Abstract
Introduction
The aim of this work is to propose Boolean-defined low disease activity (LDA) and to test its utility in rheumatoid arthritis (RA).
Methods
We used data from a longitudinal academic clinical database of RA in Peking University First Hospital over a decade. The initial proposal of Boolean-defined LDA was proposed with ascending thresholds from 2 to 5 in steps of 1 (referred to as Boolean-LDA2/3/4/5). Agreement and residual swollen joint count (SJC) pattern with the index-based [Simplified Disease Activity Index (SDAI) and Clinical Disease Activity Index (CDAI)] LDA was analyzed. To confirm discovery, we randomly classified RA patients in a 3:2 ratio into either analysis cohort or validation cohort.
Results
In total, 4881 visits of 672 patients were included in the analysis cohort. Of these visits, the frequencies of achieving LDA were 71.9% (SDAI), 73.6% (CDAI), 52.8% (Boolean-LDA2), 65.2% (Boolean-LDA3), 73.5% (Boolean-LDA4), and 80.7% (Boolean-LDA5). High consistency and similar SJC pattern with SDAI-LDA or CDAI-LDA were observed in Boolean-LDA3 (kappa = 0.796, 0.771). Further analysis found meeting SDAI-LDA but not Boolean-LDA3 was largely attributable to higher patient’s global assessment (PGA) scores (62.9%). In further modification of Boolean-LDA3, better agreement with SDAI-LDA or CDAI-LDA was reached when exclusively increasing PGA cutoffs to 4.0, 4.5 or replacing PGA by evaluator’s global assessment (EGA) with cutoff to 3.0. These findings were further replicated in randomly generated validation cohort of 449 patients with 3306 clinic visits.
Conclusions
Using cutoff of 3 to Boolean-LDA provides great clinical utility with index-based LDA, especially when exclusively increasing PGA cutoffs to 4.0, 4.5 or replacing PGA by EGA with cutoffs to 3.0. This may deserve being considered in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Reaching low-disease activity (LDA) is an alternative therapeutic goal, particularly in rheumatoid arthritis patients (RA) with long-standing disease. |
Boolean-defined LDA are not unequivocally established, which indeed restricted the application of the definition in daily practice. |
What was learned from this study? |
Boolean-defined LDA with cutoff of 3 shows high consistency with SDAI- or CDAI-LDA. |
Higher PGA leads to most inconsistences between Boolean-LDA with cutoff of 3 and SDAI-LDA. |
Using cutoff of 3 to Boolean-LDA provides great clinical utility with index-based LDA, especially when exclusively increasing PGA cutoffs to 4.0, 4.5 or replacing PGA by EGA with cutoffs to 3.0, which should be validated in other settings and may deserve considering in clinical practice. |
Digital Features
This article is published with digital features to facilitate understanding of the article. You can access the digital features on the article’s associated Figshare page. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13348442
Introduction
Rheumatoid arthritis (RA) is a chronic, systemic autoimmune disease characterized by progressive, symmetric arthritis, leading to irreversible joint destruction [1, 2]. Over the past decades, treat-to-target strategy and novel therapeutic agents have tremendously transformed the clinical trajectory of RA patients [3,4,5]. In the American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR) management recommendations for RA, a state of clinical remission is placed as the primary target for RA treatment [6]. Alternatively, low disease activity (LDA) may also be an acceptable therapeutic goal, particularly in long-standing disease, in the context of complicated clinical scenario [7].
In general, the states of LDA and remission can be defined according to different composite measures with corresponding cutoffs, including the disease activity score based on 28-joint count (DAS28) [8], Simplified Disease Activity Index (SDAI) [9], and Clinical Disease Activity Index (CDAI) [10]. As for each target, each of these different composite measures or cutoffs are intended to measure the same construct. Ideally, they would all strongly agree with each other and result in the same treatment consequences. Although CDAI- and SDAI-defined LDA and remission are reported to strongly agree with each other, other measures had higher discordance [11, 12]. For example, the DAS28 remission allows for a significant number of residual swollen joints, which cannot be overcome by modifying the cutoff [13, 14]. Apart from these criteria, ACR/EULAR Boolean definition provided remission criteria for RA patients almost one decade ago, which includes swollen joint count (SJC), tender joint count (TJC), patient’s global assessment (PGA, 0–10 scale), and C-reactive protein (CRP) levels (mg/dl). A patient must have scores of 1 or less in each component to attain Boolean remission [15]. The LDA is an alternative therapeutic goal, however, Boolean-defined LDA is not unequivocally established, which indeed restricts the application of the definition in daily practice.
