Abstract
Purpose of Review
Rotavirus vaccines were first introduced more than a decade ago and have had a tremendous impact on reducing the number of hospitalizations and deaths due to rotavirus-associated diarrhea. This review will discuss current rotavirus vaccines, post-licensure surveillance, progress in non-replicating vaccine development, and why continued research is important for understanding a virus that remains a globally leading cause of death due to diarrhea.
Recent Findings
Research advances have enhanced our understanding of how vaccines induce protection against subsequent severe disease, how the virus replicates and spreads in the face of the host immune system, and basic mechanisms governing the viral life cycle.
Summary
Much remains to be learned about how to improve vaccine success, what the molecular determinants of host range and virulence are, and what the interactions of the virus with the host are that drive its replicative success, among many other important questions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotavirus was first identified as a cause of severe endemic diarrhea in children by Ruth Bishop and colleagues in 1973 [1]. Nearly 25 years later, the first vaccine against rotavirus, RotaShield™, was approved and licensed by the FDA. Concerns over an increased incidence of intussusception led to the withdrawal of the RotaShield vaccine less than a year after its introduction [2]. Decades of research and clinical trials suffered a major setback with the vaccine withdrawal, and it took nearly another 10 years before the release of the Rotarix™ (RV1, GSK Biologics, Rixensart, Belgium) and RotaTeq™ (RV5, Merck and Co, Westpoint, Pennsylvania) vaccines. The RotaTeq and Rotarix vaccines are commercially available worldwide and have been recommended for inclusion in all national immunization programs by the World Health Organization [3]. More than 80 countries have included these two vaccines in their national vaccine program. In addition, other live-attenuated vaccines have been or are being developed, including RotaVac (India), Rotavin-MI (Vietnam), Lanzhou Lamb (China), a bovine UK strain reassortant vaccine (USA, India, and Brazil), and RV3BB (Australia).
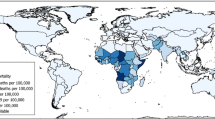
The use of vaccines has resulted in impressive reductions in the incidence of rotavirus-associated diarrhea [4]. Landmark studies estimated the number of worldwide deaths per year associated with rotavirus to be 873,000 in 1985 [5], 453,000 in 2008 [6], and 215,000 in 2013 [7]. Although vaccine efficacy ranges from 84 to 98% in high-income settings, it is below 60% in many resource-poor settings where the majority of deaths due to rotavirus-associated disease occur [8,9,10,11,12]. Continued research to improve our understanding of rotavirus replication, genetics, and pathogenesis will not only inform the design of improved vaccines in the future, it will also enhance our general knowledge of cell biology, the immune response, and vaccinology.
Overview of Rotaviruses
Rotaviruses are currently classified into eight different species, Rotavirus A-H, with two additional proposed species, Rotavirus I-J [13,14,15,16,17]. Of these species, Rotavirus A (herein referred to as “rotavirus”) is responsible for the vast majority of infections of humans but also infects numerous mammalian and avian host species [18]. As a member of the family Reoviridae, the rotavirus genome consists of 11 segments of double-stranded RNA surrounded by three layers of structural proteins that form a non-enveloped icosahedral particle. The outermost layer is comprised of two viral proteins, VP4 and VP7, which are the principal targets of the neutralizing antibody response [18]. The main rotavirus classification system is based on the serotypes of VP7 and VP4 (termed G- and P-types, respectively) but has since been expanded to include genotyping of all 11 genome segments [19]. At least 35 G-types and 50 P-types have been identified, but new genotypes continue to be discovered (https://rega.kuleuven.be/cev/viralmetagenomics/virus-classification/rcwg) [14]. In spite of the large number of genotypes, only six G-types (G1, G2, G3, G4, G9, and G12) and three P-types (P[4], P[6], and P[8]) are commonly associated with human rotavirus illness [20].
The segmented genome of rotavirus lends itself to reassortment, whereby segments from two or more viruses can mix in co-infected cells and be packaged into nascent virions. Reassortment drives genetic diversity among rotavirus strains, but mutations introduced during replication by the error-prone polymerase are also an important source of genetic diversity. Reassortment has been important in the generation of rotavirus vaccines, allowing for the combination of an attenuated animal strain of rotavirus with the outer capsid proteins of commonly circulating human strains [21]. Reassortment has also been a valuable laboratory tool, widely used to map phenotypic traits to individual gene products and serving as the basis for early approaches to reverse genetics systems [22, 23].
Rotaviruses infect mature epithelial cells at the tips of the small intestinal villi (enterocytes). Virus-mediated destruction of enterocytes results in the blunting of intestinal villi leading to malabsorption, although there are several additional factors involved in the pathogenesis of rotavirus (reviewed in [24]). Vomiting and diarrhea caused by rotavirus infection lasts approximately 7 to 10 days, which is of significantly longer duration than typically occurs with other viruses that cause gastroenteritis, and the resulting dehydration can be fatal. Rehydration is used to treat infected patients, but vaccination is the best method for prevention of severe diarrheal disease.
An infection with rotavirus does not generate sterilizing immunity; therefore, the goal of vaccination is a reduction or elimination of severe diarrhea. Antibodies have been shown to provide protection against a subsequent rotavirus challenge, but CD8+ T cells are important for resolution of a rotavirus infection [25,26,27]. Rotavirus-specific IgA in the intestinal fluid is likely the best predictor of protection against subsequent severe disease, but measurements of neutralizing antibodies from the duodenum are impractical [28]. Fecal IgA has been assessed in a few studies and appears to correlate well with levels of intestinal IgA [28]. Measurements of serum IgA and serum IgG have been correlated with protection, but technical challenges with measurement errors, time of sampling, and sampling design introduce variability among published studies [29]. Furthermore, there is no agreement on the concentration of antibody that predicts vaccine efficacy; to improve new vaccine development and clinical trials, the correlates of protection are in need of better definition. Additional basic studies to identify other correlates of protection would serve to improve our knowledge of the mechanism of immune protection against rotavirus.
Vaccine Efficacy in Developed Countries
Prior to the development of vaccines to protect against rotavirus illness, nearly all children experienced a rotavirus infection at least once. Severe symptoms of gastroenteritis, including diarrhea and/or vomiting, are most common during the first infection with rotavirus [30]. Subsequent infections are typically less severe and may be asymptomatic. Protection against moderate and severe illness is nearly 100% after two infections with rotavirus [30]. Thus, efforts to develop a vaccine for rotavirus have primarily focused on an orally administered, live-attenuated rotavirus that would mimic a natural infection without causing disease.
