9 vs. 30.5%) were similar. However, SU at baseline/diagnosis was higher in EOG patients in eight of nine studies (88.9%) and fewer patients achieved target SU with ULT (39.1 vs. 50.3%). One French study also noted that a significantly higher febuxostat dose was required in patients with EOG to achieve target SU (dosing information not provided) [62]. Further, rates of ULT use were higher in EOG than CG patients in the US study (87.0 vs. 67.9%) [57] and similar between EOG and CG patients in one French study (68.9 vs. 67.9%) [59]. In that same French cohort, ULT duration was also longer in EOG patients (11.3 vs. 6.6 years) [59].
Four of six studies (67%) with gout flare details indicated signs of more severe articular disease in patients with EOG. This included increased gout flare frequency, a higher proportion with ≥ 2 flares/year, and/or a higher proportion with polyarticular flares (one US, two French, one Chinese cohorts; Table 3) [57, 59, 62, 65]. In a Chinese cohort, patients with EOG also had a higher number of involved joints than their CG counterparts (5.2 vs. 3.8) [55]. Both studies that were not indicative of more severe articular disease reported on Chinese populations [55, 56]. Ankle/mid-foot involvement was noted in 63 vs. 48% of EOG vs. CG patients in a Chinese cohort [65], gout involvement outside of the 1st MTP joint was noted in 54 vs. 41% of EOG vs. CG patients in a French cohort [59], and first gout flare was noted in the foot/ankle (excluding the 1st MTP joint) in 31.5 vs. 20.0% of EOG vs. CG patients in the US cohort [57].
Genetics of Early-Onset Gout
Our systematic literature review identified six full-length publications and one abstract with novel and relevant information related to EOG genetics. Patient and/or gout characteristics were briefly described in the presence of urate-transporter (ABCG2) [49,50,51,52,53], solute carrier (SLC) [53, 54], or aldehyde dehydrogenase (ALDH) [53] mutations. Though these mutations are rare in the general population, nearly one-third of a small EOG cohort (7 of 26 patients [27%]) had a “probably pathogenic” ABCG2, SLC, or ALDH mutation [53]. Further, some identified clinical studies showed that EOG populations consistently had a family history of gout more often than CG populations (United States: 20.3 vs. 11.0% [N = 227, 100] [57]; France: 38.1 vs. 16.7% [N = 120, 865] [59], 60.6 vs. 24.6% [N = 39, 174] [62]; China: 37.0 vs. 32.6% [N = 387, 233] [56], 25.9 vs. 18.1% [N = 1700, 7277] [58], 42.0 vs. 30.6% [N = 69, 111] [61]).
ABCG2 Mutations
Zaidi et al. [49] examined three previously reported study populations, including those of the Genetics of Gout in Aotearoa study [66] (Aotearoa cohort; Eastern Polynesian, Western Polynesian, and New Zealand European ancestral origin subgroups), the Eurogout consortium [67] (Eurogout cohort, established by the European Crystal Network), and lesinurad clinical trials [68,69,70,71] (Ardea cohort). The ten loci most strongly associated with serum urate, as identified by Yang et al. [72], were examined in all cohorts. For their age at diagnosis groupings, the youngest tertile was diagnosed with gout at < 35 years of age and the oldest tertile was diagnosed with gout at > 50 years of age. The ABCG2 rs2231142 mutation was strongly associated with the development of gout before 35 years of age. Further, across all examined populations, patients with the ABGC2 mutation were more likely to be diagnosed with gout before 40 years of age (OR [95% CI]): 1.60 [1.41, 1.83]). The association remained significant in the Eastern Polynesian and New Zealand European ancestral origin subgroups. Regarding the remaining nine SNPs, though not statistically significant, the data suggest that several other mutations carry a higher adjusted OR for the development of gout before 35 years of age.
Zhang et al. [65] specifically examined ABCG2 protein function in a Chinese gout population, estimated using SNP sequencing of the two most common polymorphisms (rs2231142, rs72552713) and an established ABCG2 function prediction model [73]. A high prevalence of ABCG2 protein dysfunction was found in both EOG (79.5%, N = 449) and CG (86.4%, N = 329) patients, with a younger mean age of gout onset in those with the lowest ABCG2 function (full function: 37.1 years, three-quarters function: 36.7 years, one-half function: 38.0 years, one-quarter function: 30.4 years). Further, pediatric gout has been reported in patients with a strong family history of EOG that was linked to ABCG2 mutations [50, 51]. Together, these genetic findings strongly link pathogenic ABCG2 mutations and the development of EOG.