To fill the gap, we aimed to propose Boolean definition for LDA, and test its clinical utility with a comparator of either SDAI-LDA or CDAI-LDA, on basis of a large real-world database of RA patients.
Methods
Study Population
All patients were identified from the outpatient clinic of our department in real-world longitudinal database, which has been previously described and approved by the local ethics committee [5, 12, 16, 17]. In brief, a longitudinal database of a large cohort of RA patients had been established over the course of more than 10 years. RA was diagnosed according to the 1987 ACR classification criteria [18] and/or 2010 ACR/EULAR classification criteria for RA [19]. At the first visit in the database, demographics, symptom duration, RA core set variables (TJC28, SJC28, PGA, evaluator’s global assessment (EGA, 0–10 scale)), laboratory testing (CRP, mg/dl)) and treatment details (e.g. methotrexate (MTX); leflunomide (LEF); hydroxychloroquine (HCQ); sulfasalazine (SSZ)) were documented. After the initial visit, each patient contact was prospectively documented at least three-monthly for the patients in moderate/high diseases activity and every 3–12 months (usually 3–6 months) for the patients in remission/LDA. Extra follow-up was additionally scheduled besides those at regular intervals if clinically necessary. The treatment decisions at each visit were made at the discretion of rheumatologists based on disease activity scores for the explicit goal of clinical remission.
A retrospective analysis of prospectively collected data was performed for all participants in the real-world longitudinal database with RA. To confirm discovery, we randomly classified RA patients in the database at a ratio of 3:2 into either analysis cohort or validation cohort. Early or established RA was defined as the duration from onset of first arthritic symptom to the first visiting in our center with definite diagnosis of RA ≤ 1 year or > 1 year, respectively. A patient who never received disease-modifying antirheumatic drugs (DMARDs) treatment or was on DMARD treatment for less than 3 months at first visit was defined as a DMARD-naive patient. This study was approved by the Institutional Review Board (IRB) of the Peking University First Hospital (IRB number 2014–785). The participants provided their written informed consent to participate in this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Definitions of LDA
At present, various composite instruments were available to measure disease activity for RA patients, however no universal consensus on the assessment of LDA. In this study, the SDAI and CDAI index-based definitions of LDA were applied as comparators. The SDAI is obtained from a linear sum of SJC28, TJC28, PGA, EGA, and CRP (mg/dl), and SDAI ≤ 11 is defined as LDA [9]. Similarly, the CDAI is the linear sum of SJC28, TJC28, PGA, and EGA, with ≤ 10 as the definition of LDA [10].
The Boolean remission includes SJC28, TJC28, PGA, and CRP. To satisfy the remission criteria, all of these components must be ≤ 1. Since no definition of LDA exists for Boolean, we initially put forward the candidates for Boolean-LDA by increasing the cutoff of the four core set variables in steps of 1 from 2 to 3, 4, and 5. We respectively referred to them as Boolean-LDA2, Boolean-LDA3, Boolean-LDA4, and Boolean-LDA5 thereafter. Furthermore, we investigated the reasons for discordance between the initial Boolean-LDA proposals and SDAI index-based LDA, and further modifications on the impeditive variables were made to increase the agreement.
