Abstract
Introduction
Treatment strategies to improve clinical outcomes in Takayasu's arteritis (TA) with coronary lesions have ranged from pharmacological therapy to invasive procedures, such as coronary angioplasty, stenting, and surgery. However, the therapeutic strategy for this kind of patient is still unclear. This study aimed to investigate the clinical characteristics and influence of revascularization versus medical therapy in TA patients with coronary artery involvement.
Methods
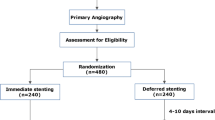
We analyzed the medical records of 806 TA patients between January 2008 and December 2019. Clinical features and treatment were analyzed, and patients were categorized into medical treatment and revascularization. Additionally, patients were sorted as percutaneous coronary intervention (PCI) and coronary artery bypass surgery (CABG) based on the strategy of revascularization.
Results
Ninety cases with coronary lesions induced by TA were enrolled. Among 90 cases, 39 patients adopted conservative treatment, and 51 patients received revascularization (28 subjects with PCI, 23 participants with CABG). The median follow-up time was 63 (45–91) months. There is no significant difference in cardiovascular death between medical treatment and revascularization (2/39, 5.1% vs. 5/51, 9.8%, P = 0.971). The analysis of subgroup indicated that the mortality caused by cardiovascular disease was also similar in the CABG and PCI (2/28, 7.1% vs. 3/23, 13.0%, P = 0.772). However, the proportion of restenosis is much higher in the PCI compared with that of CABG (39.3%, 8.7%, P = 0.022, respectively). Heart failure is an independent predictor of death in these patients.
Conclusions
There is no significant difference in cardiovascular death between medical treatment and revascularization. The analysis of the subgroup indicated that the mortality caused by cardiovascular disease was also similar in the CABG and PCI, but the restenosis is much higher in the PCI compared with that of CABG. Heart failure is an independent predictor of death in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Coronary artery involvement significantly increases mortality of patients with Takayasu's arteritis (TA), however, the optimal therapeutic strategy for this condition has not been well established. |
What was learned from the study? |
According to our data, there is no significant difference in cardiovascular death between medical treatment and revascularization. |
Besides, the analysis of subgroup indicated that the mortality caused by cardiovascular disease was also similar in the coronary artery bypass surgery (CABG) and percutaneous coronary intervention (PCI), but the restenosis is much higher in the PCI compared with that of CABG. |
Heart failure is an independent predictor of death in these patients. Our results contribute to knowledge about management of this rare type of vasculitis, providing a detailed descriptive analysis of clinical factors and treatments. |
These findings could help guide the clinician in decision-making when a vascular procedure is being considered. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13160036.
Introduction
Takayasu's arteritis (TA) is a rare chronic nonspecific vasculitis that predominantly affects the aorta and its main branches, including pulmonary and coronary arteries [1]. The majority of cases are female, with a relatively young age, usually between 20 and 40 years. The exact mechanism of this disease is still unknown. Due to the lack of specific symptoms, early diagnosis of TA remains a huge challenge for most clinicians. Coronary arterial involvement is not rare in TA and is observed in approximately 10–20% in angiographic imaging [2]. Actually, the incidence of coronary artery disease (CAD) associated with TA is likely to be underestimated, as many patients with TA do not undergo coronary angiography assessment. Among these involved coronary lesions, ostial stenosis of the left main coronary artery and/or right coronary artery are the most common lesions, with a proportion of 87.5% [2]. The optimal therapeutic strategy is a difficult task in TA, especially the monitoring of disease activity. The best treatment option for coronary lesions induced by TA has not been established. The treatment regime to improve the prognosis of CAD patients with TA includes medications (steroid and/or immunosuppressive agents), coronary balloon dilation and stents, as well as coronary artery bypass grafting. It should be emphasized, however, that there is currently no consensus or guidelines regarding the treatment of CAD related to TA. Some case studies have indicated that inflammatory coronary stenosis could be reversible by medical treatment, and we may avoid early intervention revascularization for CAD in TA [3, 4]. For a long time, coronary artery bypass surgery (CABG) has been considered to be the only option available to treat such subjects with TA after failure of medicine. However, with the advances of percutaneous interventional therapy, in addition to coronary balloon angioplasty, percutaneous coronary stenting may be used as an alternative to CABG, however in-stent restenosis is still a major concern in terms of long-term outcomes [5, 6]. Of note, a high restenosis rate does not mean a poor long-term prognosis. There is no unequivocal therapy for coronary arterial lesions for favorable long-term prognosis in CAD patients with TA. In addition, the choice of a patient’s treatment depends not only on the location and severity of the coronary lesions but also on the clinical situation such as the patient’s willingness or economic conditions. There are currently scarce data on the comparison of medical treatment and revascularization in TA patients with coronary involvement. Our hospital is a national center focused on cardiovascular disease, so many patients with severe and unusual cardiovascular diseases are admitted to our center, including TA patients with CAD. Therefore, we believe that analyzing the data of these patients enables providing some valuable clinical treatment recommendations for patients with TA involving coronary lesions. The aims of the present study were to (1) compare the long term outcomes in TA patients involved coronary lesions who received revascularization or medical Therapy, (2) evaluate the results of TA patients involving coronary lesions with open surgery or endovascular intervention.