SLC and ALDH Mutations
Huang et al. [54] identified a two-generation pedigree with familial EOG. A father and son were affected by EOG, with both having a rare missense SLC16A9 mutation that was deemed to be “possibly pathogenic.” Protein function was not examined, but findings from older studies have shown an association between SLC16A9 mutations and serum urate levels [74, 75]. A mutation in SLC22A11 has also been reported in a patient with EOG [53]. Though different loci than the genetic anomalies described above, most SLC22A12 mutations have been shown to increase susceptibility to hyperuricemia [76].
One published case of an ALDH16A1 mutation in a patient with EOG was identified in the examined time period [53]. Though the ALDH16A1 protein is thought to be inactive, its proper interaction with hypoxanthine–guanine phosphoribosyltransferase (HPRT1), a key enzyme involved in the purine salvage pathway may be needed for optimal HPRT1 function [77]. Of note, although most genetic mutations result in impaired urate excretion, patients with an ALDH16A1 mutation likely have impaired purine salvage, which results in urate overproduction [78].
Discussion
This systematic literature review identified seven publications that explored the genetics of uncontrolled gout and 11 publications that compared the clinical characteristics of EOG and CG populations. Distinct and consistent differences were identified with respect to genetic predisposition to gout, gout severity, and overall patient health at gout diagnosis.
EOG patients had more severe and harder to treat disease than their CG counterparts, as noted by increased flare rates, polyarticular involvement, and/or hyperuricemia that was more recalcitrant to oral ULT. These findings were consistent across Chinese, French, Korean, and US populations and are supported by genetic studies, which suggest that renal urate transporter anomalies play a role in EOG development, particularly ABCG2 mutations that affect transporter function and subsequent urate excretion. Given that patients with EOG had overall higher SU and were less likely to achieve target SU levels during ULT use, genetic mutations associated with gout may make this population with genetically driven gout less responsive to xanthine oxidase inhibitors, which slow the production of urate but do not increase urate excretion. In fact, the presence of an ABCG2 loss-of-function polymorphism has been shown to predict poor SU-lowering response to allopurinol [79, 80], perhaps because, in addition to urate transport, allopurinol transport into the cell is also affected by such mutations [80].
EOG patients may provide important clues on the systemic extra-articular impacts of gout. Included publications consistently showed lower cardiometabolic and renal comorbidity in patients with EOG compared to those with CG; most notably, hypertension, diabetes, coronary artery disease, and CKD. It is known that initiating oral ULT that complies with ACR treatment guidelines leads to improvement in arterial endothelial function and lowers levels of systemic inflammation that are elevated in gout patients, even during intercritical periods [81]. Further, a recent study suggests that, in patients who initiated intense ULT with pegloticase, gout flare led to a prolonged elevation in the neutrophil-to-lymphocyte ratio [82], a biomarker for systemic inflammation. Given that these comorbidities have an inflammatory component to their etiologies, that gout flares put patients at risk for subsequent cardiovascular events [83], and that urate deposition volume is positively associated with cardiovascular risk and overall mortality [35], systemic inflammation in gout patients is of great interest and further study is underway.
Obesity rates were higher in EOG patients than in CG patients in all US and Chinese populations examined. This finding is consistent with other studies showing that obesity is an independent risk factor for developing gout [84,85,86] and is associated with a younger age of gout onset [86]. Both French populations examined, had similar BMI/obesity prevalence in EOG and CG patients [53, 59]. This discrepancy between the French and other populations may be related to the low obesity rate in France near the time of data collection (approximately 15% in 2017 [87]).
