Abstract
Background
Delirium is common among elderly patients in the intensive care unit (ICU) and is associated with prolonged hospitalization, increased healthcare costs, and increased risk of death. Understanding the potential risk factors and early prevention of delirium is critical to facilitate timely intervention that may reverse or mitigate the harmful consequences of delirium.
Aim
To clarify the effects of pre-admission falls on ICU outcomes, primarily delirium, and secondarily pressure injuries and urinary tract infections.
Methods
The study relied on data sourced from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. Statistical tests (Wilcoxon rank-sum or chi-squared) compared cohort characteristics. Logistic regression was employed to investigate the association between a history of falls and delirium, as well as secondary outcomes, while Kaplan–Meier survival curves were used to assess short-term survival in delirium and non-delirium patients.
Results
Study encompassed 22,547 participants. Delirium incidence was 40%, significantly higher in patients with a history of falls (54.4% vs. 34.5%, p < 0.001). Logistic regression, controlling for confounders, not only confirmed that a history of falls elevates the odds of delirium (OR: 2.11; 95% CI: 1.97–2.26; p < 0.001) but also showed it increases the incidence of urinary tract infections (OR:1.50; 95% CI:1.40–1.62; p < 0.001) and pressure injuries (OR:1.36; 95% CI:1.26–1.47; p < 0.001). Elderly delirium patients exhibited lower 30-, 180-, and 360-day survival rates than non-delirium counterparts (all p < 0.001).
Conclusions
The study reveals that history of falls significantly heighten the risk of delirium and other adverse outcomes in elderly ICU patients, leading to decreased short-term survival rates. This emphasizes the critical need for early interventions and could inform future strategies to manage and prevent these conditions in ICU settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Falls have become the second leading cause of death worldwide [1]. In the United States, approximately 30% of people over the age of 65 experience a fall each year [2]. Falls not only cause a variety of serious consequences, such as disability, loss of autonomy, and serious neurological damage, but they also increase the risk of death [3, 4]. Across all ethnic groups, falls are responsible for a staggering 75% of unintentional deaths in people over the age of 70 [5]. The financial burden of falls in the U.S. reached approximately $5 billion in 2015, imposing significant financial costs on the healthcare infrastructure [6]. Therefore, early detection and prevention of falls are essential to promote healthy aging.
Delirium, characterized by acute neuropsychiatric symptoms such as inattention and sudden cognitive decline, is notably prevalent among elderly inpatients, with incidences reaching 70–87% [7]. This condition, often overlooked in intensive care unit (ICU) settings due to preexisting conditions in the elderly, can lead to severe consequences including functional impairment, extended hospital stays, cognitive decline, and heightened mortality rates—2–4 times higher than non-ICU settings [8,9,10]. At the same time, the management of delirium is associated with high healthcare costs and caregiver burden, the cumulative cost over 30 days for ICU patients with delirium was $17,838 [11]. This figure is expected to increase as the population continues to age. However, early detection and appropriate care can prevent or mitigate delirium in geriatric patients [12], potentially reducing healthcare costs, length of hospital stays, and mortality.
While previous literature has recognized the association between falls and delirium [13], previous studies often included a history of falls as part of a cluster of risk factors without isolating it as a standalone variable. prior investigations have not specifically focused on the unique setting of the ICU.
While prior studies have explored the link between fall history and delirium, they typically treat fall history as part of a broader set of risk factors without specific focus on the ICU context or precise timing of falls. This overlooks the unique dynamics of falls within the ICU setting and their temporal proximity to ICU admission. Moreover, existing research primarily delves into fall risk factors and general outcomes post-fall, rarely connecting falls directly to pressure injury or UTI, especially within the ICU context. ICU patients are more prone to severe outcomes like delirium due to their critical health and complex treatments such as mechanical ventilation [14]. This study advances the understanding of falls' impact on ICU patients by isolating fall history as a unique variable and exploring its link to specific outcomes like delirium, pressure injuries and urinary tract infections (UTIs). Furthermore, this study integrates survival analysis to explore how pre-admission falls impact mortality and severe outcomes, like delirium, in elderly ICU patients. By focusing on this unique environment, the research aims to provide vital insights into early intervention strategies, significantly enriching the current body of knowledge regarding patient care in critical care settings.
