Abstract
Purpose
The Multidimensional Prognostic Index (MPI) is a tool capable of holistically frame older patients in different settings and affected by different pathologies, establishing a risk of adverse events. Among them, type 2 diabetes mellitus (T2DM), a common metabolic disease in the elderly, is responsible for complications and deaths. Few previous works have focused specifically on MPI and DM, and none have followed up the patients for more than 3 years. The aim of the present study is to analyze MPI accuracy in predicting mortality in a cohort of T2DM patients followed-up for 13 years.
Methods
The enrolled subjects were evaluated with MPI, identifying three levels of risk: MPI1 (low risk, 0.0–0.33), MPI2 (moderate risk, 0.34–0.66), and MPI3 (severe risk, 0.67–1.0), and with glycated hemoglobin, and years since T2DM diagnosis.
Results
One hundred and seven patients met the inclusion criteria. MPI3 was excluded by further analysis since it was made up of only three patients. Overall, cognitive performances, autonomies in daily living, nutritional status, risk of pressure injuries, comorbidities, and taken drugs were better (p ≤ 0.0077) in MPI1 than MPI2; moreover, the story of T2DM was shorter (p = 0.0026). Cox model showed an overall 13-year survival of 51.9%, and survival rates were significantly smaller in MPI2 (HR: 4.71, p = 0.0007). Finally, increased age (HR: 1.15), poorer cognitive abilities (HR: 1.26), vascular (HR: 2.15), and kidney (HR: 2.17) diseases were independently associated with death.
Conclusion
Our results prove that MPI predicts short-, mid-, and even long-term mortality in T2DM patients, whose death seems to be related to age and cognitive status, and even more to vascular and kidney diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The increasing aging of the population has led to a proportional increase in the incidence of age-related conditions and diseases as well, such as sarcopenia [1], high falling risk, and reduced physical performance [2, 3], which lead to increased mortality, and also mild and severe neurocognitive disorders [4], metabolic syndrome [5], multifactorial anemia [6], and cardiovascular diseases, such as hypertension [7], cardiac failure [8], and atrial fibrillation [9]. Among them, Diabetes Mellitus (DM) deserves an honorable mention. It indicates a common metabolic disease, characterized by chronic hyperglycemia resulting from a deficit in insulin secretion and/or, most commonly, action [10,11,12]. The most prevalent form is called “type 2”, increasing when increasing age is called “type 2” (T2DM) [13], to differentiate it from “type 1”, caused by an absolute insulin secretion because of autoimmune mechanisms [14]. Elderly people are frequently affected by T2DM, often combined with other cardiometabolic disorders such as visceral obesity or hypertension [15,16,17]. It represents one of the most common diseases worldwide [11], and in Italy: the ARNO Diabetes Observatory showed an incidence rate of 5.83 per 1000 persons-years [18], and a prevalence of 6.2% [19], with growing incidence rates when growing age. Oral antidiabetic drugs [20,21,22], the prototype of which is metformin [23], increased survival rates and quality of life [24, 25]. Advanced forms of T2DM can instead require constant administration of insulin [26], which appeared to be over-prescribed in Italy, according to the ARNO Diabetes Observatory data [27]. Most recently, new drugs have been able to substantially change the history of the disease, namely sodium-glucose cotransporter 2 (SGLT2) inhibitors, and glucagon-like peptide-1 receptor agonists (GLP1-RA). SGLT2 inhibitors are associated with a reduction in body mass and pressure [28], improving cardiorenal outcomes [29]; GLP1-RA nowadays represents a second-line treatment in T2DM [30], and, as described for SGLT2 inhibitors, are associated with a reduction of cardiovascular risk, probably also thanks to crucial effects on renin-angiotensin system [31].
Being able to predict death assumes particular importance in elderly people, and comprehensive geriatric assessment (CGA) offers a specialistic help in this sense, by holistically examining elderly people, often with multiple diseases and impaired domains [32]. Pilotto A. et al., in 2008, validated the Multidimensional Prognostic Index (MPI) [33], a useful multidimensional tool which divides the patients into risk classes (low, moderate, and severe), predicting their probability of exitus, rehospitalization, and institutionalization. Starting life for the assessment of hospitalized subjects [33], it received subsequent validations in other settings, like the outpatient one [34, 35], intermediate care facilities [36], and, more recently, even for telephone administration [37]. It was also studied in specific populations, e.g., patients with myocardial infarction [38], acute respiratory failure [39], hip fracture [40, 41], chronic kidney disease [42], DM [43, 44], cancer [45, 46], and even COVID-19 [47]. About studies performed on DM, to the best of our knowledge, they evaluated the patients’ data for a maximum of 3 years after MPI administration [44]. Moreover, although based on common assumptions, that is the usual exclusion of older adults from trials, in the mentioned study [44], the authors specifically focused on statin treatment, demonstrating its association with reduced mortality in DM patients.