Our study had several limitations. First, the relevant number of publications that satisfied inclusion criteria was small. Second, our results may have been influenced by biases inherent to systematic literature reviews including publication and selection biases. Third, the definition of EOG was not consistent across all studies potentially leading to some overlap between groups and a potentially non-homogeneous population across studies. This lack of a uniform definition for EOG emphasizes the need for formalizing EOG as a distinct subset of the gout population. Fourth, patient medication compliance is a known challenge in managing gout, particularly in younger patients (< 45 years) [88]. However, the influence of compliance on our findings cannot be commented on because, of the 3 studies that did not exclude patients with prior ULT use [58, 59, 62], compliance information was not provided. Lastly, causality of gout for the comorbidities reported on cannot be determined from this analysis. Our findings are hypothesis generating but larger longitudinal studies with consistent EOG definition are needed to better examine patient characteristics and understand the relationship between gout and its associated comorbidities.
Conclusions
In conclusion, the literature suggests that patients with EOG present with more severe disease and are more recalcitrant to oral ULTs than patients with CG, with underlying genetic defects in urate transporters playing a large role in gout development. Therefore, those with EOG may benefit from earlier and more aggressive ULT therapy to adequately achieve their target SU. Because a large proportion of EOG patients do have a genetic predisposition to hyperuricemia, this finding is of particular importance in the young EOG population. First, patients with EOG must live with the condition for decades, making them particularly susceptible to the pain and disability associated with gout. Second, at gout diagnosis, the EOG population had a much lower cardiovascular, renal, and metabolic comorbidity burden than seen in the CG population. Therefore, referral to a rheumatologist early in the disease course may be warranted for SU management. Though more rigorous study is needed, the temporal separation between gout diagnosis and cardiometabolic comorbidity development suggests there may be a window of opportunity when early SU control in EOG patients may attenuate gout progression and subsequent comorbidity development.
References
Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK. Contemporary prevalence of gout and hyperuricemia in the United States and decadal trends: the national health and nutrition examination survey, 2007–2016. Arthritis Rheumatol. 2019;71:991–9.
Safiri S, Kolahi AA, Cross M, et al. Prevalence, incidence, and years lived with disability due to gout and its attributable risk factors for 195 countries and territories 1990–2017: a systematic analysis of the global burden of disease study 2017. Arthritis Rheumatol. 2020;72:1916–27.
Kuo CF, Grainge MJ, Zhang W, Doherty M. Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol. 2015;11:649–62.
Doherty M. New insights into the epidemiology of gout. Rheumatology. 2009; 48(2):2–8.
FitzGerald JD, Dalbeth N, Mikuls T, et al. 2020 American College of Rheumatology guideline for the management of gout. Arthritis Care Res (Hoboken). 2020;72:744–60.
Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. 2017;76:29–42.
Jordan KM, Cameron JS, Snaith M, et al. British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of gout. Rheumatology (Oxford). 2007;46:1372–4.
Thottam GE, Krasnokutsky S, Pillinger MH. Gout and metabolic syndrome: a tangled web. Curr Rheumatol Rep. 2017;19:60.
Richette P, Clerson P, Perissin L, Flipo RM, Bardin T. Revisiting comorbidities in gout: a cluster analysis. Ann Rheum Dis. 2015;74:142–7.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Med. 1998; 15:539–53.
Grayson PC, Kim SY, LaValley M, Choi HK. Hyperuricemia and incident hypertension: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2011;63:102–10.
Johnson RJ, Segal MS, Srinivas T, et al. Essential hypertension, progressive renal disease, and uric acid: a pathogenetic link? J Am Soc Nephrol. 2005;16:1909–19.
Krishnan E. Interaction of inflammation, hyperuricemia, and the prevalence of hypertension among adults free of metabolic syndrome: NHANES 2009–2010. J Am Heart Assoc. 2014;3: e000157.
Pan A, Teng GG, Yuan JM, Koh WP. Bidirectional association between self-reported hypertension and gout: The Singapore Chinese Health Study. PLoS ONE. 2015;10: e0141749.
Wandell P, Carlsson AC, Ljunggren G. Gout and its comorbidities in the total population of Stockholm. Prev Med. 2015;81:387–91.
Pan A, Teng GG, Yuan JM, Koh WP. Bidirectional association between diabetes and gout: the Singapore Chinese Health Study. Sci Rep. 2016;6:25766.
