Abstract
The Centers for Disease Control and Prevention has identified African-Americans as having increased risk of COVID-19-associated mortality. Access to healthcare and related social determinants of health are at the core of this disparity. To explore the geographical links between race and COVID-19 mortality, we created descriptive maps of COVID-19 mortality rates in relation to the percentage of populations self-identifying as African-American across the USA, by state, and Pennsylvania (PA), by county. In addition, we used bivariate and logistic regression analyses to quantify the statistical relationship between these variables, and control for area-level demographic, healthcare access, and comorbidity risk factors. We found that COVID-19 mortality rates were generally higher in areas that had higher African-American populations, particularly in the northeast USA and eastern PA. These relationships were quantified through Pearson correlations showing significant positive associations at the state and county level. At the US state-level, percent African-American population was the only significant correlate of COVID-19 mortality rate. In PA at the county-level, higher percent African-American population was associated with higher COVID-19 mortality rate even after controlling for area-level confounders. More resources should be allocated to address high COVID-19 mortality rates among African-American populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
By June 1, 2020, US cases of the novel coronavirus (COVID-19) had surpassed 1.7 million, including more than 104,000 cumulative deaths [1]. State and local officials have actively combatted the disease with prevention tactics, including stay-at-home orders, business restrictions, face mask recommendations, and contact-tracing procedures, that have surely reduced the spread of COVID-19. Nevertheless, COVID-19 has continued to spread in many areas of the USA.
Data has revealed that African-Americans and other racial and ethnic minorities are suffering the greatest burden of COVID-19 outcomes. For instance, African-American people in Wisconsin have comprised 20.5% of all COVID-19 deaths while only making up 6.3% of the total population, according to a study from the Kaiser Family Foundation that used a Racial Disproportionality Index (RDI) [2, 3]. The study findings indicated that African-American people in Wisconsin died at 3.3 times the frequency expected (as of August 17, 2020), given their total representation in the state. Meanwhile, the COVID Tracking Project has reported the national COVID-19-related mortality rate for African-Americans was 2.4 times higher than that of Caucasian Americans [3]. Similarly, a report from the Commonwealth Fund detailed racial disparities across the nation based on county-level data, showing that counties with higher African-American populations experienced greater case, mortality, and progression rates of the disease than counties with lower African-American populations [4].
The specific causes of these disproportionate COVID-19 mortality rates among African-American people are not clear, however they are likely related to persistent and historical disparities in access to care, quality treatment, and social determinants of health [5]. Recent literature has hypothesized several factors that may account for racial differences in COVID-19 mortality, including (1) disparities in environmental factors, such as increased air pollution in areas with high African-American populations, which could exacerbate lung complications [6]; (2) increased rates of comorbidities that negatively affect COVID-19 outcomes [1]; (3) differences in employment patterns and related exposure [7]; (4) disparities in access to care, including lack of insurance and geographic maldistribution of healthcare services [7, 8]; and (5) structural racism in the healthcare system resulting in biased, limited care [9].
The COVID-19 pandemic has exposed environmental health factors that contribute to increased mortality among African-American populations. Brandt et al. (2020) reported that increased air pollution impacts COVID-19 mortality both directly, by decreasing lung capacity during COVID-19 infection, and indirectly, by increasing incidence of air pollution-related diseases that increase COVID-19 mortality [6]. Due to structural racism in the USA, air pollution has historically been higher in African-American communities [6]. Recent literature has suggested that prolonged exposure to air pollution increases the likelihood of associated diseases, increasing COVID-19 severity and potentially accounting for some of the disparity in African-American COVID mortality rates [6].
Moreover, African-Americans are more likely to have health conditions that increase COVID-19 disease severity, such as obesity and asthma [1]. According to the CDC [10], nonHispanic African-American populations have high rates of obesity and are more likely to experience conditions that contribute to obesity, including unemployment, food insecurity, access to less nutritious foods, and advertising for these poor-quality foods. Similarly, the risk of mortality due to asthma is three times higher among African-Americans than Caucasian Americans [11]. This high rate of asthma has been linked to segregation policies like redlining, resulting in a disproportionate number of African-American people living in older houses or communities with high lead exposure [12], which is believed to increase asthma severity and worsen COVID-19 symptoms [13].