Statistical Analysis
The data were presented as means (standard deviation (SD)) or median (interquartile range (IQR)) depending on the level of resemblance to the normal distribution. Absolute and relative frequencies were reported for categorical variables. The frequencies of LDA were measured by each definition, reported as percentages with 95% confidence intervals (95% CIs). We assessed the agreement of proposed Boolean-LDA with the SDAI definition of LDA by k-coefficient for agreement at all documented visits and initial visits of included patients, respectively. The kappa values were interpreted according to Landis and Koch (agreement: poor < 0.00; slight 0.00–0.20; fair 0.21–0.40; moderate 0.41–0.60; substantial 0.61–0.80; almost perfect 0.81–1.00) [20]. Besides, previous reports showed the swollen joint was most significantly associated with radiographic progression in RA patients [13, 14, 21, 22]. Therefore, to reflect the impact of different Boolean-LDA on radiographic progression, in part, we compared the distribution of SJC across the different LDA definitions. All the analyses were conducted using SPSS version 22.0.
Results
Characteristics of Patients at Baseline
In total, 1121 patients with 8187 clinic visits in the longitudinal database were included and randomly grouped into analysis cohort or validation cohort, respectively (Table 1). In the analysis cohort, there were 672 participants comprising 4881 visits, with a mean onset age of 49 (SD 15) years, 77.2% females (Table 1). Most of the patients were rheumatoid factor (76.1%), anti-cyclic citrullinated peptides (85.6%) positive. 61.0% of all patients were DMARD-naïve at baseline. Of included patients with a mean disease duration of 24 (6–84) months, there were 314 (46.7%) early RA and 358 (53.3%) established RA patients. The median (IQR) SDAI and CDAI of patients at cohort entry was 16.1 (9.1–27.1) and 14.0 (8.0–24.0). DMARDs were initiated to all patients after enrollment to the cohort, with MTX (80.4%), LEF (45.2%), and HCQ (40.5%) as the top three. Glucocorticoids were applied as part of initial therapeutic strategies in 283 (42.1%) patients. The validation cohort comprising 449 participants with 3306 clinic visits possessed similar demographics, clinical characteristics, and treatment details to the analysis cohort (Table 1).
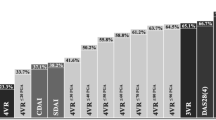
The Concordance Across LDA Definitions
The rate of reaching LDA assessed by SDAI and CDAI in all included visits was 71.9% (3510) and 73.6% (3593), respectively. For initial proposals of Boolean-LDA definitions, the frequency of LDA was as follows: 52.8% (2577) for Boolean-LDA2, 65.2% (3182) for Boolean-LDA3, 73.5% (3588) for Boolean-LDA4, and 80.7% (3937) for Boolean-LDA5 (Fig. 1). When assessing the best cutoff for concordance of index-based LDA and Boolean-defined LDA, we found that high concordance rates with SDAI- or CDAI-based LDA were observed in Boolean-LDA3 (SDAI: kappa = 0.796; CDAI: kappa = 0.771) and Boolean-LDA4 (SDAI: kappa = 0.807; CDAI: kappa = 0.794) (Fig. 2). Similar findings were observed in separate analysis of either early or established RA patients (Fig. 2). Besides, we also compared the concordance across LDA criteria based on 500 initial visits among RA patients in the analysis cohort, yielding similar results (Supplementary Fig. S1).
Rates of low disease activity assessed by SDAI, CDAI, initial proposed Boolean definition, using a cutoff in steps of 1 from 2 to 3, 4, 5 (Boolean-LDA2/3/4/5), and modified Boolean definition by increasing the cutoff of the PGA by 0.5-cm increments from 3.5 cm to 5.0 cm (Boolean-LDA3(PGA3.5/4.0/4.5/5.0)) or replacement of PGA with EGA using cutoff of 3.0 cm (Boolean-LDA3(EGA3.0)). SDAI Simplified Disease Activity Index, CDAI Clinical Disease Activity Index, PGA patient’s global assessment, EGA evaluator’s global assessment
The agreement in included visits between initial proposed Boolean definition of LDA, using a cutoff in steps of 1 from 2 to 3, 4, 5 (Boolean-LDA2/3/4/5) and SDAI- or CDAI-based LDA. a The concordances and discordances. b Kappa value. LDA low disease activity, SDAI Simplified Disease Activity Index, CDAI Clinical Disease Activity Index
Previous studies have indicated residual SJC was most closely associated with the radiographical progression in RA patients [13, 14, 21, 22]. We therefore compared the distribution of residual SJC between SDAI or CDAI-based LDA and proposed Boolean definition of LDA (Fig. 3). When SDAI (CDAI)-defined LDA was achieved, the proportion of SJC = 1, SJC = 2 and SJC ≥ 3 was 14.16% (14.22%), 6.67% (7.26%), and 2.59% (2.95%), respectively. As expected, the residual SJC of Boolean-LDA increased with the cutoff increment and most similar distribution of SJC was observed between index-based LDA and Boolean-LDA3 (13.55% of SJC = 1; 7.17% of SJC = 2; 2.36% of SJC = 3) (Fig. 3). Taken together, Boolean-LDA3 showed great performance in defining LDA.