Rho YH, Lu N, Peloquin CE, et al. Independent impact of gout on the risk of diabetes mellitus among women and men: a population-based BMI-matched cohort study. Ann Rheum Dis. 2016;75:91–5.
Tung YC, Lee SS, Tsai WC, Lin GT, Chang HW, Tu HP. Association between gout and incident type 2 diabetes mellitus: a retrospective cohort study. Am J Med. 2016;129(1219):e17-25.
Zhu Y, Pandya BJ, Choi HK. Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007–2008. Am J Med. 2012;125(679–87): e1.
Juraschek SP, Miller ER 3rd, Gelber AC. Body mass index, obesity, and prevalent gout in the United States in 1988–1994 and 2007–2010. Arthritis Care Res (Hoboken). 2013;65:127–32.
Rathmann W, Funkhouser E, Dyer AR, Roseman JM. Relations of hyperuricemia with the various components of the insulin resistance syndrome in young black and white adults: the CARDIA study. Coronary Artery Risk Development in Young Adults. Ann Epidemiol. 1998; 8:250–61.
Singh JA, Cleveland JD. Gout and the risk of incident atrial fibrillation in older adults: a study of US Medicare data. RMD Open. 2018;4: e000712.
Kuo CF, Yu KH, See LC, et al. Risk of myocardial infarction among patients with gout: a nationwide population-based study. Rheumatology (Oxford). 2013;52:111–7.
Liu SC, Xia L, Zhang J, et al. Gout and risk of myocardial infarction: a systematic review and meta-analysis of cohort studies. PLoS ONE. 2015;10: e0134088.
Singh JA, Ramachandaran R, Yu S, et al. Is gout a risk equivalent to diabetes for stroke and myocardial infarction? A retrospective claims database study. Arthritis Res Ther. 2017;19:228.
Choi HK, Curhan G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation. 2007;116:894–900.
Clarson LE, Chandratre P, Hider SL, et al. Increased cardiovascular mortality associated with gout: a systematic review and meta-analysis. Eur J Prev Cardiol. 2015;22:335–43.
Kuo CF, See LC, Luo SF, et al. Gout: an independent risk factor for all-cause and cardiovascular mortality. Rheumatology (Oxford). 2010;49:141–6.
Vincent ZL, Gamble G, House M, et al. Predictors of mortality in people with recent-onset gout: a prospective observational study. J Rheumatol. 2017;44:368–73.
Disveld IJM, Zoakman S, Jansen T, et al. Crystal-proven gout patients have an increased mortality due to cardiovascular diseases, cancer, and infectious diseases especially when having tophi and/or high serum uric acid levels: a prospective cohort study. Clin Rheumatol. 2019;38:1385–91.
Klauser AS, Halpern EJ, Strobl S, et al. Dual-energy computed tomography detection of cardiovascular monosodium urate deposits in patients with gout. JAMA Cardiol. 2019;4:1019–28.
Barazani SH, Chi WW, Pyzik R, et al. Quantification of uric acid in vasculature of patients with gout using dual-energy computed tomography. World J Radiol. 2020;12:184–94.
Feuchtner GM, Plank F, Beyer C, et al. Monosodium urate crystal deposition in coronary artery plaque by 128-slice dual-energy computed tomography: an ex vivo phantom and in vivo study. J Comput Assist Tomogr. 2021;45:856–62.
Gamala M, Jacobs JWG, Linn-Rasker SP, et al. Cardiovascular risk in patients with new gout diagnosis: is monosodium urate volume at ankles and feet on dual-energy computed tomography associated with previous cardiovascular events? Clin Exp Rheumatol. 2020;38:763–6.
Marty-Ané A, Norberciak L, Andrès M, et al. Crystal deposition measured with dual-energy computed tomography: association with mortality and cardiovascular risks in gout. Rheumatology (Oxford). 2021;60:4855–60.
Roughley M, Sultan AA, Clarson L, et al. Risk of chronic kidney disease in patients with gout and the impact of urate lowering therapy: a population-based cohort study. Arthritis Res Ther. 2018;20:243.
Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17:90.
Singh JA, Cleveland JD. Gout is associated with a higher risk of chronic renal disease in older adults: a retrospective cohort study of US Medicare population. BMC Nephrol. 2019; 20:93.