Methods
Design and Setting
From January 2008 to December 2019, we conducted a retrospective study and reviewed the electronic medical records of patients with a diagnosis of TA who were admitted to our hospital. The present study was approved by the Ethics Committee of Fuwai Hospital and was conducted in accordance with the second Declaration of Helsinki. Informed consent of the patients was exempted from IRB because the study collected data retrospectively, and all personal information was removed and not associated with personal identity.
Selection of Patients
TA cases were collected electronically via the information systems of our hospital using The International Classification of Diseases Tenth Revision (ICD-10) code for TAK. The diagnosis of TA according to the 1990 American College of Rheumatology (ACR) criteria was confirmed [7]. The subjects with TA involving coronary lesions detected by coronary angiography (CAG) were enrolled. These participants were divided into a revascularization group and a medical therapy group. Based on the strategy of revascularization, patients were sorted as a percutaneous coronary intervention (PCI) group and a CABG group for subgroup analysis.
Data Collection
Demographic data including age, sex, medical history, current medicine, lifestyle habits, height (cm), and weight (kg), and clinical manifestations, physical examination, laboratory tests, coronary angiographic findings, interventions measure, and open surgery were recorded and analyzed. CAD is defined as more than 50% reduction of diameter in more than one major coronary artery. The results of CAG were also classified into three types: type 1, stenosis or occlusion of the coronary ostia and the proximal segments of the coronary arteries; type 2, diffuse or focal coronary arteritis, which may extend diffusely to all epicardial branches or may involve focal segments; and type 3, coronary aneurysm [8]. CAD severity was calculated by the SYNTAX II Score. The SYNTAX II Score was measured by an intervention cardiologist that was blinded to the outcomes of patients. All the data used in the present study were mutually checked by two researchers to guarantee their accuracy and completeness.
Risk Factor Definitions
Hypertension was diagnosed as a resting blood pressure > 140 mmHg for systolic blood pressure and/or > 90 mmHg for diastolic blood pressure measured with an appropriate cuff size on two different days and/or current use of antihypertensive medications. Hyperlipidemia was defined as current use of cholesterol-lowering medications and/or a total cholesterol value > 200 mg/dl, triglycerides > 150 mg/dl) low-density lipoprotein cholesterol (LDL-C) > 130 mg/dl in a plasma sample drawn after an overnight fast. Diabetes mellitus was confirmed if a patient had a history of a fasting blood glucose level > 125 mg/dl or used insulin and/or oral antidiabetic agents. Renal dysfunction was defined as estimated glomerular filtration rate (eGFR) < 90 ml/min/1.73 m2. Smokers were defined as current smoking or with a severe history of smoking.