Additionally, various occupational disparities also increase the probability that minorities will be exposed to COVID-19. For example, African-Americans and Hispanics are two times more likely to work in animal slaughtering and processing industries where COVID-19 outbreaks have taken place [14]. In addition, compared to Caucasian populations, African-Americans are 4% more likely to have occupations that require working in close proximity to others [14], thus increasing their risk of infection. Higher employment rates, especially in close proximity “essential-worker” positions like healthcare, transportation, and other service industry jobs, correspond with increased COVID-19 infection rates, and these jobs are disproportionately held by African-Americans [7].
Disparities in both access to and delivery of quality healthcare for African-Americans compound these factors. Examples of disparities related to access to care and treatment include lower insurance levels among African-Americans, Hispanics, and a number of Asian groups compared to Caucasians [15]. Lower county-level insurance coverage rates have been associated with both COVID infection rates and African-American population proportion, and researchers have hypothesized that the lack of insurance coverage for African-Americans partly accounts for the higher COVID mortality among this demographic group [7]. A recent study in Georgia found that counties with the highest COVID mortality rates had both the highest African-American populations and the lowest proportions of intensive care unit beds and primary care providers [8].
Additionally, structural racism and bias in the medical field have emerged as a further major concern potentially impacting African-American mortality. Researchers have pointed to both structurally inherent bias leading to poorer care and barriers for access to care leading to greater likelihood of delayed care and complications for African-Americans [9]. For example, African-American populations are less likely to receive appropriate treatment for myocardial infarctions, according to one study [16].
Therefore, we wanted to learn more about the relationship between COVID-19 and race. Only 26 US states were reporting COVID-19 mortality rates by race as of April 17, 2020 [17]. Among these states was Pennsylvania (PA), which, as of August 31, 2020, had around 7673 total COVID-19 deaths [18]. According to 2018 data, PA is about 80.1% White, 11.2% African-American, 3.5% Asian, and about 5.1% reporting as other races [19]. However, the race distribution is not equal throughout the state; Philadelphia county is 42.3% African-American while the remaining counties are 21.4% African-American or lower [20]. This difference in demographic diversity is what led us to study PA in particular. However, while PA has reported deaths by race overall, it has not reported them on the county level [18]. To analyze relationships between mortality rates and risk factors in PA and throughout the USA, we visualized and compared the geographic distribution of COVID-19 death rates and overall African-American populations.
The purpose of our ecological study was to explore correlations between COVID-19 mortality and the distribution of the African-American population by US states and within the state of PA. Additionally, we conducted statistical modeling to learn whether these correlations persisted after controlling for other potential confounders, including demographics, healthcare access, behavioral risk factors, and chronic diseases.
Methods
A base map of the contiguous USA was downloaded from the US Census TIGER/LINE databank [21]. COVID-19 death rates for US states and PA counties were downloaded from PolicyMap. The source data for COVID-19 rates was from The New York Times, based on reports from state and local health agencies on May 27, 2020 [22].
The source of the estimated percentages of African-American populations was the US Census American Communities Survey (2014–2018) and was downloaded via PolicyMap. Potential confounders explored included the following: median household income, hospital beds per population, primary care providers per population, self-reported primary care access, obesity rate, smoking rate, high blood pressure rate (HBP), chronic obstructive pulmonary disease (COPD)/emphysema/chronic bronchitis rate, and diabetes rate. Statistics on primary care provider rates and hospital bed rates were derived from the Human Resources and Services Administration (HRSA) via PolicyMap (2016). Self-reported percentages of having a personal provider, smoking cigarettes regularly (adults), having COPD, emphysema, or chronic bronchitis, having diabetes, having HBP, and being obese (BMI ≥30) were sourced from the CDC Behavioral Risk Factor Surveillance System (BRFSS) via PolicyMap (2017).
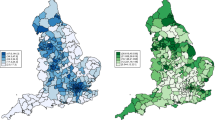
This information was mapped using ESRI ArcGIS version 10.3.1. We imported data from PolicyMap into Microsoft Excel, edited to ensure that geographic linkage variables corresponded between programs, and joined tabular Excel data to basemaps in ArcGIS. We created choropleth maps of COVID-19 mortality rates across the USA (state-level) and in PA (county-level), with category cutoff values created using natural quantile breaks. We added estimated percentages of African-American populations to each map as graduated point data, with larger points representing larger percentage of African-Americans within the population.
