Abstract
Background
Inorganic phosphate (Pi) is an essential mineral for human. Hypophosphatemia and hyperphosphatemia cause rickets/osteomalacia and ectopic calcification, respectively, indicating that serum Pi level needs to be regulated. Fibroblast growth factor (FGF) 23 is a principal hormone to regulate serum Pi level. FGF23 is produced by the bone, especially by the osteoblasts and osteocytes, and works by binding to FGF receptor (FGFR) 1c and α-Klotho complex in the kidney. FGF23 reduces serum Pi level by inhibiting both renal phosphate reabsorption and intestinal phosphate absorption via reduction of serum 1,25-dihydroxyvitamin D level. It has been unclear how the bone senses changes of serum Pi level and how the bone regulates the production of FGF23.
Recent findings
Our recent results indicate that the post-translational modification of FGF23 protein through a gene product of GALNT3 is the main regulatory mechanism of enhanced FGF23 production by high dietary Pi. Furthermore, high extracellular Pi directly activates FGFR1 and its downstream intracellular signaling pathway regulates the expression level of GALNT3.
Conclusions
We propose that FGFR1 works as a Pi-sensing receptor in the regulation of FGF23 production and serum Pi level. There is a negative feedback system, which is a basic mechanism of endocrine regulation, in the regulation of serum Pi involving FGFR1, and FGF23. These findings may lead to the development of new therapeutic methods to treat diseases caused by abnormal Pi level.


Similar content being viewed by others
References
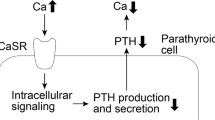
Brown EM, Gamba G, Riccardi D, Lombardi M, Butters R, Kifor O, Sun A, Hediger MA, Lytton J, Hebert SC (1993) Cloning and characterization of an extracellular Ca(2+)-sensing receptor from bovine parathyroid. Nature 366(6455):575–580. https://doi.org/10.1038/366575a0
Fukumoto S, Martin TJ (2009) Bone as an endocrine organ. Trends Endocrinol Metab 20(5):230–236. https://doi.org/10.1016/j.tem.2009.02.001
Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, Yu X, Rauch F, Davis SI, Zhang S, Rios H, Drezner MK, Quarles LD, Bonewald LF, White KE (2006) Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet 38(11):1310–1315. https://doi.org/10.1038/ng1905
Liu S, Zhou J, Tang W, Jiang X, Rowe DW, Quarles LD (2006) Pathogenic role of Fgf23 in Hyp mice. Am J Physiol Endocrinol Metab 291(1):E38–49. https://doi.org/10.1152/ajpendo.00008.2006
ADHR Consortium (2000) Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat Genet 26(3):345–348. https://doi.org/10.1038/81664
Yamashita T, Yoshioka M, Itoh N (2000) Identification of a novel fibroblast growth factor, FGF-23, preferentially expressed in the ventrolateral thalamic nucleus of the brain. Biochem Biophys Res Commun 277(2):494–498. https://doi.org/10.1006/bbrc.2000.3696
Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T (2001) Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Natl Acad Sci USA 98(11):6500–6505. https://doi.org/10.1073/pnas.101545198
Kinoshita Y, Fukumoto S (2018) X-Linked hypophosphatemia and FGF23-related hypophosphatemic diseases: prospect for new treatment. Endocr Rev 39(3):274–291. https://doi.org/10.1210/er.2017-00220
Itoh N, Ornitz DM (2004) Evolution of the Fgf and Fgfr gene families. Trends Genet 20(11):563–569. https://doi.org/10.1016/j.tig.2004.08.007