Treatment and Follow-Up
The choice of treatment regimen was determined by the doctor in charge and patient’s treatment willingness. Evaluation of inflammation activity in TA patients is challenging, and there is no consensus on the definition of disease activity. Clinical symptoms coupled with erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), as well as radiological imaging (e.g., CT angiography, magnetic resonance angiography, 18F-FDG positron emission tomography), are used for assessment of disease activity [9, 10]. The active status with disease activity was categorized as satisfying one of the criteria of (i) an elevated ESR (≥ 21 mm/h) or CRP (≥ 0.9 mg/dl) level, (ii) a thickened arterial wall (≥ 3 mm) with mural enhancement on either CT angiography; (iii) increased FDG uptake in the aortic arch and epiaortic arteries. Patients should receive immunosuppressive therapy if inflammation of TA is active before revascularization except in cases of emergency surgery. Based on our experience, corticosteroids are the first-line treatment for control of active inflammation, with suggested initial dosages of 0.5–1 mg/kg/day. All patients confirmed with TA were given glucocorticoids. If necessary, corticosteroids are used in combination with immunosuppressants. Other treatments follow the CAD guidelines. Follow-up visits were scheduled at 6 and 12 months, and then each year following discharge. Blood routine, renal function, CRP, and ESR were monitored. If patients had symptoms associated with myocardial ischemia, CAG or coronary CT imaging were performed. Restenosis was considered as a recurrence of pectoris angina and residual diameter stenosis > 50% confirmed by CAG.
Outcome Measures
The primary outcome was the mortality caused by cardiac diseases, since the coronary lesions were detected by CAG. The second outcome was composite events (or major cardiovascular adverse events, MACE), which included death from cardiovascular causes, myocardial infarction, stroke, hospitalization for angina or heart failure, and repeat coronary artery revascularization.
Statistical Analysis
Continuous variables with normal distribution are expressed as mean with standard deviation, and continuous variables without normal distribution are expressed as median (interquartile range), whereas categorical variables are reported as absolute numbers and percentages. Differences between groups were tested by independent t test or Mann–Whitney U test. Comparisons between groups were made using Chi-square tests for categorical data. Fisher’s exact tests were conducted if the expected frequencies were less than 5. Mortality rates or composite events were estimated by the Kaplan–Meier method, and differences between groups were assessed by means of the log-rank test. The univariate and multivariate Cox proportional regression hazard models were used to analyze the independent risk factors related to mortality or composite events. A two-sided P value less than 0.05 was considered to be statistically significant. Statistical analysis was performed with SPSS software (version 18; SPSS, Chicago, IL, USA).
Results
Demographic Data and Clinical Features
We analyzed the medical records of 806 TA patients. Ninety patients who underwent CAG with chest pain, chest tightness, heart failure, fatigue, or syncope were enrolled. The prevalence of coronary lesions in TA patients was 11.2%. The clinical characteristics are depicted in Table 1. The median follow-up time was 63 (45–91) months. The male-to-female ratio of this study was 1:3.6 (71 female, 20 male), with a mean age of 47.5 years. Among the 90 TA patients with coronary lesions, 39 adopted conservative drug treatment, and 51 received revascularization (28 subjects with PCI, 23 participants with CABG). One patient in the conservative treatment received revascularization for worsened symptoms. There were no significant differences regarding gender, age, comorbidities, ESR, CRP, disease activity, left ventricular ejection fraction (LVEF), and estimated glomerular filtration rate (eGFR).
Characteristics of Coronary Involvement and Distributions
The detailed distribution of coronary involvement is summarized in Table 2. The ostial and proximal segments of coronary lesions were most frequently involved 77 patients (77/90, 85.6%; 31/39, 79.5% vs. 46/51, 90.2%, P = 0.152), and 15 subjects (15/90, 16.7%; 5/39, 12.8% vs. 10/51, 19.6%, P = 0.392) with distal segments. Only one patient had coronary aneurysms. Of these subjects, 43 patients (43/90, 47.8%; 16/39, 41.0% vs. 27/51, 52.9%, P = 0.262) were involved the left main coronary artery (LMCA), 52 subjects (52/90, 57.8%; 18/39, 46.2% vs. 34/51, 66.7%, P = 0.051) with left anterior descending coronary artery (LAD) involvement and 59 participants (65.6%; 20/39, 51.3% vs. 39/51, 76.5%, P = 0.013) had right coronary artery (RCA) lesions. It was similar in single-vessel disease and double-vessel disease, but triple-vessel disease in the revascularization group is higher than that of medical treatment group. However, there was no significant difference in the severity of coronary lesions assessed by SYNTAX II score between groups.