According to that, the aim of the present work is to study MPI accuracy in predicting mortality in a cohort of T2DM patients followed-up for 13 years.
Methods
Design of the study
This prospective study included subjects evaluated at the Geriatric Outpatient Service of the University Hospital of Monserrato, Cagliari, Italy, in 2009 and followed-up for a 13-year period.
Inclusion criteria
Age ≥ 65 years; diagnosis of T2DM.
Exclusion criteria
Age < 65 years; absence of T2DM diagnosis; contraindication to MPI (e.g., acute confusion, delirium), informed consent not provided.
Assessment
The enrolled subjects were evaluated with MPI, which ranges from 0 to 1, identifying three levels of risk: MPI1 (low risk, 0.0–0.33), MPI2 (moderate risk, 0.34–0.66), and MPI3 (severe risk, 0.67–1.0) [33]. It is developed by considering the total scores of eight domains:
-
Short Portable Mental Status Questionnaire (SPMSQ) [48], for cognitive assessment. It includes 10 items, and its total scores, corrected for years of school, ranges from 0 (absence of cognitive impairment) to 10 (maximum impairment). Scores < 5 indicate no or mild impairment, from 5 to 7 moderate impairment, and from 8 to 10 severe impairment
-
Activities of Daily Living (ADL) [49], for the assessment of residual autonomies. Its total score ranges from 6 (complete independence) to 0 (complete dependence)
-
Instrumental Activities of Daily Living (IADL) [49], for the assessment of residual autonomies. Its total score ranges from 8 (independence) to 0 (complete dependence)
-
Mini Nutritional Assessment (MNA) [50, 51], for the assessment of nutritional status. Its total score ranges from 30 (excellent nutritional status) to 0 (severe malnutrition). Scores < 17 indicate malnutrition, 17–23.5 risk of malnutrition, ≥ 24 adequate nutritional status
-
Exton-Smith Scale (ESS) [52], for the assessment of the risk of pressure injuries. Its total score ranges from 20 (absence of risk) to 5 (maximum risk). Scores ≤ 12 indicate a surely increased risk
-
Comorbidity Index Rating Scale (CIRS) [53], for the assessment of the comorbidity burden. It evaluates 14 categories of pathologies concerning some organs and systems, hypertension, psychiatric and behavioral aspects. The Comorbidity Index (CIRS-IC) corresponds to the number of categories with ≥ 3 score, indicating an at least moderate and needing treatment alteration
-
Number of different drugs taken
-
Social support (household composition, institutionalization, services)
They were also evaluated with:
-
Glycated hemoglobin (HbA1c) [54], for the estimation of long-term glycemic control
-
Years since T2DM diagnosis
The abovementioned assessment was administered by trained geriatricians in the outpatient setting.
Statistical analysis
Variables were expressed as means and SDs or in percentages (%), where appropriate. Kolmogorov–Smirnov method was used to test normal distribution in continuous variables. Chi-squared test (χ2) and Student’s t-test were used to compare the variables in the groups. Cox proportional hazard model was designed in order to estimate the survival probability: its results were expressed as Hazard Ratios (HRs), and p values > 0.1 were excluded from the model.
The results are reported indicating p values in reference to a 95% Confidence Interval (CI).
MedCalc software (Version 20.218, Ostend, Belgium) was used for the statistical analysis.
Considering confidence level: 95%, confidence interval: 5%, standard deviation (SD): 0.5, Z-score (z): 1.96, and error margin (e): 10%, the final sample (N) should consist of at least 96 subjects, according to the formula
Results
According to inclusion criteria, our study included 107 community-dwelling people aged 65 years or more, of whom 63 were women (58.9%), with an average (SD) age of 74.9 years (5.9). The characteristics of the sample are shown in Table 1.
