Abstract
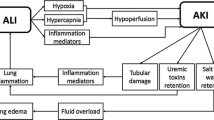
Lung and kidney functions are intimately related in both health and disease. The regulation of acid–base equilibrium, modification of partial pressure of carbon dioxide and bicarbonate concentration, and the control of blood pressure and fluid homeostasis all closely depend on renal and pulmonary activities. These interactions begin in fetal age and are often responsible for the genesis and progression of diseases. In gestational age, urine is a fundamental component of the amniotic fluid, acting on pulmonary maturation and growth. Moreover, in the first trimester of pregnancy, kidney is the main source of proline, contributing to collagen synthesis and lung parenchyma maturation. Pathologically speaking, the kidneys could become damaged by mediators of inflammation or immuno-mediated factors related to a primary lung pathology or, on the contrary, it could be the renal disease that determines a consecutive pulmonary damage. Furthermore, non immunological mechanisms are frequently involved in renal and pulmonary diseases, as observed in chronic pathologies such as sleep apnea syndrome, pulmonary hypertension, progressive renal disease and hemodialysis. Kidney damage has also been related to mechanical ventilation. The aim of this review is to describe pulmonary-renal interactions and their related pathologies, underscoring the need for a close collaboration between intensivists, pneumologists and nephrologists.
Similar content being viewed by others
References
Kayashima Y, Smithies O, Kakoki M (2012) The kallikrein-kinin system and oxidative stress. Curr Opin Nephrol Hypertens 21:92–96
Izzo JL Jr, Weir MR (2011) Angiotensin-converting enzyme inhibitors. J Clin Hypertens (Greenwich) 13:667–675
Hislop A, Hey E, Reid L (1979) The lungs in congenital bilateral renal agenesis and dysplasia. Arch Dis Child 54:32–38
Salant DJ (2010) Goodpasture’s disease–new secrets revealed. N Engl J Med 363:388–391
Santoro D, Pellicanò V, Visconti L, Trifirò G, Cernaro V, Buemi M (2015) Monoclonal antibodies for renal diseases: current concepts and ongoing treatments. Expert Opin Biol Ther 15:1119–1143
Hié M, Costedoat-Chalumeau N, Saadoun D, Azoulay E (2013) The pulmonary-renal syndrome: a diagnostic and therapeutic emergency for the internist and the intensivist. Rev Med Interne 34:679–686
Ioachimescu OC, Stoller JK (2008) Diffuse alveolar hemorrhage: diagnosing it and finding the cause. Cleve Clin J Med 75:264–265
Jennette JC (2013) Overview of the 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Clin Exp Nephrol 17:603–606
Munshi BD, Sengupta S, Sharan A, Mukhopadhyay S, Ghosh B, Dasgupta A, Bhattacharyya R (2015) Anti-neutrophil cytoplasmic antibody (ANCA)-negative small vessel vasculitis: a rare cause of pulmonary renal syndrome. Intern Med 54:2759–2763
Jennette JC, Falk RJ, Andrassy K et al (1994) Nomenclature of systemic vasculitides: the proposal of an international consensus conference. Arthritis Rheum 37:187–192
Agarwal G, Sultan G, Werner SL, Hura C (2014) Hydralazine induces myeloperoxidase and proteinase 3 anti-neutrophil cytoplasmic antibody vasculitis and leads to pulmonary renal syndrome. Case Rep Nephrol 2014:868590
Dolman KM, Gans RO, Vervaat TJ et al (1993) Vasculitis and antineutrophil cytoplasmic autoantibodies associated with propylthiouracil therapy. Lancet 342:651–652
Grau RG (2015) Drug-induced vasculitis: new insights and a changing lineup of suspects. Curr Rheumatol Rep 17:71
