Abstract
Purpose
We aimed at identifying clinical risk factors or early markers of metabolic syndrome (MetS) in people with spinal cord injury (SCI) that would facilitate a timely diagnosis and implementation of preventive/therapeutic strategies.
Methods
One hundred sixty-eight individuals with chronic (> 1 year) SCI underwent clinical and biochemical evaluations. MetS was diagnosed according to modified criteria of the International Diabetes Federation validated in people with SCI. Wilcoxon rank-sum test and χ2 test were used to compare variables between groups with and without MetS. Multiple logistic regression analysis was performed to reveal independent associations with MetS among variables selected by univariate linear regression analyses.
Results
MetS was diagnosed in 56 of 132 men (42.4%) and 17 of 36 women (47.2%). At univariate regression analyses, putative predictors of MetS were an older age, a higher number of comorbidities, a lower insulin-sensitivity, the presence and intensity of pain, a shorter injury duration, a poorer leisure time physical activity (LTPA) and an incomplete motor injury. At the multiple logistic regression analysis, a significant independent association with MetS only persisted for a poorer LTPA in hours/week (OR: 0.880, 95% CI 0.770, 0.990) and more severe pain symptoms as assessed by the numeral rating scale (OR: 1.353, 95% CI 1.085, 1.793).
Conclusion
In people with chronic SCI, intense pain symptoms and poor LTPA may indicate a high likelihood of MetS, regardless of age, SCI duration, motor disability degree, insulin-sensitivity and comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Life expectancy of spinal cord-injured people has improved markedly in recent decades due to improvements in clinical care of the acute post-injury phase. [1]. Thus, many more patients than in the past survive the acute phase and enter the chronic phase of spinal cord injury (SCI), that is, the stage that begins 1 year after the injury. In that neurologically stable condition, direct and indirect permanent consequences of neurological damage and disability result in systemic comorbidities that unfavorably impact quality of life and increase cardiovascular mortality. The deep anthropometric and body composition changes following SCI strongly contribute to the increased cardiovascular morbidity and mortality [2].
Lack of neurotrophic input of motor nerve projections results in muscle wasting below the injury level up to sarcopenia [3, 4], leading to reduced energy expenditure [5]. On this basis, in people with SCI, body energy balance is positive, as energy intake easily exceeds energy expenditure [6], resulting in increased fat mass, largely distributed at the visceral level [7]. Visceral fat is very sensitive to lipolytic stimuli; therefore, its accumulation is accompanied by an increased release of non-esterified fatty acids in the blood circulation and their deposition into muscle cells and liver [8]. This could explain the very high prevalence of non-alcoholic fatty liver disease (NAFLD) [9,10,11], as well as the intramuscular fat accumulation [12], peculiar to people with SCI. These pathogenetic processes generate insulin resistance that unfavorably affects glucose and lipid metabolism [13]. The constellation of visceral obesity and its correlates, including insulin resistance, glycemic dysregulation, dyslipidemia, and hypertension has been referred to as “metabolic syndrome” (MetS), a cluster of clinical and metabolic features that increase the cardiovascular risk [8].
In people with SCI, however, the diagnosis of MetS is challenged by the same alterations in body composition that promote its onset. Because of muscle atrophy, BMI underestimates obesity [14, 15] and spinal cord-injured people with a BMI value > 22 kg/m2 should be considered as being at high risk for obesity [16]. To further complicate this issue, waist circumference measurement might overestimate visceral fat due to anterior abdominal wall muscle laxity. In addition, especially for injuries above T6, autonomic dysregulation causes blood pressure instability that makes hypertension an unreliable marker of MetS. For these reasons, widely validated diagnostic criteria of MetS in the general population [17, 18] are not reliable in people with SCI for whom modified International Diabetes Federation (IDF) criteria have been proposed [19, 20] with the inclusion of a BMI ≥ 22 kg/m2 as a surrogate marker of obesity suitable for SCI [15, 21, 22]. Nevertheless, given the diagnostic challenges, in many people with SCI, MetS may be identified late or go completely undetected. Failure or delay in taking appropriate lifestyle measures and treatments places these individuals at high risk for cardiovascular morbidity and mortality. Identifying clinical variables that could represent risk factors for MetS or its early markers would facilitate a timely diagnosis, allowing the implementation of necessary preventive and therapeutic strategies.
