Abstract
Background
Teaching cardiac ultrasound to medical students in a brief course is a challenge. We aimed to evaluate the feasibility of teaching large groups of medical students the acquisition and interpretation of cardiac ultrasound images using a pocket ultrasound device (PUD) in a short, specially designed course.
Methods
Thirty-one medical students in their first clinical year participated in the study. All were novices in the use of cardiac ultrasound. The training consisted of 4 hours of frontal lectures and 4 hours of hands-on training. Students were encouraged to use PUD for individual practice. Finally, the students’ proficiency in the acquisition of ultrasound images and their ability to recognize normal and pathological states were evaluated.
Results
Sixteen of 27 (59%) students were able to demonstrate all main ultrasound views (parasternal, apical, and subcostal views) in a six-minute test. The most obtainable view was the parasternal long-axis view (89%) and the least obtainable was the subcostal view (58%). Ninety-seven percent of students correctly differentiated normal from severely reduced left ventricular function, 100% correctly differentiated a normal right ventricle from a severely hypokinetic one, 100% correctly differentiated a normal mitral valve from a rheumatic one, and 88% correctly differentiated a normal aortic valve from a calcified one, while 95% of them correctly identified the presence of pericardial effusion.
Conclusions
Training of medical students in cardiac ultrasound during the first clinical year using a short, focused course is feasible and enables students with modest ability to acquire the main transthoracic ultrasound views and gain proficiency in the diagnosis of a limited number of cardiac pathologies.
Similar content being viewed by others
Background
The diagnosis of cardiac disease is based on medical history, physical examination, and complementary studies. The cardiovascular physical exam, based mainly on cardiac auscultation, can be performed during the first patient-doctor encounter. However, its diagnostic accuracy is suboptimal [1,2,3,4,5,6,7,8]. Some cardiovascular pathologies are difficult to identify by means of physical examination due to imperceptible or barely detectable clinical manifestations [4, 6, 9,10,11,12], with no connection to physicians’ skills. In order to improve their diagnostic capability, physicians make use of complementary diagnostic imaging techniques. Ultrasound offers precise anatomical and functional information on the cardiovascular system and is the most commonly used technique for diagnosing cardiovascular diseases [2, 6, 10, 13, 14].
Decara et al. showed that the utilization of hand-held ultrasound devices significantly augmented the accuracy of medical students’ cardiac diagnoses at the bedside compared to traditional physical examination [3]. However, the practicability of echocardiography is limited due to the cost of the device, its cumbersome size, and the lack of availability of expert personnel to perform and interpret studies.
New, small, user-friendly ultrasound equipment has been in use for the last decade. Recently, the pocket ultrasound device (PUD), with high imaging resolution, has become commercially available [14]. The PUD has the same characteristics as the traditional stethoscope routinely used by physicians in their physical examinations for the last 150 years: it is portable, free of adverse effects, and has no contraindications. The PUD allows for a quick and accurate observation of a patient’s internal structures as well as their function, and thus enhances the diagnostic potential of the “auscultation-assisted” physical examination [1,2,3,4,5, 8, 11, 14,15,16,17,18].
Acquiring ultrasound skills in medical school is vitally important, but teaching these skills presents challenges. Recently, a consensus of 34 experts in the field of ultrasound in medical education established recommended ultrasound training milestones that all medical students should reach before they graduate [19].
The main limitations of ultrasound-assisted physical examination are related to time of training until proficiency is achieved in obtaining echo views and in the ability to identify cardiac pathologies. Teaching the acquisition of cardiac ultrasound imaging is based mainly on hands-on practice in a one-on-one fashion, under the direct supervision of highly qualified instructors. This makes the teaching of large numbers of medical personnel unfeasible, primarily due to the limited number of instructors and teaching costs.
Methods
Devising a time-efficient and effective method of teaching cardiac ultrasound to larger groups is challenging, but could facilitate the incorporation of this important diagnostic modality into medical school curriculums.
