Abstract
Introduction
SB4 is the first approved biosimilar of etanercept, a biologic tumor necrosis factor inhibitor, to treat various autoimmune diseases including axial spondylarthritis (axSpA), rheumatoid arthritis (RA), psoriatic arthritis (PsA), and plaque psoriasis (PsO). This post-marketing surveillance (PMS) study of SB4 investigated safety and effectiveness in routine clinical practice and is part of the drug approval process in Korea.
Methods
This prospective, multi-center, open-label, observational, phase IV PMS study was designed to enroll patients with axSpA, RA, PsA, and PsO in Korea from September 2015 to September 2019. Both etanercept-naïve patients or patients switched from reference etanercept were included. SB4 was administered weekly via subcutaneous injections using pre-filled syringes. Safety was assessed by the incidence of adverse events (AEs), adverse drug reactions (ADRs) and serious adverse events (SAE). Effectiveness was assessed by the change from baseline of investigator-rated Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) in patients with ankylosing spondylitis (AS) and disease activity score-28 (DAS28) in patients with RA.
Results
Among 316 enrolled patients, 314 were included in the safety analysis (176 with AS and 138 with RA). The overall incidence of AEs, ADRs and serious AEs were 17.8, 9.9, and 1.3%, respectively. Most AEs were mild (66.7%) or moderate (31.1%) and not related to SB4 (58.9%). Most common AEs were injection site pruritus (1.9%) and injection site rash (1.3%). At week 24, mean disease activity scores significantly decreased compared to baseline in naïve patients with AS and RA (BASDAI 2.7 vs. 6.2, p < 0.0001; DAS28 3.8 vs. 5.7, p < 0.0001) and in switched patients with AS and RA (BASDAI 1.0 vs. 1.3, p = 0.0018; DAS28 2.4 vs. 2.9, p = 0.0893).
Conclusion
This first real-world evidence of SB4 from a phase IV PMS study in Korea shows comparable effectiveness to historical SB4 real-world evidence without any new significant safety signals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This post-marketing surveillance (PMS) study evaluated the safety and effectiveness of SB4 in patients with ankylosing spondylitis (AS) and rheumatoid arthritis (RA) in Korea. |
SB4 showed a safety profile with an incidence of adverse events of 17.8% and an incidence of serious adverse events of 1.3% without any new safety signals compared to historical etanercept data. |
SB4 demonstrated effectiveness in both patients with AS and RA by significantly reducing mean disease activity scores BASDAI (− 1.6, p < 0.0001 vs. baseline) and DAS28 scores (− 1.6, p < 0.0001 vs. baseline) at week 24, respectively. |
These findings further support the safety and effectiveness of SB4 in both etanercept-naïve and switched from reference etanercept patients with AS and RA in real-world practice. |
Introduction
Etanercept is the first approved biologic tumor necrosis factor (TNF) antagonist (fusion protein TNFRp75-Fc) for the treatment of rheumatoid arthritis (RA) and other autoimmune diseases comprising, axial spondylarthritis (axSpA), juvenile idiopathic arthritis (JIA), psoriatic arthritis (PsA), and plaque psoriasis (PsO) [1, 2].
SB4 was developed by Samsung Bioepis and was the first approved etanercept biosimilar in the European Union (EU) in 2016 (Benepali™; European Medicines Agency, EMA), in the United States (US) in 2019 (Eticovo®; US Food and Drug Administration agency, FDA), in Canada and Australia in 2016 (Brenzys®; Health Canada, HC and Therapeutic Goods Administration, TGA) and in Korea in 2015 (Etoloce®; Ministry of Food and Drug Safety, MFDS) in all indications as the reference etanercept [3].