On this basis, the present study aims to identify lifestyle and clinical factors independently associated with MetS in people with chronic SCI.
Patients and methods
Design and study population
One hundred sixty-eight consecutive patients (132 men and 36 women; mean age, 54.7 ± 17.2 years) admitted to a routine rehabilitation program because of traumatic SCI were included in this retrospective study. All patients had a documented history of clinically and neurologically stable SCI for more than 1 year. No patient had acute illness hindering the rehabilitative program.
The study was approved by the Ethics Committee of L’Aquila and Teramo provinces, Italy (Approval Code: 11/CE/15 of May 7, 2015) and all enrolled subjects signed an informed consent.
Clinical evaluations
Chronic medical comorbidities were assessed using a Web-based calculator (https://www.mdcalc.com/calc/3917/charlson-comorbidity-index-cci) of the age-adjusted Charlson Comorbidity Index (CCI). This tool assigns a weighted score to different medical conditions according to both the relative risk of 1-year mortality and the patient's age. The scores are then summed to provide an overall weighted comorbidity index [23].
Patients underwent a thorough neurological examination according to the guidelines of the International Standards for Neurological Examination and Functional Classification of Spinal Cord Injury; the level and completeness of the lesion were defined using the American Spinal Injury Association (ASIA) protocol [24]. According to the ASIA scale, patients with complete injury and no sensory or motor function in the most distal sacral segment were classified as A; those with incomplete injury were classified as B, C, or D. Category B referred to incomplete sensory injury; category C referred to incomplete both sensory and motor injury in which more than half of the 10 key muscle pairs had strength < 3 on a scale ranging from 0 to 5; category D indicated incomplete both sensory and motor injury in which at least half of the key muscles had strength ≥ 3.
The Numeral Rating Scale (NRS) was used to assess the presence of pain related to the SCI and to measure its intensity, according to the recommendations of the National Institute on Disability Research [25]. Participants were asked to verbally rank pain on a scale ranging from 0 to 10, with 0 representing the absence of pain and 10 the maximum pain imaginable.
Body weight was measured with patients wearing light clothing, using a professional mechanical scale (Wunder SA BI Srl, Monza, Italy). Height was determined after patients was placed on the bed, with legs straightened, head on Frankfurt plane, and feet in dorsal flexion. Height was measured with an elastic tape by segmentally measuring the distances between heel and knee, knee and hip, and hip and head. Body mass index (BMI) was calculated in kg/m2.
Diagnosis of MetS complied with the modified IDF criteria validated in spinal cord-injured people by Gater and al. [19, 20]: BMI ≥ 22 kg/m2 plus any 2 or more of the following features: blood pressure ≥ 130/85 mmHg (or on treatment for hypertension), triglycerides ≥ 150 mg/dL (or on treatment for dyslipidemia), high-density lipoproteins (HDL) < 40 mg/dL for men and < 50 mg/dL for women (or on treatment for dyslipidemia), fasting plasma glucose ≥ 100 mg/dL (or previously diagnosed with type 2 diabetes mellitus).
Functional independence in activities of daily living (ADL) was quantified using the Spinal Cord Independence Measure (SCIM). This is a 19-item tool to measure the functional independence degree in performing ADL: SCIM quantifies each function separately, providing a final score from 0 (total dependence) to 100 (total independence) [26].
