Abstract
Introduction
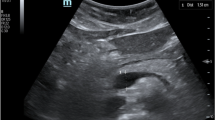
Previous studies have described techniques for performing ultrasound of the left internal thoracic artery. The purpose of this study is to assess the ability of medical students with little prior ultrasound experience to quickly find and identify the left internal thoracic artery after a brief instructional session.
Materials and Methods
Fifty-one first-year medical students were taught to perform ultrasound of the left internal thoracic artery. The instruction consisted of a 5-min didactic followed by a 2-min real-time ultrasound demonstration. Each participant was then given a maximum of 2 min to find the artery while scanning a standardized patient. A radiologist made the determination of whether or not the student pointed out the correct structure within that time period. If the student was successful, then the time to locate the artery was recorded. The students also completed a questionnaire about the ultrasound experience.
Results
Forty (78 %) of the 51 students correctly identified the artery in less than 2 min. For those students, the mean time to locate the artery was 69.5 s. Four students pointed out the incorrect structure. Seven students ran out of time before pointing out a structure. Nearly all of the students indicated that they enjoyed the experience and that it increased their interest in ultrasound.
Conclusions
This study showed that novice ultrasound users can quickly learn to locate the left internal thoracic artery with ultrasound.


Similar content being viewed by others
References
Moore KL, Dalley AF, Agur AMR. Clinically oriented anatomy. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2014. p. 2014.
Tsang TSM, Freeman WK, Sinak LJ, Seward JB. Echocardiographically guided pericardiocentesis: evolution and state-of-the-art technique. Mayo Clin Proc. 1998;73:647–52.
Tsang TSM, Enriquez-Sarano M, Freeman WK, Barnes ME, Sinak LJ, Gersh BJ, Bailey KR, Seward JB. Consecutive 1127 therapeutic echocardiographically guided pericardiocenteses: clinical profile, practice patterns, and outcomes spanning 21 years. Mayo Clin Proc. 2002;77:429–36.
Lindenberger M, Kjellberg M, Karlsson E, Wranne B. Pericardiocentesis guided by 2-D echocardiography: the method of choice for treatment of pericardial effusion. J Intern Med. 2003;253:411–7.
Fitch MT, Nicks BA, Pariyadath M, McGinnis HD, Manthey DE. Emergency pericardiocentesis. N Engl J Med. 2012;366:e17.
Kronzon I, Glassman LR, Tunick PA. Avoiding the left internal mammary artery during anterior pericardiocentesis. Echocardiography. 2003;20:533–4.
Blanco P, Volpicelli G. Looking a bit superficial to the pleura. Critical Ultrasound J. 2014;6:13.
Mehra S, Buch A, Truong CN, Moshiri M, Shriki JE, Bhargava P. Post-traumatic internal mammary artery pseudoaneurysm: a rare complication of pericardiocentesis. Radiol Case Rep. 2014; (Online)9:931.
Ehrsam J-E, Spittell PC, Seward JB. Internal mammary artery: 100 % visualization with new ultrasound technology. J Am Soc Echocardiogr. 1998;11:10–2.
Nagdev A, Mantuani D. A novel in-plane technique for ultrasound-guided pericardiocentesis. Am J Emerg Med. 2013;31:1424e5–9.
Wang V, Cheng YT, Liu D. Improving education: just-in-time splinting video. The Clinical Teacher. 2015;12:1–4.
Davis JS, Garcia GD, Wycoff MM, Alsafran S, Graygo JM, Withum KF, Schulman CI. Use of mobile learning module improves skills in chest tube insertion. J Surg Res. 2012;177:21–6.
Niles D, Sutton RM, Donoghue A, Kalsi MS, Roberts K, Boyle L, Nishisaki A, Arbogast KB, Helfaer M, Nadkarni V. “Rolling Refreshers”: a novel approach to maintain CPR psychomotor skill competence. Resuscitation. 2009;80:909–12.
Kamdar G, Kessler DO, Tilt L, Srivastava G, Khanna K, Chang TP, Balmer D, Auerbach M. Qualitative evaluation of just-in-time simulation-based learning: the learners’ perspective. Simul Healthc. 2013;8(1):43–8.
Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–57.
Lujan HL, DiCarlo SE. First-year medical students prefer multiple learning styles. Adv Physiol Educ. 2006;30(1):13–6.
Acknowledgments
The authors would like to thank Matthew Aussprung MS-4, Michael Corso MS-1, and Tyler Stoltz MS-4 for volunteering to be standardized patients for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
General Electric Healthcare through an educational partnership with the University of South Carolina, School of Medicine provides ultrasound systems and technical support for a student ultrasound curriculum.
Rights and permissions
About this article
Cite this article
Bell III, F.E., Neuffer, F.H., Rao, V.V. et al. Teaching Medical Students Left Internal Thoracic Artery Ultrasound. Med.Sci.Educ. 26, 207–211 (2016). https://doi.org/10.1007/s40670-016-0233-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-016-0233-z