In a pivotal phase III study, SB4 demonstrated equivalent efficacy and comparable safety and immunogenicity to reference etanercept in patients with RA [4, 5]. The open-label extension of that study confirmed the tolerability of SB4 for up to 100 weeks [6]. Neither loss of efficacy nor an increase in immunogenicity or treatment-emergent adverse events (TEAEs) were observed over the 100-week treatment period [6]. A further analysis comparing SB4-treated etanercept-naïve patients (n = 126) and patients switched from reference etanercept to SB4 at week 52 (n = 119) revealed comparable efficacy (ACR20 of 77.9 and 79.1%, respectively), safety (TEAE rate of 47.6 and 48.7%, respectively) at week 100 [6]. These findings were confirmed by accumulated real-world evidence, which included 13,552 patients with RA, PsA, axSpA, SpA, PsO, enteropathic arthritis, JIA, and other rheumatic diseases who were etanercept-naïve or switched from reference etanercept to SB4 [7]. Hereafter, etanercept-naïve patients will be referred to as “naïve”, and reference etanercept-switched patients will be referred to as “switched” patients.
In Korea, post-marketing surveillance (PMS) studies are part of the drug approval process, allowing re-examination of safety results of new medications that are already approved and on the market for a designated period (4–6 years) [8]. This PMS study aimed to evaluate the safety and effectiveness of SB4 in clinical practice in Korea. Furthermore, effectiveness of SB4 in naïve and switched patients was assessed and compared with other real-world data of SB4.
Methods
Study Design
This prospective, multi-center, open-label, observational, phase IV PMS study was designed to include patients with axSpA, RA, PsA, and PsO, in Korea. The study protocol was reviewed and approved by the ethics committees or institutional review boards of each participating institutions (Supplemental Material). All patients were provided written informed consent prior to treatment initiation. This PMS study was conducted in accordance with the Helsinki Declaration (1964 and its later amendments), and any other relevant laws and regulations.
Treatment decisions were left to the investigator’s discretion according to their routine practice. Patients were injected with doses of 50 mg SB4 subcutaneously using pre-filled syringes (PFS).
Study Population
Patients were included if they were willing to participate in this PMS study and were using the study drug within its scope of labeled information. Patients with hypersensitivity to etanercept or any other ingredient of the study drug, or sepsis, risk of sepsis, or an active chronic or localized infection including tuberculosis were excluded.
Study Outcomes
The primary endpoint of this study is safety, evaluated as incidence of adverse events (AEs), adverse drug reactions (ADRs) and serious adverse events (SAEs) after the administration of SB4 for each indication. A SAE was defined as any event leading to death or a life-threatening situation, hospitalization or prolongation of hospitalization, persistent or significant disability or incapacity, congenital anomaly or birth defect or being another important medical event. Investigator classified the severity of each AE and SAE reported during the study period based on their own clinical judgement as Mild (self-awareness of symptoms without interfering daily life, allowing continuous treatment without changing the administration of the study drug), Moderate (subject feels interference with daily life, requiring dose reduction of the study drug or treatment) or Severe (unable to maintain daily life due to significant impairment, requiring discontinuation of the study drug). The relationship between the AE and the drug was classified according to the investigator’s discretion among four criteria of Certain, Probable/likely, Possible, and Unlikely unless it was conditional or not assessable.
Secondary endpoints comprised the overall improvement of investigator’s overall effectiveness assessment using a binary classification of effective and ineffective for responders and non-responders, respectively. Responders were those who showed improvement in disease activity scores after SB4 administration. Non-responders comprised those whose disease activity scores did not improve or worsened after the administration of SB4.
The disease activity scores were Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) for patients with axSpA (including those with AS), Disease Activity Score in 28 joints (DAS28) for patients with RA, Psoriasis Area Severity Index (PASI) for patients with PsO, and the number of joints with tenderness and edema for patients with PsA [9,10,11,12,13]. BASDAI was selected as disease activity score for axSpa because this is the standard score used by the Korean national insurance and therefore available for this observational study.
