Abstract
Background
Ensuring health equity, especially for vulnerable populations in less developed settings with poor health system is essential for the current and future global health threats. This study examined geographical variations of COVID-19 mortality and its association with population health characteristics, health care capacity in responding pandemic, and socio-economic characteristics across 514 districts in Indonesia.
Methods
This nationwide ecological study included aggregated data of COVID-19 cases and deaths from all 514 districts in Indonesia, recorded in the National COVID-19 Task Force database, during the first two years of the epidemic, from 1 March 2020 to 27 February 2022. The dependent variable was district-level COVID-19 mortality rate per 100,000 populations. The independent variables include district-level COVID-19 incidence rate, population health, health care capacity, and socio-demographics data from government official sources. We used multivariable ordinal logistic regression to examine factors associated with higher mortality rate.
Results
Of total 5,539,333 reported COVID-19 cases, 148,034 (2.7%) died, and 5,391,299 (97.4%) were recovered. The district-level mortality rate ranged from 0 to 284 deaths per 100,000 populations. The top five districts with the highest mortality rate were Balikpapan (284 deaths per 100,000 populations), Semarang (263), Madiun (254), Magelang (250), and Yogyakarta (247). A higher COVID-19 incidence (coefficient 1.64, 95% CI 1.22 to 1.75), a higher proportion of ≥ 60 years old population (coefficient 0.26, 95% CI 0.06 to 0.46), a higher prevalence of diabetes mellitus (coefficient 0.60, 95% CI 0.37 to 0.84), a lower prevalence of obesity (coefficient -0.32, 95% CI -0.56 to -0.08), a lower number of nurses per population (coefficient -0.27, 95% CI -0.50 to -0.04), a higher number of midwives per population (coefficient 0.32, 95% CI 0.13 to 0.50), and a higher expenditure (coefficient 0.34, 95% CI 0.10 to 0.57) was associated with a higher COVID-19 mortality rate.
Conclusion
COVID-19 mortality rate in Indonesia was highly heterogeneous and associated with higher COVID-19 incidence, different prevalence of pre-existing comorbidity, healthcare capacity in responding the pandemic, and socio-economic characteristics. This study revealed the need of controlling both COVID-19 and those known comorbidities, health capacity strengthening, and better resource allocation to ensure optimal health outcomes for vulnerable population.
Similar content being viewed by others
Background
The coronavirus disease 2019 (COVID-19) pandemic caused by the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused millions of deaths worldwide [1]. As of 23 December 2022, there have been over 6.6 million deaths among over 650 million total confirmed COVID-19 cases reported to the World Health Organization (WHO) [1]. It was estimated that the full impact of the pandemic has been much greater than what is indicated by reported deaths due to COVID-19 [2]. The global impact of the pandemic was heterogeneous and has been associated with different level of pre-existing health systems capacity in managing and responding the pandemic [3, 4].
Ensuring health equity, especially for vulnerable populations in less developed settings with poor health systems is essential for the current COVID-19 pandemic and future global health threats [5,6,7,8,9,10,11]. At community-level, it is known that the severity of illness and clinical outcomes can be affected by the concentration of comorbidities in susceptible groups in communities [12,13,14,15], and through disparities in access to health care for preventive measures or prompt diagnosis and treatment [15, 16]. Recent findings in US, Chile and Brazil suggested that COVID-19 poor outcome was concentrated in groups with higher socio-demographics and health system vulnerability [15, 17,18,19,20,21]. However, evidence of the geographical variations of COVID-19 impact from low- and middle-income countries (LMIC) where differences in age distribution, comorbidities, access to quality health services, and other factors, may significantly influence mortality risk, are limited.