Leisure Time Physical Activity (LTPA) refers to physical activities that people choose to perform in their free time: in people with SCI, it includes walking/wheeling, and sports played in a gym. The LTPA Questionnaire (LTPAQ) for People with SCI was used to quantify these activities [27]. This tool provides a measure of hours of LTPA performed at each intensity (mild, moderate, and heavy intensity LTPA) over the previous 7 days. As previously reported [28,29,30], only total score was included in the analyses, as it strongly correlated with mild, moderate, and heavy intensity LTPA sub-scores [29].
Laboratory examinations
A single morning venous blood sample after at least 12 h of fasting was obtained from each participant between 8:00 and 9:00 a.m. Standard methods and commercial kits (Instrumentation Laboratory Company, Lexington, MA, USA) were used for all the biochemical and hematologic measurements. Insulin resistance was assessed using the homeostatic model assessment of insulin resistance (HOMA-IR), according to the formula: insulin (mU/L) × glucose (m/dL)/405 [31].
Statistical analysis
Statistical analysis was performed using the R statistical software (version 4.0.4, 2021, The R Foundation for Statistical Computing, Vienna, Austria). After ascertaining the non-normal data distribution with the Shapiro–Wilk test, we used the Wilcoxon rank-sum test (Mann–Whitney U test) to compare variables between subjects with and without MetS. Proportional differences were assessed by the χ2 test. Multiple logistic regression analysis was performed to reveal independent associations with MetS among variables selected by univariate linear regression analyses. Variance inflation factors (VIFs) were calculated to check the collinearity assumption: a VIF < 5 was considered to indicate no significant collinearity. Significance of differences in the prevalence of MetS throughout the 1st to the 3rd tertile of increasing pain NRS score and LTPA levels were assessed by χ2 test for trend (Mantel–Haenszel test). Statistical significance was accepted when p < 0.05.
Results
A diagnosis of MetS was made in 56 of 132 men (42.4%) and 17 of 36 women (47.2%). Table 1 shows the characteristics of the study population categorized by MetS. Patients with MetS were significantly older and had higher triglycerides and lower HDL levels, higher HOMA-IR, BMI, CCI, systolic and diastolic blood pressure, pain NRS score and poorer LTPA. Moreover, in patients with MetS, the prevalence of complete motor injury was lower, as was the duration of injury (DOI).
As shown in Table 2, at the univariate regression analyses, putative significant predictors of MetS were an older age, a higher CCI, a higher pain NRS score and HOMA-IR, as well as a shorter DOI, a poorer LTPA and the presence of incomplete motor injury. At the multiple logistic regression analysis, a significant independent association with MetS only persisted for a poorer LTPA and more severe pain symptoms, as indicated by a higher pain NRS score.
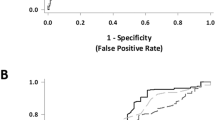
As the pain NRS score and LTPA level increased from the 1st tertile to the 3rd tertile, the prevalence of MetS significantly increased (χ2 test for trend: 7.46, p = 0.02, Fig. 1A) and decreased (χ2 test for trend: 9.53, p = 0.008, Fig. 1B), respectively.
Prevalence of metabolic syndrome (MetS) by A pain intensity quantified in tertiles of increasing numeral rating scale (NRS) score and B weekly leisure time physical activity (LTPA). Statistical significance for differences among groups of NRS scores, obtained by categorizing data into tertiles: χ2 test for trend = 7.46, p = 0.02; Statistical significance for differences among groups of LTPA, obtained by categorizing data into tertiles: χ2 test for trend = 9.53, p = 0.008)
Discussion
Among the many possible determinants and attributes of MetS in people with SCI, this study has narrowed the field to a limited number of variables. The results of univariate regression analyses showed a significant association of MetS with older age, more comorbidities, lower insulin sensitivity, more intense pain symptoms, a poorer physical activity, a lower degree of neuromotor disability, and a more recent clinical history of SCI.
