Abstract
Purpose
To assess the prevalence of pre-diabetes phenotypes, i.e., impaired fasting glucose (IFG), impaired glucose tolerance (IGT), increased HbA1c (IA1c), and their association with metabolic profile and atherogenic lipid profile in youths with overweight/obesity (OW/OB).
Methods
This cross-sectional study analyzed data of 1549 youths (5–18 years) with OW/OB followed in nine Italian centers between 2016 and 2020. Fasting and post-load measurements of glucose, insulin, and HbA1c were available. Insulin resistance (IR) was estimated by HOMA-IR and insulin sensitivity (IS) by reciprocal of fasting insulin. The atherogenic lipid profile was assessed by triglycerides-to-HDL ratio or cholesterol-to-HDL ratio. Insulinogenic index was available in 939 youths, in whom the disposition index was calculated.
Results
The prevalence of overall pre-diabetes, IFG, IGT and IA1c was 27.6%, 10.2%, 8% and 16.3%, respectively. Analyzing each isolated phenotype, IGT exhibited two- to three-fold higher odds ratio of family history of diabetes, and worse metabolic and atherogenic lipid profile vs normoglycemic youths; IFG was associated only with IR, while IA1c showed a metabolic and atherogenic lipid profile intermediate between IGT and IFG.
Conclusion
Prevalence of pre-diabetes was high and IA1c was the most prevalent phenotype in Italian youths with OW/OB. The IGT phenotype showed the worst metabolic and atherogenic lipid profile, followed by IA1c. More studies are needed to assess whether HbA1c may help improving the prediction of diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity (OB) affects millions of youths worldwide and imposes early in the life a heavy burden of cardiovascular and metabolic comorbidities, such as hypertension, dyslipidemia, liver steatosis and abnormal glucose regulation. In particular, it has been estimated that the prevalence of type 2 diabetes (T2DM) among adolescents will quadruple by 2050 [1]. Specifically, pre-diabetes represents an emerging clinical priority in the setting of pediatric obesity [2] since it has increased at an alarming rate among obese youths [3]. Furthermore, it may be associated with an accelerated decline in the beta cell function and to the onset of overt diabetes. Diagnostic criteria for pre-diabetes have changed over time. In the last years, the American Diabetes Association (ADA) has proposed the assessment of glycosylated hemoglobin (HbA1c) in alternative to fasting or post-load glycemia for the screening of pre-diabetes both in children and adults [4]. Consequently, pre-diabetes may be now defined by three different conditions, i.e., impaired fasting glucose (IFG), impaired glucose tolerance (IGT), and elevated levels of HbA1c (5.7–6.4%) (IA1c) or a combination of them. These phenotypes are not distinct pathological entities, but rather represent different phases of a disease that is a continuum, where each group of patients may be in a different stage of progression. Each phenotype, which is expression of a distinct alteration of glucose metabolism, is individually associated to a cluster of adverse cardiovascular risk factors and conveys greater risk for the development of T2DM over time. These issues are well known in adulthood but are less explored in youths.
The prevalence of pre-diabetes in children and adolescents with OB is influenced by ethnicity, age or severity of weight excess. It may also vary according to the definition adopted. A change in the overall prevalence of pre-diabetes is expected to occur by including IA1c as diagnostic criterion. Therefore, updated studies are needed to characterize the impact of the new phenotypes on the prevalence of pre-diabetes with respect to previous criteria. For instance, the National Health and Nutrition Examination Surveys (2005–2006 through 2015–2016) has recently reported updated estimates of the prevalence of pre-diabetes based on IFG, IGT, or IA1c in adolescents with OB compared to normal weight (25.7% of 16.4%, respectively) [3]. In this multi-ethnic population, a wide heterogeneity in the overall prevalence of pre-diabetes was found by race/ethnicity. In fact, a higher prevalence in Black non-Hispanic or Hispanic was reported compared to the White non-Hispanic population [3]. This finding may explain the different prevalence of pre-diabetes in the US or European children or adolescents with overweight (OW) or OB [5,6,7,8,9,10,11]. Therefore, country-specific studies are needed, considering that HbA1c levels may vary according to the ethnic background, lifestyle or socioeconomic conditions.