The earliest stages of rotavirus vaccine development used a “Jennerian” approach in which a related, live-attenuated virus from a non-human-animal host was used as an immunogen to induce protection against severe disease (reviewed in [21]). However, because a number of different rotavirus serotypes/genotypes circulate globally, a “modified Jennerian” approach was used to achieve broader antigenic coverage. Animal rotavirus isolates that had undergone safety testing were used to generate human-animal rotavirus reassortants that incorporated the VP7 outer capsid protein from different human rotavirus serotypes into the background animal virus isolate [21]. Multivalent vaccines were thought to be necessary to ensure adequate protection against multiple circulating viral serotypes. Post-licensure monitoring has demonstrated that cross-protection occurs against strains not present in the vaccines, although cross-protection is not always complete against severe disease [31].
The first rotavirus vaccine licensed for use was RotaShield, a tetravalent combination of rhesus-human rotavirus reassortants [21]. This vaccine was withdrawn from the US market in 1999, less than 1 year after its implementation, due to an association with approximately 1 excess case of intussusception per 10,000 vaccine recipients [32, 33]. Intussusception is an intestinal obstruction caused by the telescoping of one part of the intestine into an adjacent part of the intestine. The withdrawal of RotaShield occurred before any post-licensure data of the benefit of vaccination was available, prompting a lengthy and important debate about the risk-benefit ratio of rotavirus vaccines. Because of the association with intussusception, large-scale clinical trials were necessary to evaluate the risk of intussusception with RotaTeq and Rotarix vaccines. RotaTeq is a pentavalent combination of bovine-human reassortants, whereas Rotarix is a monovalent vaccine derived from a human virus isolate [34]. Clinical trials with RotaTeq and Rotarix in Latin America, the USA, and Europe demonstrated 85–98% vaccine efficacy against severe rotavirus gastroenteritis [35, 36]. Since vaccine implementation in the USA in 2006, hospitalizations due to rotavirus have declined by 60–83% in children under 5 years of age, and hospitalizations due to all causes of diarrhea have decreased by 29–50% when compared to pre-vaccine years [37,38,39]. In addition, there is evidence for a reduction in rotavirus transmission in children who are too old to receive the vaccine and adults, suggesting that herd immunity has an impact on reducing cases of diarrhea [40,41,42]. Since vaccine introduction in the USA, the seasonality of rotavirus begins later in the year, is of shorter duration, and the magnitude is diminished [43, 44].
Vaccine Efficacy in Resource-Poor Countries
Lower vaccine efficacy has been documented in many resource-poor countries. Trials using RotaTeq conducted in Ghana, Kenya, and Mali demonstrated an efficacy of 64% in the first year of life [10], and studies in Vietnam and Bangladesh demonstrated an efficacy of 51% [11]. Trials using Rotarix conducted in South Africa and Malawi found the vaccine to be 40–64% effective [12, 45, 46•]. The reasons for lower vaccine efficacy are unclear, and a significant research effort is warranted given that the majority of lives lost due to rotavirus occur in these locations.
The immune response to other orally administered vaccines, such as polio and cholera, has also been lower and less consistent in resource-poor locations [47,48,49]. Nutritional deficiency may account for decreased vaccine efficacy, and the lack of specific nutritional factors, including zinc, vitamin A, and vitamin D, could play a role in reduced vaccine uptake [50]. The presence of pre-existing maternal antibodies may have a neutralizing effect on orally administered vaccines [51, 52]. Although breastfeeding is a possible source of maternal antibodies [53], a number of studies have demonstrated that withholding breastfeeding prior to rotavirus vaccine administration does not impact seroconversion among infants when compared to infants with unlimited breastfeeding [54,55,56].
In low-resource countries, there is greater genetic diversity and emergence of new and unusual rotavirus strains that may also account for some of the reduction in vaccine efficacy [57, 58]. Given that cross-protection has been shown to occur, greater strain variation may only be partly responsible for reduced vaccine efficacy [31].
Colonization by commensal microbiota early in life is important in the immunological development of the mucosal immune response [59]. The role of the microbiota in oral vaccine uptake is not well understood, but there appears to be a correlation with rotavirus vaccine immunogenicity and the composition of the microbiota [60]. Recently, a study examined the impact of probiotic supplementation on rotavirus vaccination, but no significant improvement on vaccine immunogenicity was observed [61]. Combining probiotics with zinc supplementation offered a modest improvement, but further investigation will be necessary. The failure of oral vaccines in the developing world is most likely to be attributed to environmental enteropathy, a subclinical condition caused by constant fecal-oral contamination resulting in intestinal inflammation [62]. Chronic exposure to fecal pathogens is thought to cause inflammation and structural changes in the small intestine, which may in turn cause impairment of intestinal absorptive and immunologic functions. Concomitant infections of the enteric tract may also directly interfere with the uptake of live, oral vaccines. Because environmental enteropathy may be the main cause of reduced vaccine efficacy for diseases other than rotavirus, there should be a significant research push to understand this condition.
Rotavirus is the leading pathogen detected in diarrheal samples from children in their first year of life, and the incidence of rotavirus among infants is more than twice that observed for any other pathogen [63]. The introduction of rotavirus vaccines, even with lower efficacy, has a tremendous impact in low-resource settings because of the high disease burden. In a setting such as Mali, with a birth cohort of 758,000 in 2016, a vaccine with 60% efficacy would prevent approximately 31,500 cases of life-threatening rotavirus infection during the first year of life [64]. Yet, improving rotavirus vaccine efficacy in the countries that suffer from the greatest burden of disease will have the largest impact on reducing the number of deaths and easing the burden on health care facilities.
Research efforts need to be aimed at understanding the reasons behind the low vaccine efficacy in resource-poor locations so that improvements can be made to vaccine performance in these settings. Post-licensure monitoring has been ongoing in many countries that have implemented rotavirus vaccine programs. Such monitoring is, and will continue to be, important to monitor fecal shedding of vaccine strains, to measure waning population immunity, to identify possible shifts in circulating strains of virus over time, and to track intussusception associated with vaccination. Changes to vaccine effectiveness over time may accelerate improvements to current vaccines or the development of new vaccines. Ideally, a vaccine in which only a single dose is necessary to effectively prevent severe disease would have added impact in that it could capture a larger population of susceptible individuals. Additional live-attenuated rotavirus vaccine candidates continue to be developed, but the field must first gain a more complete understanding of the reasons behind reduced oral vaccine uptake.