Advancing age is commonly associated with a progressive decrease in physical activity and worsening overall health status due to the onset of comorbidities, including the MetS components [32]. Decreased physical activity, quantified in terms of LTPA in the present study, may contribute directly to the increased incidence of comorbidities, insulin resistance and MetS [2]. An additional factor with a possible pathogenetic role is pain. The prevalence of MetS significantly increased throughout the lowest to the highest tertile of pain NRS score. Neuropathic and/or nociceptive chronic pain symptoms represent a major complaint in people with SCI [33]. Pain may further limit mobility and thus the ability to engage in physical activity: the resulting drop in energy expenditure increases fat accumulation and the risk of developing comorbidities and MetS [2]. Poor physical activity and hypomobility, in turn, could contribute to muscle spasticity that exacerbates pain symptoms [33], thus triggering a vicious circle. The possible mechanisms by which MetS is associated with a lower degree of motor disability and a shorter DOI in our univariate regression analyses remain speculative but could involve lifestyles. In people with recent history of SCI, an incomplete psychological and social-relational adjustment to the disabling condition [34] could result in a propensity to exhibit behavioral correlates of emotional distress [35, 36] at risk for the development of comorbidity, including MetS components. This might occur, paradoxically, with greater likelihood in people with incomplete motor SCI, since, as previously reported [37], spinal cord-injured people with less severe disability degree, have an increased independence in lifestyle and eating habits. In keeping with these findings, in a recent series of 166 Korean patients with chronic SCI, a lower neurological level of injury was a significant and independent predictor of MetS [38]. Indeed, other authors have documented that people with paraplegia exhibited more unfavorable anthropometric features than those with tetraplegia [39].
Obviously, the cross-sectional design of this study does not allow the causal directionality of the associations under investigation to be established, but some information can be inferred from the multiple logistic regression analysis. When all variables selected by the univariate analyses were included in the same multivariable model, only a poorer LTPA and a higher pain score at the NRS exhibited a significant and independent association with MetS. This finding demonstrated that the relationship between pain and MetS is not necessarily mediated by reduced physical activity. Indeed, the association of MetS with poor LTPA and more intense pain symptoms may be complex and bidirectional: on one hand, obesity and comorbidities, components of MetS, may constrain the ability to engage in physical activity; on the other hand, there is preclinical, clinical, and epidemiologic evidence for an association between MetS and sensory peripheral neuropathy independent of prediabetes, diabetes, and glycemic status [40, 41]. The main mediators of this association would be obesity and dyslipidemia [40]. Obesity is the hallmark of MetS and is accompanied by the release into circulation of a large pool of long-chain fatty acids (LCFAs) that penetrate the blood–neurogenic barrier, causing oxidative stress-mediated neuroinflammation [42]. LCFAs alter axonal mitochondrial transport and impair electron chain activity [43]. The resulting mitochondrial dysfunction results in impaired oxidative phosphorylation with reduced adenosine triphosphate (ATP) production and generation of reactive oxygen species (ROS) [44, 45]. The nuclear factor kappa B (NF-kB), a transcriptional factor activated by oxidative stress and hyperglycemia, is at the center of neuroinflammation by MetS [46] as it modulates several downstream pro-inflammatory genes, particularly cyclooxygenase-2 (COX-2) [47]. These mechanisms as whole underlie neuronal and Schwann cell injury that ultimately contributes to MetS neuropathy resulting in chronic pain [40].