Indonesia has suffered the highest number of COVID-19 confirmed cases and deaths in Southeast Asia, second only to India in all of Asia [22], at over 6.7 million cases and 160,583 deaths (2.4% case fatality rate (CFR)) up to 29 December 2022 [23]. The first SARS-CoV-2 epidemic wave occurred from 2 March 2020 to 30 April 2021, and a more intense second wave dominated by Delta variant peaked in July 2021 [24], followed by the third wave peaked in February 2022 [23]. The majority of cases and deaths in Indonesia were reported in Java Island, a more developed setting populated by 152 million individuals (56% of the total Indonesia’s population). Recent studies from Indonesia’s capital city of Jakarta suggested that COVID-19 disproportionately affected individuals with older age and pre-existing chronic comorbidities, as well as those areas within Jakarta with lower vaccine coverage, and higher poverty and population density [25, 26]. However, data on the impact of COVID-19 across 514 districts of Indonesia that have different pre-existing burdens of major infectious diseases such as malaria, tuberculosis, HIV and other tropical infections [27], as well as non-communicable diseases like cardiovascular diseases, cancers, chronic pulmonary diseases, diabetes, and others [28], are scarce.
Indonesia is the fourth most populous country (population 270 million) and the LMIC featuring great geographic, cultural and socio-economic diversity across the archipelago. The 2020 Human Development Index (HDI) ranged from 0.32 in Kabupaten Nduga, Papua Province to 0.87 in Kota Yogyakarta, Yogyakarta Province [29]. In addition, substantial proportions of the Indonesian population face barriers in accessing quality health care services due to under-resourced and fragile health systems [27]. A heavily decentralised health systems [30] has resulted in distinct public health capacity across 514 districts of Indonesia. For example, the 2018 Public Health Development Index (PHDI) ranges from 35% in Kabupaten Paniai, Papua Province to 75% in Kabupaten Gianyar, Bali province [31]. That heterogeneity and the large number of COVID-19 cases and deaths provides insights directly relevant to the national public health response to the COVID-19 crisis, and other LMIC settings. Due to the absence of individual-level data of COVID-19 cases and mortality, no study has been done to assess nationwide geographical variations of COVID-19 impacts in Indonesia. In this study, we utilised district-level aggregated data to assess geographical variations of COVID-19 mortality, socio-economics, population health-related conditions, and health care capacity among all 514 districts of Indonesia and how those factors were associated with COVID-19 mortality rate during the first 24 months of the epidemic in Indonesia (March 2020 through February 2022). The study findings will inform decision on health resource allocation and public health interventions to better control COVID-19 pandemic and strengthen health systems resilience in the future.
Methods
Study design and participants
This was a nationwide ecological study to assess COVID-19 burden, geographical distributions, and factors associated with mortality rate in all 514 districts in Indonesia. The study analysed aggregated data of individuals diagnosed with COVID-19 based on either rapid antigen diagnostic test (Ag RDT) or polymerase chain reaction (PCR) recorded by the National COVID-19 Task Force from 1 March 2020 to 27 February 2022. In accordance with Indonesia’s national COVID-19 guideline, individuals are categorized as COVID-19 confirmed cases if tested positive by Ag RDT or PCR.
The dependent variable in this study was district-level COVID-19 mortality rate per 100,000 population. The independent variables assessed were COVID-19 incidence rate, proportion of ≥ 60 years old individuals, prevalence of hypertension, prevalence of diabetes mellitus, prevalence of central obesity, prevalence of pneumonia, COVID-19 vaccine coverage for ≥ 60 years old population, number of doctors, nurses, midwives, and hospitals per 10,000 population, expenditure, life expectancy at birth, and length of formal education.
Data collection
The aggregated data of weekly number of COVID-19 cases, incidence rate per 100,000 population, number of COVID-19 deaths among confirmed cases, and mortality rate per 100,000 population by district from 1 March 2020 to 27 February 2022 were collected from the government official COVID-19 database managed by the National COVID-19 Task Force [32]. District-level data on the number of populations were collected from Statistics Bureau Database available in each province. Data on the number of doctors, nurses, midwives, and hospitals per October 2021 were collected from the Indonesia Ministry of Health records. Data on pre-existing prevalence of hypertension, diabetes mellitus, central obesity, and clinical pneumonia were collected from the latest available National Public Health Development Index (PHDI) 2018 Report [31]. Data on the COVID-19 two-dose vaccine coverage for ≥ 60 years old population by district per 27 February 2022 were collected from the National COVID-19 Vaccination Database [33]. Data on expenditure, life expectancy at birth, and length of formal education were collected from the latest available Human Development Index 2020 Report [29]. The detailed definition and data source of each variable is presented in Table 1.