To our knowledge, no study has assessed the prevalence of pre-diabetes according to the three categories of IFG, IGT or IA1c in Italian children with OW/OB. Furthermore, few studies analyzed the association between pre-diabetes phenotypes and cardiovascular risk factors in youths [12].
Therefore, the aim of this cross-sectional multicenter study was to evaluate the prevalence of IFG, IGT and IA1c in a large sample of Italian outpatient youths with OW/OB and to compare parameters of beta cell function, insulin sensitivity and cardio-metabolic risk among these different phenotypes.
Subjects and methods
Participants
This retrospective multicenter study was undertaken within the Childhood Obesity study group of the Italian Society for Pediatric Endocrinology and Diabetology (ISPED). Nine tertiary Italian centers for the diagnosis and care of pediatric obesity distributed throughout the country participated and provided anthropometric and biochemical data of 1562 children and adolescents aged 5–18 years consecutively observed in the period June 2016–June 2020. Thirteen youths who showed glycemic data within the category of T2DM were excluded. Lastly, data of 1549 young people (774 boys and 775 girls) with complete anthropometric and biochemical data were analyzed. This study was approved by the Ethics Committee of the AORN Santobono-Pausilipon (reference number 22877/2020) and conformed to the guidelines of the European Convention of Human Rights and Biomedicine for Research in Children as elsewhere described. The study was also in accordance with the 1975 Declaration of Helsinki, revised in 1983, and informed consent was obtained from the parents or tutors of all participants.
Measurement
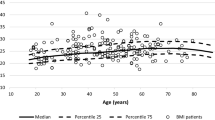
Height and weight were measured in each center by a single trained operator as previously described [13]. Body mass index (BMI) was transformed into standard deviation score (SDS), based upon the Italian BMI percentiles [14]. Prepubertal stage was defined by Tanner Stage I of breast development in girls and testicular volume in boys [15]. After 12 h of fasting, blood samples were drawn for glucose (G0) insulin (I0) and HbA1c measurements. Oral glucose tolerance test (OGTT) was performed in the whole sample using 1.75 g/kg of glucose up to a maximum of 75 g, and two-hour post-load glucose (G120) was analyzed [4]. Data of glucose (G30) and insulin (I30) at 30′ during OGTT were available in a subsample of 952 youths. Insulin resistance (IR) was calculated by homeostatic model assessment (HOMA-IR). Insulin sensitivity (IS) was calculated as 1/I0 [16].
Insulinogenic index (IGI) was calculated as Δ(I0–I30)/Δ(G0–G30), where insulin was expressed as µU/mL and glucose as mg/dL. Disposition index (DI) was calculated according to the following formula: IGI × 1/I0 [17]
Biochemical analyses were performed in the centralized laboratory of each center. HbA1c was assessed by high-performance liquid chromatography. All laboratories belong to the Italian National Health System and are certified according to International Standards IS 000 (www.iso000.it/), undergoing to semi-annual quality controls and inter-lab comparisons.
Definitions
Prediabetes was defined as any of the following phenotypes: impaired fasting glucose (IFG) (fasting glucose ≥ 100 < 126 mg/dL), and/or impaired glucose tolerance (IGT) (post-load glucose ≥ 140 < 200 mg/dL) and/or increased levels of glycosylated hemoglobin (IA1c) (HbA1c ≥ 5.7 < 6.5% or ≥ 39 < 48 mmol/mol), Overweight (OW) and obesity (OB) were defined on the basis of the Italian BMI standards (respectively the 75th and 95th percentiles).
IR was estimated by 97th percentile of HOMA-IR distribution by age and gender in normal weight Italian children [18]. Low IS or low DI were defined by the 25th percentile of respectively 1/I0 or DI in our sample.
Family history of T2DM was defined by the presence of T2DM in at least one among the first- or second-degree relatives.
Statistical analysis
Continuous data were expressed as mean ± standard deviation (SD), numbers and proportions as percentage (%) and 95% confidence interval (CI). Variables with skewed distribution (i.e., HOMA-IR, 1/I0, I0, I30, IGI, DI) were log-transformed for the analysis and expressed as median and interquartile range of non-transformed values. Mean values were compared using Student’s t test or ANCOVA, adjusted for centers, pairwise comparisons were estimated by Sidak post hoc analysis. Distribution of categories was compared by χ2 and, when needed, exact tests were performed using the Monte Carlo method and the Bonferroni correction. The concordance between the three phenotypes was tested by Cohen’s kappa (k) coefficient.
