Abstract
Background
Cardiometabolic multimorbidity (CM) has been found to be associated with higher mortality and functional limitations. However, few studies have investigated the longitudinal association between CM and disability in the Chinese population and whether these associations vary by smoking status.
Methods
The study included 16,754 participants from four waves (2011, 2013, 2015, and 2018) of China Health and Retirement Longitudinal Study (CHARLS) (mean age: 59, female: 51%). CM was assesed at baseline and defined as having two or more of diabetes, stroke, or heart disease. Disability was repeatedly measured by summing the number of impaired activities of daily living (ADL) and instrumental activities of daily living (IADL) during the 7-year follow-up. Linear mixed-effects model was used to determine the association of CM and trajectories of disability and to assess the modification effect of smoking status in these associations.
Results
Participants with CM at baseline had a faster progression of disability compared to those without CM (CM: β = 0.13, 95% CI: 0.05 to 0.21). Current smokers with CM developed disability faster than their counterparts (Pinteraction for smoking=0.011). In addition, there was a significant association between CM and the annual change of disability in current smokers (β = 0.34, 95% CI: 0.17 to 0.50) while no such association was observed in current non-smokers (β = 0.08, 95% CI: -0.02 to 0.17).
Conclusion
CM was associated with more a rapid disability progression. Notably, being current smokers may amplify the adverse effects of CM on disability progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disability, defined as difficulty in performing activities necessary for independent living, has been increasing, a global trend partly driven by increasingly aging population and diseases [1]. Available studies suggest its association with adverse health outcomes, including increased health care utilization, low quality of life, and high risk of mortality [2,3,4]. Chronic non-communicable disease has attracted increasing attentions, with studies reporting a correlation between chronic disease and a higher risk of disability, especially in middle-aged and older populations, thus necessitating modulation to prevent or delay the progression of disability [5].
Non-communicable diseases, especially cardio-metabolic diseases, are rapidly increasing in low- and middle-income countries [6]. Cardiometabolic multimorbidity (CM) is the simultaneous presence of two or more cardiometabolic diseases (diabetes, stroke, and heart disease), which is rapidly increasing as the population ages [7]. The Emerging Risk Factors Collaboration (ERFC) reported that any combination of cardiometabolic diseases was associated with multiplicative mortality risk, with each additional disease doubling the risk of mortality [7]. Additionally, exposure to CM was shown to increase the odds of activity limitation among Canada adults [8]. In the Chinese population, however, no relative correlation between the above-mentioned CM and disability have been explored.
Smoking is one of the major threats to global public health as well as a leading risk factor for premature death and disability from non-communicable diseases in Chinese [9, 10]. Additionally, previous research has supported that smoking increases the risk of cardiovascular disease, stroke, and diabetes [11, 12]. This poor lifestyle with respect to tobacco exposure may play a role in the association between CM and activity limitation.
In view of these considerations, we aimed to explore the effect of CM on the progression of disability and to explore the possible role of smoking status through a nationally representative cohort-China Health and Retirement Longitudinal Study (CHARLS).
Method
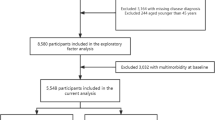
Data were obtained from the China Health and Retirement Longitudinal Study (CHARLS) that is a nationally representative cohort survey based on community residents aged 45 years and older. Using a multi-stage probability sampling method, the baseline survey began in 2011 with a follow-up survey conducted every two years, including a biennial face-to-face interview to assess the social, economic and health status of participants and blood sample collected once in every two follow-up periods [13]. In this study, we used four waves (2011, 2013, 2015, and 2018) of CHARLS. Those who (1) younger than 45 years old (n = 368); (2) with no information on diabetes, stroke and heart diseases (n = 294); (3) with no information on disability at baseline (n = 289) were excluded, leaving 16,754 participants to be remained in the analytical sample (Fig. 1).