Ornitz DM, Itoh N (2015) The fibroblast growth factor signaling pathway. Wiley interdisciplinary Reviews Developmental Biology 4(3):215–266. https://doi.org/10.1002/wdev.176
Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, Fujita T, Nakahara K, Fukumoto S, Yamashita T (2004) FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res 19(3):429–435. https://doi.org/10.1359/jbmr.0301264
Urakawa I, Yamazaki Y, Shimada T, Iijima K, Hasegawa H, Okawa K, Fujita T, Fukumoto S, Yamashita T (2006) Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature 444(7120):770–774. https://doi.org/10.1038/nature05315
Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblatt KP, Baum MG, Schiavi S, Hu MC, Moe OW, Kuro-o M (2006) Regulation of fibroblast growth factor-23 signaling by klotho. The J Biol Chem 281(10):6120–6123. https://doi.org/10.1074/jbc.C500457200
Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, Ohyama Y, Kurabayashi M, Kaname T, Kume E, Iwasaki H, Iida A, Shiraki-Iida T, Nishikawa S, Nagai R, Nabeshima YI (1997) Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature 390(6655):45–51. https://doi.org/10.1038/36285
Chen G, Liu Y, Goetz R, Fu L, Jayaraman S, Hu MC, Moe OW, Liang G, Li X, Mohammadi M (2018) alpha-Klotho is a non-enzymatic molecular scaffold for FGF23 hormone signalling. Nature 553(7689):461–466. https://doi.org/10.1038/nature25451
Shimada T, Muto T, Urakawa I, Yoneya T, Yamazaki Y, Okawa K, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T (2002) Mutant FGF-23 responsible for autosomal dominant hypophosphatemic rickets is resistant to proteolytic cleavage and causes hypophosphatemia in vivo. Endocrinology 143(8):3179–3182. https://doi.org/10.1210/endo.143.8.8795
Frishberg Y, Ito N, Rinat C, Yamazaki Y, Feinstein S, Urakawa I, Navon-Elkan P, Becker-Cohen R, Yamashita T, Araya K, Igarashi T, Fujita T, Fukumoto S (2007) Hyperostosis-hyperphosphatemia syndrome: a congenital disorder of O-glycosylation associated with augmented processing of fibroblast growth factor 23. J Bone Miner Res 22(2):235–242. https://doi.org/10.1359/jbmr.061105
Hang HC, Yu C, Ten Hagen KG, Tian E, Winans KA, Tabak LA, Bertozzi CR (2004) Small molecule inhibitors of mucin-type O-linked glycosylation from a uridine-based library. Chem Biol 11(3):337–345. https://doi.org/10.1016/j.chembiol.2004.02.023
Bennett EP, Mandel U, Clausen H, Gerken TA, Fritz TA, Tabak LA (2012) Control of mucin-type O-glycosylation: a classification of the polypeptide GalNAc-transferase gene family. Glycobiology 22(6):736–756. https://doi.org/10.1093/glycob/cwr182
Topaz O, Shurman DL, Bergman R, Indelman M, Ratajczak P, Mizrachi M, Khamaysi Z, Behar D, Petronius D, Friedman V, Zelikovic I, Raimer S, Metzker A, Richard G, Sprecher E (2004) Mutations in GALNT3, encoding a protein involved in O-linked glycosylation, cause familial tumoral calcinosis. Nat Genet 36(6):579–581. https://doi.org/10.1038/ng1358
Perwad F, Azam N, Zhang MY, Yamashita T, Tenenhouse HS, Portale AA (2005) Dietary and serum phosphorus regulate fibroblast growth factor 23 expression and 1,25-dihydroxyvitamin D metabolism in mice. Endocrinology 146(12):5358–5364. https://doi.org/10.1210/en.2005-0777
Ferrari SL, Bonjour JP, Rizzoli R (2005) Fibroblast growth factor-23 relationship to dietary phosphate and renal phosphate handling in healthy young men. J Clin Endocrinol Metab 90(3):1519–1524. https://doi.org/10.1210/jc.2004-1039