The odds ratio of family history of T2DM, IR, low IS, low DI was tested using logistic regression analysis using backward procedure and age, prepubertal stage and BMI and phenotypes of pre-diabetes as covariates. A P value < 0.05 was considered statistically significant. The statistical analysis was performed using the IBM SPSS Statistics, Version 20.0. Armonk, NY.
Results
The features of the whole sample and separately for boys and girls are reported in Table 1. Sex differences were found for G0, 1/I0 and systolic BP (higher in boys) and I0 and HOMA-IR (higher in girls). No differences were found for age, BMI, and BMI-SDS.
The percentages of isolated or any combined presence of two or more phenotypes are reported in Table 2. The most frequent phenotype was represented by IA1c, either isolated or combined with other phenotypes. The percentage of isolated IFG and IGT was quite similar, while IFG was slightly more frequent than IGT, when it was associated with any other phenotype. Prevalence of pre-diabetes and its phenotypes by gender and by age groups is shown in Fig. 1. Regarding gender distribution, a higher prevalence of IGT was observed in girls vs boys (P = 0.025). Regarding age distribution, a higher prevalence of IGT and pre-diabetes was observed in adolescents (age ≥ 10 years) vs children (age < 10 years). A similar trend (albeit not statistically significant) was observed for IFG (P = 0.059). On the contrary, no age-related difference was observed for IA1c.
The agreement between phenotypes was poor (k index 0.14 between IFG and IGT, 0.20 between IFG and IA1c, and 0.07 between IGT and IA1c).
The features of whole sample divided according to the absence of any glucose derangements, the isolated presence or any combined presence of IFG, IGT and IA1c are reported in Table 3. As expected, G0, G120, and HbA1c differed among groups by definition. Furthermore, groups differed significantly for age, family history of T2DM, and BMI, but not for BMI-SDS. The group with ≥ 2 phenotypes exhibited the oldest age, the highest BMI-SDS, I0 and HOMA-IR and the lowest insulin sensitivity (1/I0) compared to the other groups. On the contrary, the group without pre-diabetes showed a better cardio-metabolic profile, with lower levels of both lipids and BP.
In the subsample of 958 youths in whom the IGI was available, the isolated IGT phenotype was characterized by more prevalent relatives with T2DM, and lower values of IGI and DI (Table, Supplementary materials).
The proportions of youths with IR, low IS and low DI, across the different pre-diabetes phenotypes are reported in Fig. 2 of Supplementary materials.
The strength of the associations (expressed as Odds Ratios adjusted for centers, age, prepubertal status, and BMI) between phenotypes of pre-diabetes and metabolic abnormalities or markers of atherogenic dyslipidemia is shown in Table 4. Compared to youths without pre-diabetes (reference category), family history of T2DM was associated only with isolated IGT, while the abnormalities underlying beta cell function and insulin sensitivity were associated with either isolated IGT or any combined phenotype. On the contrary, only IR was associated with isolated IFG, while IR and low DI were associated with IA1c, but at a lesser extent than isolated IGT.
Discussion
The present study has demonstrated that more than a quarter of Italian children and adolescents with OW/OB had pre-diabetes and that IA1c was the most prevalent phenotype. Compared to the other phenotypes, isolated IGT was strongly associated with family history of T2DM and showed the worst metabolic profile in terms of insulin resistance, low insulin sensitivity, low DI and atherogenic lipid profile.
The assessment of A1c for the diagnosis of pre-diabetes is still supported by limited data in children, as underlined by the most recent ADA guidelines [4]. However, there are many advantages of using A1c, since it does not require fasting, has low intra-individual variability, and it is a good predictor of diabetes-related complications in adults [19]. Several studies have assessed the prevalence of IA1c in the pre-diabetes range and the potentiality of this biochemical marker to predict T2DM in youths with obesity compared to FPG and 2hPG, yielding contrasting results [20,21,22,23].