Of note, the negative association between MetS and insulin sensitivity was lost in the fully adjusted multiple logistic regression analysis. In keeping with this result, in a recent study by Solinsky et al. [48], although 95 individuals with SCI exhibited a significantly higher prevalence of obesity and lower levels of HDL when compared to 1609 able-bodied controls from the population of National Health and Nutrition Examination Education Survey (NHANES), the rate of insulin resistance, as assessed by HOMA-IR, was similar between the two groups. These findings may reflect the peculiarities of the pathogenesis of MetS in people with SCI. It is possible to speculate that the SCI-related chronic inflammatory state, in addition to contributing to the onset of neuro-pathic pain, may promote at the muscle and adipose tissue level mechanisms of glucose and lipid deregulation underlying MetS, regardless of insulin sensitivity degree. Indeed, although HOMA-IR was significantly higher in patients with MetS than in those without MetS, in both groups, its median values were largely within the normal range. On the other hand, the lack of independent association between MetS and higher HOMA-IR does not seem to depend on a lack of reliability of the latter to identify insulin resistance in people with SCI, since in a recent study by Farkas et al. [49], HOMA-IR and Quantitative Insulin-sensitivity Check Index (QUICKI) were the indices of insulin sensitivity with the best agreement with the intravenous glucose tolerance test in this population.
This study has some limitations. First, the relatively small sample size and the enrollment within a clinical rehabilitation setting. These two peculiarities may limit the generalizability of the results to the community-dwelling spinal cord-injured population. Despite a relatively sized series, the high prevalence of the endpoint (e.g., MetS) allowed the inclusion of a fair number of independent variables in the multiple regression model to adjust analysis for possible major confounders. Nevertheless, a residual confounding effect from unmeasured variables potentially mediating the revealed associations cannot be ruled out. In this light, factors related to lifestyle and/or psychological functioning could play a major role and deserve to be investigated in targeted studies.
In conclusion, in people with chronic SCI, intense pain symptoms and poor physical activity may suggest a high likelihood of MetS, regardless of age, DOI, degree of motor disability, insulin sensitivity and comorbidities. Given the challenges in diagnosing MetS in this population [2], pain and physical inactivity can help health care providers to identify the most at-risk individuals early so that all necessary measures for prevention and treatment of cardiovascular implications can be implemented.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Savic G, DeVivo MJ, Frankel HL, Jamous MA, Soni BM, Charlifue S (2017) Causes of death after traumatic spinal cord injury-a 70-year British study. Spinal Cord 55(10):891–897. https://doi.org/10.1038/sc.2017.64
Barbonetti A, Castellini C, Francavilla S, Francavilla F, D’Andrea S (2022) Metabolic syndrome in spinal cord injury: impact on health. Acad Press. https://doi.org/10.1016/B978-0-12-822427-4.00031-9
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR (2014) Effects of spinal cord injury on body composition and metabolic profile - part I. J Spinal Cord Med 37(6):693–702. https://doi.org/10.1179/2045772314Y.0000000245
Alazzam AM, Goldsmith JA, Khalil RE, Khan MR, Gorgey AS (2023) Denervation impacts muscle quality and knee bone mineral density after spinal cord injury. Spinal Cord 61(4):276–284. https://doi.org/10.1038/s41393-023-00885-3