Statistical analysis
District-level COVID-19 incidence and mortality rate per 100,000 populations, proportion of ≥ 60 years old population, prevalence of hypertension (%), prevalence of diabetes mellitus (%), prevalence of central obesity (%), prevalence of pneumonia (%), COVID-19 vaccine coverage for ≥ 60 years old population (%), number of doctors, nurses, midwives, and hospitals per 100,000 population, expenditure (millions IDR), life expectancy at birth (years), and length of formal education (years) were calculated then categorised into quartiles.
Descriptive statistics included proportions and the chi-squared test to compare district-level characteristics between different quartiles. Spearman’s correlation tests were done to assess correlation between each district-level variable. We used bivariable and multivariable ordinal logistic regression models to determine factors associated with higher mortality rate at district level, expressed as regression coefficient, with 95% confidence intervals (CI). All independent variables with p-value < 0.10 in bivariable analysis were included in the multivariable models. Final model selection was informed by likelihood ratio tests.
The proportion of missing data were 2.3% for prevalence of hypertension, 0.6% for diabetes, 1.4% for central obesity, and 7.6% for number of hospitals. Missing-indicator analysis by explanatory variable stratification and by regression analysis identified missing at random, thus justified the exclusion of 47 (9%) districts from the final multivariable model. We set statistical significance at 0.05, and all tests were two-sided. All analyses were done in Stata/IC 15.1 (StataCorp, College Station, TX, USA). Maps showing geographical distribution of COVID-19 incidence and mortality rate were generated using QGIS 3.20 software. This study is reported as per Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [32].
Results
Cumulative COVID-19 incidence and mortality rate at national-level
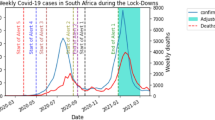
A total of 5,539,333 COVID-19 cases from all 514 districts in Indonesia were recorded on the Indonesia National COVID-19 Database between 1 March 2020 and 27 February 2022. Of those, 148,034 (2.7%) were deceased, and 5,391,299 (97.4%) were recovered. The overall incidence and mortality rates were 2,050 and 55 per 100,000 populations, respectively. Indonesia had experienced three pandemic waves with the highest mortality recorded in week 73rd (12 to 18 July 2021) where cases were predominantly infected by Delta variant (Fig. 1). Overall, the incidence and mortality rate increased over time, with DKI Jakarta being area with consistently high incidence and mortality rate over time (Fig. 2).
COVID-19 incidence and mortality rate at district-level
The incidence and mortality rate varied widely by district (Fig. 3). Whilst the incidence rate ranged from 8.1 to 10,626.1 per 100,000 populations (Fig. 3A), the mortality rate ranged from 0 to 283.8 per 100,000 populations (Fig. 3B). Based on Table 2, the top ten highest incidence rate were reported in Kota Jakarta Pusat (10,626 cases per 100,000 populations), Kota Jakarta Selatan (10,308), Kota Bontang (9708), Kota Jakarta Timur (8934), Kabupaten Bulungan (8904), Kota Jakarta Barat (8285), Kota Depok (8229), Kota Jakarta Selatan (8055), Kota Yogyakarta (7806), and Kota Denpasar (7773). The top ten highest mortality rate were reported in Kota Balikpapan (284 deaths per 100,000 populations), Kota Semarang (263), Kota Madiun (254), Kota Magelang (250), Kota Yogyakarta (249), Kota Bontang (247), Kota Surakarta (199), Kota Palangkaraya (184), Kota Tanjungpinang (183), and Kabupaten Berau (178) (Table 3). Summary of incidence and mortality rate in all 514 districts can be found in Supplementary Table 1 and 2.
COVID-19 burden and other characteristics
The summary of district-level COVID-19 burden and other characteristics associated with COVID-19 mortality rate across 514 districts in Indonesia is presented in Supplementary Table 3. Of 129 districts in the highest mortality rate quartile, 71% had the highest incidence rate. 44% of districts with the highest mortality rate had the highest proportion of ≥ 60 years old population (range 10–20%), and 48% had the highest prevalence of diabetes mellitus (range 3–50%). Regarding health care capacity, 47% of districts with the highest mortality rate had the highest COVID-19 vaccine coverage for ≥ 60 years old population (range 46–86%), and 24% had the lowest number of nurses per 100,000 populations (range 0.5–11). Regarding socio-economic, 57% of districts with the highest mortality rate had the highest expenditure (range IDR 12–24 million) (See Supplementary Table 3 for details).