We divided the sample into three groups, according to MPI scores, obtaining MPI1 (0.0–0.33, made up of 87 subjects), MPI2 (0.34–0.66, made up of 17 subjects), and MPI3 (0.67–1.0, made up of 3 subjects). Since MPI3 presented a significantly lower number of subjects, it was excluded by further analysis. In Table 2, the more common comorbidities are summarized and divided into two groups. The most frequent was hypertension (83.6% of the sample). Peripheral vascular (33.3% vs 64.7%, p = 0.0155), ear/eye (49.4% vs 76.5%, p = 0.0417), musculoskeletal (29.9% vs 58.8%, p = 0.0224), and neurological diseases (12.6% vs 41.2%, p = 0.0046) were significantly more common in MPI2 than in MPI1. As in Table 3, 36.5% of the sample was receiving only diet therapy, while metformin was the most common oral antidiabetic drug taken (28.9%). Moreover, 31.7% took at least one type of insulin (“rapid” and/or “slow”): in particular, 20.6% took “rapid” insulin, 27.1% “slow” insulin, and 14% followed a multiple daily injection therapy. Finally, 7.5% of the patients followed a multidrug regimen, and 6.5% took basal-supported oral therapy (BOT). About other drugs, diuretics (28.7% vs 58.8%, p = 0.0169) and proton pump inhibitors (24.1 vs 52.9%, p = 0.0170) were more commonly taken by MPI2 than MPI1 patients.
As in Table 4, age, ADL, IADL, MNA, and ESS were significantly higher in MPI1 than in MPI2. On the contrary, SPMSQ, CIRS-CI, number of drugs taken, and years since T2DM diagnosis were significantly lower in MPI1 than MPI2. The analysis also showed that HbA1c values did not significantly differ among the groups.
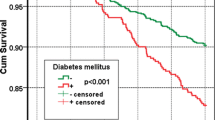
The whole sample was followed-up for 13 years, and the overall 13-year survival rate was 51.9% (the analysis of year-by-year-survival rates is shown in Table 5). The comparison of survival curves (Figure 1) revealed a significant difference among the two groups (p = 0.0007). MPI1 group presented higher survival rates than MPI2 since year 1 (94.3% vs 88.2%), afterwards the gap among them widening, until reaching 63.2% vs 23.5% survival rate on the eleventh year, as confirmed by the HR of 4.71 (CI 1.91–11.57). For the sake of completeness, the MPI3’s 2-years survival rate was 0%, and merging MPI2 and MPI3 the abovementioned gap widened to 63.2% vs 20.0% on the eleventh year (HR: 6.29, CI 2.68–14.79).
The Cox regression model, conducted in order to study the independence of different variables associated with the “death” outcome, included age, SPMSQ, ADL, IADL, MNA, CIRS-IC, numbers of drugs taken, HbA1c, years since T2DM diagnosis, and also the presence/absence of the diseases listed in Table 2, and the assumption of the drugs listed in Table 3. It highlighted age (HR: 1.15, CI 1.01–1.22, p < 0.0001), SPMSQ (HR: 1.26, CI 1.03–1.55, p = 0.0274), vascular (HR: 2.15, CI 1.25–4.12, p = 0.0205) and kidney (HR: 2.17, CI 1.21–3.89, p = 0.0089) diseases to be significantly associated with the event, while the others were excluded by the model, as in Figure 2. In particular, among vascular comorbidities, carotid atherosclerosis (42.5%), and chronic arteriopathy of the lower limbs (27.5%) were the most frequent in the sample, while cystic kidney disease (62.5%), and chronic kidney disease (31.25%) were the most represented among kidney comorbidities.
Discussion
Nowadays, T2DM represents one of the most common metabolic diseases worldwide, especially in the elderly [11, 13, 18, 19]. CGA is a specialistic tool to holistically assess older adults [32], and MPI represents one of its expressions [33] in various settings and for several diseases. Nevertheless, to the best of our knowledge, no previous focused-on-DM MPI application considered longer than 3 years outcomes. Our work fits into this line of research, aiming to study, in a cohort of T2DM patients, MPI accuracy not only in predicting short- and mid- [43, 44], but even long-term mortality. In order to achieve such an objective, we recruited subjects aged 65 years or more, with an average age of 74.9 years and followed them up for 13 years.
In the study population, the average risk of the negative event was low, cognitive abilities were adequate, and so were the autonomies in performing basic and instrumental activities of daily living as well; the population also presented a risk of malnutrition, mild risk of pressure injuries, and polypharmacotherapy [55], an important issue in elderly given the high number of under- and over-prescriptions in several diseases [56, 57]. Moreover, it averagely presented more than 4 needing treatment conditions. As far as it concerns average (SD) glycated hemoglobin, it was 7 (1.5), representing satisfactory glycemic control for elderly diabetics [53, 58].