Takashi Y, Kosako H, Sawatsubashi S, Kinoshita Y, Ito N, Tsoumpra MK, Nangaku M, Abe M, Matsuhisa M, Kato S, Matsumoto T, Fukumoto S (2019) Activation of unliganded FGF receptor by extracellular phosphate potentiates proteolytic protection of FGF23 by its O-glycosylation. Proc Natl Acad Sci USA 116(23):11418–11427. https://doi.org/10.1073/pnas.1815166116
Tagliabracci VS, Engel JL, Wiley SE, Xiao J, Gonzalez DJ, Nidumanda Appaiah H, Koller A, Nizet V, White KE, Dixon JE (2014) Dynamic regulation of FGF23 by Fam20C phosphorylation, GalNAc-T3 glycosylation, and furin proteolysis. Proc Natl Acad Sci USA 111(15):5520–5525. https://doi.org/10.1073/pnas.1402218111
Saito H, Maeda A, Ohtomo S, Hirata M, Kusano K, Kato S, Ogata E, Segawa H, Miyamoto K, Fukushima N (2005) Circulating FGF-23 is regulated by 1alpha,25-dihydroxyvitamin D3 and phosphorus in vivo. J Biol Chem 280(4):2543–2549. https://doi.org/10.1074/jbc.M408903200
Jono S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, Morii H, Giachelli CM (2000) Phosphate regulation of vascular smooth muscle cell calcification. Circ Res 87(7):E10–17
Ito N, Wijenayaka AR, Prideaux M, Kogawa M, Ormsby RT, Evdokiou A, Bonewald LF, Findlay DM, Atkins GJ (2015) Regulation of FGF23 expression in IDG-SW3 osteocytes and human bone by pro-inflammatory stimuli. Mol Cell Endocrinol 399:208–218. https://doi.org/10.1016/j.mce.2014.10.007
Imel EA, Peacock M, Gray AK, Padgett LR, Hui SL, Econs MJ (2011) Iron modifies plasma FGF23 differently in autosomal dominant hypophosphatemic rickets and healthy humans. J Clin Endocrinol Metab 96(11):3541–3549. https://doi.org/10.1210/jc.2011-1239
Farrow EG, Yu X, Summers LJ, Davis SI, Fleet JC, Allen MR, Robling AG, Stayrook KR, Jideonwo V, Magers MJ, Garringer HJ, Vidal R, Chan RJ, Goodwin CB, Hui SL, Peacock M, White KE (2011) Iron deficiency drives an autosomal dominant hypophosphatemic rickets (ADHR) phenotype in fibroblast growth factor-23 (Fgf23) knock-in mice. Proc Natl Acad Sci USA 108(46):E1146–1155. https://doi.org/10.1073/pnas.1110905108
Takashi Y, Fukumoto S (2018) FGF23 beyond phosphotropic hormone. Trends Endocrinol Metab 29(11):755–767. https://doi.org/10.1016/j.tem.2018.08.006
Michigami T, Kawai M, Yamazaki M, Ozono K (2018) Phosphate as a signaling molecule and its sensing mechanism. Physiol Rev 98(4):2317–2348. https://doi.org/10.1152/physrev.00022.2017
Beck GR Jr, Zerler B, Moran E (2000) Phosphate is a specific signal for induction of osteopontin gene expression. Proc Natl Acad Sci USA 97(15):8352–8357. https://doi.org/10.1073/pnas.140021997
Beck GR Jr, Knecht N (2003) Osteopontin regulation by inorganic phosphate is ERK1/2-, protein kinase C-, and proteasome-dependent. J Biol Chem 278(43):41921–41929. https://doi.org/10.1074/jbc.M304470200
Nishino J, Yamazaki M, Kawai M, Tachikawa K, Yamamoto K, Miyagawa K, Kogo M, Ozono K, Michigami T (2017) Extracellular phosphate induces the expression of dentin matrix protein 1 through the FGF receptor in osteoblasts. J Cell Biochem 118(5):1151–1163. https://doi.org/10.1002/jcb.25742
Kimata M, Michigami T, Tachikawa K, Okada T, Koshimizu T, Yamazaki M, Kogo M, Ozono K (2010) Signaling of extracellular inorganic phosphate up-regulates cyclin D1 expression in proliferating chondrocytes via the Na+/Pi cotransporter Pit-1 and Raf/MEK/ERK pathway. Bone 47(5):938–947. https://doi.org/10.1016/j.bone.2010.08.006