Factors associated with higher mortality rate
In the multivariable model (Table 4), a higher mortality rate was associated with a higher COVID-19 incidence (coefficient 1.64, 95% CI 1.22 to 1.75), a higher proportion of ≥ 60 years old population (coefficient 0.26, 95% CI 0.06 to 0.46), a higher prevalence of diabetes mellitus (coefficient 0.60, 95% CI 0.37 to 0.84), a lower prevalence of central obesity (coefficient -0.32, 95% CI -0.56 to -0.08), a lower number of nurses per population (coefficient -0.27, 95% CI -0.50 to -0.04), a higher number of midwives per population (coefficient 0.32, 95% CI 0.13 to 0.50), and a higher expenditure (coefficient 0.34, 95% CI 0.10 to 0.57). There was no association between COVID-19 mortality rate with prevalence of hypertension, prevalence of pneumonia, vaccine coverage for ≥ 60 years ole population, number of doctors and hospitals per population, life expectancy at birth, and length of formal education (p > 0.05 each). Correlation matrix of COVID-19 burden, prevalence of health-related conditions, vaccine coverage for > 60 years old population, health care capacity, and socio-economic characteristics can be seen in Fig. 4 and Supplementary Table 4.
Correlation matrix of COVID-19 burden, prevalence of health-related conditions, vaccine coverage for > 60 years old population, health care capacity, and socio-economic characteristics. Significance level of the correlation can be seen in Supplementary Table 4
Discussion
This nationwide ecological study analysed the epidemiological surveillance data of confirmed COVID-19 cases reported from 514 districts in the first 24 months of the SARS-CoV-2 transmission in Indonesia. Indonesia had experienced three pandemic waves with the highest mortality recorded in week 73rd (12 to 18 July 2021) where cases were predominantly infected by Delta variant. The overall COVID-19 case fatality rate was 2.7% (148,034/5,539,333), which equate to a mortality rate of 55 per 100,000 populations. The mortality rate increased over time and was highly heterogeneous over space, with the top ten highest rate seen in Kota Balikpapan, Kota Semarang, Kota Madiun, Kota Magelang, Kota Yogyakarta, Kota Bontang, Kota Surakarta, Kota Palangkaraya, Kota Tanjungpinang, and Kabupaten Berau. A higher district-level mortality rate was associated with a higher COVID-19 incidence, a higher proportion of ≥ 60 years old population, a higher prevalence of diabetes mellitus, a lower prevalence of central obesity, a lower number of nurses per population, a higher number of midwives per population, and a higher expenditure.
Our study described the geographical variations and factors associated with higher COVID-19 mortality in Indonesia. Our findings suggest that the mortality rates tend to be higher in districts located in more developed provinces in Java and Kalimantan Islands (Fig. 2A), and in districts with a higher expenditure. Whilst no previous studies have reported the geographical patterns of COVID-19 mortality in Indonesia, a previous province-level analysis reported DKI Jakarta and other provinces in Java and Kalimantan Islands as the hotspots of cases in the early phase of COVID-19 epidemic in Indonesia [33]. In addition, concordant with the multivariable model suggesting a higher COVID-19 incidence rate as the strongest predictor of a higher COVID-19 mortality rate, the overlapped spatial distribution of high mortality and incidence rate (Fig. 2A-B) further illustrates that districts with a higher incidence rate were more likely to have a higher mortality rate.
Consistent with individual-level risk factors from diverse settings [18, 25, 34, 35], our district-level analysis suggests that higher proportion of elder population and higher prevalence of diabetes mellitus were significantly associated with higher COVID-19 mortality rate in Indonesia. Our analysis reinforces findings from a previous study suggesting that individual-level risk factors such as older age and pre-existing diabetes were associated with an elevated risk of COVID-19 death during the early epidemic phase in DKI Jakarta, Indonesia [25]. These findings indicate the need of controlling both SARS-Cov-2 transmission and non-communicable diseases, especially in areas with high prevalence of diabetes mellitus. Reducing COVID-19 mortality in such settings may necessitate comprehensive and specific interventions such as improving diagnosis and case management of those known non-communicable diseases, community awareness, as well as a sustainable and accessible social security network that may reduce vulnerability of these communities.