TA-Related Revascularization and Medicine
In this study, 23 patients received CABG, 28 participants with PCI, and the remaining 39 subjects adopted conservative drug treatment. During follow-up, there were five patients in the CABG group that developed exertional angina and 11 participants in the PCI group. Of these patients, two subjects received interventional treatment for bridge-stenosis, three failed to revascularize in the CABG group, and 11 underwent revascularization for in-stent restenosis. To our surprise, the proportion of patients who insisted on long-term oral glucocorticoid is relatively low (38.5% in the conservative group vs. 47.1% in the revascularization group, P = 0.415).
Mortality Rate and Cause of Death and Predictors Associated With Death
Two patients died in the medical treatment group (one from acute myocardial infarction and another from heart failure) and five died in the revascularization group (one from acute thrombosis after coronary artery stenting, four from heart failure, two in the PCI group and three in the CABG group). Kaplan–Meier survival analysis showed that it was similar between medical treatment and revascularization group (Fig. 1). Although mortality had no significance, the symptoms related to ischemia were more common in the conservative treatment group, especially in the patients without steroid and immunosuppressive agents. The univariate analysis suggested that disease activity and heart failure were associated with mortality, but multivariate Cox proportional regression hazard models indicated that heart failure was independently associated with mortality after adjustment for other risk factors (Table 3).
MACE Comparison between Medical Treatment and Revascularization Group
Table 4 summarizes the MACE outcomes between the medical treatment and revascularization groups. There were no significant differences in MI, stroke, heart failure, and cardiac death, except for revascularization. Kaplan–Meier analysis showed that MACE is similar between groups (P = 0.110, Fig. 2).
Subgroup Analysis of PCI and CABG
The baseline characteristics regarding PCI and CABG are summarized in Table 5. The CABG group had a higher proportion of MI and a lower LVEF compared to the PCI group, and other features such as age, comorbidities, ESR, CRP, disease activity, eGFR, and medications were similar. Kaplan–Meier analysis indicated that there was no significant difference in the event-free survival between the PCI group and the CABG group (Fig. 3). Table 6 describes the MACE between subgroups. The percentage of MI, stroke, heart failure, and cardiac death showed no differences. However, the proportion of revascularization in the PCI group was much higher than that of the CABG group (P = 0.022). Kaplan–Meier analysis indicated that MACE (composite events) in the CABG group was significantly lower than that of PCI (Fig. 4), and multivariate Cox proportional regression hazard models suggested that heart failure and revascularization strategy was independently associated with MACE after adjustment for other risk factors (Table 7).
Discussion
In the present study, we investigated the long-term results of TA patients with coronary artery involvement with medical treatment or revascularization. We found that there is no significant difference in cardiovascular death between medical treatment and revascularization. Besides, the analysis of subgroup indicated that the mortality caused by cardiovascular disease was also similar in the CABG group and PCI group. But the proportion of restenosis is much higher in the PCI group compared with that of CABG group.
The probable mechanism of coronary artery stenosis caused by TA is the progress of chronic inflammation of the ascending aorta, which causes endothelial cell hyperplasia, contraction of the fibrotic media and adventitia. In the advanced stage, destruction of the elastic fibers in the medial wall can cause dilatation or aneurismal.
Changes [11]. According to previous studies, the prevalence was estimated that 10-20% of all TA patients have coronary artery involvement [2, 8, 12], based on autopsy and clinical diagnosis. In our study, the prevalence of coronary lesions in TA patients was 11.2%. However, not all patients with TA underwent coronary imaging evaluation. Therefore, the incidence of TA with coronary involvement is likely to be underestimated. Kang et al. have recently reported a higher incidence of coronary lesions diagnosed with CT. It is up to 53.2% [13]. It is suggested that more attention should be paid to the TA patients with CAD. Because these patients are at risk of serious complications such as death from myocardial infarction. However, seen from the criteria of the ACR for diagnosing TA, the role of coronary lesions of TA had been ignored.