The distribution of swollen joint count in the included clinic visits meeting low disease activity based on SDAI, CDAI, and initial proposed Boolean definition, using a cutoff in steps of 1 from 2 to 3, 4, 5 (Boolean-LDA2/3/4/5). LDA low disease activity, SDAI Simplified Disease Activity Index, CDAI Clinical Disease Activity Index
The Reasons for Discordance Between Boolean-LDA3 and SDAI-LDA
Of 4881 included visits, a total of 431 discordances were observed, with meeting SDAI-LDA but not Boolean-LDA3 in 380 visits and meeting Boolean-LDA3 but not SDAI-LDA 51 visits. Subsequently, the reasons for meeting SDAI-LDA but not Boolean-LDA3 were analyzed. Of 380 discordances, the most common reason was higher PGA score (239; 62.9%), followed by higher TJC (87; 23.0%), CRP (39; 10.3%), and SJC (36; 9.5%) (Supplementary Fig. S2). For the higher PGA score, there were 137 times of 3.1–4.0, 86 times of 4.1–5.0, and 16 times of over 5.0 (Supplementary Fig. S2). On the other hand, there was a total of 51 visits meeting Boolean LDA3 criteria but not SDAI-LDA. The mean SDAI for the visits meeting Boolean LDA3 criteria but not SDAI-LDA was 12.2, ranging from 11.1 (SJC28 of 1, TJC28 of 2, PGA of 3, EGA of 3, and CRP of 1.18) to 14.6 (SJC28 of 3, TJC28 of 3, PGA of 3, EGA of 3, and CRP of 2.61).
Further Modification of Boolean-LDA3
Accordingly, the further modifications of PGA for Boolean-LDA3 were made by increasing the cutoff of the PGA criterion stepwise by 0.5 increments from 3.5 to 5.0 (Boolean-LDA3(PGA3.5/4.0/4.5/5.0)) or replacement of PGA with EGA using cutoff of 3.0 (Boolean-LDA3 (EGA3.0)).
For modified proposals of Boolean-LDA3, the frequency of included visits was 65.4% for Boolean-LDA3 (PGA3.5), 69.1% for Boolean-LDA3 (PGA4.0), 69.2% for Boolean-LDA3 (PGA4.5), 72.3% for Boolean-LDA3 (PGA5.0) and 70.7% for Boolean-LDA3 (EGA3.0) (Fig. 1). Highest consistency was reached with Boolean-LDA3 (EGA3.0) (SDAI: kappa = 0.851; CDAI: kappa = 0.825) (Fig. 4). Similar findings were detected either in early RA (SDAI: kappa = 0.833; CDAI: kappa = 0.805) or established (SDAI: kappa = 0.863; CDAI: kappa = 0.837) (Fig. 4). The additional comparisons of the concordance across LDA criteria based on 672 initial visits among RA patients were made in analysis cohort, yielding similar results (Supplementary Fig. S3). Meanwhile, exclusively increasing PGA cutoffs or replacement of PGA with EGA using cutoff of 3.0 on basis of Boolean-LDA3 did not substantially impact the pattern of residual SJC compared with Boolean-LDA3 (Fig. 5). Therefore, Boolean-LDA3 (EGA3.0) exhibited the greatest clinical utility in defining LDA.