Measurements
Cardiometabolic multimorbidity
CM was assessed at baseline and defined as having two or more of diabetes, stroke, or heart disease [7]. Diabetes was identified when having one of the following conditions: (1) fasting plasma glucose (FPG) ≥ 126 mg/dl; (2) glycated hemoglobin (HbA1c) ≥ 6.5%; (3) self-reported doctor diagnosed diabetes; (4) diabetes treatment [14]. Fasting plasma glucose concentration was measured by enzymatic colorimetric analysis and glycated hemoglobin concentration was determined by borate affinity high performance liquid chromatography [15]. Stroke or heart disease (e.g., heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems) were identified if participants reported the specific disease diagnoses or treatment.
Disability
Activities of daily living (ADL) (6 items: eating, bathing, dressing, getting in and out of bed, toileting, and controlling urination and defecation) and instrumental activities of daily living (IADL) (5 items: doing household chores, preparing meals, shopping, managing money, and taking medications) were assessed using participant self-reported information at baseline and every follow-up visits [16, 17]. Each item has four options, participants reporting no difficulty are considered 0 point, otherwise 1 point. We first considered ADL and IADL as separate scales and then merged them together (range:0–11) for enhancing range and sensitivity of the measurement [18].
Covariates
Sociodemographic (age, sex, education, marital, residential location), behavioral habits (smoking and alcohol consumption) and health information (other non-communicable diseases, depressive symptoms, body mass index) were considered as covariates and measured at baseline. All these factors were considered associated with disability and were regarded as control covariates [19, 20].
Education was classified as ‘≤ 6 years’ and ‘> 6 years’ based on the maximum years of schooling, marital status was categorized into married and non-married (separated/ divorced/widowed/single). Residential location was assessed according to living area: ‘rural’ versus ‘urban’, smoking was dichotomized as current non-smokers (including former smokers) and current smokers. Alcohol consumption was classified as occasional drinkers (less than or equal to three times a week) and habitual drinkers (more than three times a week). Based on participants’ self-reported doctor diagnoses of certain diseases or treatments for these diseases, other non-communicable diseases (NCDs) was divided into two groups: ‘yes’ and ‘no’. Depression symptoms were measured using the 10-item Center for Epidemiologic Studies Depression Scale (ranging 0 to 30) [21]. Body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2) and defined as a continuous variable.
Statistical analysis
First, student ‘s t - test for numerical variables and chi-square tests for categorical variables were used to compare sociodemographic and health-related characteristics of participants with and without CM. Second, linear mixed-effects model was used to estimate the association between CM and the trajectory of disability over time. CM status, follow-up time, and their interactions were considered as fixed effects, while individual differences in baseline disability and in the rate of disability accumulation were regarded as random effects. The interaction between time and CM status represents the estimated difference in the annual rate of disability progression between CM group and non-CM group. Covariates including age, sex, education, marital, residential location, smoking, alcohol consumption, NCDs, depressive symptoms, and BMI were adjusted in the analysis.
Third, further analysis with a time-by-CM-by-smoking interaction was included to test the modification effect of smoking in the longitudinal association between CM and disability.
In addition, a number of sensitive analyses were conducted by repeating the analyses: (1) adjusting cognitive function as a confounding factor; (2) excluding those who had memory-related disease at baseline (n = 122) to reduce recall bias; (3) excluding those who had ADL or IADL disability at baseline (n = 2751) to minimize the influence of reverse causation.
A two-tailed P < 0.05 was considered statistically significant. All analysis were performed using STATA 15.0.
Results
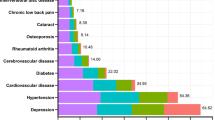
Table 1 showed the baseline characteristics of participants classified by CM status. A total of 16,754 participants were included in our study, with a mean age of 59 years old and 51% were female. Among them, 560 (3.3%) reported having CM at baseline. Compared to participants without CM, those with CM were more likely to be females, older, current non-smokers, occasional drinkers, likely to have higher BMI, NCDs, and experience more disabilities and depressive symptoms. However, we did not observe significant differences in education level, marital status, and place of residence between participants with and without CM. In addition, participants with missing values on CM or/and disabilities as well as those who dropped out tended to be older, males, occasional drinkers, have more depressive symptoms and disabilities, have higher education levels, lower BMI, and live in urban areas, and less likely to be married compared to those with complete information (Table S1).