Development of Non-replicating Vaccine Candidates
Unfortunately, there are contraindications for use of the currently licensed rotavirus vaccines, including a history of severe allergic reaction after a previous dose of rotavirus vaccine, diagnosis with severe combined immunodeficiency (SCID), or a history of intussusception [34]. Children that fall within one of these categories may benefit from the development of a non-replicating vaccine. Rotavirus vaccine administration is also age-restricted due to the enhanced risk of intussusception in children who receive the first dose of vaccine after 15 weeks of age [65]. Post-marketing surveillance of the rotavirus vaccines has detected a slight increase in the risk of intussusception (1–6 excess cases per 100,000 vaccine recipients) following oral administration of RotaTeq and Rotarix at 6–12 weeks of age [66, 67]. Although the overall benefits of vaccination greatly outweigh this risk, it may be reduced or eliminated with a non-replicating vaccine.
Understanding the neutralizing antibody epitopes on viral proteins has long been an important consideration in vaccine development, especially for non-replicating vaccines. Non-replicating subunit vaccines typically utilize the VP4 and VP7 outer capsid proteins of the virus, as these proteins are key targets of the antibody response [68]. During rotavirus infection, the VP4 protein is cleaved by host proteases into VP5* and VP8* [69]. The development of a VP8* subunit protein vaccine fused to the P2 epitope of tetanus toxin has been ongoing [70, 71•]. A recent phase 1/2 study of this vaccine in infants has shown that the vaccine is immunogenic and may reduce viral shedding in a subsequent infection [71•]. However, an absence of heterotypic immunity suggests that subunit vaccines will need to incorporate different rotavirus serotypes to provide broader protection. Defining the molecular basis for heterotypic immunity recently took a dramatic leap forward in a study of intestinal B cells from adults that demonstrated heterotypic immunoglobulins against rotavirus were primarily directed at the stalk region of VP4 (VP5*) [72•]. Heterotypic protection was also directed to the cell-binding region of VP4 (VP8*) and the VP7 outer shell protein, but to a lesser extent. The immunoglobulins directed against VP7 and VP8* tended to be homotypic or non-neutralizing, suggesting that the stalk region of VP4 represents a useful target for a more broadly effective rotavirus vaccine [72•].
The VP6 protein forms the intermediate layer of the rotavirus capsid and is highly conserved among rotaviruses. VP6 has been explored as another possible subunit vaccine candidate, in part because when expressed in vitro, VP6 can assemble as nanotubes, which offers some natural adjuvant properties [73, 74]. During a natural rotavirus infection, a significant antibody response is mounted against VP6 [75]. Murine VP6-specific antibodies have been shown to protect mice from rotavirus infection, and murine anti-VP6 antibodies can inhibit viral replication inside polarized epithelial cells at early stages of infection [76, 77]. Although anti-rotavirus antibodies appear to be the primary effectors of protection after immunization with live-attenuated vaccines, CD4+ T cells were found to reduce viral shedding in mice after immunization with recombinant VP6 [78]. Therefore, there seems to be some difference in the protective response to rotavirus immunization depending on the route of administration and whether the vaccine is live-attenuated or non-replicating.
Virus-like particles (VLPs) are another potential non-replicating rotavirus vaccine candidate. Rotavirus VLPs have been produced by coexpressing viral structural proteins using baculovirus expression systems [79]. VLP vaccines have been tested for immunogenicity in animal models but have yet to undergo testing in humans [80,81,82]. One challenge facing the non-replicating vaccine candidates undergoing development is that they will all need to account for the variety of circulating virus strains. The use of non-replicating rotavirus vaccines could offer the benefit of being formulated with other antigens, such as from norovirus, to offer protection from multiple pathogens [83]. Research on subunit and VLP vaccines for rotavirus is only in the earliest stages; thus, further work is essential to develop formulations that are safe, highly immunogenic, and offer adequate cross-protection against multiple circulating serotypes. In addition, formulation of better adjuvants would benefit vaccine development for many pathogens, including rotavirus, and are needed to improve responses in the immature immune systems of infants. However, the perceived costs associated with bringing a new vaccine to the market has slowed the development of non-replicating vaccine candidates.
Modifying Viral Determinants of Virulence or Pathogenesis to Improve Vaccines
One possible way to improve rotavirus vaccines is to modify genes that are responsible for virulence in order to attenuate a human strain. However, there is conflicting information on the genes and their products that are responsible for virulence. In some models, the VP3, VP4, VP7, and NSP4 have been shown to be responsible for virulence [84, 85]. The ways in which virulence is defined and measured varies greatly between studies. On the other hand, host range restriction, where viral strains isolated from one host species tend to have reduced replication capacity and virulence in heterologous host species, can specifically be measured by a decrease in viral replication of a heterologous virus compared to a homologous virus in the small intestine. Recently, strong evidence has been provided to support the attachment protein VP4 and the interferon antagonist protein NSP1 as important mediators of host range restriction [86]. The interferon system also appears to have an impact on limiting intestinal viral replication of heterologous rotavirus infections and may be a factor in determining the host range of virus strains [87]. Although our understanding of host range restriction is currently limited, determining the molecular mechanisms of how viruses isolated from hosts other than humans fail to cause severe disease is necessary to improve rotavirus vaccines but also to applying the successes of other vaccines that rely on host restriction (such as smallpox) to vaccine development for other viral infections.
The molecular basis for interferon-mediated inhibition of rotavirus is not understood, but it is clearly important for combating infection since rotavirus is known to encode more than one antagonist of the innate immune response [88]. The nonstructural protein NSP1 inhibits the innate immune response by preventing the induction of type I interferon. NSP1 has primarily been described to induce the proteasomal degradation of several cellular proteins required for initiating the interferon response, and the targets of degradation appear to differ depending on whether the rotavirus naturally infects a human or a different animal host [89,90,91,92]. The molecular details surrounding how NSP1 induces protein degradation are somewhat controversial, with some data to support NSP1 functioning as an E3 ubiquitin ligase, while other data suggesting it usurps host cullin-RING ubiquitin ligase complexes [93•, 94]. If NSP1 is involved in promoting replication in specific host species, then the mechanism by which NSP1 inhibits the interferon response must be clearly defined in order to be a useful target for modification in improved vaccines. Another viral protein that has been shown to inhibit the innate immune response downstream of interferon production is the capping protein VP3. VP3 has phosphodiesterase activity that cleaves interferon-inducible 2′,5′-oligoadenylates, thereby preventing activation of RNase L, which has antiviral activity [95]. Although it might be assumed that RNase L directly inhibits rotavirus replication, the effect of this interferon-stimulated gene product on rotavirus has not been examined. There is a general lack of knowledge surrounding the innate immune effectors that directly inhibit rotavirus entry, replication, and packaging. Investigative efforts into the interferon-stimulated genes that control steps in the rotavirus life cycle may help to identify other ways in which rotavirus infections can be controlled and will also provide insight into how these important cellular pathways limit viral infections. Furthermore, delineating the mechanisms for viral antagonism of immune responses is largely credited with providing our understanding of how the innate immune system functions and therefore should continue as an important area of research of many viruses.