Methods
Study design and population
The study relied on data sourced from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database, version 2.0, which is an extensive, freely accessible, and publicly available resource [15]. The MIMIC-IV database received funding support from the National Institute of Biomedical Imaging and Bioengineering (NIBIB) of the National Institutes of Health (NIH) under grant numbers R01-EB001659 (2003–2013) and R01-EB017205 (2014–2018). Approval for the use of the database was obtained from the institutional review boards of Beth Israel Deaconess Medical Center (Boston, MA) and the Massachusetts Institute of Technology (Cambridge, MA). This study was an analysis of the third-party anonymized publicly available database with pre-existing institutional review board (IRB) approval. The MIMIC-IV database comprehensively captures general patient information, disease-related data, relevant treatments administered, and patients' key blood biochemical indices [16, 17].
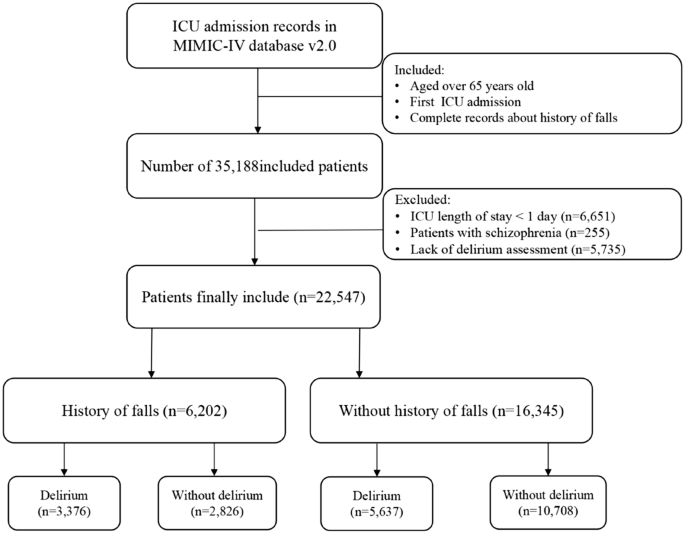
The subject selection criteria for this study were clearly defined: patients age 65 or older in whom a history of falls in the last 3 months was addressed were included. However, individuals with an ICU stay of less than one day or those without documentation of delirium and severe mental illness were intentionally excluded from this study. Ultimately, a cohort of 22,547 patients was captured in this investigation (Fig. 1).
Exposure and outcomes
Falls represent unanticipated occurrences beyond an individual's control, characterized by abrupt, involuntary, and unintended shifts in a patient's position resulting in descent to the ground or a lower level compared to their initial position [4]. The exposure factors in this study were defined as the incidence of unintentional falls among elderly, critically ill patients in the three months prior to ICU admission. A patient's fall history was meticulously assessed upon admission by trained ICU staff through a direct question: "Have you had a fall in the past three months?" An affirmative response to this question identified the patient as having a recent fall history.
Delirium, also referred to as acute encephalopathy, is characterized by changes in consciousness, attention impairment, and cognitive dysfunction [18]. We, employing the Confusion Assessment Method in the ICU (CAM-ICU) [19] and a review of physician and nursing notes [20], conducted the delirium assessment. The assessment of patients' mental status changes during their hospital stay was conducted through a comprehensive review of medical records, including initial and daily observations recorded by nursing staff, evaluations documented in progress notes by nurses or physicians specialized in delirium management, insights from specialized consultations, and summaries provided at discharge. This crucial information is meticulously documented within the "chartevents" form penned by the healthcare provider. Delirium could be defined as a patient who either had 1) a positive CAM-ICU or 2) diagnosed with delirium by a physician based on chart documentation.
Study outcomes included delirium, urinary tract infections and pressure injury, with delirium as the primary outcome and urinary tract infections and pressure injury as secondary outcomes. UTIs were diagnosed according to the International Classification of Diseases, 9th and 10th versions. Pressure injuries were carefully assessed and documented by dedicated intensive care nurses.