The variables were studied among two out of three groups based on risk stratification (MPI1, low, and MPI2, moderate risk, while MPI3, severe risk of an adverse event, made up of a significantly lower number than the others, was excluded by the analysis). Anyway, overall, cognitive performances, autonomies in daily living, nutritional status, risk of pressure injuries, comorbidities, and taken drugs were better (p ≤ 0.0077) in people with lower risk. It goes without saying that such an association is coherent with MPI calculation – being it built according to the abovementioned variables [33], while an interesting data that emerged was that people with the low risk presented a shorter story of DM than people with moderate and high risk as well (p = 0.0026). Another significant result is represented by the fact that glycated hemoglobin percentage did not show a significant difference (p = 0.0555) among the groups. It would be explained by the fact that the two groups largely differed in size: the worse glycemic control might possibly affect the increased mortality in the MPI2 group.
Following the aim of the study, we considered the deaths over 13 years, obtaining survival curves: they showed that the MPI2 group presented more than 470% of risk to die (HR: 4.71) with respect to MPI1. This deeply increased mortality cannot depend only on the higher age in MPI2 patients, but it is rather certainly influenced also by the abovementioned more compromised general status of the group, and possibly the worse glycemic control. These aspects were reinforced by the fact that multivariate analysis showed that increased age (HR: 1.15), poorer cognitive abilities (HR: 1.26), and the presence of vascular and kidney diseases (HRs: 2.15 and 2.17, respectively) were independently associated with long-term death. What emerged is consistent with the literature [59,60,61], and even with the natural history of diabetes, the most common complications of which are really represented by vascular and kidney affections [62].
Unfortunately, being MPI3 made up of a too low number of subjects, the HRs concerning it would not have been statistically significant, though they would have likely shown a clear tendency, owing to the fact that the whole group had passed away by the second follow-up year.
This is the first study monitoring DM patients evaluated with MPI over such a long period, and this represents its greatest strength. Obviously, we recognize some limitations, represented by the monocentric nature of the study, and the relatively low number of enrolled subjects, especially for the MPI3 group, all the more so because we believe that a higher representation of this group could have further reinforced the results. Another limitation is represented by the absence of data related to new drugs (SGLT2 inhibitors, GLP1-RA), which as previously stated [28,29,30,31] have modified the history of DM and the prevalence of its complications.
Conclusions
In conclusion, this study proved that MPI is able to predict short-, mid- (as previously demonstrated [44]), and even long-term mortality in T2DM patients, whose death seems to be related to age, cognitive status, and vascular and kidney diseases. Further studies with larger samples and longitudinal follow-up are needed to confirm and deepen our results, especially since new antidiabetic agents have proved to influence cardiovascular and all-cause mortality in DM.
Data availability
The data and materials used and/or analyzed during the current study are not publicly available. They are available from the corresponding author upon reasonable request.
Abbreviations
- ADL:
-
Activities of daily living
- CI:
-
95% Confidence interval
- CIRS:
-
Cumulative illness rating scale
- CIRS-IC:
-
Cumulative illness rating scale-comorbidity index
- CGA:
-
Comprehensive geriatric assessment
- DM:
-
Diabetes mellitus
- ESS:
-
Exton-Smith scale
- HbA1c:
-
Glycated hemoglobin
- IADL:
-
Instrumental activities of daily living
- MNA:
-
Mini nutritional assessment