In our sample, the overall prevalence of IA1c was 16.3%, representing the most frequent phenotype and accounting for 50% of the isolated phenotypes. Compared to our study, a higher prevalence of IA1c (21% and 23.6% respectively) was reported in two clinical studies, the former conducted in a multi-ethnic cohort of 1156 US youths with obesity [20], the latter in a clinical sample of 4848 children and adolescents with OW and OB [23]. On the contrary, a lower prevalence of IA1c (12.2%) was reported in OW/OB youths from the NANHES 2005–2016 population study [3]; in this group, IFG accounted for 29.2% and IGT for 9.0%. Discrepancies among studies are difficult to explain, since the threshold used to define IA1c was the same (5.7–6.4%) and the age range was quite similar. Probably, different settings (population versus clinical samples) and the presence of multi-ethnic populations might account for the different results.
We observed 5.4% cases with isolated IFG, which is by far lower than 26% reported in the NANHES 2005–2016 [3]. This finding is not surprising since the prevalence of isolated IFG among obese young people is widely heterogeneous among studies, ranging between 0.4% in youths of European origin [24] and 35.8% in a Swedish cohort [10]. On the contrary, the prevalence of isolated IGT was only slightly lower (5% vs 8.1%) than that reported by the NANHES 2005–2016 [3]. Indeed, the prevalence of IGT is much more consistent across different studies, ranging from 3.2% in a Sardinian population [8] to 14.2% in the Swedish cohort [10]. Of note, our study showed that the prevalence of IGT was doubled compared to what reported more than 20 years ago by Invitti et al. in Italian children and adolescents with severe obesity [26], supporting that the prevalence of pre-diabetes is rising in Italy with the increasing prevalence of obesity.
Gender differences in the prevalence of the pre-diabetes phenotypes have been reported in adults [24, 25], while few data are available in the young population with OW/OB. In agreement with the studies performed in adults, we found that girls were more likely to have isolated IGT than boys and that no gender difference occurred with regard to IA1c. Other studies performed in children with OB reported similar findings for both IGT (in children but not in adolescents) [10]. Indeed, we did not confirm the higher male prevalence for IFG as reported in adults, but in this regard, equivocal results have been described in the pediatric literature [26,27,28].
Regarding the influence of age, very few studies have assessed the prevalence of pre-diabetes in children under 10 years of age [1, 28, 29]. This is not surprising, since the ADA recommended the screening of diabetes after the age of 10 years or in the presence of pubertal signs. We observed that pre-diabetes was already present in 22.8% children, although at a significantly lower extent than adolescents. This finding was true for IFG (P = 0.059) and especially for IGT (P = 0.003). Similar to our findings, Hagman et al. [29] showed an age-dependent increase of IFG risk in two nationwide cohorts (German and Swedish) of children and adolescents with OB.
Although pre-diabetes can be transient specifically at such a young age, our findings suggest the utility of pre-diabetes screening in children with OW/OB less than 10 years as an opportunity of increasing parental engagement in weight control [30].
Several studies have demonstrated a higher prevalence of family history for T2DM in youths with OB and pre-diabetes, without differentiating among phenotypes [6, 31]. We found that 52% of our sample had family history for T2DM. Indeed, this is one of the risk factors for diabetes included in the ADA criteria for screening. Interestingly, the IGT group had a significantly higher positivity of relatives with T2DM compared to the other phenotypes. Similarly, Poon et al. reported a family history of diabetes in 80% of youths with pre-diabetes (IFG and/or IGT) as compared to 53% of normoglycemic youths in a Chinese population with OW/OB [32]. With specific regard to IGT, Goran et al. reported that 28% of overweight Latino children with a positive family history of T2DM already have IGT [7]. The strong association between family history of T2DM and IGT suggests that genetic background has greater penetrance in youths with IGT than young people with the other phenotypes.
We observed a poor agreement between IFG, IGT and IA1c, as previously demonstrated in young people with OW/OB [33, 34]. This finding indicates that the three phenotypes may reflect distinct features of glucose metabolism and different stages of the pathophysiological mechanisms [35]. Indeed, IFG was associated only with IR, whereas IGT was exhibited IR, low IS, and DI. Similar characteristics were observed in individuals with ≥ 2 phenotypes.
