Abstract
Background
Although multimorbidity is a risk factor for disability, the relationship between the accumulative patterns of multimorbidity and disability remains poorly understood. The objective of this study was to identify the latent groups of multimorbidity trajectories among mid to older age adults and to examine their associations with incident disability.
Methods
We included 5,548 participants aged ≥ 45 years who participated in the China Health and Retirement Longitudinal Study from 2011 to 2018 and had no multimorbidity (≥ 2 chronic conditions) at baseline. The group-based multi-trajectory modeling was used to identify distinct trajectory groups of multimorbidity based on the latent dimensions underlying 13 chronic conditions. The association between multimorbidity trajectories and incident disability was analyzed using the generalized estimating equation model adjusting for potential confounders.
Results
Of the 5,548 participants included in the current analysis, 2,407 (43.39%) developed multimorbidity during the follow-up. Among participants with new-onset multimorbidity, four trajectory groups were identified according to the combination of newly diagnosed diseases: “Cardiometabolic” (N = 821, 34.11%), “Digestive-arthritic” (N = 753, 31.28%), “Cardiometabolic/Brain” (N = 618, 25.68%), and “Respiratory” (N = 215, 8.93%). Compared to participants who did not develop multimorbidity, the risk of incident disability was most significantly increased in the “Cardiometabolic/Brain” trajectory group (OR = 2.05, 95% CI: 1.55–2.70), followed by the “Cardiometabolic” (OR = 1.96, 95% CI: 1.52 –2.53) and “Digestive-arthritic” (OR = 1.70, 95% CI: 1.31–2.20) trajectory groups.
Conclusions
The growing burden of multimorbidity, especially the comorbid of cardiometabolic and brain diseases, may be associated with a significantly increased risk of disability for mid to older age adults. These findings improve our understanding of multimorbidity patterns that affect the independence of living and inform the development of strategies for the primary prevention of disability.
Similar content being viewed by others
Background
Older adults living with disability and impaired physical function may have a significantly increased risk of mortality and worse quality of life [1,2,3,4]. Over 45% of older adults aged 60 years and above have difficulty performing daily activities [5]. A growing body of literature suggests a strong association between chronic diseases and loss of physical functioning. Prior studies have confirmed that the level of disability increases with a higher number of chronic diseases [6, 7]. With advances in medical care and longer life expectancy, a growing percentage of adults are living with multiple chronic diseases [8]. The prevalence of multimorbidity, defined as the co-existence of two or more medical conditions within a person [9], is estimated to be 34 to 61% in older adults [10], which is associated with a higher risk of disability, [11,12,13,14,15] poor quality of life, [16, 17] and mortality [18]. Moreover, former studies have demonstrated a trend toward the earlier onset of multimorbidity [19]. Multimorbidity has become common in mid-life in many countries [20, 21]. For instance, a Canadian study showed that the prevalence of multimorbidity was 30% among adults aged 45 to 49 years, 34% among 50 to 54 years, and 45% among 55 to 59 years [20]. It is important to understand how multimorbidity contributes to the development of disability for mid to older age adults.
Most research to date has analyzed multimorbidity as a binary variable or the count of chronic conditions, which may be insufficient to reflect the heterogeneity of chronic diseases comprising multimorbidity. Recent studies suggest that persons affected by specific combinations of chronic conditions may have a particularly high risk of disability [22, 23]. For example, Marengoni and colleagues identified six unique multimorbidity patterns: psychiatric, musculoskeletal/respiratory/gastrointestinal, sensory impairment/cancer, metabolic/sleep disorders, cardiovascular/anemia/dementia, and an unspecific pattern. Compared to older adults with the unspecific pattern, those with the cardiovascular/anemia/dementia, musculoskeletal/respiratory/gastrointestinal, and sensory impairment/cancer patterns had an increased risk of impairment in activities of daily living (ADL) and instrumental activities of daily living (IADL) [24]. However, previous studies of multimorbidity and disability have several limitations. First, few studies have investigated the prospective relationship between multimorbidity patterns and disability [22]. Second, little is known about the developmental trajectories of multimorbidity and their impact on disability. Although some studies have started to explore the trajectories of multimorbidity in older adults, most relied on the binary multimorbidity status or the number of diseases. The accumulation patterns of multiple chronic diseases remain largely unknown. Finally, chronic diseases often emerge before the age of 60 after long-term exposure to risk factors, yet few studies have evaluated the trajectories of multimorbidity starting from middle age.