Variable collection
Navicat Premium software, version 16, using Structured Query Language, was used for data extraction. The maximum percentage of missing values for any of the extracted variables did not exceed 20%, and multiple imputation was used to deal with these missing data [21]. The selection of covariates in our study was based on a comprehensive approach that took into account prior literature, clinical expertise, and the availability of data within the database. The following variables were included in this study:
-
1.
General characteristics: age, sex, marital status, race, language, weight, hospital and ICU length of stay.
-
2.
Scores: Glasgow Coma Scale (GCS), Sequential Organ Failure Assessment (SOFA), Braden scores and Charlson Comorbidity Index (CCI).
-
3.
Comorbidities: myocardial infarct, congestive heart failure, dementia, rheumatic disease, mild liver disease, diabetes, renal disease, malignant cancer, severe liver disease, cerebrovascular disease, hypertension, sepsis, depression, pain, paraplegia, peripheral vascular disease and metastatic solid tumor.
-
4.
Vital signs: heart rate mean, mean blood pressure, respiratory rate mean and temperature mean.
-
5.
Laboratory parameters: SpO2 mean, albumin, Blood Urea Nitrogen (BUN) and creatinine.
-
6.
Treatments and drugs: enteral nutrition, mechanical thrombectomy, dialysis present, vasoactive agents, sedatives and invasive mechanical ventilation.
-
7.
Outcomes: delirium, pressure injury, urinary tract infection and 30-day, 180-day, and 360-day mortality.
Covariates
In this study, independent variables with potential impact on outcomes were considered as covariates and adjusted for within regression models based on clinical expertise and literature review. For delirium, adjustments were made for age, sex, race, marital status, dementia, depression, cerebrovascular disease, sedative use, CCI, SOFA, GCS, and Braden scores. For aspiration pneumonia and pressure injuries, adjustments were made for age, sex, race, GCS, CCI, SOFA, and Braden scores.
Statistical methods
This observational study was conducted in adherence to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines to ensure comprehensive and transparent reporting of the research findings [22]. The study initially performed a descriptive statistical analysis on the collected and organized data. Patients were stratified based on falls presence or absence in the three months before admission. Continuous variables were expressed as medians with interquartile ranges, and differences were compared using the Wilcoxon rank-sum test. Categorical variables were presented as counts and percentages, and group differences were assessed using the chi-squared test. Logistic regression models determined the association between fall history and outcomes, yielding odds ratios (OR) and 95% confidence intervals (CI).