We then used SPSS to explore statistical correlations between variables. We log transformed (Log base 10) COVID-19 mortality to use as our main dependent variable, due to the skewed nature of the mortality data [23]. We excluded US territories from the state analysis, and all PA counties with COVID-19 mortality rate of zero from the county analysis (including Clearfield, Potter, Crawford, Somerset, Warren, Elk, Venango, Jefferson, Greene, Sullivan, Forest, Cameron, and Montour counties). Using both the state and county data, respectively, we performed bivariate analyses between COVID-19 mortality and all potential risk factors, including percentage African-American, using Pearson’s correlations. The bivariate analyses were used to determine which variables to include in multivariable linear regression models to predict COVID-19 mortality rates. We used linear regression models to control for confounding variables (risk factors) that were correlated with COVID-19 mortality in the bivariate analyses. For all statistical analyses, significance was determined based on a p value < 0.05.
Main Findings
As of May 27, 2020, COVID-19 mortality rates were higher in the eastern region of the USA compared to central and western regions, with the highest rates (around 53.58–149.55 deaths per 100,000 population) in the northeast (Fig. 1). The percentages of African-American populations (US Census, 2014–2018) showed similar descriptive patterns as COVID-19 mortality rates, increasing from the west towards the northeast. All northeastern states with mortality rates within the highest category (53.58–149.55 deaths per 100,000 population) also had the highest percentage of African-American populations (22.12–46.94%), with the exception of Connecticut, Rhode Island, and Massachusetts. In these states, African-American populations ranged between 6.55–10.56%.
Many states with low percentages of African-Americans also had low death rates. For instance, in California, 5.79% of the population was African-American, and the mortality rate was 10.12 deaths per 100,000 population, and in Montana, 0.44% of the population was African-American, and 1.63 deaths occurred per 100,000 population.
Looking specifically at PA, COVID-19 mortality rates were similarly high in the eastern part of the state (Fig. 2). Several counties in this region, such as Philadelphia and Monroe, had high COVID-19 death rates ranging from 52.95–95.12 deaths per 100,000 population. These eastern counties also had comparably high African-American population sizes between 3.3 and 4.8%. Counties with the lowest percentages of African-American populations tend to be in north-central or northwest PA, with the majority of counties also having low COVID-19 mortality rates. For example, the population of Elk County was 0.55% African-American and the COVID-19 mortality was 0, and the population of Tioga County was 0.66% African-American with a COVID-19 mortality rate of 4.85 per 100,000.
Statistical Analyses
For US states and for counties within PA, we used Pearson’s correlations (r) to identify significant relationships between log-transformed COVID-19 mortality rates and the following variables: percent African-American population, median household income, hospital beds per population, primary care providers per population, self-reported primary care access, obesity rate, smoking rate, HBP rate, COPD/emphysema/chronic bronchitis rate, and diabetes rate. Variables that were significantly related to COVID-19 mortality were included in a multivariable linear regression model to remove the influence of confounding.
For US states, COVID-19 mortality was only significantly correlated with percent African-American population (r = 0.445, n = 51, p < 0.001). As other variables were not significantly related to COVID-19 mortality, we chose to run a simple linear regression model to quantify the relationship between these variables (Table 1). To interpret the linear regression model, we removed the log-transformation, and found that for every one-percent increase in the African-American population, there was a 2.12% increase in COVID-19 mortality among US states and the District of Columbia.
For PA counties, our bivariate Pearson correlation analysis identified positive correlations between COVID-19 mortality and percent African-American (r = 0.400, n = 54, p = 0.003) and between COVID-19 mortality and income (r = 0.492, n = 54, p < 0.001). Conversely, we observed negative correlations between COVID-19 mortality and COPD (r = − 0.448, n = 54, p = 0.001); and COVID-19 mortality and smoking (r = − 0.427, n = 54, p = 0.001).
Our multivariable linear regression model to predict COVID-19 mortality (Table 2) showed a positive linear association between COVID-19 mortality and percent African-American among PA counties, after controlling for median household income, percent smoking, and percent diagnosed with COPD.
After controlling for potential confounding variables that were correlated with log transformed COVID-19 mortality in our multivariable regression model, we found that the relationship between % African-American and log-transformed COVID-19 mortality rates persisted. For every unit increase in % African-American, there was a 0.035 unit increase in log-transformed COVID-19 mortality rate (t = 2.870, p = 0.006), controlling for median household income, percentage smoking, and percentage diagnosed with COPD. To interpret the linear regression model, we removed the log-transformation, and found that for every 1% increase in the African-American population, there was a 3.56% increase in COVID-19 mortality in PA counties.