Our study’s objectives were to assess the feasibility and efficacy of having novice medical students perform and read basic cardiac ultrasound studies during their first clinical rotation after participating in a newly designed, brief (eight-hour), focused cardiac ultrasound course using a PUD. Specifically, we aimed to validate this teaching method by testing whether students could achieve standard echocardiographic views and analyze basic transthoracic cardiac ultrasound images and basic cardiac pathologies.
Study population
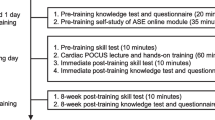
A total of 31 medical student volunteers in their first clinical year (fourth year of a six-year medical school program) were enrolled in the study. The course took place during the first 2 weeks of an eight-week internal medicine rotation. The importance of the course was conveyed to the class and the schedule was presented a month before the initiation of the rotation. Next, the students were notified simultaneously about the course and all the students agreed to participate in it. The students all signed an informed consent form. None of the students had any prior experience with the use of ultrasound, so pretesting did not appear to be necessary. The results of students’ performance in this study were not available to medical school faculty and therefore did not influence their evaluations.
The intervention
The course consisted of frontal lectures and hands-on training sessions. The course objectives were to teach students how to obtain standard cardiac ultrasound images from standard transthoracic views and how to recognize normal cardiac ultrasound anatomy as well as pathological states of the left ventricle, the right ventricle, the mitral and aortic valves, the inferior vena cava, and the pericardium.
Students’ training consisted of 4 hours of frontal lectures and an additional 4 hours of hands-on practice under the direct supervision of cardiologists and echocardiographic sonographers. The eight-hour course was incorporated into the eight-week internal medicine rotation in place of lectures that students could view independently in a pool of lectures that is available to them as e-Learning material. During their eight-week rotation, following the course, students were encouraged to use PUD autonomously (without supervision), practicing image acquisition on healthy volunteers and hospitalized patients. Students were asked to record acquired images for later revision with a tutor for feedback and skill improvement. This post-course self-training was not obligatory.
Lectures
The 4 hours of lectures were divided into two weekly sessions of 2 hours each. The subjects covered in the lectures were the following: basic ultrasound physics, principles of two-dimensional ultrasound imaging, the Doppler effect, and cardiac ultrasound anatomy from parasternal, apical, and subcostal views. Previous clinical echocardiographic cases were used to teach students pattern recognition of normal and abnormal LV and RV function, identification of aortic valve structure (normal, bicuspid, and degenerative calcified), normal mitral valve versus mitral valve with rheumatic damage, presence of pericardial effusion, and dilated versus normal IVC. Color Doppler imaging was used to teach students to identify aortic and mitral regurgitation of any degree.
Hands-on practice
During the same week the lectures were given, students had a total of 4 hours of guided hands-on training (divided into two sections of 2 hours each). Students practiced image acquisition utilizing standard ultrasound devices (Vivid 6 and Vivid I, General Electric). These devices optimized image acquisition for teaching purposes by providing a larger screen and better image quality than the pocket devices. Training sessions were led by cardiologists or echocardiographic sonographers with teaching experience on healthy student volunteers who served as models. Training was performed in small groups (up to four students) and focused on the acquisition of standard cardiac ultrasound images.
The practiced views included the parasternal long-axis view, the parasternal short-axis view (three levels: aortic, mitral, and midpapillary), the apical four-, two-, and three-chamber views (4-ch, 2-ch, 3-ch respectively), and the subcostal view. Students were taught to move the transducer with gentle maneuvers and to perform three main motions: alignment, rotation, and tilt, in order to produce the optimal image in each of the ultrasound windows. Students were also instructed to use general 2D gain and image depth controls for better ultrasound images. Figures 1, 2 and 3 show details of the anatomical points that the students had to obtain in each of the ultrasound views.