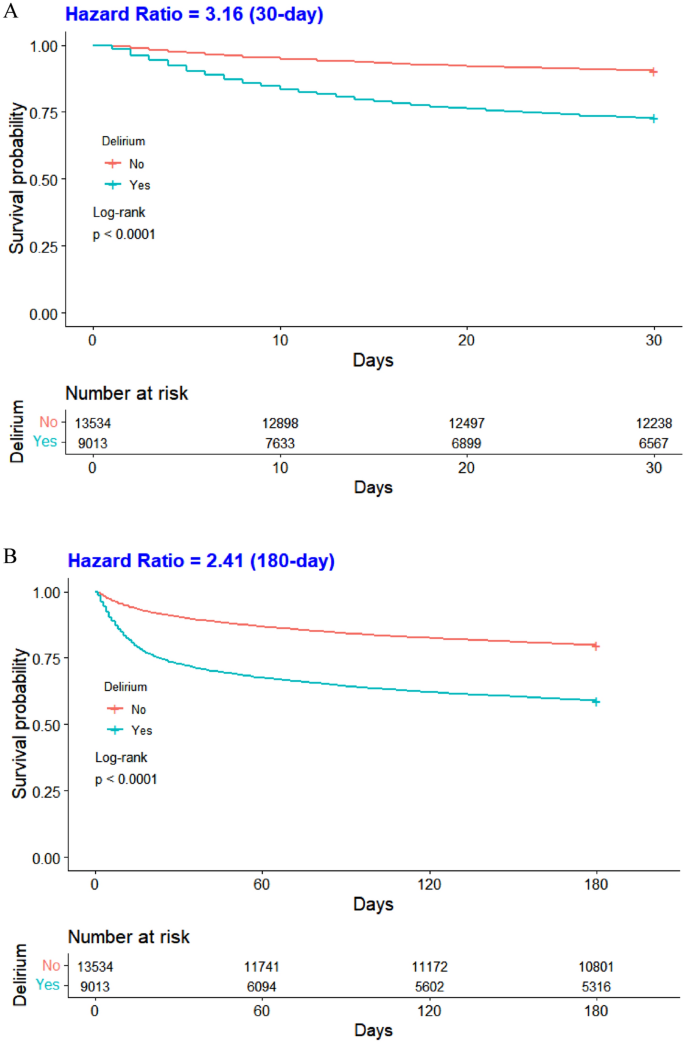
To show the survival rates at 30, 180, and 360 days among the elderly ICU patients who developed delirium, we estimated Kaplan–Meier survival curves and assessed differences in survival distributions between groups using the log-rank test. To examine joint associations, we divided the entire cohort into four groups based on the variables: a history of falls and the presence of delirium. Baseline data for these four groups were tabulated, and between-group differences were assessed using the Kruskal–Wallis H test for continuous variables and the chi-squared test for categorical variables. Hazard ratios (HRs) and 95% confidence intervals for mortality at 30, 180, and 360 days were calculated for the different groups compared with older patients, no history of falls, and no delirium.
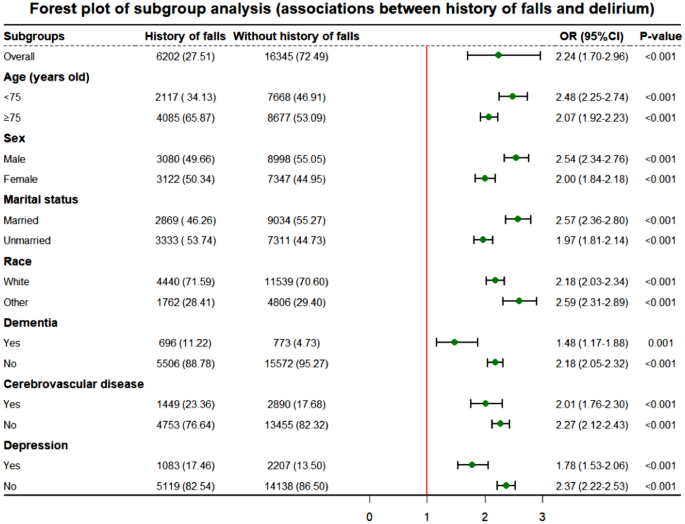
Subsequently, this study examined the association between a history of falls and delirium in different subgroups of elderly ICU patients. We examined the association within the subgroups of sex, age, race, marital status, dementia, cerebrovascular disease, and depression. To assess the combined association, we divided the total population into four categories based on history of falls and presence of delirium. The short-term mortality risk in the different groups was calculated in contrast to ischemic stroke patients without fall history and delirium.
Finally, two sensitivity analyses were conducted to assess our findings' robustness. Covariate adjustments were made using propensity score matching (PSM). Propensity scores, derived from logistic regression models incorporating sex, age, race, marital status, body weight, ventilation status, GCS, CCI, and SOFA scores, were estimated. Employing a 1:1 matching algorithm with the nearest neighbor method, the matched population underwent comparison using the Wilcoxon rank-sum test or chi-squared test. To address potential unmeasured confounding factors, the E-value was calculated—an indicator in observational studies gauging the impact of such factors on study outcomes. Higher E-values signify greater result robustness and decreased susceptibility to confounding influences.
Data were processed using R software (version 4.3.0, https://www.r-project.org/). A p-value of less than 0.05 was considered indicative of statistical significance.