Data Collection
Demographic data including sex, age, weight, duration of disease, treatment classification, smoking history, and pack-years were collected at the first study visit (week 0). In addition, information about medical history, medication history (i.e., disease-modifying anti-rheumatic drugs (DMARDs) and concomitant medications), and baseline disease activity prior to the study drug administration in respective indication were collected.
The status of study drug administration, concomitant medication history, safety, and effectiveness were assessed at baseline and weeks 4, 12, and 24 or early termination visit. In addition, general assessment of the drug (i.e., continuation or discontinuation) was conducted at week 24 or early termination visit.
Statistical Analysis
Sample Size and Analysis Sets
A sample size of 300 was found adequate based on agreement with the MFDS, and in accordance with the re-examination regulations [8]. The safety set included patients who received SB4 at least once and the effectiveness set comprised patients who received at least one SB4 dose and had at least one effectiveness assessment before and after SB4 administration.
Statistical Analyses
Patient demographics and disease characteristics were summarized by indications using mean and standard deviation (SD) for continuous variables, and percentages for categorical variables.
AEs were classified and analyzed according to MedDRA 22.0, using the standard disease names [14]. For each adverse event, the overall incidence was calculated. All AEs were analyzed in terms of seriousness, severity, causality, and outcome.
Effectiveness results are presented as and percentages for response rates. The changes in disease activity scores from baseline were analyzed using the paired t test or Wilcoxon signed-rank test. An ad hoc analysis was conducted to compare the effectiveness of SB4 from baseline to week 24 in both naïve and reference switched patients.
All analyses were done using SAS (version 9.2 or higher).
Results
Patient Disposition
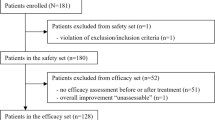
A total of 316 patients were enrolled in 19 centers between September 07, 2015, and September 06, 2019 (Fig. 1). Two patients were excluded from the analysis because they did not meet the inclusion criteria. At the end of the study, 94.9% (300/316) remained on SB4. The safety analysis set included 314 patients, and the effectiveness analysis set comprised 248 patients who had available efficacy data.
Baseline and Disease Characteristics
The study population comprised 176 (56.1%) patients with AS and 138 (43.9%) patients with RA, with a mean (SD) disease duration of 9.0 (7.0) and 8.4 (7.3) years, respectively (Table 1). None of the patients had a diagnosis of PsO, PsA or non-radiographic axSpA. The mean (SD) age was 48.2 (13.8) years, 175 were male (55.7%), and the majority were treated in an outpatient setting (97.1%). Most patients had no smoking history (81.5%). Among those with smoking history (n = 58) and known amount of consumption (n = 40), the mean (SD) cigarette consumption was 15.7 (12.5) packs/year. Among 314 patients, 248 patients were included in the effectiveness analysis set. In patients with AS, mean (SD) BASDAI was 3.4 (3.0). In patients with RA, mean (SD) DAS28 was 5.0 (1.7).
Safety
Throughout the study period, the incidences of AEs and ADRs were 17.8 and 9.9%, respectively. Notably, the incidence rate of AEs was lower in patients with AS (12.4%) compared to patients with RA (23.9%). The majority of AEs were considered mild (66.7%) or moderate (31.1%) and considered unlikely (58.9%) or possibly (26.7%) related to the study drug. Most common AEs were injection site reactions (ISRs) (5.7%), belonging to the high-level group term administration site conditions, which comprised injection site pruritus (1.9%) and injection site rash (1.3%) as most frequent events (Table 2). Severe AEs (2.2%) included one case of synovitis and one tenosynovitis, however both were considered not related to SB4.
The incidence of SAEs was 1.3% (Table 3) and the incidence of serious ADRs 0.6%. One patient with AS (0.6%) reported a SAE of dizziness and three patients with RA (2.2%) reported a total of five SAEs, comprising arthralgia, synovitis, tenosynovitis, nausea, and pneumonia. SAEs of dizziness and pneumonia were considered drug-related.