The agreement in included visits between SDAI- or CDAI-based LDA and modified Boolean definition by increasing the cutoff of the PGA by 0.5 cm increments from 3.5 cm to 5.0 cm (Boolean-LDA3(PGA3.5/4.0/4.5/5.0)) or replacement of PGA with EGA using cutoff of 3.0 cm (Boolean-LDA3(EGA3.0)). a The concordances and discordances; b kappa value. LDA low disease activity, SDAI Simplified Disease Activity Index, CDAI Clinical Disease Activity Index, PGA patient’s global assessment, EGA evaluator’s global assessment
The distribution of swollen joint count in the included clinic visits meeting low disease activity based on SDAI, CDAI, and modified Boolean definition by increasing the cutoff of the PGA by 0.5-cm increments from 3.5 to 5.0 cm (Boolean-LDA3(PGA3.5/4.0/4.5/5.0)) or replacement of PGA with EGA using cutoff of 3.0 cm (Boolean-LDA3(EGA3.0)). LDA low disease activity, SDAI Simplified Disease Activity Index, CDAI Clinical Disease Activity Index, PGA patient’s global assessment, EGA evaluator’s global assessment
Validation Analysis
Finally, we validated our results in a randomly generated internal cohort, which included 449 RA patients with 3306 visits. Their baseline characteristics are shown in Table 1. In the validation cohort, high concordance rates and most similar pattern of SJC with SDAI or CDAI definition of LDA were achieved with Boolean-LDA3 (SDAI: kappa = 0.802; CDAI: kappa = 0.791 for all patients; SDAI: kappa = 0.785; CDAI: kappa = 0.780 for early RA; SDAI: kappa = 0.810; CDAI: kappa = 0.797 for established RA) and further modification with a substitute EGA for PGA provided best agreement with either SDAI or CDAI definition of LDA (SDAI: kappa = 0.849; CDAI: kappa = 0.836 for all patients; SDAI: kappa = 0.830; CDAI: kappa = 0.819 for early RA; SDAI: kappa = 0.861; CDAI: kappa = 0.846 for established RA) (Supplementary Fig. S4–5).
Discussion
To our knowledge, this is the first study aiming to propose Boolean-defined LDA and test its utility in RA. Based on the large real-world cohort of early and established RA patients in our center, we proposed the initial and modified Boolean-LDA, and further tested their performance in comparison with SDAI- and CDAI-based LDA, which are frequently applied in current daily practice. Moreover, we also compared the SJC patterns in the clinic visits meeting the corresponding LDA definitions.
Generally, Boolean-defined LDA with a cutoff of 3 showed high consistency and similar SJC distribution to the SDAI- or CDAI-defined LDA in our cohort. Further analysis of the reasons for the discordances between Boolean-LDA3 and SDAI-LDA suggested over half of the discordances were attributable to the higher PGA, mostly ranging from 3.1 to 5.0. Accordingly, the targeted modifications of PGA were designed by increasing the cutoff of the PGA criterion stepwise by 0.5 increments from 3.5 to 5.0, and replacing PGA by EGA using cutoff of 3.0. The results showed great concordance rates with similar pattern of residual SJC were achieved when exclusively increasing PGA cutoffs to 4.0, 4.5 or replacing PGA by EGA with cutoffs to 3.0. In fact, although Boolean definition of remission seems to be most strict, it has also been criticized. Patients with no inflamed joints and a normal CRP often however with PGA exceeding the cutoff of 1 are rated as non-remission [23]. Previous clinical research found patients in SDAI or CDAI remission however not Boolean remission had higher PGA compared with patients in Boolean remission [24]. In a recent study pooling six different large clinical trials of 1680 early and established RA, Studenic et al. found increasing PGA cutoff to 1.5 or 2.0 would provide high consistency between Boolean remission and SDAI-based remission [25]. Similarly, in the present study, we found the most common reason for meeting SDAI-LDA but not Boolean-LDA3 was higher PGA, mostly ranging from 3.1 to 5.0. Further modifications indicated great agreement with a similar pattern of SJC was reached when increasing PGA cutoffs to 4.0, 4.5 or replacing PGA by EGA with cutoffs to 3.0.