Result
Baseline characteristics of the study cohort
After careful screening, a total of 22,547 elderly patients were included in the study. Of these, 6,206 patients had experienced a fall within the three months prior to ICU admission. Table 1A,1B,1C,1D describes the baseline characteristics of the study cohort, categorized by exposure factor (Table 1B,1C,1D in Supplementary Materials). Of the total patient population, 12,078 (53.6%) were male, with a median age of 76.71 years (interquartile range: 70.65–83.82 years) and a median ICU length of stay of 2.44 days (interquartile range: 1.60–4.30 days). Compared to patients without a fall history, those with a fall history had an older median age (79.57 vs. 75.78 years), lower weight (73.00 kg vs. 77.80 kg), and a higher proportion of unmarried individuals (including single, divorced, widowed, etc.). These differences were statistically significant (P < 0.05).
Associations between history of falls and the risks of delirium, urinary tract infection, and pressure injury
Table 2 shows an association between a history of falls and the risk of adverse outcomes in ICU patients. According to the results of the multivariate logistic regression analysis performed, compared to patients without a history of falls, those with such a history had a significantly increased prevalence of delirium during their critical illness, with an adjusted odds ratio (OR) of 2.11 (95% CI: 1.97–2.26). In addition, patients with a history of falls were also at risk for urinary tract infection and pressure injury, with adjusted odds ratios (ORs) of 1.50 (95% CI: 1.40–1.62) and 1.36 (95% CI: 1.26–1.47), respectively. These findings suggested that a history of falls could be an independent risk factor for delirium, UTIs, and pressure injury in the ICU.
In addition, this study compared the survival rates of geriatric critically ill patients, both with and without delirium, at 30, 180, and 360-day intervals (Fig. 2A,2B,2C). The Kaplan–Meier survival curve demonstrated that elderly patients who developed delirium had significantly lower survival rates at 30, 180, and 360 days compared to those who without delirium (all p < 0.001).
Subgroup analysis
In this study, a subgroup analysis elucidated the relationship between exposure and the primary outcome (delirium) to further our understanding of the association between a history of falls and delirium within subpopulations. The results show substantial statistical variation across all subgroups, suggesting a persistent association between a history of falls and the incidence of delirium within these boundaries (Fig. 3). Apparently, a history of falls may serve as a critical risk factor for delirium in ICU patients, with these findings applicable to individuals across different sex and age groups.
Joint association
This study investigated the combined impact of a history of falls and delirium on mortality rates at 30, 180, and 360 days, presented in eTable 3 [Supplementary materials]. Baseline characteristics of the four patient cohorts were detailed in eTable 2 [Supplementary materials], highlighting differences between groups. The multivariate Cox proportional hazards model demonstrated that, compared to older patients without falls and delirium, those with both conditions had the highest mortality risk at 30, 180, and 360 days, with adjusted HRs of 4.07 (3.72, 4.45), 3.07 (2.87, 3.28), and 2.79 (2.62, 2.97), respectively.
Sensitivity analysis
After PSM, most baseline parameters showed no significant differences between the two cohorts. Univariate and multivariate logistic regression analyses on the matched cohort yielded results consistent with the original population (eTable 2 in Supplementary Materials). This underscores the association between a history of falls and delirium, urinary tract infection, and pressure injury in elderly patients during critical illness (all p < 0.05). These outcomes emphasize the robustness and stability of our findings.
Discussion
This study utilized publicly available MIMIC-IV data from the United States to investigate the association between falls within the previous 3 months and adverse outcomes in ICU patients, focusing on short-term mortality in elderly patients with delirium. Findings revealed that a history of falls within three months before hospital admission heightened the risk of delirium. These results align with prior research [23, 24]. A possible explanation may be that falls in older adults typically signal a decline in physical and cognitive function, as evidenced by impaired attention, executive function, and slowed gait [25]. A one-point decline in the Mini-Mental State Examination score corresponded to a subsequent 20% increase in the risk of falling [3]. Falls could also induce brain injury and physical trauma, leading to pain, extended hospital stays, and intensified treatment, all factors accelerating delirium onset [13, 26]. Identifying and addressing fall-related risk factors is crucial in preventing delirium in ICU patients. Healthcare professionals can utilize a patient's fall history before admission as an indicator for potential delirium, informing targeted interventions alongside other high-risk factors.