Individual practice using the pocket ultrasound device
Students were encouraged to practice image acquisition during the eight-week clinical rotation. This PUD practice was completely voluntary and no number of required practice hours was defined. Every five students were provided with a PUD (Vscan from General Electric) for individual practice. The easy-to-use device is shaped like a small flip-phone and has an attached 2.5 MHz cardiac transducer. It has a 3.5-in. display screen and weighs 390 g. With two separate control settings (depth and gain), the Vscan produces a black-and-white real-time two-dimensional ultrasound image as well as a color-coded blood flow image. Images can be frozen and simple linear measurements can be performed. All images produced with the device can be saved on the system’s memory card for later viewing and feedback.
Practice was neither predefined nor mandatory. Students performed cardiac ultrasound studies on one another as well as on their patients as part of the physical examination. We therefore advised our students to inform the patients they examined that the ultrasound study they performed did not in any way replace a comprehensive echocardiographic study, and that no diagnosis or clinical decision would be made based on it.
Post-intervention assessment
At the end of the eight-week clinical rotation, enrolled students underwent two exams. The first was designed to assess hands-on cardiac ultrasound image acquisition of the main transthoracic views (the six-minute exam, see below), while the second aimed to validate their abilities to recognize different cardiac ultrasound views, particularly their ability to differentiate normal from pathologic ventricular, valvular, IVC, and pericardial findings (ultrasound image interpretation exam).
The six-minute exam
The goal of this exam was to assess students’ ability to produce transthoracic cardiac ultrasound images. Each student had 6 minutes to obtain the main echocardiographic views in a predetermined order using a PUD: PLAV (Fig. 1a), PSAV (at the aortic, mitral, and mid-papillary levels; Fig. 1b), apical views (4-ch, 2-ch, 3-ch; Fig. 2) and subcostal views (standard and focused on IVC; Fig. 3).
During the exam, the supervising physician used a checklist of cardiac anatomical points that each student was required to identify in each one of the main transthoracic ultrasound views and a final score was obtained according to the student’s performance (Additional file 1: Appendix A). The views were obtained on healthy models who were pre-screened and had good ultrasound windows.
By the end of the six-minute period, the exam ended, regardless of the number of windows acquired and the students were asked to report their personal self-training time during the rotation in hours.
Ultrasound image interpretation exam
The exam consisted of 23 questions, each with one echo clip. The students were evaluated for their ability to identify the main cardiac ultrasound views and recognize normal and abnormal LV and RV function, the anatomy of the aortic and mitral valves, IVC size and respiratory variation, valvular dysfunction, and the presence of pericardial effusion.
Statistical analysis
The data collected was documented using summary tables. Continuous variables with normal distribution were presented as mean and standard deviation with 95% confidence interval when appropriate. Ordinary variables or continuous variables with non-normal distribution were presented as median with an interquartile range (IQR). Categorical variables were presented as counts and percentages of the total.
Continuous variables were analyzed using student t-test. Non-parametric procedures (Mann–Whitney) were used if parametric assumptions could not be satisfied even after data transformation attempts. Parametric model assumptions were assessed using Normal-plot or the Shapiro-Wilks test for verification of normality and Levene’s test for verification of homogeneity of variances.
Categorical variables were tested using Pearson’s χ2 test for contingency tables or Fisher Exact test when appropriate. Correlations between variables were tested using Pearson or Spearman tests, depending on variable distribution.
All statistical tests and/or confidence intervals, as appropriate, were performed at α = 0.05 (two-sided) and presented with their 95% confidence interval when appropriate.
Results
All 31 students completed the eight-hour course, as required by the study protocol. All students but one could visualize the parasternal long-axis view (PLAV), all visualized at least one level (aortic, mitral, mid-papillary) of the parasternal short-axis view (PSAV), all visualized at least one of the three apical views (four-, three- and two-chamber views) and 89% visualized at least one anatomical view of the subcostal view (Table 1).
The average grade on the cardiac ultrasound view recognition test was 73%. Thirty students (97%) were able to correctly identify normal LV function and LV dysfunction. All 31 students differentiated normal mitral valve from rheumatic mitral valve injury and 95% of the students diagnosed the presence of pericardial effusion.