LDA is an acceptable therapeutic goal, particularly in long-standing disease. The corresponding analyses were separately performed in both early and established RA population and yielded similar findings, which supports the potential clinical utility of the Boolean-defined LDA presented in the present study. In addition, subsequent validation in a randomly generated internal cohort of 449 RA patients with similar findings supported the validity of the Boolean-LDA with a substitute EGA for PGA using cutoff of 3. In summary, the agreement was almost great and the distribution of residual SJC was similar among CDAI-LDA, SDAI-LDA, and Boolean-LDA with cutoff of 3, especially increasing PGA cutoffs to 4.0, 4.5 or replacing PGA by EGA with cutoffs to 3.0. Our study, for the first time, proposed the definition of Boolean LDA, and could help promote the adoption of Boolean definition in daily practice.
There are several potential weaknesses of this study that should be acknowledged. No radiographic or functional assessment was analyzed in this study, which may weaken the strength of the proposed Boolean definition of LDA. In consideration of the association between residual SJC and radiographic progression according to previous studies [13, 14, 21, 22], we further compared the distribution of SJC in the clinic visits meeting LDA based on the corresponding LDA definitions, and yielded similar pattern of residual SJC. This finding may strengthen the clinical utilization of the proposed Boolean-defined LDA. Of course, the impact of proposed Boolean-LDA on radiographic and physical outcomes definitely needs to be further validated in future studies. On the other hand, although subgroup analyses according to diseases course and internal validation analysis were performed in the present study, the findings were solely on basis of single-center longitudinal cohort of unselected RA population, which may limit the external generalization of the present results. Therefore, extended studies are warranted to prove these findings in other ethnicities or regions in the future. In addition, this paper represents a proof-of-concept study. The weight of the core set variables of diseases activity requires more discussion. Therefore, future studies are expected to optimize Boolean LDA definition on the basis of radiographic and functional outcomes.
Conclusions
In conclusion, our findings suggest that Boolean-LDA with cutoff of 3 leads to great agreement and most similar residual SJC pattern with the SDAI- and CDAI-based definition of LDA, especially when exclusively increasing PGA cutoffs to 4.0, 4.5 or replacing PGA by EGA with cutoffs to 3.0. This needs to be replicated in other settings and can be used in the management of RA patients in daily practice.
References
Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 2016;388:2023–38.
Safiri S, Kolahi AA, Hoy D, et al. Global, regional and national burden of rheumatoid arthritis 1990–2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis. 2019;78:1463–71.
Ramiro S, Landewé RB, van der Heijde D, et al. Is treat-to-target really working in rheumatoid arthritis? A longitudinal analysis of a cohort of patients treated in daily practice (RA BIODAM). Ann Rheum Dis. 2020;79:453–9.
Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79:685–99.
Xie W, Li J, Zhang X, et al. Trends in the activity of rheumatoid arthritis as the consequence of treat-to-target strategy: eight-year data from 2009 to 2016. Clin Exp Rheumatol. 2018;36:820–8.
Brinkmann GH, Norvang V, Norli ES, et al. Treat to target strategy in early rheumatoid arthritis versus routine care—a comparative clinical practice study. Semin Arthritis Rheum. 2019;48:808–14.
Nikiphorou E, Norton SJ, Carpenter L, et al. Remission vs low disease activity: function, quality of life and structural outcomes in the Early Rheumatoid Arthritis Study and Network. Rheumatology (Oxford). 2020;59:1272–80.
Fransen J, Creemers MC, Van Riel PL. Remission in rheumatoid arthritis: agreement of the disease activity score (DAS28) with the ARA preliminary remission criteria. Rheumatology (Oxford). 2004;43:1252–5.
Smolen JS, Breedveld FC, Schiff MH, Kalden JR, Emery P, Eberl G, et al. A Simplified Disease Activity Index for rheumatoid arthritis for use in clinical practice. Rheumatology (Oxford). 2003;42:244–57.