In the ICU setting, the interplay between a history of falls and the onset of UTIs and pressure injuries is multifaceted. Findings indicated an increased likelihood of pressure injuries in patients with falls, consistent with prior research [27]. The explanation lies in fall-related injuries restricting mobility, reducing turning frequency, and predisposing patients to prolonged pressure, thereby compromising skin integrity and fostering pressure ulcers [28]. Falls, causing brain damage and functional decline, often result in compromised bowel control, contributing to pressure injuries around the buttocks due to combined effects of urine, fecal stimulation, and pressure [29]. This research also discovered a correlation between a history of falls and urinary tract infections, aligning with the conclusions of prior studies [30]. Falls in older individuals elevate UTI risks through injuries necessitating catheterization, bacterial colonization, urethral mucosa damage, and a weakened immune response. Reduced mobility, often a consequence of falls, necessitates extended periods of immobilization and potentially the use of urinary catheters, both of which significantly elevate the risk of UTIs. Concurrently, immobilization increases the likelihood of developing pressure injuries due to sustained pressure on certain body areas. In ICUs, complex care protocols such as sedation and the use of physical restraints may inadvertently reduce patient mobility, thereby increasing the likelihood of UTIs and pressure injuries. It is crucial for ICU healthcare professionals to prioritize the prevention of these conditions through careful monitoring and the implementation of specific interventions. Strategies such as frequent repositioning and meticulous urinary catheter management are essential to minimize these risks and improve patient outcomes.
Delirium emerged as an independent risk factor for heightened mortality risk in this study. Patients developing delirium exhibited significantly reduced survival rates at 30, 180, and 360 days compared to their non-delirium counterparts, aligning with prior research [31]. Delirium represents an episode of acute brain failure and its damage to the brain may not be fully reversible and is closely associated with long-term cognitive decline [32], which can severely impact a patient's quality of life. Delirium onset is linked with inflammation and neuronal apoptosis, potentially leading to brain atrophy and diminished survival [33]. Concurrently, delirium-associated complications like aspiration pneumonia and increased restraint use extended hospital stays, elevating ICU infection risks and acting as an independent mortality risk factor [34]. Each additional hour of delay in hospitalization raised the risk of death by approximately 3% [35]. The joint effects unveiled a substantial mortality increase at 30, 180, and 360 days in patients with both a history of falls and delirium compared to those without. This survival analysis is pivotal for filling the research void by providing concrete data on mortality risks at critical junctures post-admission, thereby offering a clearer guide for clinical strategies aimed at reducing fall-related fatalities among ICU patients.
Our research demonstrates that a history of falls within three months prior to ICU admission significantly increases the likelihood of delirium, decreases survival rates, and elevates the incidence of secondary outcomes such as pressure ulcers and urinary tract infections in ICU patients. This highlights the critical need for early screening and intervention strategies focusing on fall history to mitigate these risks. By prioritizing fall history in patient evaluations, healthcare professionals can identify high-risk individuals for targeted preventive measures, thereby improving patient care and outcomes in the ICU.
This study boasts several strengths. Firstly, the substantial sample size enhances statistical precision, reducing variance and uncertainty in research findings. Secondly, the innovative assessment method, utilizing the CAM-ICU scale and nursing notes, ensures result stability and reliability. Thirdly, sensitivity analyses confirm the robustness of conclusions. Lastly, explicit definition of fall timing in the Morse Fall Scale score and identification of falls within three months quantify fall history, pinpointing associated high-risk factors [36]. These strengths significantly bolster the study's credibility.
There are also several limitations to the study. Firstly, its retrospective nature may lead to selection and information biases. Secondly, relying on nursing notes for assessing falls and delirium could result in underreporting. Lastly, the findings from a single tertiary academic medical center in Boston might not be broadly applicable to other settings. To overcome these limitations, future research should adopt a prospective study design could minimize biases associated with retrospective analyses. In addition, expanding the study to include multiple centers with diverse patient populations would improve the generalizability of the findings. Finally, integrating quantitative tools alongside nursing notes could offer a more comprehensive evaluation of falls and delirium, enriching the data quality.