The average PUD individual practice time (which was not obligatory) was 3.3 ± 2.7 h per student. The maximum individual practice time was 10 h (reported by one student). Four students reported no individual practice at all.
The six-minute exam
Twenty-seven of 31 (87%) students performed the exam. All participants were able to obtain at least one anatomical view of the eight transthoracic views within the 6 minutes allowed. The most obtainable view (the view that the largest number of students could achieve) was the PLAV, with a median rate of 89% (SD 23%), while the least obtainable view was the subcostal view, with a median rate of 58% (SD 34%).
Parasternal views
Twenty-six of 27 students (96%) obtained at least one image with one of the four anatomical points required for the PLAV view (correct alignment, total endocardial demarcation of LV, and visualization of mitral leaflets or aortic valve cusps). Although seven students (26%) could not achieve the correct alignment for PLAV anatomical points, endocardial demarcation and mitral and aortic valves were visualized by most students (89%, 96%, and 95% respectively; Table 1).
All students were able to obtain at least one image of the eight anatomical points defined for the PSAV view at the aortic level (aortic, tricuspid, and pulmonic valves, interatrial septum), mitral level (complete LV endocardial demarcation, mitral valve), and midpapillary level (complete LV endocardial demarcation, papillary muscles). Students performed better in scanning the midpapillary than the mitral or the aortic level (average grades of 89%, 85%, and 78% respectively; Table 1).
Apical views
All of the students were able to obtain at least one of the three apical views, namely 4-ch, 2-ch, and 3-ch. Eighteen students (67%) obtained all apical views. Six (22%) students obtained two out of the three apical views, and three (11%) students were able to obtain only one of the three apical views. The most obtainable apical view was 4-ch (89%) and the least obtainable was 3-ch (77%). Table 1 shows that students had less success in imaging entire ventricles (up to 56% for the LV and up to 48% for the RV) than for imaging the valves (up to 89% for the mitral and 70% for the aortic valve) from the apex.
Subcostal view
The subcostal view comprised the last part of the six-minute exam and the students were required to show two views: the long-axis four-chamber standard view and the tilted view of the IVC. Twenty-four of 27 students (89%) were able to produce at least one anatomical view of five predetermined anatomical points for this view (Appendage A). Imaging of the IVC was achieved by 16 of 27 students (59%). The rest of the results for this view are summarized in Table 1.
Ultrasound image interpretation exam
This exam was divided into different topics: cardiac view recognition, ventricular function identification, valvular abnormality identification, pericardial abnormality recognition, and IVC recognition.
Cardiac view recognition
All 31 students took the exam. The average grade on cardiac ultrasound view recognition was 73 ± 30. Table 2 shows the students’ scores for the interpretation of cardiac ultrasound images.
Left and right ventricular function
Thirty students (97%) were able to correctly identify normal LV function and LV dysfunction. Twenty-eight of 31 (90%) students were able to recognize hyperdynamic LV function. All the students were able to differentiate normal from severely hypokinetic RV.
Mitral and aortic valves
All the students differentiated normal mitral valve from rheumatic mitral valve injury. Twenty-two students (71%) were able to recognize a calcified aortic valve. Bicuspid aortic valve was diagnosed by 8 of 31 (25%) students.
Twenty-five students (81%) were able to recognize a jet of mitral regurgitation and 17 students (54%) identified a regurgitant jet of aortic regurgitation by color Doppler.
Pericardium and IVC
Ninety-five percent of the students diagnosed the presence of pericardial effusion from the subcostal view. Dilated IVC was recognized by 16 students (52%).
Discussion
We designed a brief cardiac ultrasound course for medical students during their first clinical year with the aim of providing them with tools for expanding the physical examination. This condensed course combines 4 hours of lectures for the entire group, 4 hours of small-group hands-on sessions, and additional elective individual practice time with a PUD.