- MPI:
-
Multidimensional prognostic index
- MPI1:
-
MPI 0.0–0.33
- MPI2:
-
MPI 0.34–0.66
- MPI3:
-
MPI 0.67–1.00
- n.:
-
Number
- SD:
-
Standard deviation
- SPMSQ:
-
Short Portable Mental State Questionnaire
- T2DM:
-
Type 2 diabetes mellitus
References
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia [published correction appears in Lancet. 2019 Jun 29;393(10191):2590]. Lancet 393(10191):2636–2646. https://doi.org/10.1016/S0140-6736(19)31138-9
Salis F, Mandas A (2023) Physical performance and falling risk are associated with five-year mortality in older adults: an observational cohort study. Medicina 59(5):964. https://doi.org/10.3390/medicina59050964
Wang DXM, Yao J, Zirek Y, Reijnierse EM, Maier AB (2020) Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle 11(1):3–25. https://doi.org/10.1002/jcsm.12502
Salis F, Costaggiu D, Mandas A (2023) Mini-mental state examination: optimal cut-off levels for mild and severe cognitive impairment. Geriatrics 8(1):12. https://doi.org/10.3390/geriatrics8010012
Moura ARDS, Paz SMRSD, Frota KMG, Carvalho CMRG (2022) Lifestyle associated with risk of metabolic syndrome in adults and the elderly. Nutrition 99–100:111647. https://doi.org/10.1016/j.nut.2022.111647
Salis F, Locci G, Mura B, Mandas A (2023) Anemia in elderly patients-the impact of hemoglobin cut-off levels on geriatric domains. Diagnostics (Basel) 13(2):191. https://doi.org/10.3390/diagnostics13020191
Robles NR, Macias JF (2015) Hypertension in the elderly. Cardiovasc Hematol Agents Med Chem 12(3):136–145. https://doi.org/10.2174/1871525713666150310112350
Sunayama T, Matsue Y, Dotare T, Maeda D, Iso T, Morisawa T, Saitoh M, Yokoyama M, Jujo K, Takahashi T, Minamino T (2022) Multidomain frailty as a therapeutic target in elderly patients with heart failure. Int Heart J 63(1):1–7. https://doi.org/10.1536/ihj.21-839
Salis F, Palimodde A, Demelas G, Scionis MI, Mandas A (2023) Frailty and comorbidity burden in atrial fibrillation. Front Public Health 9(11):1134453. https://doi.org/10.3389/fpubh.2023.1134453
Guthrie RA, Guthrie DW (2004) Pathophysiology of diabetes mellitus. Crit Care Nurs Q 27(2):113–125. https://doi.org/10.1097/00002727-200404000-00003
American Diabetes Association (2013) Diagnosis and classification of diabetes mellitus. Diabetes Care 36(Suppl 1):S67-74. https://doi.org/10.2337/dc13-S067
Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L, Groop PH, Handelsman Y, Insel RA, Mathieu C, McElvaine AT, Palmer JP, Pugliese A, Schatz DA, Sosenko JM, Wilding JP, Ratner RE (2017) Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes 66(2):241–255. https://doi.org/10.2337/db16-0806. (Epub 2016 Dec 15)
Brunton S (2016) Pathophysiology of type 2 diabetes: the evolution of our understanding. J Fam Pract 65(4 Suppl):supp_az_0416
Desai S, Deshmukh A (2020) Mapping of type 1 diabetes mellitus. Curr Diabetes Rev 16(5):438–441. https://doi.org/10.2174/1573399815666191004112647
Park JJ (2021) Epidemiology, pathophysiology, diagnosis and treatment of heart failure in diabetes. Diabetes Metab J 45(2):146–157. https://doi.org/10.4093/dmj.2020.0282. (Epub 2021 Mar 25. Erratum in: Diabetes Metab J. 2021 Sep; 45(5):796)
Chobot A, Górowska-Kowolik K, Sokołowska M, Jarosz-Chobot P (2018) Obesity and diabetes—not only a simple link between two epidemics. Diabetes Metab Res Rev 34(7):e3042. https://doi.org/10.1002/dmrr.3042. (Epub 2018 Jul 17)
Grossman A, Grossman E (2017) Blood pressure control in type 2 diabetic patients. Cardiovasc Diabetol 16(1):3. https://doi.org/10.1186/s12933-016-0485-3
Bonora E, Cataudella S, Marchesini G, Miccoli R, Vaccaro O, Fadini GP, Martini N, Rossi E, under the mandate of the Italian Diabetes Society (2021) Incidence of diabetes mellitus in Italy in year 2018. A nationwide population-based study of the ARNO Diabetes Observatory. Nutr Metab Cardiovasc Dis 31(8):2338–2344. https://doi.org/10.1016/j.numecd.2021.04.017. (Epub 2021 May 3)