The innate immune system is important in protecting infants from bacterial and viral infections because it provides a rapid, early defense against invading pathogens. Infants do not have a fully developed adaptive immune response since they have not yet had extensive exposure to foreign antigens [96]. Some in vitro and in vivo studies have shown that innate immune effectors that help to defend against rotavirus infection may play a role in the age restriction of rotavirus infections, but there is still much to learn. Studies have implicated Toll-like receptor 3, which is a double-stranded RNA sensor of the innate immune response, in the age-related susceptibility of rotavirus infections [97]. Mice lacking type III interferon receptors have also been shown to exert less control over rotavirus infections, suggesting type III interferon has an important role in restricting rotavirus, and other enteric virus, infections [98, 99]. Under some conditions, intestinal epithelial cells of adult mice were found to be unresponsive to type I interferon [98], but follow-up studies suggest that there may be an age-related change in the responsiveness of intestinal epithelial cells to type I interferon, from a robust response in neonates to one that diminishes as the mouse matures [100•]. Dissecting the ways in which the type I and type III interferon systems restrict enteric infections such as rotavirus will likely provide important insight into the age- and host-restricted replication of many important pathogens, but these important research questions will require much additional study.
Conclusion
Why do we need to continue research on rotaviruses? The diminished vaccine efficacy in resource-poor countries and the exclusion of certain patients from rotavirus vaccination highlights a need for improvements to vaccine design. In order to make the most rational improvements possible, there must be a more thorough knowledge base surrounding the innate and adaptive immune response to rotavirus, the viral targets that could be modified to improve vaccines, and the mechanisms underlying how targetable viral proteins function. Vaccine effectiveness must also be continually monitored to determine if commonly circulating strains of rotavirus will change over time, or if a newly pathogenic rotavirus emerges through natural variation. Ideally, research will lead to the development of a rapid response vaccine that could quickly be adapted to hypothetical future outbreak strains of the virus. But there are many additional questions about rotavirus that deserve to be addressed, not only for their value in determining how rotavirus replicates and interacts with its host but also because they drive a greater understanding of immunology, molecular virology, and cell biology as a whole. Do histo-blood group antigens determine susceptibility to rotavirus infection as has been proposed for noroviruses? How are the virally induced centers of replication (viroplasms) organized, and are they potential drug targets? How does a virus with a segmented genome orchestrate the timing and packaging of the correct number of genome segments? By what mechanisms does interferon inhibit rotavirus replication, and is interferon a crucial factor in host range restriction? The recent development of an entirely plasmid-based reverse genetics system is a long-awaited breakthrough that offers many new opportunities to study rotavirus biology and greatly impacts the ability to easily insert specific mutations or gene segments into the virus in the creation of new live-attenuated vaccine candidates [101•].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bishop RF, Davidson GP, Holmes IH, Ruck BJ. Virus particles in epithelial cells of duodenal mucosa from children with acute non-bacterial gastroenteritis. Lancet. 1973;2(7841):1281–3.
Centers for Disease C, Prevention. Withdrawal of rotavirus vaccine recommendation. MMWR Morb Mortal Wkly Rep. 1999;48(43):1007.
Rotavirus vaccines WHO position paper: January 2013—Recommendations. Vaccine. 2013;31(52):6170–1. doi: https://doi.org/10.1016/j.vaccine.2013.05.037.
Burnett E, Jonesteller CL, Tate JE, Yen C, Parashar UD. Global impact of rotavirus vaccination on childhood hospitalizations and mortality from diarrhea. J Infect Dis. 2017;215(11):1666–72. https://doi.org/10.1093/infdis/jix186.
Medicine Io. The prospects of immunizing against rotavirus1986.
Tate JE, Burton AH, Boschi-Pinto C, Steele AD, Duque J, Parashar UD, et al. 2008 estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(2):136–41. https://doi.org/10.1016/S1473-3099(11)70253-5.
Tate JE, Burton AH, Boschi-Pinto C, Parashar UD, World Health Organization-Coordinated Global Rotavirus Surveillance N. Global, regional, and National Estimates of rotavirus mortality in children <5 years of age, 2000-2013. Clin Infect Dis. 2016;62(Suppl 2):S96–S105. https://doi.org/10.1093/cid/civ1013.
Boom JA, Tate JE, Sahni LC, Rench MA, Hull JJ, Gentsch JR, et al. Effectiveness of pentavalent rotavirus vaccine in a large urban population in the United States. Pediatrics. 2010;125(2):e199–207. https://doi.org/10.1542/peds.2009-1021.
Vesikari T, Karvonen A, Prymula R, Schuster V, Tejedor JC, Cohen R, et al. Efficacy of human rotavirus vaccine against rotavirus gastroenteritis during the first 2 years of life in European infants: randomised, double-blind controlled study. Lancet. 2007;370(9601):1757–63. https://doi.org/10.1016/S0140-6736(07)61744-9.
Armah GE, Sow SO, Breiman RF, Dallas MJ, Tapia MD, Feikin DR, et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in sub-Saharan Africa: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;376(9741):606–14. https://doi.org/10.1016/S0140-6736(10)60889-6.
Zaman K, Dang DA, Victor JC, Shin S, Yunus M, Dallas MJ, et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in Asia: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;376(9741):615–23. https://doi.org/10.1016/S0140-6736(10)60755-6.
Madhi SA, Cunliffe NA, Steele D, Witte D, Kirsten M, Louw C, et al. Effect of human rotavirus vaccine on severe diarrhea in African infants. N Engl J Med. 2010;362(4):289–98. https://doi.org/10.1056/NEJMoa0904797.
Adams MJ, Lefkowitz EJ, King AMQ, Harrach B, Harrison RL, Knowles NJ, et al. Changes to taxonomy and the international code of virus classification and nomenclature ratified by the international committee on taxonomy of viruses (2017). Arch Virol. 2017;162(8):2505–38. https://doi.org/10.1007/s00705-017-3358-5.