This is a “proof of concept” study that shows that teaching a large group of students to conduct basic cardiac ultrasound exams in a relatively short period of time is feasible. Students were also able to accurately differentiate normal from severely decreased LV and RV function, normal mitral valves from rheumatic mitral valve injury, and normal aortic valves from calcified aortic valves, and to identify pericardial effusion correctly.
Numerous studies have demonstrated the feasibility of teaching medical students, residents, and novice non-cardiologists the performance and interpretation of cardiac ultrasound [1, 3, 4, 8, 11, 12, 16,17,18, 20,21,22,23,24,25,26,27]. Our results are similar to those of some of the previously published studies (by our group and others), which showed that novice personnel and medical students can, after brief training, accurately differentiate severe LV dysfunction from normal function, diagnose rheumatic injury of the mitral valve [27], and recognize the presence of pericardial effusion after just a few hours of training [11, 12, 22, 28]. However, none of these previous studies were conducted on a large group of medical students during their first clinical year, objectively assessing their hands-on performance as well as their ability to interpret basic pathologies.
Panoulas and colleagues trained only five final-year medical students after their cardiology rotation and showed improved clinical diagnosis [21]. Andersen and colleagues trained 30 fifth-year medical students, but in this study the intensity (teacher-student ratio) of hands-on teaching was not specified and the study suffered from selection bias, as the assessment of scanning quality was dependent on students’ log books, where students chose their best clips and were not evaluated in an objective test as they were in our study [11]. Stokke and colleagues briefly trained (in a four-hour course) 21 medical students using PUD, but compared their findings to auscultation and did not present objective scanning quality assessment [29].
We have objectively measured students’ performance and showed that a large class can become proficient in conducting and assessing basic cardiac ultrasound clips by participating in relatively short hands-on training in groups of four. Our students did only fairly well in terms of their ability to acquire all cardiac images. Sixteen of 27 (59%) students were able to demonstrate all the views (parasternal, apical, and subcostal) within 6 minutes. But most students obtained at least one transthoracic echocardiographic view, while the most obtainable view was the parasternal long-axis view (89%) and the least obtainable was the subcostal view (58%). It is possible that the six-minute test was too short to allow novice operators to obtain all main cardiac views. This notion is supported by the fact that the last view to be obtained in the exam (the subcostal view) was also the least obtainable. A longer exam would probably have improved students’ scores.
Another novel intervention was the incorporation of non-obligatory individual PUD practice time during the eight-week clinical rotation. This teaching modality may have contributed to the students’ performance as measured by the six-minute exam. However, we could not assess the correlation between the number of individual practice hours and final exam scores due to inadequate self-reporting by the students.
Strzecka and colleagues recently showed a learning curve effect among novice operators after a short course on PUD. Medical students detected major abnormalities with an acceptable diagnostic value that increased with the number of examinations performed [12]. Ruddox and colleagues found poor scanning performance when medical residents received only a two-hour training program (a one-hour practical demonstration followed by a one-hour hands-on training session) [22]. Students demonstrated poor ability to recognize impaired cardiac function, pericardial effusion, and valvular heart disease after this very brief training. Anderson and colleagues trained 30 fifth-year volunteer medical students who received a total of 9 hours (three sessions) of combined practical and theoretical training in the use and interpretation of ultrasound images. Students were encouraged to perform at least 75 PUD examinations prior to being tested [11]. Seventy-four percent of the students recorded acceptable cardiovascular organ imaging. In agreement with our results, students were better at interpreting cardiac images than acquiring them. Their diagnostic accuracy in correctly identifying reduced LV function, pericardial effusion, pleural effusion, lung comets, IVC diameter, and respiratory variation was 94% (CI 89.0–96.5). At present, the recommendations regarding a minimum number of studies (performance of at least 75 echocardiographic studies and interpretation of 150 complete studies under supervision) are indicated for sonographers and physicians who are learning comprehensive echocardiographic studies with premium echocardiographic devices. Due to inconsistent data that exists to date, there is no consensus on the minimum number of studies or hours of training needed to teach cardiac ultrasound as a diagnostic tool in medical schools.