Bonora E, Cataudella S, Marchesini G, Miccoli R, Vaccaro O, Fadini GP, Martini N, Rossi E (2020) Clinical burden of diabetes in Italy in 2018: a look at a systemic disease from the ARNO Diabetes Observatory. BMJ Open Diabetes Res Care 8(1):e001191. https://doi.org/10.1136/bmjdrc-2020-001191
Kecskemeti V, Bagi Z, Pacher P, Posa I, Kocsis E, Koltai MZ (2002) New trends in the development of oral antidiabetic drugs. Curr Med Chem 9(1):53–71. https://doi.org/10.2174/0929867023371427
Dahlén AD, Dashi G, Maslov I, Attwood MM, Jonsson J, Trukhan V, Schiöth HB (2022) Trends in antidiabetic drug discovery: FDA approved drugs, new drugs in clinical trials and global sales. Front Pharmacol 12:807548. https://doi.org/10.3389/fphar.2021.807548
Flory J, Lipska K (2019) Metformin in 2019. JAMA 321(19):1926–1927. https://doi.org/10.1001/jama.2019.3805
Tsapas A, Avgerinos I, Karagiannis T, Malandris K, Manolopoulos A, Andreadis P, Liakos A, Matthews DR, Bekiari E (2020) Comparative effectiveness of glucose-lowering drugs for type 2 diabetes: a systematic review and network meta-analysis. Ann Intern Med 173(4):278–286. https://doi.org/10.7326/M20-0864. (Epub 2020 Jun 30)
Mohammed I, Hollenberg MD, Ding H, Triggle CR (2021) A critical review of the evidence that metformin is a putative anti-aging drug that enhances healthspan and extends lifespan. Front Endocrinol (Lausanne). 12:718942. https://doi.org/10.3389/fendo.2021.718942
Sayyed Kassem L, Aron DC (2020) The assessment and management of quality of life of older adults with diabetes mellitus. Expert Rev Endocrinol Metab 15(2):71–81. https://doi.org/10.1080/17446651.2020.1737520. (Epub 2020 Mar 16)
Chellappan DK, Yap WS, Bt Ahmad Suhaimi NA, Gupta G, Dua K (2018) Current therapies and targets for type 2 diabetes mellitus. Panminerva Med 60(3):117–131. https://doi.org/10.23736/S0031-0808.18.03455-9. (Epub 2018 Apr 24)
Bonora E, Cataudella S, Marchesini G, Miccoli R, Vaccaro O, Fadini GP, Martini N, Rossi E, mandate of the Italian Diabetes Society (2021) Initial treatment of diabetes in Italy. A nationwide population-based study from of the ARNO Diabetes Observatory. Nutr Metab Cardiovasc Dis 31(9):2661–2668. https://doi.org/10.1016/j.numecd.2021.06.006. (Epub 2021 Jun 22)
Cowie MR, Fisher M (2020) SGLT2 inhibitors: mechanisms of cardiovascular benefit beyond glycaemic control. Nat Rev Cardiol 17(12):761–772. https://doi.org/10.1038/s41569-020-0406-8. (Epub 2020 Jul 14)
Salvatore T, Galiero R, Caturano A, Rinaldi L, Di Martino A, Albanese G, Di Salvo J, Epifani R, Marfella R, Docimo G, Lettieri M, Sardu C, Sasso FC (2022) An overview of the cardiorenal protective mechanisms of SGLT2 inhibitors. Int J Mol Sci 23(7):3651. https://doi.org/10.3390/ijms23073651
Ng E, Shaw JE, Wood A, Maple-Brown LJ, Hare MJ (2022) Glucagon-like peptide-1 receptor agonist (GLP1-RA) therapy in type 2 diabetes. Aust J Gen Pract 51(7):513–518. https://doi.org/10.31128/AJGP-07-21-6057
Puglisi S, Rossini A, Poli R, Dughera F, Pia A, Terzolo M, Reimondo G (2021) Effects of SGLT2 inhibitors and GLP-1 receptor agonists on renin-angiotensin-aldosterone system. Front Endocrinol (Lausanne). 12:738848. https://doi.org/10.3389/fendo.2021.738848
Salis F, Loddo S, Zanda F, Peralta MM, Serchisu L, Mandas A (2022) Comprehensive geriatric assessment: application and correlations in a real-life cross-sectional study. Front Med (Lausanne). 9:984046. https://doi.org/10.3389/fmed.2022.984046
Pilotto A, Ferrucci L, Franceschi M, D’Ambrosio LP, Scarcelli C, Cascavilla L, Paris F, Placentino G, Seripa D, Dallapiccola B, Leandro G (2008) Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res 11(1):151–161. https://doi.org/10.1089/rej.2007.0569
Overbeek FCMS, Goudzwaard JA, van Hemmen J, van Bruchem-Visser RL, Papma JM, Polinder-Bos HA, Mattace-Raso FUS (2022) The multidimensional prognostic index predicts mortality in older outpatients with cognitive decline. J Clin Med 11(9):2369. https://doi.org/10.3390/jcm11092369