Interestingly, the IA1c phenotype showed an intermediate risk profile compared to the other phenotypes. Hence, we can hypothesize that IA1c may detect a population at an earlier stage risk to develop T2DM compared to IGT. Since the reversal from pre-diabetes to normoglycemia is common in adolescents, especially in those with IFG, A1c is likely to be biomarker more reliable then IFG over time. Indeed, a lower regression to normoglycemia was reported in adults with IA1c compared to the other phenotypes [36], supporting the hypothesis that this phenomenon may be dependent on a greater stability of IA1c. If this evolution is also confirmed by prospective studies in childhood, the utility of HbA1c monitoring could be crucial in adolescents at high risk of developing diabetes. Prediabetes in adolescents has been associated with a worse cardiovascular profile [3, 37]. Interestingly, by analyzing the single phenotypes, we found a significant association between isolated IGT or IA1c and biomarkers of atherogenic risk. The present study extends our previous findings on the worse cardiovascular profile in obese youths with IGT [11] to include also the IA1c phenotype, highlighting that both phenotypes represent categories metabolically distinct from IFG.
Our study presents some limitations. The cross-sectional design does not allow inferences on the progression of each phenotype of pre-diabetes, in addition the prevalence of pre-diabetes is limited to categories of youths with OW/OB and cannot be extended to the general population. Furthermore, HbA1c and insulin measurements were not centralized in a single laboratory, thus variability between the different centers could not be totally excluded. In addition, our data were obtained in a sample of Caucasian youths, therefore they cannot be easily compared to other studies based on multi-ethnic populations. However, this feature may represent also a strength of our study, since the prevalence of pre-diabetes in Caucasian populations is by far less explored. Furthermore, the comprehensive analysis of metabolic characteristics of each phenotype and their association with the atherogenic major cardio-metabolic risk factors may represent another strength of our study.
Conclusion
Our study has demonstrated that in an outpatient population of youths with OW/OB the prevalence of pre-diabetes is high and that IA1c was the most prevalent phenotype. IA1c showed intermediate characteristics in terms of both metabolic impairment and atherogenic risk profile as compared to IFG and IGT. More studies are needed to assess whether A1c may help improving the prediction of diabetes.
Data availability
De-identified individual participant data will not be made available.
Abbreviations
- 1/I 0 :
-
Reciprocal of fasting insulin
- ADA:
-
American Diabetes Association
- BMI:
-
Body mass index
- CMR:
-
Cardiometabolic risk
- DBP:
-
Diastolic blood pressure
- G 0 :
-
Fasting glucose
- G 120L :
-
Glucose at 120′ during OGTT
- HbA1c:
-
Glycosylated hemoglobin
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- I 0 :
-
Fasting insulin
- IA1c:
-
Increased HbA1c
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- ISPED:
-
Italian Society of Pediatric Endocrinology and Diabetology
- OB:
-
Obesity
- OGTT:
-
Oral glucose tolerance test
- OR:
-
Odds ratio
- OW:
-
Overweight
- SBP:
-
Systolic blood pressure
- TC/HDL ratio:
-
Total cholesterol-to-HDL ratio
References
Imperatore G, Boyle JP, Thompson TJ et al (2012) Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 35:2515–2520. https://doi.org/10.2337/dc12-0669
Dingle E, Brar PC (2017) Prediabetes in obese adolescents: an emerging clinical priority. Clin Pediatr 56(2):115–116. https://doi.org/10.1177/0009922816681138
Andes LJ, Cheng YJ, Rolka DB, Gregg EW, Imperatore G (2020) Prevalence of prediabetes among adolescents and young adults in the United States, 2005–2016. JAMA Pediatr 174:e194498. https://doi.org/10.1001/jamapediatrics.2019.4498
American Diabetes Association (2022) Standards of medical care in diabetes 2022. Diabetes Care 45(Suppl 1):S1–S2. https://doi.org/10.2337/dc22-Sint