Overall, 22 AEs led to complete treatment discontinuation in 17 patients (24.4%) and 5 AEs resulted in temporary suspension of treatment in 5 patients (5.6%). There were no significant differences in safety profiles depending on age, smoking history and comorbidities.
Effectiveness
Among 314 patients, 66 patients were excluded from effectiveness analysis set; 11 patients discontinued the treatment, and 55 patients did not have effectiveness data available. Response rates among naïve patients at week 24 were 90.9% (60/66) among patients with AS and 98.6% (69/70) in RA. There was no significant difference in baseline characteristics between responders and non-responders.
Naïve patients with AS and RA showed significant decreases in mean [SD] BASDAI (– 3.5 [2.1], p < 0.0001) and DAS28 scores (– 1.9 [1.0], p < 0.0001) at week 24 compared to baseline (Fig. 2). Accordingly, the proportion of AS patients with BASDAI ≥ 4 decreased from 93.9 to 23.3% and the proportion of RA patients with DAS28 > 5.1 from 78.6 to 15.0% (Fig. 3).
Mean disease activity scores (BASDAI, DAS28) of naïve and switched patients with AS and RA. AS ankylosing spondylitis, BASDAI Bath Ankylosing Spondylitis Disease Activity Index, DAS28 disease activity score-28, Naïve patients that were not treated with etanercept previously, RA rheumatoid arthritis, Switched patients that were previously treated with reference etanercept
Proportions of patients categorized by disease activity scores (%, n). AS ankylosing spondylitis, BASDAI Bath Ankylosing Spondylitis Disease Activity Index, DAS28 disease activity score-28, Naïve patients that were not treated with etanercept previously, RA rheumatoid arthritis, Switched patients that were previously treated with reference etanercept
Switched patients with AS and RA showed stable mean [SD] disease activity scores at week 24 compared to baseline (BASDAI: 1.0 [1.0] vs. 1.3 [1.5]; DAS28: 2.4 [0.6] vs. 2.9 [1.1]) (Fig. 2). However, the proportion of AS patients with BASDAI ≥ 4 was halved from 9.0 to 4.5% and no RA patient had DAS28 > 5.1 after switching at week 24 (Fig. 3). The proportion of RA patients with DAS28 ≥ 3.2 decreased from 43.5 to 7.1% after switching to SB4.
Discussion
This prospective, multi-center, open-label, observational, phase IV PMS study evaluated the safety and effectiveness of SB4 in patients with AS or RA in Korea. Findings for safety and effectiveness are in line with real-world evidence of both etanercept and SB4, indicating comparable safety and effectiveness in both naïve and switched patients without any new safety signals.
The overall incidence rates of AEs and SAEs in this PMS study (17.8 and 1.3%, respectively) were lower than those observed in 299 RA patients in the phase III study of SB4 (55.2 and 4.3%, respectively) [4]. This difference may be attributed to the differences in patients’ baseline characteristics since this PMS study included both naïve and switched patients, but the phase III study included only naïve patients. SAEs of arthralgia, synovitis, and tenosynovitis can be explained by the underlying disease of patients and were only observed in patients with RA. SAEs of nausea, pneumonia and dizziness were considered drug-related and already reflected in the precautions for use [15]. Overall, there were no significant differences in safety profiles depending on age, smoking history and comorbidities that were recently identified as risk factors for the use of certain Janus kinase inhibitors (JAKi), resulting in a black box warning for these products.