Matthijnssens J, Ciarlet M, McDonald SM, Attoui H, Banyai K, Brister JR, et al. Uniformity of rotavirus strain nomenclature proposed by the rotavirus classification working group (RCWG). Arch Virol. 2011;156(8):1397–413. https://doi.org/10.1007/s00705-011-1006-z.
Matthijnssens J, Otto PH, Ciarlet M, Desselberger U, Van Ranst M, Johne R. VP6-sequence-based cutoff values as a criterion for rotavirus species demarcation. Arch Virol. 2012;157(6):1177–82. https://doi.org/10.1007/s00705-012-1273-3.
Mihalov-Kovacs E, Gellert A, Marton S, Farkas SL, Feher E, Oldal M, et al. Candidate new rotavirus species in sheltered dogs, Hungary. Emerg Infect Dis. 2015;21(4):660–3. https://doi.org/10.3201/eid2104.141370.
Banyai K, Kemenesi G, Budinski I, Foldes F, Zana B, Marton S, et al. Candidate new rotavirus species in Schreiber’s bats, Serbia. Infect Genet Evol. 2017;48:19–26. https://doi.org/10.1016/j.meegid.2016.12.002.
Estes MK, Greenberg HB. Fields virology. Rotaviruses. Philadelphia: Lippincott Williams & Wilkins; 2013.
Matthijnssens J, Ciarlet M, Rahman M, Attoui H, Banyai K, Estes MK, et al. Recommendations for the classification of group A rotaviruses using all 11 genomic RNA segments. Arch Virol. 2008;153(8):1621–9. https://doi.org/10.1007/s00705-008-0155-1.
Santos N, Hoshino Y. Global distribution of rotavirus serotypes/genotypes and its implication for the development and implementation of an effective rotavirus vaccine. Rev Med Virol. 2005;15(1):29–56. https://doi.org/10.1002/rmv.448.
Hoshino Y, Kapikian AZ. Rotavirus vaccine development for the prevention of severe diarrhea in infants and young children. Trends Microbiol. 1994;2(7):242–9. https://doi.org/10.1016/0966-842X(94)90629-7.
Komoto S, Sasaki J, Taniguchi K. Reverse genetics system for introduction of site-specific mutations into the double-stranded RNA genome of infectious rotavirus. Proc Natl Acad Sci U S A. 2006;103(12):4646–51. https://doi.org/10.1073/pnas.0509385103.
Trask SD, Taraporewala ZF, Boehme KW, Dermody TS, Patton JT. Dual selection mechanisms drive efficient single-gene reverse genetics for rotavirus. Proc Natl Acad Sci U S A. 2010;107(43):18652–7. https://doi.org/10.1073/pnas.1011948107.
Greenberg HB, Estes MK. Rotaviruses: from pathogenesis to vaccination. Gastroenterology. 2009;136(6):1939–51. https://doi.org/10.1053/j.gastro.2009.02.076.
Franco MA, Greenberg HB. Role of B cells and cytotoxic T lymphocytes in clearance of and immunity to rotavirus infection in mice. J Virol. 1995;69(12):7800–6.
McNeal MM, Barone KS, Rae MN, Ward RL. Effector functions of antibody and CD8+ cells in resolution of rotavirus infection and protection against reinfection in mice. Virology. 1995;214(2):387–97. https://doi.org/10.1006/viro.1995.0048.
Franco MA, Tin C, Greenberg HB. CD8+ T cells can mediate almost complete short-term and partial long-term immunity to rotavirus in mice. J Virol. 1997;71(5):4165–70.
Grimwood K, Lund JC, Coulson BS, Hudson IL, Bishop RF, Barnes GL. Comparison of serum and mucosal antibody responses following severe acute rotavirus gastroenteritis in young children. J Clin Microbiol. 1988;26(4):732–8.
Angel J, Steele AD, Franco MA. Correlates of protection for rotavirus vaccines: possible alternative trial endpoints, opportunities, and challenges. Hum Vaccin Immunother. 2014;10(12):3659–71. https://doi.org/10.4161/hv.34361.
Velazquez FR, Matson DO, Calva JJ, Guerrero L, Morrow AL, Carter-Campbell S, et al. Rotavirus infection in infants as protection against subsequent infections. N Engl J Med. 1996;335(14):1022–8. https://doi.org/10.1056/NEJM199610033351404.
Leshem E, Lopman B, Glass R, Gentsch J, Banyai K, Parashar U, et al. Distribution of rotavirus strains and strain-specific effectiveness of the rotavirus vaccine after its introduction: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(9):847–56. https://doi.org/10.1016/S1473-3099(14)70832-1.
Centers for Disease C, Prevention. Intussusception among recipients of rotavirus vaccine—United States, 1998-1999. MMWR Morb Mortal Wkly Rep. 1999;48(27):577–81.
Murphy TV, Gargiullo PM, Massoudi MS, Nelson DB, Jumaan AO, Okoro CA, et al. Intussusception among infants given an oral rotavirus vaccine. N Engl J Med. 2001;344(8):564–72. https://doi.org/10.1056/NEJM200102223440804.
Lopman BA, Payne DC, Tate JE, Patel MM, Cortese MM, Parashar UD. Post-licensure experience with rotavirus vaccination in high and middle income countries; 2006 to 2011. Curr Opin Virol. 2012;2(4):434–42. https://doi.org/10.1016/j.coviro.2012.05.002.
Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med. 2006;354(1):23–33. https://doi.org/10.1056/NEJMoa052664.
Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med. 2006;354(1):11–22. https://doi.org/10.1056/NEJMoa052434.
Yen C, Tate JE, Wenk JD, Harris JM 2nd, Parashar UD. Diarrhea-associated hospitalizations among US children over 2 rotavirus seasons after vaccine introduction. Pediatrics. 2011;127(1):e9–e15. https://doi.org/10.1542/peds.2010-1393.
Cortese MM, Tate JE, Simonsen L, Edelman L, Parashar UD. Reduction in gastroenteritis in United States children and correlation with early rotavirus vaccine uptake from national medical claims databases. Pediatr Infect Dis J. 2010;29(6):489–94. https://doi.org/10.1097/INF.0b013e3181d95b53.
Cortes JE, Curns AT, Tate JE, Cortese MM, Patel MM, Zhou F, et al. Rotavirus vaccine and health care utilization for diarrhea in U.S. children. N Engl J Med. 2011;365(12):1108–17. https://doi.org/10.1056/NEJMoa1000446.