A prolonged teaching program would be impractical when teaching novice medical personnel on a large scale. On the other hand, very short training could be insufficient to achieve the true benefit of ultrasound-assisted physical examination and comprise a source of mistakes and misdiagnoses. It seems that at least 8 hours of PUD training (according to our results and previously published data) may be sufficient for medical students to learn to accurately assess basic cardiac parameters by echocardiography, but insufficient to generate independent ultrasound cardiac imaging using pocket devices. The acquisition of the ability to use PUDs independently may be enhanced by more structured guidance for individual use of PUD during clinical rotations. We do believe that the “consolidation process” of bedside ultrasound studies is directly related to the availability of PUDs for student use. In our hospital, each internal medicine ward has one PUD device. In addition, in our course we used four PUDs provided by the cardiology department of the hospital affiliated with the medical school to the students for their free practice during the eight-week internal medicine rotation. The PUDs were available for each student every 4 days. In our estimation, this number of PUDs allowed our students to practice ultrasound image acquisition at an acceptable frequency.
Practicing by utilizing PUD in relevant medical school clinical rotations will improve students’ ability to perform focused cardiac ultrasound examinations. We believe that incorporating the six-minute hands-on exam and the pathological clip exam into the final rotation’s formal student assessment as well as requiring students in clinical rotations to submit logbooks of PUD images will further improve their bedside point-of-care ultrasound performance.
Our study has some limitations. Students did not accurately report self-training time, and thus provided only estimated data that limited our ability to reliably test the correlations between the amount of self-training and the final exam scores. Perhaps obligatory guided self-training sessions during the clinical rotation would have improved hands-on performance on the six-minute exam. In addition, we used young, healthy models, known to have good acoustic windows, for the six-minute hands-on test, and not actual medical patients.
The ultrasound image recognition exam made use of pathological pre-recorded clips, which were presented to the students on a screen instead of real patients with pathologies in real medical settings. No pretest was needed as none of the students had any prior experience with the use of ultrasound.
Teaching cardiac ultrasound to large groups of medical students is challenging. Incorporating ultrasound into anatomy and physiology curriculums in the preclinical years could improve students’ skills during the clinical years. Replacing highly qualified sonographers and cardiologists with medical students who have received formal instruction could provide an option for coping with the reality of a limited number of instructors being available for hands-on practice [25, 26]. More support of training in the wards may be possible once more physicians begin using this tool as part of regular practice during clinical rounds. The use of web-based learning modules as well as simulators (currently available for learning basic as well as advanced ultrasound) to complement practice sessions are options that we are assessing both to reduce costs and to make this type of course more efficient.
Conclusions
Large-scale instruction of medical students in cardiac ultrasound during the first clinical years is feasible. Brief training in cardiac ultrasound that includes lectures, hands-on sessions, and individual practice allows medical students to gain proficiency in the diagnosis of a limited number of cardiac states and provides them with a modest ability to acquire transthoracic ultrasound views. Therefore, in order to modify traditional methods of physical examination and diagnosis by including ultrasound assessment as a complement of the physical examination, it seems appropriate to incorporate basic courses similar to the one described here into medical school curriculums.
Abbreviations
- AL:
-
Anterolateral
- AML:
-
Anterior mitral leaflet
- AoV:
-
Aortic valve
- Des AO:
-
Descending Aorta
- IAS:
-
Interatrial septum
- IVC:
-
Inferior vena cava
- IVS:
-
Interventricular septum
- LA:
-
Left atrium.