Conclusion
This study demonstrates that a history of falls significantly influences the onset of delirium in elderly ICU patients, also increasing urinary tract infections and pressure injuries. Moreover, patients with delirium exhibited significantly lower short-term survival rates than their healthy counterparts, posing a substantial threat to patient health. These findings highlight the need for healthcare professionals to adopt predictive measures and targeted interventions to enhance patient care and reduce costs, potentially guiding future research to refine management and preventive strategies for delirium and related conditions in the ICU.
References
Gu Y, Zhang Y, Huang M et al (2018) Your WiFi knows you fall: a channel data-driven device-free fall sensing system. In: 2018 5th IEEE international conference on cloud computing and intelligence systems (CCIS). IEEE, pp 943–947
Joo H, Wang G, Yee SL et al (2017) Economic burden of informal caregiving associated with history of stroke and falls among older adults in the US[J]. Am J Prev Med 53:S197–S204
Ambrose AF, Paul G, Hausdorff JM (2013) Risk factors for falls among older adults: a review of the literature[J]. Maturitas 75:51–61
Cheng H, Wang Z, Gu WJ et al (2022) Impact of falls within 3 months on the short-term prognoses of elderly patients in intensive care units: a retrospective cohort study using stabilized inverse probability treatment weighting[J]. Clin Interv Aging 17:1779–1792
Fuller GF (2000) Falls in the elderly[J]. Am Fam Phys 61:2159–2168
Florence CS, Bergen G, Atherly A et al (2018) The medical costs of fatal falls and fall injuries among older adults[J]. J Am Geriatr Soc 66:693–698
Fong TG, Tulebaev SR, Inouye SK (2009) Delirium in elderly adults: diagnosis, prevention and treatment[J]. Nat Rev Neurol 5:210–220
Ouimet S, Kavanagh BP, Gottfried SB et al (2007) Incidence, risk factors and consequences of ICU delirium[J]. Intensive Care Med 33:66–73
van den Boogaard M, Schoonhoven L, van der Hoeven JG et al (2012) Incidence and short-term consequences of delirium in critically ill patients: a prospective observational cohort study[J]. Int J Nurs Stud 49:775–783
Inouye SK, Westendorp RGJ, Saczynski JS (2014) Delirium in elderly people[J]. Lancet 383:911–922
Vasilevskis EE, Chandrasekhar R, Holtze CH et al (2018) The cost of ICU delirium and coma in the intensive care unit patient[J]. Med Care 56:890–897
Marcantonio ER (2017) Delirium in hospitalized older adults[J]. N Engl J Med 377:1456–1466
Sillner AY, Holle CL, Rudolph JL (2019) The overlap between falls and delirium in hospitalized older adults: a systematic Review[J]. Clin Geriatr Med 35:221–236
Bloomer MJ, Woszczeiko C, Hutchinson AM (2022) Older age, delirium, dementia, frailty, and critical care: care priorities[J]. Intensive Crit Care Nurs 73:103297
Johnson AEW, Bulgarelli L, Shen L et al (2023) MIMIC-IV, a freely accessible electronic health record dataset[J]. Scientific Data 10:1
Wu WT, Li YJ, Feng AZ et al (2021) Data mining in clinical big data: the frequently used databases, steps, and methodological models[J]. Mil Med Res 8:44
Yang J, Li Y, Liu Q et al (2020) Brief introduction of medical database and data mining technology in big data era[J]. J Evid Based Med 13:57–69
Wei F, Cheng H, He R et al (2024) Geriatric nutritional risk index independently predicts delirium in older patients in intensive care units: a multicenter cohort study[J]. Arch Gerontol Geriatr 118:105288
Barr J, Fraser GL, Puntillo K et al (2013) Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit[J]. Crit Care Med 41:263–306
Saczynski JS, Kosar CM, Xu G et al (2014) A tale of two methods: chart and interview methods for identifying delirium[J]. J Am Geriatr Soc 62:518–524
Austin PC, White IR, Lee DS et al (2021) Missing data in clinical research: a tutorial on multiple imputation[J]. Can J Cardiol 37:1322–1331
von Elm E, Altman DG, Egger M et al (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies[J]. International J Sur (London, England) 12:1495–1499
Boorsma M, Joling KJ, Frijters DHM et al (2012) The prevalence, incidence and risk factors for delirium in Dutch nursing homes and residential care homes[J]. Int J Geriatr Psychiatry 27:709–715