Lopman BA, Curns AT, Yen C, Parashar UD. Infant rotavirus vaccination may provide indirect protection to older children and adults in the United States. J Infect Dis. 2011;204(7):980–6. https://doi.org/10.1093/infdis/jir492.
Gastanaduy PA, Curns AT, Parashar UD, Lopman BA. Gastroenteritis hospitalizations in older children and adults in the United States before and after implementation of infant rotavirus vaccination. JAMA. 2013;310(8):851–3. https://doi.org/10.1001/jama.2013.170800.
Anderson EJ, Shippee DB, Weinrobe MH, Davila MD, Katz BZ, Reddy S, et al. Indirect protection of adults from rotavirus by pediatric rotavirus vaccination. Clin Infect Dis. 2013;56(6):755–60. https://doi.org/10.1093/cid/cis1010.
Tate JE, Haynes A, Payne DC, Cortese MM, Lopman BA, Patel MM, et al. Trends in national rotavirus activity before and after introduction of rotavirus vaccine into the national immunization program in the United States, 2000 to 2012. Pediatr Infect Dis J. 2013;32(7):741–4. https://doi.org/10.1097/INF.0b013e31828d639c.
Aliabadi N, Tate JE, Haynes AK, Parashar UD. Centers for disease C, prevention. Sustained decrease in laboratory detection of rotavirus after implementation of routine vaccination—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2015;64(13):337–42.
Groome MJ, Page N, Cortese MM, Moyes J, Zar HJ, Kapongo CN, et al. Effectiveness of monovalent human rotavirus vaccine against admission to hospital for acute rotavirus diarrhoea in south African children: a case-control study. Lancet Infect Dis. 2014;14(11):1096–104. https://doi.org/10.1016/S1473-3099(14)70940-5.
• Bar-Zeev N, Kapanda L, Tate JE, Jere KC, Iturriza-Gomara M, Nakagomi O, et al. Effectiveness of a monovalent rotavirus vaccine in infants in Malawi after programmatic roll-out: an observational and case-control study. Lancet Infect Dis. 2015;15(4):422–8. https://doi.org/10.1016/S1473-3099(14)71060-6. This study showed that the administration of Rotarix reduced rotavirus-associated hospital admissions by 54% among infants, but not older children, in a resource-poor setting.
Su-Arehawaratana P, Singharaj P, Taylor DN, Hoge C, Trofa A, Kuvanont K, et al. Safety and immunogenicity of different immunization regimens of CVD 103-HgR live oral cholera vaccine in soldiers and civilians in Thailand. J Infect Dis. 1992;165(6):1042–8. https://doi.org/10.1093/infdis/165.6.1042.
Patriarca PA, Wright PF, John TJ. Factors affecting the immunogenicity of oral poliovirus vaccine in developing countries: review. Rev Infect Dis. 1991;13(5):926–39. https://doi.org/10.1093/clinids/13.5.926.
Suharyono, Simanjuntak C, Witham N, Punjabi N, Heppner DG, Losonsky G, et al. Safety and immunogenicity of single-dose live oral cholera vaccine CVD 103-HgR in 5-9-year-old Indonesian children. Lancet. 1992;340(8821):689–94. https://doi.org/10.1016/0140-6736(92)92231-4.
Babji S, Kang G. Rotavirus vaccination in developing countries. Curr Opin Virol. 2012;2(4):443–8. https://doi.org/10.1016/j.coviro.2012.05.005.
Chan J, Nirwati H, Triasih R, Bogdanovic-Sakran N, Soenarto Y, Hakimi M, et al. Maternal antibodies to rotavirus: could they interfere with live rotavirus vaccines in developing countries? Vaccine. 2011;29(6):1242–7. https://doi.org/10.1016/j.vaccine.2010.11.087.
Appaiahgari MB, Glass R, Singh S, Taneja S, Rongsen-Chandola T, Bhandari N, et al. Transplacental rotavirus IgG interferes with immune response to live oral rotavirus vaccine ORV-116E in Indian infants. Vaccine. 2014;32(6):651–6. https://doi.org/10.1016/j.vaccine.2013.12.017.
Moon SS, Wang Y, Shane AL, Nguyen T, Ray P, Dennehy P, et al. Inhibitory effect of breast milk on infectivity of live oral rotavirus vaccines. Pediatr Infect Dis J. 2010;29(10):919–23. https://doi.org/10.1097/INF.0b013e3181e232ea.
Groome MJ, Moon SS, Velasquez D, Jones S, Koen A, van Niekerk N, et al. Effect of breastfeeding on immunogenicity of oral live-attenuated human rotavirus vaccine: a randomized trial in HIV-uninfected infants in Soweto, South Africa. Bull World Health Organ. 2014;92(4):238–45. https://doi.org/10.2471/BLT.13.128066.
Rongsen-Chandola T, Strand TA, Goyal N, Flem E, Rathore SS, Arya A, et al. Effect of withholding breastfeeding on the immune response to a live oral rotavirus vaccine in north Indian infants. Vaccine. 2014;32(Suppl 1):A134–9. https://doi.org/10.1016/j.vaccine.2014.04.078.
Ali A, Kazi AM, Cortese MM, Fleming JA, Moon S, Parashar UD, et al. Impact of withholding breastfeeding at the time of vaccination on the immunogenicity of oral rotavirus vaccine—a randomized trial. PLoS One. 2015;10(6):e0127622. https://doi.org/10.1371/journal.pone.0127622.
Todd S, Page NA, Duncan Steele A, Peenze I, Cunliffe NA. Rotavirus strain types circulating in Africa: review of studies published during 1997-2006. J Infect Dis. 2010;202(Suppl):S34–42. https://doi.org/10.1086/653555.
Miles MG, Lewis KD, Kang G, Parashar UD, Steele AD. A systematic review of rotavirus strain diversity in India, Bangladesh, and Pakistan. Vaccine. 2012;30(Suppl 1):A131–9. https://doi.org/10.1016/j.vaccine.2011.10.002.
Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol. 2009;9(5):313–23. https://doi.org/10.1038/nri2515.
Harris VC, Armah G, Fuentes S, Korpela KE, Parashar U, Victor JC, et al. Significant correlation between the infant gut microbiome and rotavirus vaccine response in rural Ghana. J Infect Dis. 2017;215(1):34–41. https://doi.org/10.1093/infdis/jiw518.