Discussion
This article visually and statistically analyzes US state-level and PA county-level COVID-19 mortality rates and the distribution of African-American populations. Variables associated with COVID-19 mortality were included in a multivariable linear regression model to remove potential confounding. Due to the ongoing nature of this pandemic, these findings should be regarded as an interim appraisal. Still, worth noting are various geographical trends on both levels. As of May 27, 2020, COVID-19 mortality rates were higher in US states and PA counties in the east of both regions. This comes as no surprise given that New York City was the “epicenter” for the pandemic [24] and that eastern PA counties have higher population density than the rest of the state [25]. Likewise, African-American population sizes appeared highest in these locations.
Pearson correlations were used to identify positive associations between percent African-American population and log-transformed COVID-19 mortality rates for the USA and PA. However, it is interesting that, on the national level, COVID-19 mortality was only significantly correlated with percent African-American population and not other factors such as diabetes or COPD rate. In PA, COVID-19 mortality was significantly correlated with percent African-American population but also median household income, percent smoking, and COPD rate. When the above risk factors were controlled for, the association between percent African-American and COVID-19 mortality persisted, demonstrating that the association between African-American population and COVID-19 mortality cannot be “explained away” by any of these potential confounding variables at the group level.
As it is unlikely that there is a genetic explanation for higher mortality rates among African-American populations [26], our findings suggest that this relationship may be due to social and environmental factors. Examples of such factors include racial bias in healthcare resulting in lower access to quality and affordable healthcare, both of which drive health inequities apparent in this pandemic [27]. This inequity may be due to delayed access in care because of lower rates in health insurance coverage, according to Poteat et al. [28]. Compared to Caucasian Americans, African-Americans are 1.5 times more likely to either be uninsured or underinsured [28]. Also, in some states, African-Americans with cough and fever symptoms were found to be less likely to receive a COVID-19 test than their Caucasian counterparts [29].
The findings of this investigation stress the importance of equity in addition to equality. Whereas equality focuses on distributing similar resources to all people, equity emphasizes customized distributions that account for disparities between groups [30]. Research suggests that inequitable access to affordable and quality healthcare partially explains unequal COVID-19 mortality rates between races in the USA. It is therefore vital that public health efforts work to eliminate these inequities and provide a customized prevention approach for African-American communities, in order to mitigate unequal health outcomes during the current pandemic, and prevent them for the next.
Our findings also indicate the importance of tracking data on race as it relates to COVID-19. States across the nation should offer more data on race and COVID-19 mortalities, including county-level data, so that public health officials can have adequate surveillance data to identify and, ultimately, address the causes of disparities by race. Similar calls to action are taking place across the country [31], as this step is crucial to fully understand the extent of this disease burden.
Additionally, our findings of COVID-19 mortality trends and associations among African-Americans can inform policy on where to designate resources. These findings also emphasize a need to implement holistic programming to address uneven distributions of access to quality care [27, 32]. State governments can intentionally reduce inequities by providing free SARS-CoV-2 testing sites in African-American communities [33]. In Philadelphia, organizations like the Black Doctors COVID-19 Consortium have already begun such an initiative and would benefit from additional support [34]. These stakeholders should also pressure state governments to expand Medicaid to promote wider access to care [35]. Moreover, incentivizing emission reductions in minority populations, funding green programs, and encouraging input from community members will address health concerns emerging from environmental injustice [36].
It is important to note the methodological limitations of this ecologic study. First, the data used in this report was restricted to the aforementioned timeframe and selected risk factors. Therefore, this report does not describe earlier or future descriptive trends. Second, due to the group-level nature of the data, our results are limited to description and analyses of relationships between US states and counties. While we identified a positive relationship between COVID-19 mortality and percent African-American population, the same results cannot be applied to individuals—we provide no evidence that African-Americans are more likely to die from complications resulting from COVID-19, due to the limitations of the ecologic data. Third, not all racial and ethnic groups are represented in this study, and there is no delineation between subgroups within the African-American community. Future analysis could explore the relationship between COVID-19 mortality and demographics among counties in the full US population.