PMS studies provide valuable insights to real-world effectiveness and safety in both naïve and switched patients [16]. For naïve patients, the change in mean BASDAI from baseline to week 24 (− 3.6) in this study, was similar to that reported in 522 patients by a Nordic observational study (− 2.6), 6 months after the switch from reference etanercept [17]. As for switched patients, mean BASDAI and DAS28 scores at week 24 in this PMS study were comparable to that in 395 patients with RA and axSpA in the BENEFIT study which describes real-world SB4 data [18]. In the BENEFIT study, mean (95% confidence interval, CI) BASDAI was 2.3 (n = 139; CI 2.0–2.6) and DAS28 was 2.1 (n = 256; CI 2.0–2.2) at 6-month after switch. Overall, this PMS study showed that both naïve and switched patients with RA and AS reported a decrease in disease activity scores, and that there was no loss in effectiveness after switch until week 24. No new safety signals were observed in this PMS study as shown in BENEFIT study.
In a 3-year, real-world drug survival and efficacy study of SB4 in patients with RA (n = 120), AS (36) and PsA 80) and patients, who were previously treated with reference etanercept, DAS28 and BASDAI remained stable over the 3 years (median scores after 3 years vs. baseline 2.5 vs. 2.37 and 1.05 vs. 1, respectively) [19].
The high retention rate in this study (94.9%) was similar to that reported by a Swedish study (90%) at 6 months, which used real-world data of 143 patients at an outpatient rheumatology center who were switched from reference etanercept [20]. Retention rates in the 3-year drug survival study of switched patients with RA, AS and PsA were 88, 94.4, and 86%, respectively [19]. A retrospective evaluation of 220 patients (85 RA, 33 AS, 81 PsA and 14 with other conditions; median follow-up 12.1 months) who were switched from reference etanercept to SB4 showed retention rates of 99.1, 88.6, and 64.6% at 6, 12, and 18 months, respectively [21]. Among 35 patients with clinically defined disease flares, 12 could be controlled with medication (e.g., NSAIDs, csDMARDs) and 13 were back-switched to reference etanercept. Routine patient monitoring to address disease flares immediately and patient information to address potential negative perceptions of biosimilars or any change in therapy (nocebo effect) may increase acceptance of biosimilars and reduce discontinuation rates from biosimilars [22].
These retention rates may indicate that SB4 is well tolerated after a switch from reference etanercept with controlled disease activity and acceptable safety profile. ISRs are common AEs of subcutaneously administered biologics and occur mostly within 24–48 h of the injection [23]. In this PMS study, the low incidence rate of ISRs (5.7%, 20 ISRs in 18 patients) was comparable to that in the SB4 group of the phase III study. The lower incidence of ISRs of SB4 may be explained by two factors, namely the composition of the formulation and the container closure system of the PFS. Compared to reference etanercept, SB4 does not contain l-arginine in its formulation and the needle shield is latex-free which can contribute to lower ISRs [23]. In the phase III study, the overall incidence of ISRs, defined by the MedDRA HLGT (high-level group term) of administration site reaction, was significantly lower in the SB4 group (3.7%, 22 ISRs in 11 patients) than in the reference group (17.5%, 157 ISRs in 52 patients) [5].
Notably, drug delivery devices of biosimilars can be different from the reference products if the device can demonstrate equivalent efficacy and PK and comparable safety. The development of a pre-filled pen (PFP) allows patients to conveniently self-administer drugs in a home setting [24]. Considering the limited hand dexterity of patients with rheumatoid diseases, it is of importance to facilitate easiness of injection to optimize treatment adherence via a PFP [24]. In the previous study rating PFP of SB4 with 191 patients and 90 health-care professionals, the PFP of SB4 was recognized as preferred in managing RA patients based on its easier use [25]. Therefore, a biosimilar equipped with an improved administration device can make a true difference to patients apart from cost aspects.
This study has a limitation in terms of a small number of study subjects (e.g., the number of naïve or switched patients per indication) and that only patients with axSpA and RA could have been enrolled although also enrolment of patients with PsA and PsO was foreseen. There were too few patients with PsA and PsO compared to patients with axSpA and RA, and etanercept is not a prior option in their treatment. While the duration of the disease and the type of prior treatment were recorded, the duration how long switched patients have received reference etanercept was not separately recorded due to the observational setting of the study, and therefore, no conclusion on a potential impact of outcomes can be made. Since the study focused on evaluating the safety profile in real-world practice as per regulatory requirements, efficacy-related outcomes were not collected in full detail. Further potential biases could have been introduced by the non-comparative open-label design, the short-term duration of 24 weeks, and the number of patients.