Gallucci M, Battistella G, Bergamelli C, Spagnolo P, Mazzuco S, Carlini A, Di Giorgi E, Boldrini P, Pilotto A (2014) Multidimensional prognostic index in a cognitive impairment outpatient setting: mortality and hospitalizations. The Treviso Dementia (TREDEM) study. J Alzheimers Dis 42(4):1461–1468. https://doi.org/10.3233/JAD-140516
Veronese N, Vianello S, Danesin C, Tudor F, Pozzobon G, Pilotto A (2021) Multidimensional prognostic index and mortality in intermediate care facilities: a retrospective study. J Clin Med 10(12):2632. https://doi.org/10.3390/jcm10122632
Custodero C, Senesi B, Pinna A, Floris A, Vigo M, Fama M, Mastropierro V, Sabbà C, Prete C, Pilotto A (2021) Validation and implementation of telephone-administered version of the multidimensional prognostic index (TELE-MPI) for remote monitoring of community-dwelling older adults. Aging Clin Exp Res 33(12):3363–3369. https://doi.org/10.1007/s40520-021-01871-6. (Epub 2021 May 18)
Cammalleri V, Bonanni M, Bueti FM, Matteucci A, Cammalleri L, Stifano G, Muscoli S, Romeo F (2021) Multidimensional prognostic index (MPI) in elderly patients with acute myocardial infarction. Aging Clin Exp Res 33(7):1875–1883. https://doi.org/10.1007/s40520-020-01718-6. (Epub 2020 Oct 1)
Custodero C, Gandolfo F, Cella A, Cammalleri LA, Custureri R, Dini S, Femia R, Garaboldi S, Indiano I, Musacchio C, Podestà S, Tricerri F, Pasa A, Sabbà C, Pilotto A (2021) Multidimensional prognostic index (MPI) predicts non-invasive ventilation failure in older adults with acute respiratory failure. Arch Gerontol Geriatr 94:104327. https://doi.org/10.1016/j.archger.2020.104327. (Epub 2020 Dec 24)
Vitale E, Notarnicola A, Moretti L, Antonio E, Pesce V, Moretti B (2012) Multidimensional prognostic index in the elderly with hip or neck femur fracture. Orthop Rev (Pavia). 4(2):e15. https://doi.org/10.4081/or.2012.e15. (Epub 2012 Apr 12)
Musacchio C, Custodero C, Razzano M, Raiteri R, Delrio A, Torriglia D, Stella M, Puntoni M, Sabbà C, Barone A, Pilotto A (2022) Association between multidimensional prognostic index (MPI) and pre-operative delirium in older patients with hip fracture. Sci Rep 12(1):16920. https://doi.org/10.1038/s41598-022-20734-2
Pilotto A, Panza F, Sancarlo D, Paroni G, Maggi S, Ferrucci L (2012) Usefulness of the multidimensional prognostic index (MPI) in the management of older patients with chronic kidney disease. J Nephrol 25(Suppl 19):S79-84. https://doi.org/10.5301/jn.5000162
Pilotto A, Noale M, Maggi S, Addante F, Tiengo A, Perin PC, Rengo G, Crepaldi G (2014) Hypoglycemia is independently associated with multidimensional impairment in elderly diabetic patients. Biomed Res Int 2014:906103. https://doi.org/10.1155/2014/906103. (Epub 2014 Feb 13)
Pilotto A, Panza F, Copetti M, Simonato M, Sancarlo D, Gallina P, Strandberg T, MPI_AGE Project Investigators (2015) Statin treatment and mortality in community-dwelling frail older patients with diabetes mellitus: a retrospective observational study. PLoS ONE 10(6):e0130946. https://doi.org/10.1371/journal.pone.0130946
Giantin V, Falci C, De Luca E, Valentini E, Iasevoli M, Siviero P, Maggi S, Martella B, Crepaldi G, Monfardini S, Manzato E (2018) Performance of the multidimensional geriatric assessment and multidimensional prognostic index in predicting negative outcomes in older adults with cancer. Eur J Cancer Care (Engl). 27(1):e12585. https://doi.org/10.1111/ecc.12585. (Epub 2016 Oct 10)
Giantin V, Valentini E, Iasevoli M, Falci C, Siviero P, De Luca E, Maggi S, Martella B, Orrù G, Crepaldi G, Monfardini S, Terranova O, Manzato E (2013) Does the multidimensional prognostic index (MPI), based on a comprehensive geriatric assessment (CGA), predict mortality in cancer patients? Results of a prospective observational trial. J Geriatr Oncol 4(3):208–217. https://doi.org/10.1016/j.jgo.2013.04.008. (Epub 2013 May 24)
Pilotto A, Azzini M, Cella A, Cenderello G, Castagna A, Pilotto A, Custureri R, Dini S, Farinella ST, Ruotolo G, Padovani A, Custodero C, Veronese N, Italian Geriatric Society Hospital and Community (SIGOT) Study Group (2021) The multidimensional prognostic index (MPI) for the prognostic stratification of older inpatients with COVID-19: a multicenter prospective observational cohort study. Arch Gerontol Geriatr 95:104415. https://doi.org/10.1016/j.archger.2021.104415. (Epub 2021 Apr 5)