Conclusion
The disproportionate effect of COVID-19 on the African-American community clearly demands action at the local, state, and US national levels. Through GIS mapping, we observed similar descriptive patterns of COVID-19 mortality and African-American population among US states and PA counties. Higher rates occurred in northeast states and eastern counties, where African-American population sizes were relatively high. These descriptive patterns were confirmed through bivariate statistical tests, and persisted after controlling for confounders. We need equity-driven public health interventions to address these disparities, including social, behavioral, economic, and policy changes prioritizing areas exhibiting the greatest burden of COVID-19 mortality, especially in minority communities. Examples include providing free SARS-CoV-2 testing in African-American communities, expanding Medicaid, and incentivizing emission reductions in minority communities. Of vital importance is the need for more comprehensive race-specific COVID-19 outcome data. With access to this data, researchers can readily identify geographic and demographic focus areas for population based prevention efforts, and improve health equity.
Data Availability
The mapping data utilized for this report were derived from the following sites:
1. U.S. Census. TIGER/Line shapefiles. 2010. https://www.census.gov/cgi-bin/geo/shapefiles/index.php?year=2010&layergroup=Counties+%28and+equivalent%29 Accessed 8 June 2020.
2. PolicyMap. Health. 2020. https://tju-policymap-com.proxy1.lib.tju.edu/maps Accessed 26 August 2020.
3. PolicyMap. Demographics. 2010. https://tju-policymap-com.proxy1.lib.tju.edu/maps Accessed 26 August 2020.
References
Centers for Disease Control and Prevention. Cases in the U.S. In: Coronavirus disease 2019 (COVID-19). CDC. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed 1 June 2020.
Kaiser Family Foundation. State data and policy actions to address Coronavirus. KFF. 2020. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/. Accessed 31 Aug 2020.
The COVID Racial Data Tracker. COVID-19 is affecting Black, Indigenous, Latinx, and other people of color the most. The COVID Tracking Project at The Atlantic. 2020. https://covidtracking.com/race. Accessed 15 Sept 2020.
Zephyrin L, Radley DC, Getachew Y, Baumgartner JC, Schneider EC. COVID-19 more prevalent, deadlier in U.S. counties with higher Black populations. The Commonwealth Fund. 2020. https://www.commonwealthfund.org/blog/2020/covid-19-more-prevalent-deadlier-us-counties-higher-black-populations. Accessed 15 Sept 2020.
Child Welfare Information Gateway. Racial disproportionality and disparity in child welfare. Child Welfare. 2016. https://www.childwelfare.gov/pubPDFs/racial_disproportionality.pdf#page=2&view=Prevalence. Accessed 1 June 2020.
Brandt EB, Beck AF, Mersha TB. Air pollution, racial disparities, and COVID-19 mortality. J Allergy Clin Immunol. 2020;146:61–3. https://doi.org/10.1016/j.jaci.2020.04.035.
Millett GA, Jones AT, Benkeser D, Baral S, Mercer L, Beyrer C, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. https://doi.org/10.1016/j.annepidem.2020.05.003.
Moore JX, Langston ME, George V, Coughlin SS. Epidemiology of the 2020 pandemic of COVID-19 in the state of Georgia: inadequate critical care resources and impact after 7 weeks of community spread. J Am Coll Emerg Physicians Open. 2020;1:527–32. https://doi.org/10.1002/emp2.12127.
Krouse HJ. COVID-19 and the widening gap in health inequity. Otolaryngol Head Neck Surg. 2020;163:65–6. https://doi.org/10.1177/0194599820926463.
Peterson R, Pan L, Blanck HM. Racial and ethnic disparities in adult obesity in the United States: CDC’s tracking to inform state and local action. Prev Chronic Dis. 2019;16. https://doi.org/10.5888/pcd16.180579.
U.S. Department of Health and Human Services. Asthma and African Americans. Office of Minority Health. 2018. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=15. Accessed 1 June 2020.
Gross T. A ‘forgotten history’ of how the U.S. government segregated America. NPR. 2017. https://www.npr.org/2017/05/03/526655831/a-forgotten-history-of-how-the-u-s-government-segregated-america. Accessed 1 June 2020.
Mohammed AA, Mohamed FY, El-Okda E, Ahmed AB. Blood lead levels and childhood asthma. Indian Pediatr. 2015;52:303–306. https://indianpediatrics.net/apr2015/303.pdf. Accessed 1 Jun 2020.
Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. 2020. https://doi.org/10.1002/ajim.23145. Accessed 8 Aug 2020.
Bulatao RA, Anderson NB. Understanding racial and ethnic differences in health in late life: a research agenda. 2004. https://www.ncbi.nlm.nih.gov/books/NBK24693/. Accessed 8 August 2020.