- LC:
-
Left coronary cusp
- LV:
-
Left ventricle
- NC:
-
Noncoronary cusp
- PM:
-
Posteromedial
- PML:
-
Posterior mitral leaflet
- PV:
-
Pulmonic valve
- RA:
-
Right atrium
- RC:
-
Right coronary cusp
- RV:
-
Right ventricle
- RVOT:
-
Right ventricle outflow tract
- TV:
-
Tricuspid valve
References
Mjolstad OC, Dalen H, Graven T, Kleinau JO, Salvesen O, Haugen BO. Routinely adding ultrasound examinations by pocket-sized ultrasound devices improves inpatient diagnostics in a medical department. Eur J Intern Med. 2012;23(2):185–91.
Steinberger J, Moller JH, Berry JM, Sinaiko AR. Echocardiographic diagnosis of heart disease in apparently healthy adolescents. Pediatrics. 2000;105(4 Pt 1):815–8.
Decara JM, Kirkpatrick JN, Spencer KT, Ward RP, Kasza K, Furlong K, et al. Use of hand-carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses. J Am Soc Echocardiogr. 2005;18(3):257–63.
Kobal SL, Atar S, Siegel RJ. Hand-carried ultrasound improves the bedside cardiovascular examination. Chest. 2004;126(3):693–701.
Spencer KT, Anderson AS, Bhargava A, Bales AC, Sorrentino M, Furlong K, et al. Physician-performed point-of-care echocardiography using a laptop platform compared with physical examination in the cardiovascular patient. J Am Coll Cardiol. 2001;37(8):2013–8.
Attenhofer Jost CH, Turina J, Mayer K, Seifert B, Amann FW, Buechi M, et al. Echocardiography in the evaluation of systolic murmurs of unknown cause. Am J Med. 2000;108(8):614–20.
Mangione S. Cardiac auscultatory skills of physicians-in-training: a comparison of three English-speaking countries. Am J Med. 2001;110(3):210–6.
Kobal SL, Trento L, Baharami S, Tolstrup K, Naqvi TZ, Cercek B, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002–6.
Sonderegger-Iseli K, Burger S, Muntwyler J, Salomon F. Diagnostic errors in three medical eras: a necropsy study. Lancet. 2000;355(9220):2027–31.
Jaffe WM, Roche AH, Coverdale HA, McAlister HF, Ormiston JA, Greene ER. Clinical evaluation versus Doppler echocardiography in the quantitative assessment of valvular heart disease. Circulation. 1988;78(2):267–75.
Andersen GN, Viset A, Mjolstad OC, Salvesen O, Dalen H, Haugen BO. Feasibility and accuracy of point-of-care pocket-size ultrasonography performed by medical students. BMC Med Educ. 2014;14:156.
Filipiak-Strzecka D, John B, Kasprzak JD, Michalski B, Lipiec P. Pocket-size echocardiograph--a valuable tool for nonexperts or just a portable device for echocardiographers? Adv Med Sci. 2013;58(1):67–72.
Aguirre FV, Pearson AC, Lewen MK, McCluskey M, Labovitz AJ. Usefulness of Doppler echocardiography in the diagnosis of congestive heart failure. Am J Cardiol. 1989;63(15):1098–102.
Rugolotto M, Hu BS, Liang DH, Schnittger I. Rapid assessment of cardiac anatomy and function with a new hand-carried ultrasound device (OptiGo): a comparison with standard echocardiography. Eur J Echocardiogr. 2001;2(4):262–9.
Colli A, Prati D, Fraquelli M, Segato S, Vescovi PP, Colombo F, et al. The use of a pocket-sized ultrasound device improves physical examination: results of an in- and outpatient cohort study. PLoS One. 2015;10(3):e0122181.
Andersen GN, Graven T, Skjetne K, Mjolstad OC, Kleinau JO, Olsen O, et al. Diagnostic influence of routine point-of-care pocket-size ultrasound examinations performed by medical residents. J Ultrasound Med. 2015;34(4):627–36.
Kimura BJ, Amundson SA, Willis CL, Gilpin EA, DeMaria AN. Usefulness of a hand-held ultrasound device for bedside examination of left ventricular function. Am J Cardiol. 2002;90(9):1038–9.