According to previous reports [2, 8], coronary lesions are divided into three types based on the results of coronary angiography. Type 1 is stenosis or occlusion of the coronary ostia and the proximal segment of the coronary arteries. Type 2 is diffuse or focal coronary arteritis, which can extend to all epicardial branches or may involve focal segments (skip lesions). Type 3 is the presence of coronary artery aneurysms. Type 1 is believed to be the most common lesion, while types 2 and 3 are considered uncommon. In our study, similar to previous studies, type 1 lesions are the most common. The ostial and proximal segments of coronary lesions were involved in 77 patients (85.6%). Of note, type 2 lesions were not uncommon, and 15 subjects (16.7%) had distal segments. This result reminds us that diffuse lesions may also be caused by the TA. Only one patient had coronary aneurysms. The ostia and proximal segments of RCA, LAD, and LMCA were the most common lesions involved (65.6, 57.8, and 47.8%, respectively). Additionally, previous studies had shown that the SYNTAX score was an independent predictor of the prognosis of patients with CAD [14, 15]. However, our results did not support the previous findings. A reasonable explanation for this is that the coronary lesions involved in TA are different from CAD caused by atherosclerotic plaque. Coronary lesions could be inhibited or reversed by controlling the activity of disease with glucocorticoids and (or) immunosuppressants. On the other hand, TA patients with coronary artery involvement may have developed abundant collateral coronary circulation during the long-term chronic ischemia period.
Therapeutic strategies for TA patients with coronary involvement include medications with glucocorticoid and immunosuppressive agents, endovascular intervention, or surgical vascular reconstruction. It must be stressed, however, that there is no consensus on how coronary lesions linked to TA should be treated. Some case studies indicated that inflammatory coronary stenosis could be reversible by medical treatment, and we may avoid early intervention revascularization for coronary lesions in TA [3, 4]. These cases demonstrated that inflammatory coronary stenosis might be reversible or controlled, and we could avoid early invasive revascularization for CAD in patients with TA. There are currently scarce data on the comparison of medical treatment and revascularization in TA patients with coronary involvement, even in a small group of subjects. Our outcomes suggested that the survival was similar between the medical treatment and revascularization groups. Although mortality had no significance, the symptoms related to ischemia were more common in the conservative treatment group, especially in patients without steroids and immunosuppressive agents. Cipriano and colleagues reported that the prognosis of patients with coronary involvement who have received conservative treatment is often poor with a high risk of death caused by cardiac events [16]. However, there were no records on the medications in these patients. Additionally, there was no intervention of revascularization arms. It is hard to evaluate the outcomes of conservative treatments. With the progression of medical treatment of TA patients with coronary lesions, the prognosis of patients has been improved. Univariate analysis suggested that disease activity and heart failure were associated with mortality, but multivariate Cox proportional regression hazard models indicated that heart failure was independently associated with mortality after adjustment for other risk factors. This finding was supported by previous studies [17, 18].
In theory, fixed, irreversible coronary lesions may be amenable by revascularization procedures, with the result of low morbidity and mortality. In terms of outcomes of treatment, the traditional view is that CABG has better long-term results than PCI. Several previous studies have shown that percutaneous transluminal angioplasty with or without stenting has led to unsatisfactory results [19,20,21]. With the emergence of a new generation of drug-eluting stents, it is believed that the incidence of restenosis may be significantly reduced. Recently, Wang et al. [6] and Yang et al. [22] reported long-term results regarding the comparison of CABG and PCI. In the first study, a high rate of restenosis was observed following PCI (63.2%), despite the use of new drug-eluting stents (rapamycin in seven cases, zotarolimus in three cases, and paclitaxel in two cases) when compared with CABG (25.0%) at a median follow-up time of 101 months [6]. The second study found that the incidence of MACE was higher in the PCI group than CABG group during the median follow-up of 48 months, especially in those who underwent intervention during disease activity. However, for patients with stable arteritis, the long-term efficacy of PCI is similar to that of CABG [22]. Our subgroup analysis indicated that the survival rate had no significant difference between PCI and CABG, but the MACE (composite events) in the CABG group was significantly lower than that of the PCI group. The difference is mainly due to restenosis after revascularization. The rate of restenosis was 39.3% in the PCI group and 8.7% in the CABG group (P = 0.022), but sometimes we often encounter severe calcification in the aorta in patients with TA. For such patients, PCI could be an alternative treatment strategy for CABG. It was worth noting that there were five patients with uncontrolled disease activity in those with restenosis. This suggests that it is necessary to control the disease activity for prevention of in-stent restenosis, which is in line with previous research [23]. Interestingly, two patients in the PCI group had normal levels of ESR and CRP with prednisone and cyclophosphamide, but in-stent restenosis still occurred repeatedly. This implies that the pathophysiological mechanism of TA involving coronary arteries is more complicated than we thought. We need to explore new biomarkers for monitoring disease activity, and more sensitive, specific, and targeted medical drugs in the future study. Several candidates have been investigated, including serum autoantibodies, interleukins (ILs), vascular endothelial growth factor (VEGF), matrix metalloproteinase (MMPs), pentraxin 3 (PTX3), as well as adipokines [24]. What is more, FDG-PET examination may play an important role in early diagnosis and for monitoring disease activity. The SUV ratio cutoff for determining TA activity was 1.27 with a sensitivity and specificity of 79.3 and 100.0%, respectively [25].