Our findings suggesting a higher mortality rate among districts with a higher expenditure was inconsistent with previous findings from a large cohort study in DKI Jakarta, suggesting that risk of mortality was higher for individuals living in areas with higher level of poverty [24]. Whilst previous studies from more developed settings such as in the US [11, 36] and Sweden [37] suggested that higher mortality was associated with lower level of education, our present study found there was no association between mortality rate and level of formal education. A lower educational level might be associated with a lower health literacy that can lead to lower access and understanding of public health information. A tailored risk communication and community engagement strategy targeting population living in districts with lower education level is warranted in addressing health inequity in the future.
Consistent with a previous province-level analysis (n = 34) that found the absence of correlation between mortality rate with doctor to population ratio during the first six months of the epidemic [38], our district-level analysis also found the absence of association between mortality rate with doctor to population ratio during the first 24 months of the epidemic. This finding contrasts a previous finding from a higher-income country, reporting an association between higher COVID-19 mortality rate with higher physicians density in France [39]. Nonetheless, our study suggests that a higher mortality rate was associated with a lower number of nurses per population. In Indonesia, the lack of healthcare workers, combined with the high number of infections [40] and deaths among health care workers and doctors [41], especially during the early phase of the epidemic, had weakened the health system resilience. A recent review of Indonesian healthcare system suggested that the currently available medical staffs are insufficient to deal with the pandemic, and that the referral system in Indonesia has been hampered by a shortage of specialists and poorly equipped referral facilities, as well as weak coordination, even before the pandemic [42]. In the context of a heavily decentralized health system such as in Indonesia [30], coordination and prioritisation of available resources and public health intervention will be critical to ensure optimal health outcomes for vulnerable communities, especially for those areas with lower capacity. Short-term human resources strategies can include recruiting trained health care volunteers and redistributing healthcare professionals within province. Moreover, optimising role of residents, fast-tracking nurse training through an accelerated program [43], and recruiting final-year medical students to join the task force within their limits of competence [44] can be potential long-term strategies.
A previous cohort study in DKI Jakarta reported that higher COVID-9-related mortality risk was significantly associated with lower COVID-19 vaccine coverage at subdistrict-level [24]. By contrast, our current study found that there was no association between district-level COVID-9 mortality rate with COVID-19 vaccine coverage among > 60 years old population in Indonesia. This absence of association could possibly be explained by the very low vaccine coverage across the 514 districts. The vaccine coverage was highly varied from 0.03% to 86.20%. The majority of districts (82.3%) still had a vaccine coverage of less than 50% after one year of vaccine roll-out (27 February 2022), thus further highlights the extent of inequity across the country. A previous study from Brazil reported that rapid scaling up of vaccination coverage among elderly Brazilians was associated with significant declines in relative mortality compared with younger individuals, in a setting where the gamma variant predominated [45]. Despite of the current limited available drugs and ineffective vaccine against new emerging variants of SARS-CoV-2 [46], those findings from DKI Jakarta and Brazil, highlight that rapid vaccination roll outs targeting the most vulnerable is crucial in reducing COVID-19-related deaths. As per 29 December 2022, the coverage for two-dose and three-doses COVID-19 vaccination in Indonesia was 86.94% (204,014,895/234,666,020 targeted population) and 74.47% (174,756,560/234,666,020), respectively [47].