Qin H, Guo Q, Shen N et al (2014) Chest imaging manifestations in lupus nephritis. Clin Rheumatol 33:817–823
Tamai K, Tomii K, Nakagawa A, Otsuka K, Nagata K (2015) Diffuse alveolar hemorrhage with predominantly right-sided infiltration resulting from cardiac comorbidities. Intern Med 54:319–324
de Prost N, Parrot A, Cuquemelle E et al (2012) Diffuse alveolar hemorrhage in immunocompetent patients: etiologies and prognosis revisited. Respir Med 106:1021–1032
Lacava V, Coppolino G, Puntorieri E et al (2015) Nephro-oncology: a link in evolution. Ren Fail 37:1260–1266
Bernard GR, Artigas A, Brigham KL, Brigham KL et al (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Ferguson ND, Frutos-Vivar F, Esteban A, Fernández-Segoviano P, Aramburu JA, Nájera L, Stewart TE (2005) Acute respiratory distress syndrome: under recognition by clinicians and diagnostic accuracy of three clinical definitions. Crit Care Med 33:2228–2234
Definition Task Force ARDS, Ranieri VM et al (2012) Acute respiratory distress syndrome: the Berlin Definition. JAMA 307:2526–2533
Endo S, Shibata S, Sato N et al (2010) A prospective cohort study of ALI/ARDS in the Tohoku district of Japan (second report). J Anesth 24:351–358
Chiumello D, Marino A, Brioni M et al (2013) Visual anatomical lung CT scan assessment of lung recruitability. Intensive Care Med 39:66–73
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ (2004) Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 100:9–15
Galbois A, Ait-Oufella H, Baudel JL et al (2010) Pleural ultrasound compared with chest radiographic detection of pneumothorax resolution after drainage. Chest 138:648–655
Bellani G, Messa C, Guerra L et al (2009) Lungs of patients with acute respiratory distress syndrome show diffuse inflammation in normally aerated regions: a [18F]-fluoro-2-deoxy-d-glucose PET/CT study. Crit Care Med 37:2216–2222
Matsuoka S, Hunsaker AR, Gill RR, Jacobson FL, Ohno Y, Patz S, Hatabu H (2008) Functional MR imaging of the lung. Magn Reson Imaging Clin N Am 16:275–289
Ware LB, Matthay MA (2005) Clinical practice. Acute pulmonary edema. N Engl J Med 353:2788–2796
Yao YM, Luan YY, Zhang QH, Sheng ZY (2015) Pathophysiological aspects of sepsis: an overview. Methods Mol Biol 1237:5–15
Rubenfeld GD, Caldwell E, Peabody E et al (2005) Incidence and outcomes of acute lung injury. N Engl J Med 353:1685–1693
Guinot PG, Dupont H, Longrois D (2015) Some questioning about the assessment of renal perfusion in sepsis. Crit Care Med 43:e262–e264
Prowle JR, Bellomo R (2015) Sepsis-associated acute kidney injury: macrohemodynamic and microhemodynamic alterations in the renal circulation. Semin Nephrol 35:64–74
Darmon M, Clec’h C, Adrie C et al (2014) Acute respiratory distress syndrome and risk of AKI among critically ill patients. Clin J Am Soc Nephrol 9:1347–1353
Huet F, Semama DS, Gouyon JB, Guignard JP (1999) Protective effect of perindoprilat in the hypoxemia-induced renal dysfunction in the newborn rabbit. Pediatr Res 45:138–142
Semama DS, Thonney M, Guignard JP (1995) Does endothelin-1 mediate the hypoxemia-induced renal dysfunction in newborn rabbits? Biol Neonate 67:216–222
Ballèvre L, Thonney M, Guignard JP (1996) Role of nitric oxide in the hypoxemia-induced renal dysfunction of the newborn rabbit. Pediatr Res 39:725–730
Kilburn KH, Dowell AR (1971) Renal function in respiratory failure. Effects of hypoxia, hyperoxia, and hypercapnia. Arch Intern Med 127:754–762