Tresaco B, Bueno G, Moreno LA et al (2003) Insulin resistance and impaired glucose tolerance in obese children and adolescents. J Physiol Biochem 59:217–24. https://doi.org/10.1007/BF03179918
Wabitsch M, Hauner H, Hertrampf M (2004) Type II diabetes mellitus and impaired glucose regulation in Caucasian children living in Germany. Int J Obes Relat Metab Disord 28:307–313. https://doi.org/10.1038/sj.ijo.0802555
Goran MI, Bergman RN, Avila Q et al (2004) Impaired glucose tolerance and reduced beta-cell function in overweight Latino children with a positive family history for type 2 diabetes. J Clin Endocrinol Metab 89:207–212. https://doi.org/10.1210/jc.2003-031402
Cambuli VM, Incani M, Pilia S et al (2009) Oral glucose tolerance test in Italian overweight/obese children and adolescents results in a very high prevalence of impaired fasting glycaemia, but not of diabetes. Diabetes Metab Res Rev 25:528–534. https://doi.org/10.1002/dmrr.980
Körner A, Wiegand S, Hungele A et al (2013) Longitudinal multicenter analysis on the course of glucose metabolism in obese children. Int J Obes (Lond) 37:931–936. https://doi.org/10.1038/ijo.2012.163
Ek AE, Rőssner SM, Hagman E et al (2015) High prevalence of prediabetes in a Swedish cohort of severely obese children. Pediatr Diabetes 16:117–128. https://doi.org/10.1111/pedi.12136
Di Bonito P, Pacifico L, Chiesa C, Valerio G et al (2017) Impaired fasting glucose and impaired glucose tolerance in children and adolescents with overweight/obesity. J Endocrinol Invest 40:409–416. https://doi.org/10.1007/s40618-016-0576-8
Liu C, Wu S, Pan X (2021) Clustering of cardio-metabolic risk factors and pre-diabetes among U.S. adolescents. Sci Rep 11:5015. https://doi.org/10.1038/s41598-021-84128-6
Di Bonito P, Valerio G, Grugni G et al (2015) Comparison of non-HDL-cholesterol versus triglycerides-to-HDL-cholesterol ratio in relation to cardio-metabolic risk factors and preclinical organ damage in overweight/obese children: the CARITALY study. Nutr Metab Cardiovasc Dis 25:489–494. https://doi.org/10.1016/j.numecd.2015.01.012
Cacciari E, Milani S, Balsamo A et al (2006) Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J Endocrinol Invest 29:581–93. https://doi.org/10.1007/BF03344156
Tanner JM, Whitehouse RH (1976) Clinical longitudinal standards from birth to maturity for height, weight, velocity and stages of puberty. Arch Dis Child 51:170–9
George L, Bacha F, Lee S, Tfayli H, Andreatta E, Arslanian S (2011) Surrogate estimates of insulin sensitivity in obese youth along the spectrum of glucose tolerance from normal to prediabetes to diabetes. J Clin Endocrinol Metab 96:2136–2145. https://doi.org/10.1210/jc.2010-2813
Sjaarda LG, Bacha F, Lee S et al (2012) Oral disposition index in obese youth from normal to prediabetes to diabetes: relationship to clamp disposition index. J Pediatr 161:51–57. https://doi.org/10.1016/j.jpeds.2011.12.050
Shashaj B, Luciano R, Contoli B et al (2016) Reference ranges of HOMA-IR in normal-weight and obese young Caucasians. Acta Diabetol 53:251–260. https://doi.org/10.1007/s00592-015-0782-4
Haemer MA, Grow HM, Fernandez C et al (2014) Addressing prediabetes in childhood obesity treatment programs: support from research and current practice. Child Obes 10:292–303. https://doi.org/10.1089/chi.2013.0158
Nowicka P, Santoro N, Liu H et al (2011) Utility of hemoglobin A(1c) for diagnosing prediabetes and diabetes in obese children and adolescents. Diabetes Care 34:1306–1311. https://doi.org/10.2337/dc10-1984
Sjaarda LA, Michaliszyn SF, Lee S et al (2012) HbA(1c) diagnostic categories and β-cell function relative to insulin sensitivity in overweight/obese adolescents. Diabetes Care 35:2559–2563. https://doi.org/10.2337/dc12-0747
Nam HK, Cho WK, Kim JH, Rhie YJ et al (2018) HbA1c cutoff for prediabetes and diabetes based on oral glucose tolerance test in obese children and adolescents. J Korean Med Sci 33:e93. https://doi.org/10.3346/jkms.2018.33.e93
Ehehalt S, Wiegand S, Körner A, Schweizer R et al (2017) Diabetes screening in overweight and obese children and adolescents: choosing the right test. Eur J Pediatr 176:89–97. https://doi.org/10.1007/s00431-016-2807-6