Limitations
First, this is a retrospective cohort study. Second, it was based on a single-center database. However, as a national research center for TA, our patients come from all over the country. The sample size we enrolled is large enough to represent the characteristics of TA patients with coronary artery involvement. The strengths of our study include a large cohort of patients with TA who have undergone medical treatment or revascularization (PCI or CABG) and have a long-term follow-up outcome.
Conclusions
The present study data indicate that there is no significant difference in cardiovascular death between medical treatment and revascularization. Besides, the analysis of subgroup indicated that the mortality caused by cardiovascular disease was also similar in the CABG group and PCI group, but the proportion of restenosis is much higher in the PCI group compared with that of CABG group. Heart failure is an independent predictor of death in these patients. The current challenges we face in treating this condition mainly include a lack of awareness of early diagnosis, delays in diagnosis due to various clinical manifestations, and limited disease activity assessment methods.
References
Mason JC. Takayasu arteritis–advances in diagnosis and management. Nat Rev Rheumatol. 2010;6:406–15.
Endo M, Tomizawa Y, Nishida H, Aomi S, Nakazawa M, Tsurumi Y, Kawana M, Kasanuki H. Angiographic findings and surgical treatments of coronary artery involvement in Takayasu arteritis. J Thorac Cardiovasc Surg. 2003;125:570–7.
Iga K, Gohma I, Hori K. Regression of the left main trunk lesion by steroid-administration in Takayasu aortitis. Chest. 1991;99:508–10.
Isomatsu Y, Hoshino S, Tsukui H, Hara M, Nishiya Y, Ishikawa T. Regression of left main coronary ostium stenosis after surgical revascularization and steroid therapy. Jpn J Thorac Cardiovasc Surg. 2000;48:594–6.
Furukawa Yutaka, Tamura Toshihiro, Toma Masanao, Abe Mitsuru, Saito Naritatsu, Ehara Natsuhiko, et al. Sirolimus-eluting stent for in-stent restenosis of left main coronary artery in Takayasu arteritis. Circ J. 2005;69:752–5.
Wang X, Dang A, Lv N, Cheng N, Cheng X, Yang Y, et al. Long-term outcomes of coronary artery bypass grafting versus percutaneous coronary intervention for Takayasu arteritis patients with coronary artery involvement. Semin Arthritis Rheum. 2017;47:247–52.
Fries JF, Hunder GG, Bloch DA, Michel BA, Arend WP, Calabrese LH, et al. American College of Rheumatology 1990 criteria for the classification of vasculitis. Summary. Arthritis Rheum. 1990;33:1135–6.
Matsubara O, Kuwata T, Nemoto T, Kasuga T, Numano F. Coronary artery lesions in Takayasu arteritis: pathological considerations. Heart Vessels Suppl. 1992;7:26–31.
Saadoun D, Lambert M, Mirault T, Resche-Rigon M, Koskas F, Cluzel P, et al. Retrospective analysis of surgery versus endovascular intervention in Takayasu arteritis: a multicenter experience. Circulation. 2012;125:813–9.
Fields CE, Bower TC, Cooper LT, Hoskin T, Noel AA, Panneton JM, et al. Takayasu’s arteritis: operative results and influence of disease activity. J Vasc Surg. 2006;43:64–71.
Soto ME, Espinola-Zavaleta N, Ramirez-Quito O, Reyes PA. Echocardiographic follow-up of patients with Takayasu’s arteritis: five-year survival. Echocardiography. 2006;23:353–60.