Farkas GJ, Sneij A, McMillan DW, Tiozzo E, Nash MS, Gater DR Jr (2022) Energy expenditure and nutrient intake after spinal cord injury: a comprehensive review and practical recommendations. Br J Nutr 128(5):863–887. https://doi.org/10.1017/S0007114521003822
Farkas GJ, Pitot MA, Berg AS, Gater DR (2019) Nutritional status in chronic spinal cord injury: a systematic review and meta-analysis. Spinal Cord 57(1):3–17. https://doi.org/10.1038/s41393-018-0218-4
Cirnigliaro CM, LaFountaine MF, Dengel DR, Bosch TA, Emmons RR, Kirshblum SC, Sauer S, Asselin P, Spungen AM, Bauman WA (2015) Visceral adiposity in persons with chronic spinal cord injury determined by dual energy X-ray absorptiometry. Obesity (Silver Spring) 23(9):1811–1817. https://doi.org/10.1002/oby.21194
Zafar U, Khaliq S, Ahmad HU, Manzoor S, Lone KP (2018) Metabolic syndrome: an update on diagnostic criteria, pathogenesis, and genetic links. Hormones (Athens) 17(3):299–313. https://doi.org/10.1007/s42000-018-0051-3. (Epub 2018 Aug 31 PMID: 30171523)
Shin JC, Park CI, Kim SH, Yang EJ, Kim EJ, Rha DW (2006) Abdominal ultrasonography findings in patients with spinal cord injury in Korea. J Korean Med Sci 21(5):927–931. https://doi.org/10.3346/jkms.2006.21.5.927
Barbonetti A, Caterina Vassallo MR, Cotugno M, Felzani G, Francavilla S, Francavilla F (2016) Low testosterone and non-alcoholic fatty liver disease: evidence for their independent association in men with chronic spinal cord injury. J Spinal Cord Med 39(4):443–449. https://doi.org/10.1179/2045772314Y.0000000288
Di Giulio F, Castellini C, Tienforti D, Felzani G, Baroni MG, Barbonetti A (2023) Independent association of hypovitaminosis d with non-alcoholic fatty liver disease in people with chronic spinal cord injury: a cross-sectional study. J Endocrinol Invest. https://doi.org/10.1007/s40618-023-02124-1
Elder CP, Apple DF, Bickel CS, Meyer RA, Dudley GA (2004) Intramuscular fat and glucose tolerance after spinal cord injury—a cross-sectional study. Spinal Cord 42(12):711–716. https://doi.org/10.1038/sj.sc.3101652
Gallagher EJ, Leroith D, Karnieli E (2011) The metabolic syndrome—from insulin resistance to obesity and diabetes. Med Clin North Am 95(5):855–873. https://doi.org/10.1016/j.mcna.2011.06.001
Jones LM, Legge M, Goulding A (2003) Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil 84(7):1068–1071. https://doi.org/10.1016/s0003-9993(03)00045-5
Nash MS, Groah SL, Gater DR, Dyson-Hudson TA, Lieberman JA, Myers J, Sabharwal S, Taylor AJ (2019) Identification and management of cardiometabolic risk after spinal cord injury. J Spinal Cord Med 42(5):643–677. https://doi.org/10.1080/10790268.2018.1511401
Laughton GE, Buchholz AC, Martin Ginis KA, Goy RE, SHAPE SCI Research Group (2009) Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal Cord 47(10):757–762
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15(7):539–553
Ford ES (2005) Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care 28(11):2745–2749. https://doi.org/10.2337/diacare.28.11.2745
Gater DR Jr, Farkas GJ, Berg AS, Castillo C (2019) Prevalence of metabolic syndrome in veterans with spinal cord injury. J Spinal Cord Med 42(1):86–93. https://doi.org/10.1080/10790268.2017.1423266
Gater DR Jr, Farkas GJ, Dolbow DR, Berg A, Gorgey AS (2021) Body composition and metabolic assessment after motor complete spinal cord injury: development of a clinically relevant equation to estimate body fat. Top Spinal Cord Inj Rehabil 27(1):11–22. https://doi.org/10.46292/sci20-00079
Silveira SL, Ledoux TA, Robinson-Whelen S, Stough R, Nosek MA (2017) Methods for classifying obesity in spinal cord injury: a review. Spinal Cord 55(9):812–817. https://doi.org/10.1038/sc.2017.79
Nash MS, Gater DR Jr (2020) Cardiometabolic disease and dysfunction following spinal cord injury: origins and guideline-based countermeasures. Phys Med Rehabil Clin N Am 31(3):415–436. https://doi.org/10.1016/j.pmr.2020.04.005