This study had several limitations. Firstly, this study was based on routine surveillance data derived from district-level health office case reports. The imperfect contact tracing, testing, and reporting activities could result in underreporting of cases, especially those asymptomatic and mild cases, which could cause an overestimation of case fatality rate and an underestimation of mortality rate per population in this study. Secondly, as this study was based on aggregated data available at district level, our analysis was unable to capture and adjust the effect of important individual-level risk factors. For example, at individual level analysis, the association between a higher COVID-19 mortality with a lower prevalence of central obesity might be confounded by the presence of important effect modifiers variables such as type 2 diabetes, hypertension, and cardiovascular disease [48]. However, we were unable to assess these interactions at our district-level analysis. Therefore, interpretation of the study findings should be restricted to district-level risk factors. Thirdly, the use of data from the 2018 PHDI (the most updated available data) may not reflect the current health systems capacity in responding COVID-19 pandemic in Indonesia. However, the use of these data reflects the existing public health systems capacity in Indonesia prior to the pandemic, which were important indicators of health systems resilience. Finally, previous studies in Indonesia have suggested the association between COVID-19 mortality rate with population density [24] and ratio of hospitals bed [38]. However, these variables were not evaluated in our study, due to limited access to the relevant data. The absence of association for several explanatory variables and the unexplainable association between a higher mortality with a higher number of midwives per population in the present study might be due to the current limitations.
Conclusions
In conclusion, our analysis suggested that COVID-19 pandemic disproportionately affected districts with high COVID-19 incidence rate, high proportion of elder population, high prevalence of diabetes mellitus, and low nurses to population ratio. These findings indicate that vulnerability to death associated with COVID-19 includes not only elders and comorbid, but also communities living in area with higher COVID-19 incidence and lower health care capacity. These findings may inform decisions on health resource allocation against COVID-19 delivering the greatest possible health dividends by prioritising interventions, including even distribution of essential health care need for the most vulnerable communities in LMIC, especially with decentralised health systems like in Indonesia. Improved diagnosis and case management of those known comorbidities may reduce risk of COVID-19 mortality in these communities. Future nationwide studies incorporating individual and district-level data to assess vulnerability associated with COVID-19-related morbidity and mortality are needed to better comprehend the COVID-19 impact and to better prioritise interventions for the most vulnerable communities.
Availability of data and materials
After publication, the datasets used for this study will be made available to others on reasonable requests to the corresponding author, including a detailed research proposal, study objectives and statistical analysis plan.
Abbreviations
- CFR:
-
Case Fatality Rate
- CI:
-
Confidence Interval
- COVID-19:
-
Coronavirus disease 2019
- HDI:
-
Human Development Index
- LMIC:
-
Low- and middle-income countries
- PHDI:
-
Public Health Development Index
- PCR:
-
Polymerase Chain Reaction
- Ag RDT:
-
Rapid Antigen Diagnostic Test
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- WHO:
-
World Health Organization
References
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available: https://covid19.who.int [Accessed 30 December 2022].
Wang H, Paulson KR, Pease SA, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022;399(10334):1513–36.
Haldane V, Foo CD, Abdalla SM, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nature Med. 2021;27:964–80.
Kandel N, Chungong S, Omaar A, et al. Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. Lancet. 2020;395:1047–53.
World Health Organization. Strategic preparedness, readiness and response plan to end the global COVID-19 emergency in 2022. Geneva: World Health Organization; 2022.
Lowcock EC, Rosella LC, Foisy J, et al. The social determinants of health and pandemic h1n1 2009 influenza severity. Am J Public Health. 2012;102:51–8.
Mayoral JM, Alonso J, Garín O, et al. Social factors related to the clinical severity of influenza cases in Spain during the A ( H1N1) 2009 virus pandemic. BMC Public Health. 2013;118:1–7.
Grantz KH, Rane MS, Salje H, et al. Disparities in influenza mortality and transmission related to sociodemographic factors within Chicago in the pandemic of 1918. Proc Natl Acad Sci U S A. 2016;113:13839–44.
Mamelund SE. A socially neutral disease? Individual social class, household wealth and mortality from Spanish influenza in two socially contrasting parishes in Kristiania 1918–19. Soc Sci Med. 2006;62:923–40.
Fallah MP, Skrip LA, Gertler S, Yamin D, Galvani AP. Quantifying poverty as a driver of ebola transmission. PLoS Negl Trop Dis. 2015;9:1–9.
Fahriani M, Anwar S, Yufika A, et al. Disruption of childhood vaccination during the COVID-19 pandemic in Indonesia. Narra J. 2021;1(1):e7.