Zrour C, Haddad R, Zoghbi M et al (2020) Prospective, multi-centric benchmark study assessing delirium: prevalence, incidence and its correlates in hospitalized elderly Lebanese patients[J]. Aging Clin Exp Res 32:689–697
Montero-Odasso M, Speechley M (2018) Falls in cognitively impaired older adults: implications for risk assessment and prevention[J]. J Am Geriatr Soc 66:367–375
MacLullich AM, Ferguson KJ, Miller T et al (2008) Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses[J]. J Psychosom Res 65:229–238
Kim J, Lee JY, Lee E (2022) Risk factors for newly acquired pressure ulcer and the impact of nurse staffing on pressure ulcer incidence[J]. J Nurs Manag 30:O1–O9
Doran D, Lefebre N, O’Brien-Pallas L et al (2014) The relationship among evidence-based practice and client dyspnea, pain, falls, and pressure ulcer outcomes in the community setting[J]. Worldviews Evidence-Based Nurs 11:274–283
García-Mayor S, Morilla-Herrera JC, Lupiáñez-Pérez I et al (2018) Peripheral perfusion and oxygenation in areas of risk of skin integrity impairment exposed to pressure patterns. a phase I trial (POTER study)[J]. J Adv Nurs 74:465–471
Amarsy R, Guéret D, Benmansour H et al (2019) Determination of Escherichia coli phylogroups in elderly patients with urinary tract infection or asymptomatic bacteriuria[J]. Clin Microbiol Infect: Off Publ Eur Soc Clin Microbiol Infect Dis 25:839–844
Maldonado JR (2017) Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium[J]. Crit Care Clin 33:461–519
Goldberg TE, Chen C, Wang Y et al (2020) Association of delirium with long-term cognitive decline: a meta-analysis[J]. JAMA Neurol 77:1373–1381
van Gool WA, van de Beek D, Eikelenboom P (2010) Systemic infection and delirium: when cytokines and acetylcholine collide[J]. Lancet (London, England) 375:773–775
Aung Thein MZ, Pereira JV, Nitchingham A et al (2020) A call to action for delirium research: Meta-analysis and regression of delirium associated mortality[J]. BMC Geriatr 20:325
Churpek MM, Wendlandt B, Zadravecz FJ et al (2016) Association between ICU transfer delay and hospital mortality: a multicenter investigation[J]. J Hosp Med 11:757–762
Morse JM, Black C, Oberle K et al (1982) A prospective study to identify the fall-prone patient[J]. Soc Sci Med 28:81–86
Funding
This work was supported by the National Natural Science Foundation of China (No.72274078); the Guangdong Provincial Key Laboratory of Traditional Chinese Medicine Informatization (No.2021B1212040007).
Author information
Authors and Affiliations
Contributions
FB, HC and ZW created the study protocol, performed the statistical analyses and wrote the first manuscript draft. QL and JL conceived the study and critically revised the manuscript. YH, ZZ and CL assisted with the study design and performed data collection. FB and HC confirmed the data and assisted with the statistical analyses. YW and YZ contributed to data interpretation and manuscript revision. QL and JL, as senior authors, reviewed and edited all versions of this manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Human and animal rights and informed consent
Data extracted from the MIMIC-IV database do not require individual informed consent because the research data is publicly available, and all patient data are de-identified.
Data Availability Statement
Data are openly available in a public repository that can be accessed upon completion of the Protecting Human Research Participants web-based training from the National Institutes of Health. The datasets generated and analyzed during the current study are available from the corresponding authors, Jun Lyu and Qi-yuan Lyu, upon reasonable request.
Ethical approval
This is a retrospective study based on MIMIC-IV database. The patient's information has been hidden before the study. There is no need for the patient's informed consent and no ethical conflict
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bu, F., Cheng, Ht., Wang, Zl. et al. Effect of a fall within three months of admission on delirium in critically Ill elderly patients: a population-based cohort study. Aging Clin Exp Res 36, 111 (2024). https://doi.org/10.1007/s40520-024-02740-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-024-02740-8