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23(10):433–441. https://doi.org/10.1111/j.1532-5415.1975.tb00927.x
Pashmdarfard M, Azad A (2020) Assessment tools to evaluate activities of daily living (ADL) and instrumental activities of daily living (IADL) in older adults: a systematic review. Med J Islam Repub Iran 13(34):33. https://doi.org/10.34171/mjiri.34.33
Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, Albarede JL (1999) The mini nutritional assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15(2):116–122. https://doi.org/10.1016/s0899-9007(98)00171-3
Loddo S, Salis F, Rundeddu S, Serchisu L, Peralta MM, Mandas A (2022) Nutritional status and potentially inappropriate medications in elderly. J Clin Med 11(12):3465. https://doi.org/10.3390/jcm11123465
Bliss MR, McLaren R, Exton-Smith AN (1966) Mattresses for preventing pressure sores in geriatric patients. Mon Bull Minist Health Public Health Lab Serv 25:238–268
Parmelee PA, Thuras PD, Katz IR, Lawton MP (1995) Validation of the cumulative illness rating scale in a geriatric residential population. J Am Geriatr Soc 43(2):130–137. https://doi.org/10.1111/j.1532-5415.1995.tb06377.x
Weykamp C (2013) HbA1c: a review of analytical and clinical aspects. Ann Lab Med 33(6):393–400. https://doi.org/10.3343/alm.2013.33.6.393. (Epub 2013 Oct 17)
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE (2017) What is polypharmacy? A systematic review of definitions. BMC Geriatr 17(1):230 (Published 2017 Oct 10)
Salis F, Palimodde A, Rundeddu S, Mandas A (2023) STOPP/START anti-aggregation and anticoagulation alerts in atrial fibrillation [published online ahead of print, 2023 Apr 18]. Curr Vasc Pharmacol. https://doi.org/10.2174/1570161121666230418163016
Rankin A, Cadogan CA, Patterson SM, Kerse N, Cardwell CR, Bradley MC, Ryan C, Hughes C (2018) Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 9(9):CD008165. https://doi.org/10.1002/14651858.CD008165.pub4
Farcet A, Delalande G, Oliver C, Retornaz F (2016) À propos du dosage de l’HbA1c chez le sujet âgé [about the HbA1c in the elderly]. Geriatr Psychol Neuropsychiatr Vieil 14(1):42–48. https://doi.org/10.1684/pnv.2016.0588
Nanayakkara N, Curtis AJ, Heritier S et al (2021) Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia 64(2):275–287. https://doi.org/10.1007/s00125-020-05319-w
Koye DN, Magliano DJ, Nelson RG, Pavkov ME (2018) The global epidemiology of diabetes and kidney disease. Adv Chronic Kidney Dis 25(2):121–132. https://doi.org/10.1053/j.ackd.2017.10.011
Schlesinger S, Neuenschwander M, Barbaresko J et al (2022) Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies. Diabetologia 65(2):275–285. https://doi.org/10.1007/s00125-021-05592-3
Faselis C, Katsimardou A, Imprialos K, Deligkaris P, Kallistratos M, Dimitriadis K (2020) Microvascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol 18(2):117–124. https://doi.org/10.2174/1570161117666190502103733
Funding
Open access funding provided by Università degli Studi di Cagliari within the CRUI-CARE Agreement. This research received no external funding.
Author information
Authors and Affiliations
Contributions
FS and AM contributed to the study design, and the interpretation of the findings; FS and EC contributed to data collection; FS performed data analysis and wrote the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the University of Cagliari (protocol code NP/2022/1382, 30 March 2022).
Informed Consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salis, F., Cossu, E. & Mandas, A. The multidimensional prognostic index (MPI) predicts long-term mortality in old type 2 diabetes mellitus patients: a 13-year follow-up study. J Endocrinol Invest 47, 191–200 (2024). https://doi.org/10.1007/s40618-023-02135-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02135-y