Aletaha D, Nell VP, Stamm T, et al. Acute phase reactants add little to composite disease activity indices for rheumatoid arthritis: validation of a clinical activity score. Arthritis Res Ther. 2005;7:R796–806.
Fleischmann R, Strand V, Wilkinson B, et al. Relationship between clinical and patient-reported outcomes in a phase 3 trial of tofacitinib or MTX in MTX-naive patients with rheumatoid arthritis. RMD Open. 2016;2:e000232.
Xie W, Li J, Zhang Z. The impact of different criteria sets on early remission and identifying its predictors in rheumatoid arthritis: results from an observational cohort (2009–2018). Clin Rheumatol. 2020;39:381–9.
Aletaha D, Smolen JS. Joint damage in rheumatoid arthritis progresses in remission according to the disease activity score in 28 joints and is driven by residual swollen joints. Arthritis Rheum. 2011;63:3702–11.
Schoels M, Alasti F, Smolen JS, et al. Evaluation of newly proposed remission cut-points for disease activity score in 28 joints (DAS28) in rheumatoid arthritis patients upon IL-6 pathway inhibition. Arthritis Res Ther. 2017;19:155.
Felson DT, Smolen JS, Wells G, et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 2011;63:573–86.
Xie W, Li J, Zhang X, et al. Sustained clinical remission of rheumatoid arthritis and its predictive factors in an unselected adult Chinese population from 2009 to 2018. Int J Rheum Dis. 2019;22:1670–8.
Zhang H, Zhang H, Gao D, et al. Overlapping Sjogren’s syndrome reduces the probability of reaching target in rheumatoid arthritis patients: a propensity score matched real-world cohort from 2009 to 2019. Arthritis Res Ther. 2020;22:100.
Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24.
Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Van Leeuwen MA, van der Heijde DM, van Rijswijk MH, et al. Interrelationship of outcome measures and process variables in early rheumatoid arthritis: a comparison of radiologic damage, physical disability, joint counts, and acute phase reactants. J Rheumatol. 1994;21:425–9.
Smolen JS, van der Heijde DM, St. Clair EW, et al. Predictors of joint damage in patients with early rheumatoid arthritis treated with high‐dose methotrexate with or without concomitant infliximab: results from the ASPIRE trial. Arthritis Rheum 2006; 54:702– 10.
Studenic P, Smolen JS, Aletaha D. Near misses of ACR/EULAR criteria for remission: effects of patient global assessment in Boolean and index-based definitions. Ann Rheum Dis. 2012;71:1702–5.
Aletaha D, Wang X, Zhong S, et al. Differences in disease activity measures in patients with rheumatoid arthritis who achieved DAS, SDAI, or CDAI remission but not Boolean remission. Semin Arthritis Rheum. 2020;50:276–84.
Studenic P, Felson D, de Wit M, et al. Testing different thresholds for patient global assessment in defining remission for rheumatoid arthritis: are the current ACR/EULAR Boolean criteria optimal? Ann Rheum Dis. 2020;79:445–52.
Acknowledgements
We thank the participants of the study.
Funding
This work and the journal’s Rapid Service Fee were supported by the National Natural Science Foundation of China (grant number: 81771740, 81971524).
Authorship
All named authors meet the International Committee of Medical Journal. Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Wenhui Xie, Guangtao Li, Hong Huang, and Zhuoli Zhang have nothing to disclose.
Prior Presentation
A pre-print of this work has been released at Research Square (Xie et al., 02 Nov 2020), available at http://dx.doi.org/10.21203/rs.3.rs-98323/v1
Compliance with Ethics Guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This retrospective study was approved by the Institutional Review Board (IRB) of the Peking University First Hospital (IRB number 2014–785). The participants provided their written informed consent to participate in this study.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xie, W., Li, G., Huang, H. et al. How to Define Boolean Low Disease Activity in Rheumatoid Arthritis: Experience from a Large Real-world Cohort. Rheumatol Ther 8, 289–301 (2021). https://doi.org/10.1007/s40744-020-00270-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-020-00270-z