Tann OR, Tulloh RM, Hamilton MC. Takayasu’s disease: a review. Cardiol Young. 2008;18:250–9.
Kang EJ, Kim SM, Choe YH, Lee GY, Lee KN, Kim DK. Takayasu arteritis: assessment of coronary arterial abnormalities with 128-section dual-source CT angiography of the coronary arteries and aorta. Radiology. 2014;270:74–81.
Chakravarty T, Buch MH, Naik H, White AJ, Doctor N, Schapira J, et al. Predictive accuracy of SYNTAX score for predicting long-term outcomes of unprotected left main coronary artery revascularization. Am J Cardiol. 2011;107:360–6.
Caixeta A, Généreux P, Palmerini T, Lansky AJ, Mehran R, Dangas GD, et al. Prognostic utility of the SYNTAX score in patients with single versus multivessel disease undergoing percutaneous coronary intervention (from the Acute Catheterization and Urgent Intervention Triage StrategY [ACUITY] trial). Am J Cardiol. 2014;113:203–10.
Cipriano PR, Silverman JF, Perlroth MG, Griepp RB, Wexler L. Coronary arterial narrowing in Takayasu’s aortitis. Am J Cardiol. 1977;39:744–50.
Numano F. Differences in clinical presentation and outcome in different countries for Takayasu’s arteritis. Curr Opin Rheumatol. 1997;9:12–5.
Li J, Zhu M, Li M, Zheng W, Zhao J, Tian X, et al. Cause of death in Chinese Takayasu arteritis patients. Medicine (Baltimore). 2016;95:e4069.
Fava MP, Foradori GB, Garcia CB, Cruz FO, Aguilar JG, Kramer AS, et al. Percutaneous transluminal angioplasty in patients with Takayasu arteritis: five-year experience. J Vasc Interv Radiol. 1993;4:649–52.
Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takayasu arteritis. Ann Intern Med. 1994;120:919–29.
Labarca C, Makol A, Crowson CS, Kermani TA, Matteson EL, Warrington KJ. Retrospective comparison of open versus endovascular procedures for Takayasu Arteritis. J Rheumatol. 2016;43:427–42.
Yang Y, Tian T, Yang K, Zhang Y, Meng X, Fan P, et al. Outcomes of percutaneous coronary intervention and coronary artery bypass grafting in patients with Takayasu arteritis. Int J Cardiol. 2017;241:64–9.
Amano J, Suzuki A. Coronary artery involvement in Takayasu’s arteritis Collective review and guideline for surgical treatment. J Thorac Cardiovasc Surg. 1991;102:554–60.
Sun Y, Huang Q, Jiang L. Radiology and biomarkers in assessing disease activity in Takayasu arteritis. Int J Rheum Dis. 2019;22(Suppl 1):53–9.
Zhang X, Zhou J, Sun Y, Shi H, Ji Z, Jiang L. 18F-FDG-PET/CT: an accurate method to assess the activity of Takayasu’s arteritis. Clin Rheumatol. 2018;37:1927–35.
Acknowledgements
We thank Yanyan Zhao for her contribution to data analysis and Yue Chang for his SYNTAX II score assessment in this study. We thank all participants for their involvement in this study.
Funding
This study was funded by the clinical research and application associated with heart and great vessel disease (2018YFB1107102). The Rapid Service Fee was funded by the clinical research and application associated with heart and great vessel disease (2018YFB1107102).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Zhiwei Huang, Hongliang Zhang, Man Wang, Weixian Yang, Shubin Qiao, and Fenghuan Hu have nothing to disclose.
Compliance with Ethics Guidelines
The present study was approved by the Ethics Committee of Fuwai Hospital and was conducted in accordance with the second Declaration of Helsinki. Informed consent of the patients was exempted from IRB because the study collected data retrospectively, and all personal information was removed and not associated with personal identity.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Huang, Z., Zhang, H., Wang, M. et al. Revascularization Versus Medical Therapy in Takayasu's Arteritis Patients with Coronary Artery Involvement. Rheumatol Ther 8, 119–133 (2021). https://doi.org/10.1007/s40744-020-00251-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-020-00251-2