Conclusions
This is the first published data of SB4 in Korea, complementing the substantial SB4 real-world evidence in other regions. Results of this PMS show comparable effectiveness as reported by historical SB4 real-world evidence with no new significant safety signals. As biosimilars increase patient accessibility with reduced costs, it is expected that patients and healthcare systems could benefit by using biosimilars that have the same effectiveness and safety outcomes as their reference products [26].
References
Cobo-Ibáñez T, Martín-Mola E. Etanercept: long-term clinical experience in rheumatoid arthritis and other arthritis. Expert Opin Pharmacother. 2007;8(9):1373–97.
Guillot X, et al. Etanercept for treating axial spondyloarthritis. Expert Opin Biol Ther. 2017;17(9):1173–81.
Pelechas E, Drosos AA. Etanercept biosimilar SB-4. Expert Opin Biol Ther. 2019;19(3):173–9.
Emery P, et al. A phase III randomised, double-blind, parallel-group study comparing SB4 with etanercept reference product in patients with active rheumatoid arthritis despite methotrexate therapy. Ann Rheum Dis. 2017;76(1):51–7.
Emery P, et al. 52-week results of the phase 3 randomized study comparing SB4 with reference etanercept in patients with active rheumatoid arthritis. Rheumatology. 2017;56(12):2093–101.
Emery P, et al. Long-term efficacy and safety in patients with rheumatoid arthritis continuing on SB4 or switching from reference etanercept to SB4. Ann Rheum Dis. 2017;76(12):1986–91.
Ebbers HC, et al. Real-world evidence on etanercept biosimilar SB4 in etanercept-naïve or switching patients: a systematic review. Rheumatol Ther. 2019;6(3):317–38.
MFDS. Safety control after releasing medicinal products etc. Guideline on re-examination affairs of new drugs etc. (A guide for civil petitioner) Guide-0019-03. Jan-2019 [cited 2022 Jun-27]. Available from: https://www.mfds.go.kr/eng/brd/m_18/down.do?brd_id=eng0003&seq=71469&data_tp=A&file_seq=1.
Fransen J, Van Riel PL. The Disease Activity Score and the EULAR response criteria. Rheum Dis Clin. 2009;35(4):745–57.
Prevoo ML, et al. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38(1):44–8.
Garrett S, et al. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21(12):2286–91.
Carlin CS, et al. A 50% reduction in the Psoriasis Area and Severity Index (PASI 50) is a clinically significant endpoint in the assessment of psoriasis. J Am Acad Dermatol. 2004;50(6):859–66.
Gladman DD, et al. Assessment of patients with psoriatic arthritis: a review of currently available measures. Arthritis Rheum. 2004;50(1):24–35.
MDfR, A. What’s new: MedDRA version 22.0. 2019. Available from: https://admin.meddra.org/sites/default/files/guidance/file/whatsnew_22_0_english.pdf.
EMA. Benepali summary of product characteristics. [cited 2022 8-Jul]; Available from: https://www.ema.europa.eu/en/documents/product-information/benepali-epar-product-information_en.pdf.
La Noce A, Ernst M. Switching from reference to biosimilar products: an overview of the European approach and real-world experience so far. EMJ. 2018;3(3):74–81.
Lindström U, et al. Treatment retention of infliximab and etanercept originators versus their corresponding biosimilars: Nordic collaborative observational study of 2334 biologics naïve patients with spondyloarthritis. RMD Open. 2019;5(2): e001079.