Seligman B, Ferranna M, Bloom DE. Social determinants of mortality from COVID-19: A simulation study using NHANES. PLoS Med. 2021;18:1–13.
Acharya R, Porwal A. A vulnerability index for the management of and response to the COVID-19 epidemic in India: an ecological study. Lancet Glob Heal. 2020;8:e1142–51.
Yoshikawa Y, Kawachi I. Association of socioeconomic characteristics with disparities in COVID-19 outcomes in Japan. JAMA Netw Open. 2021;4:1–13.
Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Heal. 2021;9:e782–92.
Harlem G. Descriptive analysis of social determinant factors in urban communities affected by COVID-19. J Public Heal (United Kingdom). 2020;42:466–9.
Karmakar M, Lantz PM, Tipirneni R. Association of Social and Demographic Factors with COVID-19 Incidence and Death Rates in the US. JAMA Netw Open. 2021;4:1–12.
Mena GE, Martinez PP, Mahmud AS, Marquet PA, Buckee CO, Santillana M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science. 2021;372;eabg5298.
Oliveira EA, Colosimo EA, Simões e Silva AC, Mak RH, Martelli DB, Silva LR, et al. Clinical characteristics and risk factors for death among hospitalised children and adolescents with COVID-19 in Brazil: an analysis of a nationwide database. Lancet Child Adolesc Heal. 2021;5:559–68.
Sousa BLA, Brentani A, Costa Ribeiro CC, Dolhnikoff M, Grisi SJFE, Ferrer APS, et al. Non-communicable diseases, sociodemographic vulnerability and the risk of mortality in hospitalised children and adolescents with COVID-19 in Brazil: a cross-sectional observational study. BMJ Open. 2021;11: e050724.
Chen JT, Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J Public Heal Manag Pract. 2021;27:S46-56.
Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–4.
Peta Sebaran COVID-19. https://covid19.go.id/peta-sebaran (Accessed 30 December 2022).
Dyer O. Covid-19: Indonesia becomes Asia’s new pandemic epicentre as delta variant spreads. BMJ. 2021;374: n1815.
Surendra H, Salama N, Lestari K, Adrian V, Nurhasim A, Shankar AH, et al. Pandemic inequity in a megacity: a multilevel analysis of individual, community, and health care vulnerability risks for COVID-19 mortality in Jakarta, Indonesia. BMJ Glob Heal. 2022;7(6):e008329.
Surendra H, Elyazar IRF, Djaafara BA, et al. Clinical characteristics and mortality associated with COVID-19 in Jakarta, Indonesia : A hospital-based retrospective cohort study. Lancet Reg Heal - West Pacific. 2021;9: 100108.
Mboi N, Murty Surbakti I, Trihandini I, et al. On the road to universal health care in Indonesia, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:581–91.
World Health Organization. Noncommunicable diseases country profiles 2018. Geneva: World Health Organization; 2018.
Badan Pusat Statistik Indonesia. https://www.bps.go.id/dynamictable/2020/02/17/1771/indeks-pembangunan-manusia-menurut-kabupaten-kota-metode-baru-2010-2019.html 2019.
Mahendradhata Y, Trisnantoro L, Listyadewi S, et al. The Republic of Indonesia Health System Review, vol. 7 No. 1. New Delhi: World Health Organization, Regional Office for South-East Asia; 2017.
Kementerian Kesehatan Republik Indonesia. Indeks Pembangunan Kesehatan Masyarakat 2018. Jakarta: Lembaga Penerbit Badan Penelitian dan Pengembangan Kesehatan; 2019.
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9.
Aisyah DN, Mayadewi CA, Diva H, et al. A spatial-temporal description of the SARS-CoV-2 infections in Indonesia during the first six months of outbreak. PLoS ONE. 2020;15(12): e0243703.
Harrison SL, Fazio-Eynullayeva E, Lane DA, et al. Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: A federated electronic medical record analysis. PLoS Med. 2020;17:1–11.
Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ. 2020;369:1–12.
Hawkins RB, Charles EJ, Mehaffey JH. Socio-economic status and COVID-19–related cases and fatalities. Public Health. 2020;189:129–34.