The results from linear mixed-effects model that estimated associations between CM status and ADL and IADL disability trajectories were presented in Table 2. The average (ADL + IADL) disability scores increased over time from 0.8 in 2011, 0.8 in 2013, 1.0 in 2015 to 1.1 in 2018 (data not shown). Participants with CM had higher baseline disability scores compared to those without CM (β = 0.57, 95%CI: 0.41 to 0.73). In the fully adjusted model, compared to people with non-CM, those who with CM had faster disability progression (β = 0.13, 95%CI: 0.05 to 0.21) within seven years (Fig. 2). In addition, similar trend was observed when ADL and IADL were regarded as dependent variables, respectively (β = 0.07, 95%CI: 0.03 to 0.12; β = 0.05, 95%CI: 0.01 to 0.10) (Table 2).
Table 3 showed the moderating role of smoking status in the relationship between CM and disability trajectory. There was a significant interaction between smoking and CM on the annual-year change of disability (P interaction for smoking=0.011). That is, baseline CM was significantly associated with changes in the number of ADL and IADL disabilities in current smokers but not in current non-smokers. Table 3 showed that for current non-smokers with and without CM, the rate of increase in the number of disabilities over time was comparable, while current smokers with CM had a higher rate of increase in disability over time than current smokers without CM.
Sensitivity analysis
Similar tendency was found in the analysis when adjusting cognitive function (Table S2). Moreover, the associations between CM and trajectories of disability were similar among those without memory-related disease or disability at baseline (Table S3 and S4).
Discussion
In this community-based cohort study, we found that the presence of CM was associated with a more rapid increasing rate in the total number of (ADL + IADL) disabilities during the 7-year follow-up period among Chinese middle-aged and older adults after adjusting for potential confounding factors. In addition, there was a multiplicative interaction between CM and smoking status on disability progression, indicating that being current smokers may exacerbate the deleterious effect of CM on disability progression in middle-aged and older adults. Our current findings in a general population might be helpful in improving the health-care plan for individuals with CM, aiming to slow down the progression of disability in middle-aged and older adults.
Our findings are consistent with Brayden’s study that they have examined the cross-sectional association between CM and (ADL + IADL) limitations by using data from the Canadian Longitudinal Study on Aging [8], and we extend their results by demonstrating the predictive role of CM in the longitudinal trajectory of disability. Furthermore, a previous report by the The China Health and Nutrition Survey demonstrated the longitude correlation between CM and higher risk of ADL limitations [22]. Additionally, in our study, individuals with CM were more likely to be current non-smokers or occasional drinkers, possibly because a portion of individuals with CM were former smokers (17.63%) (have quit smoking) or former drinkers (20.17%). Due to illness, they had already quit some unhealthy habits (e.g., smoking or drinking) at baseline.
The underlying mechanisms linking cardiac metabolic diseases to ADL/IADL disability accumulation can be explained in the following aspects. For one thing, a high-risk state for disability development is based on diminished homeostatic capacity across multiple physiological systems [23]. For example, high glucose levels in diabetes patients can damage cardiac blood vessels, promote the aggregation of arterial plaques, inflammatory responses, and oxidative stress [24]. These factors can lead to the development of atherosclerosis and an increased risk of thrombosis, that subsequently leads muscle catabolism and disability as part of the frailty process [25, 26]. For another, impairment of heart function may result in exacerbated stroke consequences, including increased stroke size and heightened neurological deficits, thus accelerating the accumulation of disability [27].
Furthermore, the present study showed that association between the CM and disability accumulation was modified by smoking status, with current smokers experiencing the highest risk. Possible explanations might be that the interaction between CM and smoking may lead to more severe inflammation and oxidative stress, further impairing bodily functions, resulting in the accumulation of limitations in ADL/IADL [28,29,30]. Our results provide further evidence that special attention should be directed towards current smokers among individuals with CM, as they are important targets for reducing the accumulation of disabilities.