Selmi C, et al. BENEFIT: real-world effectiveness of SB4 after transition from reference etanercept in rheumatoid arthritis and axial spondyloarthritis. Clin Exp Rheumatol. 2021;39:365–71.
Parisi S, et al. Efficacy and drug survival after switching from etanercept to the biosimilar SB4: a real-life long-term study. J Clin Med. 2022;11(3):621. https://doi.org/10.3390/jcm11030621.
Sigurdardottir V, Svärd A. Repeated switches between reference product etanercept and biosimilar do not affect disease activity or retention rate of etanercept over 24 months: a cohort study with historical controls. Jt Bone Spine. 2019;86(4):529–30.
Bruni C, et al. The switch from etanercept originator to SB4: data from a real-life experience on tolerability and persistence on treatment in joint inflammatory diseases. Ther Adv Musculoskelet Dis. 2020;12:1759720X20964031.
Allocati E, et al. Switching among biosimilars: a review of clinical evidence. Front Pharmacol. 2022;13: 917814.
Girolomoni G, et al. Comparison of injection-site reactions between the etanercept biosimilar SB 4 and the reference etanercept in patients with rheumatoid arthritis from a phase III study. Br J Dermatol. 2018;178(3):e215–6.
van den Bemt BJ, et al. A portfolio of biologic self-injection devices in rheumatology: how patient involvement in device design can improve treatment experience. Drug Deliv. 2019;26(1):384–92.
Egeth M, et al. Patient and healthcare professionals' preference for Brenzys vs. Enbrel autoinjector for rheumatoid arthritis: a randomized crossover simulated-use study. Adv Therapy. 2017;34(5):1157–72.
Jensen TB, et al. The Danish model for the quick and safe implementation of infliximab and etanercept biosimilars. Eur J Clin Pharmacol. 2020;76(1):35–40.
Acknowledgements
Funding
Planning, conduct, and analysis of the study were funded by Samsung Bioepis. The study sponsor also funded the journal’s Rapid Service Fee.
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by SFL Regulatory Affairs and Scientific Communications and funded by Samsung Bioepis.
Author Contributions
Data acquisition: Wan-Hee Yoo, Young Mo Kang, Dong Wook Kim, Eun Ha Kang, Yeon-Ah Lee, Chang-Hee Suh, Yoon-Kyoung Sung, Sang-Hoon Lee, Jung-Yoon Choe; data analysis and interpretation, manuscript preparation, editing and review: all authors.
Disclosures
Wan-Hee Yoo, Young Mo Kang, Dong Wook Kim, Eun Ha Kang, Yeon-Ah Lee, Chang-Hee Suh, Yoon-Kyoung Sung, Sang-Hoon Lee, Jung-Yoon Choe have received financial support for research from Samsung Bioepis Co., Ltd. Dong-Ha Gu and Jiwon Lee are employees of Samsung Bioepis Co., Ltd.
The authors have no other competing interests.
Compliance with Ethics Guidelines
This post-marketing surveillance study was conducted in accordance with the Helsinki Declaration (1964 and its later amendments), and any other relevant laws and regulations. The study protocol was reviewed and approved by the ethics committees or institutional review board of each participating study site. All patients provided written informed consent prior to treatment initiation.
Data Availability
Upon request, and subject to certain criteria, conditions, and exceptions, Samsung Bioepis will provide access to individual de-identified participant data to researchers whose proposals meet the research criteria and other conditions and for which an exception does not apply. Proposals should be directed to the corresponding author. For access, data requestors must enter into a data access agreement with Samsung Bioepis.
Thanking Patient Participant(s)
The authors are grateful to the volunteers for participating in the PMS study.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yoo, WH., Kang, Y., Kim, D. et al. Safety and Effectiveness of Etanercept Biosimilar SB4 for Rheumatic Diseases in South Korea: Real-World Post-marketing Surveillance Data. Rheumatol Ther 10, 329–341 (2023). https://doi.org/10.1007/s40744-022-00515-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00515-z