Stack AG, Johnson ME, Blak B, et al. Gout and the risk of advanced chronic kidney disease in the UK health system: a national cohort study. BMJ Open. 2019;9: e031550.
Yu KH, Kuo CF, Luo SF, et al. Risk of end-stage renal disease associated with gout: a nationwide population study. Arthritis Res Ther. 2012;14:R83.
Sellmayr M, Hernandez Petzsche MR, Ma Q, et al. Only hyperuricemia with crystalluria, but not asymptomatic hyperuricemia, drives progression of chronic kidney disease. J Am Soc Nephrol. 2020;31:2773–92.
Juraschek SP, Kovell LC, Miller ER 3rd, Gelber AC. Association of kidney disease with prevalent gout in the United States in 1988–1994 and 2007–2010. Semin Arthritis Rheum. 2013;42:551–61.
Kuo CF, Grainge MJ, Mallen C, Zhang W, Doherty M. Impact of gout on the risk of atrial fibrillation. Rheumatology (Oxford). 2016;55:721–8.
Kuo CF, Grainge MJ, Mallen C, Zhang W, Doherty M. Comorbidities in patients with gout prior to and following diagnosis: case-control study. Ann Rheum Dis. 2016;75:210–7.
Chandratre P, Roddy E, Clarson L, Richardson J, Hider SL, Mallen CD. Health-related quality of life in gout: a systematic review. Rheumatology (Oxford). 2013;52:2031–40.
Hirsch JD, Terkeltaub R, Khanna D, et al. Gout disease-specific quality of life and the association with gout characteristics. Patient Relat Outcome Meas. 2010;2010:1–8.
Jin Z, Feng X, Wang D, et al. Global, regional and national trends in sex- and age-specific disability-adjusted life years of musculoskeletal disorders, 1990–2019. Rheumatology (Oxford). 2022;61:2978–86.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Zaidi F, Narang RK, Phipps-Green A, et al. Systematic genetic analysis of early-onset gout: ABCG2 is the only associated locus. Rheumatology (Oxford). 2020;59:2544–9.
Toyoda Y, Pavelcová K, Klein M, et al. Familial early-onset hyperuricemia and gout associated with a newly identified dysfunctional variant in urate transporter ABCG2. Arthritis Res Ther. 2019;21:219.
Toyoda Y, Pavelcová K, Bohatá J, et al. Identification of two dysfunctional variants in the ABCG2 urate transporter associated with pediatric-onset of familial hyperuricemia and early-onset gout. Int J Mol Sci. 2021; 22:2.
Pálinkás M, Szabó E, Kulin A, et al. Genetic polymorphisms and decreased protein expression of ABCG2 urate transporters are associated with susceptibility to gout, disease severity and renal-overload hyperuricemia. Clin Exp Med. 2022 [Epub ahead of print].
Collet C, Morel H, Ricquebourg M, et al. Identification of new and rare variants in ABCG2, SLC22A1 and ALDH16A1 genes in crystal-proven early-onset gout [abstract]. Arthritis Rheumatol. 2018;70(suppl 9):144.
Huang XF, Sun L, Zhang C, et al. Whole-exome sequencing reveals a rare missense variant in SLC16A9 in a pedigree with early-onset gout. BioMed Res Int. 2020;2020:4321419.
Li Q-H, Chen L-X, Li Y-H, et al. More obesity and higher serum uric acid in early-onset gout patients in south China [abstract]. Ann Rheum Dis. 2017;76(suppl 2):373.
Li QH, Zou YW, Lian SY, et a l. Sugar-sweeten beverage consumption Is associated with more obesity and higher serum uric acid in Chinese male gout patients with early onset. Front Nutr. 2022; 9:916811.
Li Y, Piranavan P, Sundaresan D, Yood R. Clinical characteristics of early-onset gout in outpatient setting. ACR Open Rheumatol. 2019;1:397–402.
Gao Q, Cheng X, Merriman TR, et al. Trends in the manifestations of 9754 gout patients in a Chinese clinical center: a 10-year observational study. Joint Bone Spine. 2021;88: 105078.