Based on a large and nationally representative sample of mid to older age adults from the China Health and Retirement Longitudinal Study, this study aimed to (1) identify the multimorbidity trajectory groups among mid to older age adults with new-onset multimorbidity, and (2) explore the association between multimorbidity trajectories and incident disability.
Methods
Data source
Data were obtained from the China Health and Retirement Longitudinal Study (CHARLS), a prospective cohort study of adults aged 45 years and above and their partners in China. The study used a multistage probability sampling strategy to select participants. Participants were enrolled in 2011 and were followed up in 2013, 2015, and 2018. Detailed study design of the CHARLS is available elsewhere [25].
A total of 17,708 individuals completed the baseline survey. Of these, 15,186 were surveyed at wave 2 (2013), 13,565 at wave 3 (2015), and 11,988 at wave 4 (2018). All participants with one or more missing values in chronic conditions (N = 3,164) were excluded from the data analysis. In addition, all participants who were under the age of 45 years (N = 244) or had multimorbidity (N = 3,032) at baseline were also excluded. Thus, we included 5,548 participants in the current analysis. Further, in analyzing the association between multimorbidity trajectories and incident ADL disability, additional 576 participants were excluded for the following reasons: having missing values in the baseline ADL scale variable, or having ADL disability at baseline. Detailed procedure of sample selection is shown in Fig. 1. The biomedical ethics committee of Peking University approved the CHARLS and written informed consent was obtained from all participants.
Measures
Chronic conditions and multimorbidity
We ascertained the history of 14 chronic diseases by asking “Have you been diagnosed with the following conditions by a doctor”: hypertension, dyslipidemia, diabetes, cancer, chronic lung diseases, liver disease, heart disease, stroke, kidney disease, stomach disease, emotional problems, memory-related disease, arthritis, and asthma. These diseases are the leading causes of death in Chinese and are generally irreversible [26]. The self-reported data on chronic diseases are in high agreement with that based on medical records [27]. All diseases and conditions were defined as a binary variable (1 = present, 0 = absent). Multimorbidity was defined as having two or more of any aforementioned diseases. Participants who were qualified as having multimorbidity during follow-up would be defined as having a new onset of multimorbidity, with all participants free of multimorbidity at baseline.
Physical function assessment
We used the Chinese version of the Katz Activities of Daily Living (ADL) scale to measure disability [28]. This scale assessed perceived difficulties in the six ADLs, including dressing, bathing, eating, getting into and out of bed, toileting, and controlling urination and defecation. Following previous studies [29], participants were classified as having ADL disability if they reported having any degree of difficulties in performing at least one ADL. Otherwise, they were considered as having no ADL disability. Participants who had no disability at baseline but were qualified as having ADL disability at any wave of follow-up were considered as developing an incident ADL disability.
Covariates
We included the following baseline variables as covariates: age (45–59, 60 + years), sex (male, female), self-rated health (poor, fair, good) [30], education (no formal education, primary school, middle school or above), body mass index (BMI) (underweight: < 18.5 kg/m2, normal: 18.5–22.9 kg/m2, overweight: 23.0–27.4 kg/m2, obesity: ≥ 27.5 kg/m2), [31] occupation (agricultural, non-agricultural, unemployed/retired), ever smoking (no, yes), alcohol drinking (no, yes), sleep duration (< 7 h/day, 7–8 h/day, > 8 h/day), marital status (married/cohabitation, single: divorced, separated, widowed, or never married), annual household expenditure (≤ 2800 yuan, 2801–4846 yuan, 4847–8325 yuan, > 8325 yuan), social participation (whether the respondent participated in any social activities), location of residence (rural, urban) and public health insurance status (no, yes).
Statistical analyses
The multimorbidity trajectory groups were derived according to the longitudinal data of chronic conditions. But due to the high dimensionality of the longitudinal data of chronic conditions, we cannot directly derive the trajectory groups. To address this challenge, we first used exploratory factor analysis (EFA) to construct multimorbidity patterns to reduce the dimensionality of the 14 chronic conditions. We then calculated the corresponding factor scores of the multimorbidity patterns and used the factor scores as the outcome variables in deriving trajectory of the multimorbidity using the group-based multi-trajectory modeling (GBMTM).