Calderón-Larrañaga A, Vetrano DL, Rizzuto D, et al. High excess mortality in areas with young and socially vulnerable populations during the COVID-19 outbreak in Stockholm Region, Sweden. BMJ Glob Heal. 2020;5(10):e003595.
Wirawan GBS, Januraga PP. Correlation of demographics, healthcare availability, and COVID-19 outcome: Indonesian ecological study. Front Public Heal. 2021;9:605290.
Tchicaya A, Lorentz N, Leduc K, et al. COVID-19 mortality with regard to healthcare services availability, health risks, and socio-spatial factors at department level in France: A spatial cross-sectional analysis. PLoS ONE. 2021;16:1–19.
Sinto R, Utomo D, Suwarti, et al. Antibody responses and reactogenicity of a heterologous, full-dose messenger RNA-1273 booster in heavily SARS-CoV-2–exposed CoronaVac-vaccinated health-care workers in Indonesia: a real-world observational study. Am J Trop Med Hyg. 2022;108(1):115–23.
Ekawati LL, Arif A, Hidayana I, et al. Mortality among healthcare workers in Indonesia during 18 months of COVID-19. PLOS Glob Public Health. 2022;2(12): e0000893.
Mahendradhata Y, Andayani NLPE, Hasri ET, et al. The capacity of the Indonesian healthcare system to respond to COVID-19. Front Public Health. 2021;9:649819.
Millet CM, Stickler LM, Wang H. Accelerated nursing degree programs: insights into teaching and learning experiences. In: Powers D, editor. ETS research report series, vol. 2012 No. 2. Hoboken: Wiley; 2015. p. 1–32.
AlSaif HI, AlDhayan AZ, Alosaimi MM, et al. Willingness and self-perceived competence of final-year medical students to work as part of the healthcare workforce during the COVID-19 pandemic. Int J Gen Med. 2020;13:653–61.
Victora PC, Castro PMC, Gurzenda S, et al. Estimating the early impact of vaccination against COVID-19 on deaths among elderly people in Brazil: analyses of routinely-collected data on vaccine coverage and mortality. EClinicalMedicine. 2021;38: 101036.
Sharun K, Tiwari R, Yatoo MI, et al. A comprehensive review on pharmacologic agents, immunotherapies and supportive therapeutics for COVID-19. Narra J. 2022;2(3): e92.
Vaksinasi COVID-19 Nasional. Available: https://vaksin.kemkes.go.id/#/vaccines (Accessed 30 December 2022).
Gao M, Piernas C, Astbury NM, et al. Associations between body-mass index and COVID-19 severity in 6·9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 2021;9:350–9.
Acknowledgements
We acknowledge the Ministry of Health of Republic of Indonesia, the National COVID-19 Task Force (Komite Pengendalian COVID-19 dan Pemulihan Ekonomi Nasional), and all health care workers involved in the care for the COVID-19 patients, as well as those involved in the field data collection.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. HS, DP, and NNA were supported by funding from UNDP Indonesia. HS, EP, and IRFE were funded by the Wellcome (UK) Africa Asia Programme Vietnam (106680/Z/14/Z).
Author information
Authors and Affiliations
Contributions
HS was the principal investigator of this study. HS designed the study, did the analysis, and had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. HS, DP, NNA, AIP, AAS, and EP contributed to data collection and verification. LR, DG, and MG supervised the data collection and verification. HS and IRFE drafted the paper. All authors critically revised the manuscript for important intellectual content and all authors gave final approval for the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was a secondary analysis of aggregated routine surveillance data collected by COVID-19 control program, with district as the analysis unit. Use of the data, which was aggregated, and at the population level is permitted by the Indonesian Ministry of Health under Regulation Number 45 (2014), Article 3, paragraphs 1 and 2. Given the study design and the use of aggregated data, no ethical approval was considered necessary.
Consent for publication
Not applicable.
Competing of interests
We declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Surendra, H., Paramita, D., Arista, N.N. et al. Geographical variations and district-level factors associated with COVID-19 mortality in Indonesia: a nationwide ecological study. BMC Public Health 23, 103 (2023). https://doi.org/10.1186/s12889-023-15015-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15015-0