Pascart T, Norberciak L, Ea HK, Guggenbuhl P, Lioté F. Patients with early-onset gout and development of earlier severe joint involvement and metabolic comorbid conditions: results from a cross-sectional epidemiologic survey. Arthritis Care Res (Hoboken). 2019;71:986–92.
Suh YS, Noh HS, Kim HJ, et al. Differences in clinical and dietary characteristics, serum adipokine levels, and metabolomic profiles between early- and late-onset gout. Metabolites. 2021;11:399.
Li Q, Zeng S-H, Du X-Y, et al. Fructose-containing beverages is an independent risk factor for gout early-onset in south China [abstract]. Ann Rheum Dis. 2018;77(suppl 2):142–3.
Herrou J, Al Tabaa O, Gaix-Fontaine E, et al. Phenotype of patients with early-onset gout [abstract]. Ann Rheum Dis. 2019;78(suppl 2):1301.
Amatucci A, LaMoreaux B, Bulbin D. Early-onset gout (EOG) patients are an important and recalcitrant phenotype warranting further investigation: a systematic review [abstract]. Arthritis Rheumatol. 2021;73(suppl 9):xxx.
Perng WT, Hung YM, Lai WY, Chu KA, Wang YH, Wei JC. Increased risk of glaucoma amongst new-onset gout patients aged 20–39 years: a nationwide population-based cohort study in Taiwan. Int J Clin Pract. 2021;75: e14169.
Zhang B, Fang W, Zeng X, et al. Clinical characteristics of early- and late-onset gout: a cross-sectional observational study from a Chinese gout clinic. Medicine (Baltimore). 2016;95: e5425.
Phipps-Green AJ, Merriman ME, Topless R, et al. Twenty-eight loci that influence serum urate levels: analysis of association with gout. Ann Rheum Dis. 2016;75:124–30.
Lioté F, Merriman T, Nasi S, So A. Workshop report: 4th European crystal network meeting. Arthritis Res Ther. 2013;15:304.
Saag KG, Fitz-Patrick D, Kopicko J, et al. Lesinurad combined with allopurinol: a randomized, double-blind, placebo-controlled study in gout patients with an inadequate response to standard-of-care allopurinol (a US-based study). Arthritis Rheumatol. 2017;69:203–12.
Bardin T, Keenan RT, Khanna PP, et al. Lesinurad in combination with allopurinol: a randomised, double-blind, placebo-controlled study in patients with gout with inadequate response to standard of care (the multinational CLEAR 2 study). Ann Rheum Dis. 2017;76:811–20.
Tausche AK, Alten R, Dalbeth N, et al. Lesinurad monotherapy in gout patients intolerant to a xanthine oxidase inhibitor: a 6-month phase 3 clinical trial and extension study. Rheumatology (Oxford). 2017;56:2170–8.
Dalbeth N, Jones G, Terkeltaub R, et al. Lesinurad, a selective uric acid reabsorption inhibitor, in combination with febuxostat in patients with tophaceous gout: findings of a phase III clinical trial. Arthritis Rheumatol. 2017;69:1903–13.
Yang Q, Köttgen A, Dehghan A, et al. Multiple genetic loci influence serum urate levels and their relationship with gout and cardiovascular disease risk factors. Circ Cardiovasc Genet. 2010;3:523–30.
Matsuo H, Ichida K, Takada T, et al. Common dysfunctional variants in ABCG2 are a major cause of early-onset gout. Sci Rep. 2013;3:2014.
Kolz M, Johnson T, Sanna S, et al. Meta-analysis of 28,141 individuals identifies common variants within five new loci that influence uric acid concentrations. PLoS Genet. 2009;5: e1000504.
van der Harst P, Bakker SJ, de Boer RA, et al. Replication of the five novel loci for uric acid concentrations and potential mediating mechanisms. Hum Mol Genet. 2010;19:387–95.
Zheng Q, Keliang W, Hongtao Q, Xiaosheng L. Genetic association between SLC22A12 variants and susceptibility to hyperuricemia: a meta-analysis. Genet Test Mol Biomarkers. 2022;26:81–95.
Vasiliou V, Sandoval M, Backos DS, et al. ALDH16A1 is a novel non-catalytic enzyme that may be involved in the etiology of gout via protein-protein interactions with HPRT1. Chem Biol Interact. 2013;202:22–31.