Koyner JL, Murray PT (2010) Mechanical ventilation and the kidney. Blood Purif 29:52–68
Kuiper JW, Groeneveld ABJ, Slutsky AS, Plotz FB (2005) Mechanical ventilation and acute renal failure. Crit Care Med 33:1408–1415
Pannu N, Mehta RL (2004) Effect of mechanical ventilation on the kidney. Best Pract Res Clin Anaesthesiol 18:189–203
Annat G, Viale JP, Bui Xuan B et al (1983) Effect of PEEP ventilation on renal function, plasma renin, aldosterone, neurophysins and urinary ADH, and prostaglandins. Anesthesiology 58:136–141
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The acute respiratory distress syndrome network. N Engl J Med 342:1301–1308
Rivers E, Nguyen B, Havstad S et al (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Sakr Y, Vincent JL, Reinhart K et al (2005) High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest 128:3098–3108
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Roch A, Hraiech S, Dizier S, Papazian L (2013) Pharmacological interventions in acute respiratory distress syndrome. Ann Intensive Care 3:20
Silva PL, Pelosi P, Rocco PR (2014) Fluids in acute respiratory distress syndrome: pros and cons. Curr Opin Crit Care 20:104–112
Liu KD, Matthay MA (2008) Advances in critical care for the nephrologist: acute lung injury/ARDS. Clin J Am Soc Nephrol 3:578–586
Chauhan S, Subin S (2011) Extracorporeal membrane oxygenation, an anesthesiologist’s perspective: physiology and principles. Part 1. Ann Card Anaesth 14:218–229
Peek GJ, Mugford M, Tiruvoipati R et al (2009) Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 374:1351–1363
Haneya A, Diez C, Philipp A, Bein T, Mueller T, Schmid C, Lubnow M (2015) Impact of acute kidney injury on outcome in patients with severe acute respiratory failure receiving extracorporeal membrane oxygenation. Crit Care Med 43:1898–1906
Chen Q, Yu W, Shi J, Shen J, Hu Y, Gong J, Li J, Li N (2014) The effect of extracorporeal membrane oxygenation therapy on systemic oxidative stress injury in a porcine model. Artif Organs 38:426–431
Shi J, Chen Q, Yu W et al (2014) Continuous renal replacement therapy reduces the systemic and pulmonary inflammation induced by veno-venous extracorporeal membrane oxygenation in a porcine model. Artif Organs 38:215–223
Kielstein JT, Heiden AM, Beutel G (2013) Renal function and survival in 200 patients undergoing ECMO therapy. Nephrol Dial Transpl 28:86–90
Paden ML, Warshaw BL, Heard ML, Fortenberry JD (2011) Recovery of renal function and survival after continuous renal replacement therapy during extracorporeal membrane oxygenation. Pediatr Crit Care Med 12:153–158
Hoover NG, Heard M, Reid C, Wagoner S, Rogers K, Foland J, Paden ML, Fortenberry JD (2008) Enhanced fluid management with continuous venovenous hemofiltration in pediatric respiratory failure patients receiving extracorporeal membrane oxygenation support. Intensive Care Med 34:2241–2247
Wolf MJ, Chanani NK, Heard ML, Kanter KR, Mahle WT (2013) Early renal replacement therapy during pediatric cardiac extracorporeal support increases mortality. Ann Thorac Surg 96:917–922
Faubel S, Edelstein CL (2015) Mechanisms and mediators of lung injury after acute kidney injury. Nat Rev Nephrol. doi:10.1038/nrneph.2015.158
Druhan LJ, Forbes SP, Pope AJ, Chen CA, Zweier JL, Cardounel AJ (2008) Regulation of eNOS-derived superoxide by endogenous methylarginines. Biochemistry 47:7256–7263