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251. https://doi.org/10.1016/0895-4356(94)90129-5
Maynard FM Jr, Bracken MB, Creasey G, Ditunno JF Jr, Donovan WH, Ducker TB, Garber SL, Marino RJ, Stover SL, Tator CH, Waters RL, Wilberger JE, Young W (1997) International standards for neurological and functional classification of spinal cord injury. Am Spinal Injury Assoc Spinal Cord 35(5):266–274. https://doi.org/10.1038/sj.sc.3100432
Bryce TN, Budh CN, Cardenas DD, Dijkers M, Felix ER, Finnerup NB, Kennedy P, Lundeberg T, Richards JS, Rintala DH, Siddall P, Widerstrom-Noga E (2007) Pain after spinal cord injury: an evidence-based review for clinical practice and research. Report of the National Institute on disability and rehabilitation research spinal cord injury measures meeting. J Spinal Cord Med 30(5):421–440. https://doi.org/10.1080/10790268.2007.11753405
Anderson K, Aito S, Atkins M, Biering-Sørensen F, Charlifue S, Curt A, Ditunno J, Glass C, Marino R, Marshall R, Mulcahey MJ, Post M, Savic G, Scivoletto G, Catz A, Functional Recovery Outcome Measures Work Group (2008) Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med 31(2):133–144. https://doi.org/10.1080/10790268.2008.11760704
Martin Ginis KA, Phang SH, Latimer AE, Arbour-Nicitopoulos KP (2012) Reliability and validity tests of the leisure time physical activity questionnaire for people with spinal cord injury. Arch Phys Med Rehabil 93(4):677–682. https://doi.org/10.1016/j.apmr.2011.11.005
Barbonetti A, Sperandio A, Micillo A, D’Andrea S, Pacca F, Felzani G, Francavilla S, Francavilla F (2016) Independent association of vitamin D with physical function in people with chronic spinal cord injury. Arch Phys Med Rehabil 97(5):726–732. https://doi.org/10.1016/j.apmr.2016.01.002
Barbonetti A, D’Andrea S, Castellini C, Totaro M, Muselli M, Cavallo F, Felzani G, Necozione S, Francavilla S (2021) Erectile dysfunction is the main correlate of depression in men with chronic spinal cord injury. J Clin Med 10(10):2090. https://doi.org/10.3390/jcm10102090
Barbonetti A, Cavallo F, D’Andrea S, Muselli M, Felzani G, Francavilla S, Francavilla F (2017) Lower vitamin D levels are associated with de-pression in people with chronic spinal cord injury. Arch Phys Med Rehabil 98(5):940–946. https://doi.org/10.1016/j.apmr.2016.11.006
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419. https://doi.org/10.1007/BF00280883
Kuk JL, Ardern CI (2010) Age and sex differences in the clustering of metabolic syndrome factors: association with mortality risk. Diabetes Care 33(11):2457–2461. https://doi.org/10.2337/dc10-0942
Stampacchia G, Gerini A, Morganti R, Felzani G, Marani M, Massone A, Onesta MP, Capeci W, Andretta E, Campus G, Marchino C, Cicioni V (2022) Research Partners. Pain characteristics in Italian people with spinal cord injury: a multicentre study. Spinal Cord 60(7):604–611. https://doi.org/10.1038/s41393-021-00656-y
Craig AR, Hancock KM, Dickson HG (1994) A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Paraplegia 32(10):675–679. https://doi.org/10.1038/sc.1994.109
Macleod AD (1988) Self-neglect of spinal injured patients. Paraplegia 26(5):340–349. https://doi.org/10.1038/sc.1988.48
DeVivo MJ, Black KJ, Richards JS, Stover SL (1991) Suicide following spinal cord injury. Paraplegia 29(9):620–627. https://doi.org/10.1038/sc.1991.91
Gupta N, White KT, Sandford PR (2006) Body mass index in spinal cord injury—a retrospective study. Spinal Cord 44(2):92–94. https://doi.org/10.1038/sj.sc.3101790
Shin JW, Kim T, Lee BS, Kim O (2022) Factors affecting metabolic syndrome in individuals with chronic spinal cord injury. Ann Rehabil Med 46(1):24–32. https://doi.org/10.5535/arm.21144