Duvall WL, Croft LB, Goldman ME. Can hand-carried ultrasound devices be extended for use by the noncardiology medical community? Echocardiography. 2003;20(5):471–6.
Dinh VA, Lakoff D, Hess J, Bahner DP, Hoppmann R, Blaivas M, et al. Medical student Core clinical ultrasound milestones: a consensus among directors in the United States. J Ultrasound Med. 2016;35(2):421–34.
Bruce CJ, Montgomery SC, Bailey KR, Tajik J, Seward JB. Utility of hand-carried ultrasound devices used by cardiologists with and without significant echocardiographic experience in the cardiology inpatient and outpatient settings. Am J Cardiol. 2002;90(11):1273–5.
Panoulas VF, Daigeler AL, Malaweera AS, Lota AS, Baskaran D, Rahman S, et al. Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur Heart J Cardiovasc Imaging. 2013;14(4):323–30.
Ruddox V, Stokke TM, Edvardsen T, Hjelmesaeth J, Aune E, Baekkevar M, et al. The diagnostic accuracy of pocket-size cardiac ultrasound performed by unselected residents with minimal training. Int J Cardiovasc Imaging. 2013;29(8):1749–57.
Prinz C, Dohrmann J, van Buuren F, Bitter T, Bogunovic N, Horstkotte D, et al. The importance of training in echocardiography: a validation study using pocket echocardiography. J Cardiovasc Med (Hagerstown). 2012;13(11):700–7.
Rugolotto M, Chang CP, Hu B, Schnittger I, Liang DH. Clinical use of cardiac ultrasound performed with a hand-carried device in patients admitted for acute cardiac care. Am J Cardiol. 2002;90(9):1040–2.
Celebi N, Zwirner K, Lischner U, Bauder M, Ditthard K, Schurger S, et al. Student tutors are able to teach basic sonographic anatomy effectively - a prospective randomized controlled trial. Ultraschall Med. 2012;33(2):141–5.
Kuhl M, Wagner R, Bauder M, Fenik Y, Riessen R, Lammerding-Koppel M, et al. Student tutors for hands-on training in focused emergency echocardiography--a randomized controlled trial. BMC Med Educ. 2012;12:101.
Shmueli H, Burstein Y, Sagy I, Perry ZH, Ilia R, Henkin Y, et al. Briefly trained medical students can effectively identify rheumatic mitral valve injury using a hand-carried ultrasound. Echocardiography. 2013;30(6):621–6.
DeCara JM, Lang RM, Koch R, Bala R, Penzotti J, Spencer KT. The use of small personal ultrasound devices by internists without formal training in echocardiography. Eur J Echocardiogr. 2003;4(2):141–7.
Stokke TM, Ruddox V, Sarvari SI, Otterstad JE, Aune E, Edvardsen T. Brief group training of medical students in focused cardiac ultrasound may improve diagnostic accuracy of physical examination. J Am Soc Echocardiogr. 2014;27(11):1238–46.
Acknowledgements
None.
Funding
This study was not funded.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
An English language copy of the six-minute exam used is provided as an additional file.
Authors’ contributions
SLK and LF conceptualized and designed the study. All authors were involved in data collection, analyses, and interpretation. SLK, AB, and LF drafted the manuscript. NLS, OG, and YL critically revised the manuscript for important intellectual content. All authors approved of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical approval for the data collection was obtained from the Ethics Committee of Soroka Medical Center. All the students who participated were given assurance of confidentiality that the information gathered would be used exclusively for research purposes. We also indicated that participation in the study was anonymous and voluntary and filling in the written exam meant that the students were willing to participate in the study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Appendix A. (DOCX 92 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kobal, S.L., Lior, Y., Ben-Sasson, A. et al. The feasibility and efficacy of implementing a focused cardiac ultrasound course into a medical school curriculum. BMC Med Educ 17, 94 (2017). https://doi.org/10.1186/s12909-017-0928-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-017-0928-x