Lazarus RP, John J, Shanmugasundaram E, Rajan AK, Thiagarajan S, Giri S, et al. The effect of probiotics and zinc supplementation on the immune response to oral rotavirus vaccine: a randomized, factorial design, placebo-controlled study among Indian infants. Vaccine. 2017;36(2):273–9. https://doi.org/10.1016/j.vaccine.2017.07.116.
Korpe PS, Petri WA Jr. Environmental enteropathy: critical implications of a poorly understood condition. Trends Mol Med. 2012;18(6):328–36. https://doi.org/10.1016/j.molmed.2012.04.007.
Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the global enteric multicenter study, GEMS): a prospective, case-control study. Lancet. 2013;382(9888):209–22. https://doi.org/10.1016/S0140-6736(13)60844-2.
Kotloff KL. The burden and etiology of diarrheal illness in developing countries. Pediatr Clin N Am. 2017;64(4):799–814. https://doi.org/10.1016/j.pcl.2017.03.006.
Parashar UD, Alexander JP, Glass RI, Advisory Committee on Immunization Practices CfDC, Prevention. Prevention of rotavirus gastroenteritis among infants and children. Recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep. 2006;55(RR-12):1–13.
Yih WK, Lieu TA, Kulldorff M, Martin D, McMahill-Walraven CN, Platt R, et al. Intussusception risk after rotavirus vaccination in U.S. infants. N Engl J Med. 2014;370(6):503–12. https://doi.org/10.1056/NEJMoa1303164.
Weintraub ES, Baggs J, Duffy J, Vellozzi C, Belongia EA, Irving S, et al. Risk of intussusception after monovalent rotavirus vaccination. N Engl J Med. 2014;370(6):513–9. https://doi.org/10.1056/NEJMoa1311738.
Ruggeri FM, Greenberg HB. Antibodies to the trypsin cleavage peptide VP8 neutralize rotavirus by inhibiting binding of virions to target cells in culture. J Virol. 1991;65(5):2211–9.
Crawford SE, Mukherjee SK, Estes MK, Lawton JA, Shaw AL, Ramig RF, et al. Trypsin cleavage stabilizes the rotavirus VP4 spike. J Virol. 2001;75(13):6052–61. https://doi.org/10.1128/JVI.75.13.6052-6061.2001.
Fix AD, Harro C, McNeal M, Dally L, Flores J, Robertson G, et al. Safety and immunogenicity of a parenterally administered rotavirus VP8 subunit vaccine in healthy adults. Vaccine. 2015;33(31):3766–72. https://doi.org/10.1016/j.vaccine.2015.05.024.
• Groome MJ, Koen A, Fix A, Page N, Jose L, Madhi SA, et al. Safety and immunogenicity of a parenteral P2-VP8-P[8] subunit rotavirus vaccine in toddlers and infants in South Africa: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2017;17(8):843–53. https://doi.org/10.1016/S1473-3099(17)30242-6. This study is the first phase 2 human trial of an inactivated rotavirus vaccine and shows that there is potential in non-replicating vaccine strategies.
• Nair N, Newell EW, Vollmers C, Quake SR, Morton JM, Davis MM, et al. High-dimensional immune profiling of total and rotavirus VP6-specific intestinal and circulating B cells by mass cytometry. Mucosal Immunol. 2016;9(1):68–82. https://doi.org/10.1038/mi.2015.36. This study is a detailed investigation of the neutralizing and non-neutralizing intestinal antibodies that develop following rotavirus infection.
Lepault J, Petitpas I, Erk I, Navaza J, Bigot D, Dona M, et al. Structural polymorphism of the major capsid protein of rotavirus. EMBO J. 2001;20(7):1498–507. https://doi.org/10.1093/emboj/20.7.1498.
Rodriguez M, Wood C, Sanchez-Lopez R, Castro-Acosta RM, Ramirez OT, Palomares LA. Understanding internalization of rotavirus VP6 nanotubes by cells: towards a recombinant vaccine. Arch Virol. 2014;159(5):1005–15. https://doi.org/10.1007/s00705-013-1916-z.
Weitkamp JH, Kallewaard N, Kusuhara K, Bures E, Williams JV, LaFleur B, et al. Infant and adult human B cell responses to rotavirus share common immunodominant variable gene repertoires. J Immunol. 2003;171(9):4680–8. https://doi.org/10.4049/jimmunol.171.9.4680.
Burns JW, Siadat-Pajouh M, Krishnaney AA, Greenberg HB. Protective effect of rotavirus VP6-specific IgA monoclonal antibodies that lack neutralizing activity. Science. 1996;272(5258):104–7. https://doi.org/10.1126/science.272.5258.104.
Feng N, Lawton JA, Gilbert J, Kuklin N, Vo P, Prasad BV, et al. Inhibition of rotavirus replication by a non-neutralizing, rotavirus VP6-specific IgA mAb. J Clin Invest. 2002;109(9):1203–13. https://doi.org/10.1172/JCI14397.
McNeal MM, VanCott JL, Choi AH, Basu M, Flint JA, Stone SC, et al. CD4 T cells are the only lymphocytes needed to protect mice against rotavirus shedding after intranasal immunization with a chimeric VP6 protein and the adjuvant LT(R192G). J Virol. 2002;76(2):560–8. https://doi.org/10.1128/JVI.76.2.560-568.2002.
Crawford SE, Labbe M, Cohen J, Burroughs MH, Zhou YJ, Estes MK. Characterization of virus-like particles produced by the expression of rotavirus capsid proteins in insect cells. J Virol. 1994;68(9):5945–52.
Ciarlet M, Crawford SE, Barone C, Bertolotti-Ciarlet A, Ramig RF, Estes MK, et al. Subunit rotavirus vaccine administered parenterally to rabbits induces active protective immunity. J Virol. 1998;72(11):9233–46.
Fromantin C, Jamot B, Cohen J, Piroth L, Pothier P, Kohli E. Rotavirus 2/6 virus-like particles administered intranasally in mice, with or without the mucosal adjuvants cholera toxin and Escherichia coli heat-labile toxin, induce a Th1/Th2-like immune response. J Virol. 2001;75(22):11010–6. https://doi.org/10.1128/JVI.75.22.11010-11016.2001.
Yuan L, Geyer A, Hodgins DC, Fan Z, Qian Y, Chang KO, et al. Intranasal administration of 2/6-rotavirus-like particles with mutant Escherichia coli heat-labile toxin (LT-R192G) induces antibody-secreting cell responses but not protective immunity in gnotobiotic pigs. J Virol. 2000;74(19):8843–53. https://doi.org/10.1128/JVI.74.19.8843-8853.2000.