Weaver FM, Collins EG, Kurichi J, Miskevics S, Smith B, Rajan S, Gater D (2007) Prevalence of obesity and high blood pressure in veterans with spinal cord injuries and disorders: a retrospective review. Am J Phys Med Rehabil 86(1):22–29. https://doi.org/10.1097/phm.0b013e31802b8937
Kazamel M, Stino AM, Smith AG (2021) Metabolic syndrome and peripheral neuropathy. Muscle Nerve 63(3):285–293. https://doi.org/10.1002/mus.27086
Bonomo R, Kramer S, Aubert VM (2022) Obesity-associated neuropathy: recent preclinical studies and proposed mechanisms. Antioxid Redox Signal 37(7–9):597–612. https://doi.org/10.1089/ars.2021.0278
Stavniichuk R, Shevalye H, Lupachyk S, Obrosov A, Groves JT, Obrosova IG, Yorek MA (2014) Peroxynitrite and protein nitration in the pathogenesis of diabetic peripheral neuropathy. Diabetes Metab Res Rev 30(8):669–678. https://doi.org/10.1002/dmrr.2549
Rumora AE, LoGrasso G, Haidar JA, Dolkowski JJ, Lentz SI, Feldman EL (2019) Chain length of saturated fatty acids regulates mitochondrial trafficking and function in sensory neurons. J Lipid Res 60(1):58–70. https://doi.org/10.1194/jlr.M086843
Chowdhury SK, Smith DR, Fernyhough P (2013) The role of aberrant mitochondrial bioenergetics in diabetic neuropathy. Neurobiol Dis 51:56–65. https://doi.org/10.1016/j.nbd.2012.03.016
Fernyhough P (2015) Mitochondrial dysfunction in diabetic neuropathy: a series of unfortunate metabolic events. Curr Diab Rep 15(11):89. https://doi.org/10.1007/s11892-015-0671-9
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116(7):1793–1801. https://doi.org/10.1172/JCI29069.Erratum.In:JClinInvest.2006Aug;116(8):2308
Kellogg AP, Wiggin TD, Larkin DD, Hayes JM, Stevens MJ, Pop-Busui R (2007) Protective effects of cyclooxygenase-2 gene inactivation against peripheral nerve dysfunction and intraepidermal nerve fiber loss in experimental diabetes. Diabetes 56(12):2997–3005. https://doi.org/10.2337/db07-0740
Solinsky R, Betancourt L, Schmidt-Read M, Kupfer M, Owens M, Schwab JM, Dusseau NB 2nd, Szlachcic Y, Sutherland L, Taylor JA, Nash MS (2022) Acute spinal cord injury is associated with prevalent cardiometabolic risk factors. Arch Phys Med Rehabil 103(4):696–701. https://doi.org/10.1016/j.apmr.2021.04.022
Farkas GJ, Gordon PS, Trewick N, Gorgey AS, Dolbow DR, Tiozzo E, Berg AS, Gater DR Jr (2021) Comparison of various indices in identifying insulin resistance and diabetes in chronic spinal cord injury. J Clin Med 10(23):5591. https://doi.org/10.3390/jcm10235591
Funding
Open access funding provided by Università degli Studi dell’Aquila within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
FDG, CC, SP and FA performed literature search, data analysis and interpretation, and drafted the manuscript; CC and DT prepared tables and figure; GF and MGB revised the manuscript critically for important intellectual content; AB conceived the study, supervised the manuscript writing, and critically reviewed and revised the manuscript for intellectual content, by relevantly improving the scientific content and the formal style. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare they have no financial interests. Marco Giorgio Baroni and Arcangelo Barbonetti are members of the Editorial Board of the J Endocrinol Invest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the international and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval was granted by the Ethics Committee of L’Aquila and Teramo provinces, Italy (Approval Code: 11/CE/15 of May 7, 2015).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Participants signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Di Giulio, F., Castellini, C., Palazzi, S. et al. Correlates of metabolic syndrome in people with chronic spinal cord injury. J Endocrinol Invest 47, 2097–2105 (2024). https://doi.org/10.1007/s40618-023-02298-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02298-8