Otterbein LE, Zuckerbraun BS, Haga M et al (2003) Carbon monoxide suppresses arteriosclerotic lesions associated with chronic graft rejection and with balloon injury. Nat Med 9:183–190
Yanbaeva DG, Dentener MA, Creutzberg EC, Wesseling G, Wouters EF (2007) Systemic effects of smoking. Chest 131:1557–1566
Farber MO, Roberts LR, Weinberger MH, Robertson GL, Fineberg NS, Manfredi F (1982) Abnormalities of sodium and H2O handling in chronic obstructive lung disease. Arch Intern Med 142:1326–1330
Barakat MF, McDonald HI, Collier TJ, Smeeth L, Nitsch D (2015) Quint JK (2015) Acute kidney injury in stable COPD and at exacerbation. Int J Chron Obstruct Pulmon Dis 10:2067–2077
Ricciardi CA, Lacquaniti A, Cernaro V et al (2015) Salt-water imbalance and fluid overload in hemodialysis patients: a pivotal role of corin. Clin Exp Med. doi:10.1007/s10238-015-0374-1
Simonneau G, Robbins IM, Beghetti M et al (2009) Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 54:S43–S54
Havlucu Y, Kursat S, Ekmekci C et al (2007) Pulmonary hypertension in patients with chronic renal failure. Respiration 74:503–510
Buemi M, Lacquaniti A, Bolignano D et al (2008) Dialysis and the elderly: an underestimated problem. Kidney Blood Press Res 31:330–336
Zoccali C (2012) Pulmonary hypertension in dialysis patients: a prevalent, risky but still uncharacterized disorder. Nephrol Dial Transpl 27:3674–3677
Sise ME, Courtwright AM, Channick RN (2013) Pulmonary hypertension in patients with chronic and end-stage kidney disease. Kidney Int 84:682–692
Lacquaniti A, Bolignano D, Campo S et al (2009) Malnutrition in the elderly patient on dialysis. Ren Fail 31:239–245
Lacquaniti A, Bolignano D, Donato V et al (2011) Obestatin: a new element for mineral metabolism and inflammation in patients on hemodialysis. Kidney Blood Press Res 34:104–110
Neri G, Lacquaniti A, Rizzo G, Donato N, Latino M, Buemi M (2012) Real-time monitoring of breath ammonia during haemodialysis: use of ion mobility spectrometry (IMS) and cavity ring-down spectroscopy (CRDS) techniques. Nephrol Dial Transpl 27:2945–2952
Agarwal R (2012) Prevalence, determinants and prognosis of pulmonary hypertension among hemodialysis patients. Nephrol Dial Transpl 27:3908–3914
Yan Y, Zhao HP, Wang M (2009) Severe uremic lung: a case report and review. Beijing Da Xue Xue Bao 41:596–598
Kimmel PL, Miller G, Mendelson WB (1989) Sleep apnea syndrome in chronic renal disease. Am J Med 86:308–314
Markou N, Kanakaki M, Myrianthefs P et al (2006) Sleep-disordered breathing in nondialyzed patients with chronic renal failure. Lung 184:43–49
Uyar M, Davutoğlu V, Gündoğdu N, Kosovalı D, Sarı İ (2015) Renal functions in obstructive sleep apnea patients. Sleep Breath. doi:10.1007/s11325-015-1204-0
Sakaguchi Y, Hatta T, Hayashi T et al (2013) Association of nocturnal hypoxemia with progression of CKD. Clin J Am Soc Nephrol 8:1502–1507
Kinebuchi S, Kazama JJ, Satoh M et al (2004) Short-term use of continuous positive airway pressure ameliorates glomerular hyperfiltration in patients with obstructive sleep apnoea syndrome. Clin Sci (Lond) 107:317–322
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding source
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Visconti, L., Santoro, D., Cernaro, V. et al. Kidney-lung connections in acute and chronic diseases: current perspectives. J Nephrol 29, 341–348 (2016). https://doi.org/10.1007/s40620-016-0276-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-016-0276-7