Spertus JA, Jones PG, Masoudi FA, Rumsfeld JS, Krumholz HM. Factors associated with racial differences in myocardial infarction outcomes. Ann Intern Med. 2009;150:314–324. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3387537/. Accessed 31 Aug 2020.
Johns Hopkins University. State COVID-19 data by race. In: Racial data transparency. Johns Hopkins University. 2020. https://coronavirus.jhu.edu/data/us-state-data-availability. Accessed 31 Aug 2020.
Pennsylvania Department of Health. COVID-19 data for Pennsylvania. 2020. https://www.health.pa.gov/topics/disease/coronavirus/Pages/Cases.aspx. Accessed 31 August 2020.
Data USA. Diversity. In: Pennsylvania. Deloitte. 2018. https://datausa.io/profile/geo/pennsylvania#demographics. Accessed 31 August 2020.
PolicyMap. Health. 2020. https://tju-policymap-com.proxy1.lib.tju.edu/maps. Accessed 31 August 2020.
United States Census Bureau. TIGER/Line shapefiles. US Department of Commerce. 2020. https://www.census.gov/cgi-bin/geo/shapefiles/index.php. Accessed 8 August 2020.
The New York Times. COVID-19 data. 2020. https://github.com/nytimes/covid-19-data. Accessed 27 May 2020.
Ford C. Interpreting log transformations in a linear model. University of Virginia Library. 2018. https://data.library.virginia.edu/interpreting-log-transformations-in-a-linear-model. Accessed 31 August 2020.
Chakrabarti M, Kotsonis S. How New York City became the epicenter of the coronavirus pandemic. Wbur. 2020. https://www.wbur.org/onpoint/2020/04/13/new-york-city-epicenter-pandemic. Accessed 1 June 2020.
Novak S. Pa. coronavirus update: When the stay-at-home order will end in Lehigh Valley, Philly, Poconos. Lehigh Valley. 2020. https://www.lehighvalleylive.com/coronavirus/2020/05/pa-coronavirus-update-when-the-stay-at-home-order-will-end-in-lehigh-valley-philly-poconos-1st-green-phase-counties-announced-cases-reach-66k-with-nearly-5k-deaths-covid-19-case-map-52220.html. Accessed 15 Sept 2020.
Gravlee CC. How race becomes biology: Embodiment of social inequality. Am J Phys Anthropol. 2009;139:47–57. https://doi.org/10.1002/ajpa.20983.
Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the U.S. J Clin Med. 2020;9:1–17. https://doi.org/10.3390/jcm9082442.
Poteat T, Millett GA, Nelson LE, Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: The lethal force of syndemics. Ann Epidemiol. 2020;47:1–3. https://doi.org/10.1016/j.annepidem.2020.05.004.
Williams DR, Cooper LA. COVID-19 and health equity--a new kind of “herd immunity.” JAMA. 2020;323:2478–2480. https://doi.org/10.1001/jama.2020.8051.
Kurapati S. Health equality vs. health equity. American Medical Women’s Association. 2020. https://www.amwa-doc.org/health-equality-vs-health-equity/. Accessed 18 Sept 2020.
Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398–402. https://doi.org/10.1007/s40615-020-00756-0. Accessed 18 Sept 2020.
Jahromi AH, Hamidianjahromi A. Why African-Americans are a potential target for COVID-19 infection in the United States. J Med Internet Res. 2020;22:e19934.https://doi.org/10.2196/19934.
Servick K. ‘Huge hole’ in COVID-19 testing data makes it harder to study racial disparities. Science. 2020. https://doi.org/10.1126/science.abd7715.
Black Doctors COVID-19 Consortium. 2020. https://blackdoctorsconsortium.com/. Accessed 18 Sept 2020.
Achieving health equity in the United States. American Public Health Association. 2018. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2019/01/29/achieving-health-equity. Accessed 18 Sept 2020.
Addressing environmental justice to achieve health equity. American Public Health Association. 2019. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2020/01/14/addressing-environmental-justice-to-achieve-health-equity. Accessed 18 Sept 2020.
Acknowledgments
The authors would likely to thank Jennifer F. Wilson for her invaluable support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Not applicable.
Informed Consent
Not applicable.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anaele, B.I., Doran, C. & McIntire, R. Visualizing COVID-19 Mortality Rates and African-American Populations in the USA and Pennsylvania. J. Racial and Ethnic Health Disparities 8, 1356–1363 (2021). https://doi.org/10.1007/s40615-020-00897-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00897-2