Strengths and limitations
The strengths of this study lie in its utilization of a large sample of population-based data and its prospective design, as well as the repeated measurements of outcomes (i.e., the counting of ADL and IADL limitations), that make the study with increased precision and generalizability. Moreover, the combination of ADL and IADL could help screen a wider range of disability and enhance the sensitivity of the measurement [18]. However, there are several limitations to this study. First, CM was measured only at baseline, therefore, we were unable to assess disability progression related to changes in the CM over time. Disability may have accumulated faster in individuals without CM at baseline due to new onset of CM. Biases would not have occurred if the number of CM increased at a comparable rate over time. However, due to ceiling effects in those with CM at baseline, we may have underestimated the associations of the CM with disability progression by not updating the CM status over time. Future research is needed to monitor the trajectories of the CM and examine their added prognostic value. Second, information regarding heart disease, stroke, ADL, IADL, and some covariates were self-reported, which may introduce reporting bias and potentially impact the risk estimates in this study and therefore our results need to be interpreted with caution. Third, missing values on CM could potentially introduce selection bias. Nevertheless, the missing values of CM were less (1.8%), which may not affect the overall results. Finally, longitudinal data are often incomplete or unbalanced due to loss of follow-up. However, linear mixed-effect models are capable of handling missing data and inconsistent measurement intervals within and across participants, allowing us to utilize all available data for each participant [31].
Conclusion
In this prospective study, CM was associated with disability accumulation, and this association was moderated by smoking status, with current smokers experiencing a more rapid progression of disabilities. Therefore, it is important to implement disability-prevention measures aimed at reducing smoking among middle-aged and older individuals with cardiometabolic multimorbidity.
Data availability
The dataset collected in the current study are available from the website: http://charls.pku.edu.cn/index/en.html.
References
Pope AM, Tarlov AR (1991) Disability in America: toward a national agenda for prevention. ERIC
Johnston KJ, Wen H, Hockenberry JM, Joynt Maddox KE (2018) Association between Patient Cognitive and Functional Status and Medicare Total Annual Cost of Care: implications for value-based payment. JAMA Intern Med 178(11):1489–1497
Nakazawa A, Nakamura K, Kitamura K, Yoshizawa Y (2012) Association between activities of daily living and mortality among institutionalized elderly adults in Japan. J Epidemiol 22(6):501–507
Thompson WW, Zack MM, Krahn GL, Andresen EM, Barile JP (2012) Health-related quality of life among older adults with and without functional limitations. Am J Public Health 102(3):496–502
Griffith LE, Raina P, Levasseur M, Sohel N, Payette H, Tuokko H et al (2017) Functional disability and social participation restriction associated with chronic conditions in middle-aged and older adults. J Epidemiol Commun Health 71(4):381–389
Miranda JJ, Barrientos-Gutiérrez T, Corvalan C, Hyder AA, Lazo-Porras M, Oni T et al (2019) Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat Med 25(11):1667–1679
Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, Bansal N et al (2015) Association of Cardiometabolic Multimorbidity with Mortality. JAMA 314(1):52–60
Fishbook BN, Brinton CD, Siever J, Klassen TD, Sakakibara BM (2022) Cardiometabolic multimorbidity and activity limitation: a cross-sectional study of adults using the Canadian longitudinal study on aging data. Fam Pract 39(3):455–463
Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, Abate KH et al (2017) Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the global burden of Disease Study 2015. Lancet (London England) 389(10082):1885–1906
Yang G, Wang Y, Wu Y, Yang J, Wan X (2015) The road to effective tobacco control in China. Lancet (London England) 385(9972):1019–1028
Hackshaw A, Morris JK, Boniface S, Tang JL, Milenković D (2018) Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ (Clinical Res ed) 360:j5855
Śliwińska-Mossoń M, Milnerowicz H (2017) The impact of smoking on the development of diabetes and its complications. Diabetes Vasc Dis Res 14(4):265–276