O'Ryan M, Lopman BA. Parenteral protein-based rotavirus vaccine. Lancet Infect Dis. 2017;17(8):786–7. https://doi.org/10.1016/S1473-3099(17)30244-X.
Hoshino Y, Saif LJ, Kang SY, Sereno MM, Chen WK, Kapikian AZ. Identification of group A rotavirus genes associated with virulence of a porcine rotavirus and host range restriction of a human rotavirus in the gnotobiotic piglet model. Virology. 1995;209(1):274–80. https://doi.org/10.1006/viro.1995.1255.
Bridger JC, Tauscher GI, Desselberger U. Viral determinants of rotavirus pathogenicity in pigs: evidence that the fourth gene of a porcine rotavirus confers diarrhea in the homologous host. J Virol. 1998;72(8):6929–31.
Feng N, Yasukawa LL, Sen A, Greenberg HB. Permissive replication of homologous murine rotavirus in the mouse intestine is primarily regulated by VP4 and NSP1. J Virol. 2013;87(15):8307–16. https://doi.org/10.1128/JVI.00619-13.
Feng N, Kim B, Fenaux M, Nguyen H, Vo P, Omary MB, et al. Role of interferon in homologous and heterologous rotavirus infection in the intestines and extraintestinal organs of suckling mice. J Virol. 2008;82(15):7578–90. https://doi.org/10.1128/JVI.00391-08.
Arnold MM, Sen A, Greenberg HB, Patton JT. The battle between rotavirus and its host for control of the interferon signaling pathway. PLoS Pathog. 2013;9(1):e1003064. https://doi.org/10.1371/journal.ppat.1003064.
Barro M, Patton JT. Rotavirus nonstructural protein 1 subverts innate immune response by inducing degradation of IFN regulatory factor 3. Proc Natl Acad Sci U S A. 2005;102(11):4114–9. https://doi.org/10.1073/pnas.0408376102.
Graff JW, Ettayebi K, Hardy ME. Rotavirus NSP1 inhibits NFkappaB activation by inducing proteasome-dependent degradation of beta-TrCP: a novel mechanism of IFN antagonism. PLoS Pathog. 2009;5(1):e1000280. https://doi.org/10.1371/journal.ppat.1000280.
Arnold MM, Patton JT. Diversity of interferon antagonist activities mediated by NSP1 proteins of different rotavirus strains. J Virol. 2011;85(5):1970–9. https://doi.org/10.1128/JVI.01801-10.
Morelli M, Dennis AF, Patton JT. Putative E3 ubiquitin ligase of human rotavirus inhibits NF-kappaB activation by using molecular mimicry to target beta-TrCP. mBio. 2015;6(1). doi:https://doi.org/10.1128/mBio.02490-14.
• Lutz LM, Pace CR, Arnold MM. Rotavirus NSP1 associates with components of the Cullin RING ligase family of E3 ubiquitin ligases. J Virol. 2016;90(13):6036–48. https://doi.org/10.1128/JVI.00704-16. This study was the first to identify the interaction of NSP1 with the Cul3 scaffolding protein of host cullin-RING E3 ubiquitin ligases.
Ding S, Mooney N, Li B, Kelly MR, Feng N, Loktev AV, et al. Comparative proteomics reveals strain-specific beta-TrCP degradation via rotavirus NSP1 hijacking a host Cullin-3-Rbx1 complex. PLoS Pathog. 2016;12(10):e1005929. https://doi.org/10.1371/journal.ppat.1005929.
Zhang R, Jha BK, Ogden KM, Dong B, Zhao L, Elliott R, et al. Homologous 2′,5′-phosphodiesterases from disparate RNA viruses antagonize antiviral innate immunity. Proc Natl Acad Sci U S A. 2013;110(32):13114–9. https://doi.org/10.1073/pnas.1306917110.
Levy O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat Rev Immunol. 2007;7(5):379–90. https://doi.org/10.1038/nri2075.
Pott J, Stockinger S, Torow N, Smoczek A, Lindner C, McInerney G, et al. Age-dependent TLR3 expression of the intestinal epithelium contributes to rotavirus susceptibility. PLoS Pathog. 2012;8(5):e1002670. https://doi.org/10.1371/journal.ppat.1002670.
Pott J, Mahlakoiv T, Mordstein M, Duerr CU, Michiels T, Stockinger S, et al. IFN-lambda determines the intestinal epithelial antiviral host defense. Proc Natl Acad Sci U S A. 2011;108(19):7944–9. https://doi.org/10.1073/pnas.1100552108.
Mahlakoiv T, Hernandez P, Gronke K, Diefenbach A, Staeheli P. Leukocyte-derived IFN-alpha/beta and epithelial IFN-lambda constitute a compartmentalized mucosal defense system that restricts enteric virus infections. PLoS Pathog. 2015;11(4):e1004782. https://doi.org/10.1371/journal.ppat.1004782.
• Lin JD, Feng N, Sen A, Balan M, Tseng HC, McElrath C, et al. Distinct roles of type I and type III interferons in intestinal immunity to homologous and heterologous rotavirus infections. PLoS Pathog. 2016;12(4):e1005600. https://doi.org/10.1371/journal.ppat.1005600. This study demonstrated that intestinal epithelial cells of neonatal mice were sensitive to both type I and type III interferons, but the responsiveness to type I interferon diminished as the mice age.
• Kanai Y, Komoto S, Kawagishi T, Nouda R, Nagasawa N, Onishi M, et al. Entirely plasmid-based reverse genetics system for rotaviruses. Proc Natl Acad Sci U S A. 2017;114(9):2349–54. https://doi.org/10.1073/pnas.1618424114. This study describes the first entirely plasmid-based reverse genetics system used to create recombinant rotaviruses.
Acknowledgements
Michelle M. Arnold is supported by the NIH National Institute of General Medical Sciences (NIGMS) (P30GM110703) and by the Louisiana Board of Regents (LEQSF(2015-18)-RDA-15).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Arnold reports grants from NIH National Institute of General Medical Sciences, grants from Louisiana Board of Regents, during the conduct of the study.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Recent Developments in Anti-viral Vaccines
Rights and permissions
About this article
Cite this article
Arnold, M.M. Rotavirus Vaccines: Why Continued Investment in Research Is Necessary. Curr Clin Micro Rpt 5, 73–81 (2018). https://doi.org/10.1007/s40588-018-0079-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40588-018-0079-9