Furuhashi M. New insights into purine metabolism in metabolic diseases: role of xanthine oxidoreductase activity. Am J Physiol Endocrinol Metab. 2020;319:e827–34.
Roberts RL, Wallace MC, Phipps-Green AJ, et al. ABCG2 loss-of-function polymorphism predicts poor response to allopurinol in patients with gout. Pharmacogenom J. 2017;17:201–3.
Wen CC, Yee SW, Liang X, et al. Genome-wide association study identifies ABCG2 (BCRP) as an allopurinol transporter and a determinant of drug response. Clin Pharmacol Ther. 2015;97:518–25.
Toprover M, Shah B, Oh C, et al. Initiating guideline-concordant gout treatment improves arterial endothelial function and reduces intercritical inflammation: a prospective observational study. Arthritis Res Ther. 2020;22:169.
Pillinger M, Obermeyer K, Padnick-Silver L, LaMoreaux B. Neutrophil-to-lymphocyte ratio among flaring and non-flaring uncontrolled gout patients undergoing pegloticase therapy as part of the phase 3 pivotal trials [abstract]. Arthritis Rheumatol. 2022;74(suppl 9):22.
Cipolletta E, Tata LJ, Nakafero G, Avery AJ, Mamas MA, Abhishek A. Association between gout flare and subsequent cardiovascular events among patients with gout. JAMA. 2022;328:440–50.
Evans PL, Prior JA, Belcher J, Mallen CD, Hay CA, Roddy E. Obesity, hypertension and diuretic use as risk factors for incident gout: a systematic review and meta-analysis of cohort studies. Arthritis Res Ther. 2018;20:136.
Aune D, Norat T, Vatten LJ. Body mass index and the risk of gout: a systematic review and dose-response meta-analysis of prospective studies. Eur J Nutr. 2014;53:1591–601.
DeMarco MA, Maynard JW, Huizinga MM, et al. Obesity and younger age at gout onset in a community-based cohort. Arthritis Care Res (Hoboken). 2011;63:1108–14.
World Obesity Federation. Global Obesity Observatory: France. Available from: https://data.worldobesity.org/country/france-71/#data_prevalence [Accessed 31 March 2023].
Keenan RT. Limitations of the current standards of care for treating gout and crystal deposition in the primary care setting: a review. Clin Ther. 2017;39:430–41.
Acknowledgements
Funding
Specific funds were not used to conduct this study. The Rapid Service Fee was funded by Horizon Therapeutics plc.
Medical Writing, Editorial, and Other Assistance
Horizon-affiliated authors provided medical writing support, which was funded by Horizon Therapeutics plc.
Authorship
All authors meet journal and ICMJE criteria for authorship. Large Language Models (e.g., ChatGPT) were not used at any stage of manuscript development.
Author Contributions
Conceptualization: Anthony Amatucci, David Bulbin; Methodology: Anthony Amatucci, Lissa Padnick-Silver, Brian LaMoreaux, David Bulbin; Formal analysis and investigation: Anthony Amatucci, Lissa Padnick-Silver; Writing – original draft preparation: Anthony Amatucci, Lissa Padnick-Silver; Writing – review and editing: Anthony Amatucci, Lissa Padnick-Silver, Brian LaMoreaux, David Bulbin; Funding acquisition: Not applicable; Resources: Anthony Amatucci, Brian LaMoreaux; Supervision: Anthony Amatucci. All authors read and approved the final manuscript.
Prior Presentation
Preliminary findings of this work were presented as a poster at the 2021 annual meeting of the American College of Rheumatology (Poster number: 0669; November 3–10, 2021; virtual meeting).
Disclosures
Anthony Amatucci, Lissa Padnick-Silver, and Brian LaMoreaux are employees of and stockholders in Horizon. David Bulbin has no financial incentives to disclosure.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Amatucci, A.J., Padnick-Silver, L., LaMoreaux, B. et al. Comparison Between Early-Onset and Common Gout: A Systematic Literature Review. Rheumatol Ther 10, 809–823 (2023). https://doi.org/10.1007/s40744-023-00565-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-023-00565-x