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G (2014) Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol 43(1):61–68
2. Classification and Diagnosis of Diabetes (2021) Standards of Medical Care in Diabetes-2021. Diabetes Care 44(Suppl 1):S15–s33
Chen X, Crimmins E, Hu PP, Kim JK, Meng Q, Strauss J et al (2019) Venous blood-based biomarkers in the China Health and Retirement Longitudinal Study: Rationale, Design, and results from the 2015 Wave. Am J Epidemiol 188(11):1871–1877
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) STUDIES OF ILLNESS IN THE AGED. THE INDEX OF ADL: A STANDARDIZED MEASURE OF BIOLOGICAL AND PSYCHOSOCIAL FUNCTION. JAMA 185:914–919
Lawton MP, Brody EM Assessment of older people (1969) self-maintaining and instrumental activities of daily living. Gerontologist 9(3):179–186
Spector WD, Fleishman JA (1998) Combining activities of daily living with instrumental activities of daily living to measure functional disability. Journals Gerontol Ser B Psychol Sci Social Sci 53(1):S46–57
Liu N, Cadilhac DA, Kilkenny MF, Liang Y (2020) Changes in the prevalence of chronic disability in China: evidence from the China Health and Retirement Longitudinal Study. Public Health 185:102–109
Li H, Wang A, Gao Q, Wang X, Luo Y, Yang X et al (2020) Prevalence of somatic-mental multimorbidity and its prospective association with disability among older adults in China. Aging 12(8):7218
Andresen EM, Malmgren JA, Carter WB, Patrick DL (1994) Screening for depression in well older adults: evaluation of a short form of the CES-D (center for epidemiologic studies Depression Scale). Am J Prev Med 10(2):77–84
Liang Y, Song A, Du S, Guralnik JM, Qiu C (2015) Trends in disability in activities of daily living among Chinese older adults, 1997–2006: the China Health and Nutrition Survey. The journals of gerontology Series A, Biological sciences and medical sciences. 70(6):739–745
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults: evidence for a phenotype. Journals Gerontol Ser Biol Sci Med Sci 56(3):M146–156
Park SW, Goodpaster BH, Strotmeyer ES, Kuller LH, Broudeau R, Kammerer C et al (2007) Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes Care 30(6):1507–1512
Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC (2001) Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke 32(10):2426–2432
Morley JE (2008) Diabetes, Sarcopenia, and frailty. Clin Geriatr Med 24(3):455–469 vi
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R et al (2017) Heart Disease and Stroke Statistics-2017 update: a Report from the American Heart Association. Circulation 135(10):e146–e603
Ambrose JA, Barua RS (2004) The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol 43(10):1731–1737
Yang Y, Peng N, Chen G, Wan Q, Yan L, Wang G et al (2022) Interaction between smoking and diabetes in relation to subsequent risk of cardiovascular events. Cardiovasc Diabetol 21(1):14
Lou H, Dong Z, Zhang P, Shao X, Li T, Zhao C et al (2018) Interaction of diabetes and smoking on stroke: a population-based cross-sectional survey in China. BMJ open 8(4):e017706
Wang J, Xie H, Fisher JF (2011) Multilevel models: applications using SAS®. Walter de Gruyter
Acknowledgements
We are grateful to all China Health and Retirement Longitudinal Study (CHARLS) participants and research team.
Funding
This study was supported by Natural Science Foundation of Fujian Province (2023J05043), Social Science Fund of Fujian Province (FJ2023BF078), and Young and Middle-aged Teacher Education Research Foundation of Fujian Province (JAT220103).
Author information
Authors and Affiliations
Contributions
HH, RT and SW conceived and designed this manuscript. HC, SW and CW analyzed and interpreted the data of this study. H.H. wrote the original draft. RT and SW reviewed and edited the manuscript. All authors were contributed to drafting and revising the article approved the final version to be published.
Corresponding author
Ethics declarations
Ethical approval
Ethics approval for the data collection in CHARLS was obtained from the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015).
Informed consent
Informed consent was obtained from all participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, H., Tu, R., Chen, H. et al. Longitudinal trajectories of disability among Chinese adults: the role of cardiometabolic multimorbidity. Aging Clin Exp Res 36, 79 (2024). https://doi.org/10.1007/s40520-024-02732-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-024-02732-8