Vatcheva KP, Fisher-Hoch SP, Reininger BM et al (2020) Sex and age differences in prevalence and risk factors for prediabetes in Mexican-Americans. Diabetes Res Clin Pract 159:107950. https://doi.org/10.1016/j.diabres.2019.107950
Mauvais-Jarvis F (2018) Gender differences in glucose homeostasis and diabetes. Physiol Behav 187:20–23. https://doi.org/10.1016/j.physbeh.2017.08.016
Invitti C, Guzzaloni G, Gilardini L et al (2003) Prevalence and concomitants of glucose intolerance in european obese children and adolescents. Diabetes Care 26:118–124. https://doi.org/10.2337/diacare.26.1.118
Sinha R, Fisch G, Teague B, Tamborlane WV et al (2002) Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med 14(346):802–810. https://doi.org/10.1056/NEJMoa012578
Tester J, Sharma S, Jasik CB et al (2013) Gender differences in prediabetes and insulin resistance among 1356 obese children in Northern California. Diabetes Metab Syndr 7:161–165. https://doi.org/10.1016/j.dsx.202
Hagman E, Reinehr T, Kowalski J et al (2014) Impaired fasting glucose prevalence in two nationwide cohorts of obese children and adolescents. Int J Obes (Lond) 38:40–45. https://doi.org/10.1038/ijo.2013.124
Vajravelu ME, Lee JM, Shah R et al (2020) Association between prediabetes diagnosis and body mass index trajectory of overweight and obese adolescents. Pediatr Diabetes 21:743–746. https://doi.org/10.1111/pedi.13028
Saleh M, Kim JY, March C, Gebara N, Arslanian S (2022) Youth prediabetes and type 2 diabetes: risk factors and prevalence of dysglycaemia. Pediatr Obes 17:e12841. https://doi.org/10.1111/ijpo.12841
Poon SW, Wong WH, Tsang AM et al (2021) Who should return for an oral glucose tolerance test? A proposed clinical pathway based on retrospective analysis of 332 children. J Pediatr Endocrinol Metab 19(34):877–884. https://doi.org/10.1515/jpem-2020-0689
Gómez-Díaz R, Aguilar-Salinas CA, Morán-Villota S et al (2004) Lack of agreement between the revised criteria of impaired fasting glucose and impaired glucose tolerance in children with excess body weight. Diabetes Care 27:2229–2233. https://doi.org/10.2337/diacare.27.9.2229
Ehehalt S, Wiegand S, Körner A et al (2017) Low association between fasting and OGTT stimulated glucose levels with HbA1c in overweight children and adolescents. Pediatr Diabetes 18:734–741. https://doi.org/10.1111/pedi.12461
Cali’ AM, Bonadonna RC, Trombetta M, Weiss R, Caprio S (2008) Metabolic abnormalities underlying the different prediabetic phenotypes in obese adolescents. J Clin Endocrinol Metab 93:1767–1773. https://doi.org/10.1210/jc.2007-1722
Tura A, Grespan E, Göbl CS, Koivula RW et al (2021) Profiles of glucose metabolism in different prediabetes phenotypes, classified by fasting glycemia, 2-hour OGTT, glycated hemoglobin, and 1-hour OGTT: an IMI DIRECT Study. Diabetes 70:2092–2106. https://doi.org/10.2337/db21-0227
Casagrande SS, Menke A, Linder B et al (2018) Cardiovascular risk factors in adolescents with prediabetes. Diabet Med. https://doi.org/10.1111/dme.13661.10.1111/dme.13661
Funding
Open access funding provided by Università Parthenope di Napoli within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
PDB and GV conceived and designed the study, analyzed data and interpreted, drafted and revised the manuscript for important intellectual content. MRL, DC, MGW, ADS, EMDG, AM, CM, MFF, EM, VC, FF, GM acquired data and revised the draft for important intellectual content. All the authors approved the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this manuscript to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All participating centers obtained informed consent from parents of subjects included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to add missing OASIS funding note.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Di Bonito, P., Licenziati, M.R., Corica, D. et al. Phenotypes of prediabetes and metabolic risk in Caucasian youths with overweight or obesity. J Endocrinol Invest 45, 1719–1727 (2022). https://doi.org/10.1007/s40618-022-01809-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01809-3