Yamazaki M, Ozono K, Okada T, Tachikawa K, Kondou H, Ohata Y, Michigami T (2010) Both FGF23 and extracellular phosphate activate Raf/MEK/ERK pathway via FGF receptors in HEK293 cells. J Cell Biochem 111(5):1210–1221. https://doi.org/10.1002/jcb.22842
Virkki LV, Biber J, Murer H, Forster IC (2007) Phosphate transporters: a tale of two solute carrier families. Am J Physiol Renal Physiol 293(3):F643–654. https://doi.org/10.1152/ajprenal.00228.2007
Bon N, Frangi G, Sourice S, Guicheux J, Beck-Cormier S, Beck L (2018) Phosphate-dependent FGF23 secretion is modulated by PiT2/Slc20a2. Mol Metab 11:197–204. https://doi.org/10.1016/j.molmet.2018.02.007
Bon N, Couasnay G, Bourgine A, Sourice S, Beck-Cormier S, Guicheux J, Beck L (2018) Phosphate (Pi)-regulated heterodimerization of the high-affinity sodium-dependent Pi transporters PiT1/Slc20a1 and PiT2/Slc20a2 underlies extracellular Pi sensing independently of Pi uptake. J Biol Chem 293(6):2102–2114. https://doi.org/10.1074/jbc.M117.807339
McKay MM, Morrison DK (2007) Integrating signals from RTKs to ERK/MAPK. Oncogene 26(22):3113–3121. https://doi.org/10.1038/sj.onc.1210394
Furdui CM, Lew ED, Schlessinger J, Anderson KS (2006) Autophosphorylation of FGFR1 kinase is mediated by a sequential and precisely ordered reaction. Mol Cell 21(5):711–717. https://doi.org/10.1016/j.molcel.2006.01.022
Lew ED, Furdui CM, Anderson KS, Schlessinger J (2009) The precise sequence of FGF receptor autophosphorylation is kinetically driven and is disrupted by oncogenic mutations. Sci Signal. https://doi.org/10.1126/scisignal.2000021
White KE, Cabral JM, Davis SI, Fishburn T, Evans WE, Ichikawa S, Fields J, Yu X, Shaw NJ, McLellan NJ, McKeown C, Fitzpatrick D, Yu K, Ornitz DM, Econs MJ (2005) Mutations that cause osteoglophonic dysplasia define novel roles for FGFR1 in bone elongation. Am J Hum Genet 76(2):361–367. https://doi.org/10.1086/427956
Goetz R, Mohammadi M (2013) Exploring mechanisms of FGF signalling through the lens of structural biology. Nat Rev Mol Cell Biol 14(3):166–180. https://doi.org/10.1038/nrm3528
Guagnano V, Furet P, Spanka C, Bordas V, Le Douget M, Stamm C, Brueggen J, Jensen MR, Schnell C, Schmid H, Wartmann M, Berghausen J, Drueckes P, Zimmerlin A, Bussiere D, Murray J, Graus Porta D (2011) Discovery of 3-(2,6-dichloro-3,5-dimethoxy-phenyl)-1-{6-[4-(4-ethyl-piperazin-1-yl)-phenylamin o]-pyrimidin-4-yl}-1-methyl-urea (NVP-BGJ398), a potent and selective inhibitor of the fibroblast growth factor receptor family of receptor tyrosine kinase. J Med Chem 54(20):7066–7083. https://doi.org/10.1021/jm2006222
Acknowledgements
This work was supported in part by Grant-in-Aid for Young Scientists from Japan Society for the Promotion of Science (18K15980) (to Y.T.) and by Grant-in-Aid for Scientific Research from Japan Society for the Promotion of Science (19H03676) (to S.F.).
Author information
Authors and Affiliations
Contributions
Y.T. wrote the manuscript and S.F. supervised the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any study with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takashi, Y., Fukumoto, S. Phosphate-sensing and regulatory mechanism of FGF23 production. J Endocrinol Invest 43, 877–883 (2020). https://doi.org/10.1007/s40618-020-01205-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01205-9