We used EFA to determine the latent multimorbidity patterns underlying the 14 chronic conditions in the baseline sample. The patterns were determined based on their interpretability. We used the weighted least squares means and variance (WLSMV) estimator to estimate the EFA model [32]. We evaluate the goodness of fit by the comparative fit index (CFI), standardized root mean square residual (SRMR), root mean squared error of approximation (RMSEA), and tucker and lewis index (TLI) [33,34,35]. For better interpretations, an oblique rotation of factor loading matrices was performed, with each resulting factor loading representing the strength of association between each condition and the latent multimorbidity patterns. A factor loading of ≥ 0.40 indicates a strong association. The multimorbidity patterns were named according to the conditions that were most strongly associated with them. After identifying the latent multimorbidity patterns at baseline, we estimated the factor scores for each pattern over the follow-up using factor loadings of the multimorbidity patterns at baseline. The multimorbidity pattern score ranged between -0.31 and 2.68, with a higher score suggesting a greater number of conditions belonging to a specific multimorbidity pattern. We excluded conditions with a prevalence of < 1.0% in the baseline sample to achieve better robustness [36].
Based on the longitudinal factor scores of multimorbidity patterns, we identified subgroups of participants with similar joint trajectories of the multidimensional scores using the GBMTM. In this model, the outcome variables were the factor scores of each multimorbidity pattern over the follow-up, and these variables were modeled using the censored normal distribution by setting the lowest score (-0.31) as the censored minimum and the highest score (2.68) as the censored maximum. Based on previous research on multimorbidity trajectories in Korean older adults [37], we hypothesized that there would be 2–6 distinct trajectories of multimorbidity. Model fitting proceeded iteratively by comparing models with a varying number of groups (2–6 groups) and shapes of trajectories (linear, quadratic, and cubic). Model selection was based on the Bayesian information criterion (BIC) and Akaike’s information criterion (AIC) value, in which the model with the lowest BIC and AIC value was preferred. In addition, an ideal model is one in which the proportion assigned to each trajectory group (based on the maximum posterior probability rule) is greater than 5%; the average posterior probability of group membership is at least 0.7. Finally, the final models should have sufficient clinical relevance and interpretability [38].
We used the generalized estimating equation (GEE) model with an independent correlation matrix to evaluate the association between multimorbidity trajectories and incident disability. The independent variable was multimorbidity trajectory group, with participants without multimorbidity as the referent group. The dependent variable was disability status (yes, no) which was modeled with a logit link function. All variables included in this study were repeatedly measured in 2011, 2013, 2015, and 2018. Three models were fitted consecutively: model 1 was adjusted for time, model 2 was additionally adjusted for sociodemographic characteristics (age, gender, marital status, living area, occupation, annual household expenditure, social participation, and public health insurance status), and model 3 was further adjusted for health-related characteristics (self-rated health, BMI, smoking, alcohol drinking, and sleep duration). We reported the odds ratios (ORs) with 95% confidence intervals (CIs) of the association between multimorbidity trajectory groups and disability. We tested the interaction between multimorbidity trajectory groups and time in the GEE model, but the interaction was not statistically significant, therefore the interaction term was not included in the models.
The EFA analyses were performed with Mplus version 8.0, the GBMTM was conducted using the “Traj” program in Stata version 16.0 (StataCorp, College Station, TX) [39], and the GEE model was fitted using R 4.1.2. A two-sided P value < 0.05 was considered statistically significant.
Sensitivity analysis
We conducted a set of sensitivity analyses: First, we performed three EFA using the cross-sectional data from 2013, 2015, and 2018 waves of CHARLS to assess the robustness of the EFA, where we included the same chronic conditions as those at baseline to make the results comparable with those of the main analysis. Second, to evaluate the influence of incomplete data on the trajectory analysis, we conducted sensitivity analysis by restricted participants with complete data for at least 3 waves (N = 5,888). Third, to evaluate the effects of the excluded sample, the characteristics from samples with and without participants who were excluded during sample selection were compared and fitted the GEE model regarding the association of multimorbidity and incident disability among those excluded from the current analysis. Fourth, we conducted an analysis that only excluded participants with multimorbidity at baseline (N = 6,630) to assess the impact of the excluded sample on the study results. Finally, we divided participants without multimorbidity into no morbidity and single morbidity groups to examine the impact of single morbidity on the association between multimorbidity trajectories and incident disability using the GEE model.
Results
Baseline characteristics
Of the 5,548 participants included in the current analysis, 2,407 (43.39%) developed multimorbidity during the follow-up. Detailed sample characteristics, as well as the differences between participants with and without new-onset multimorbidity, are presented in Supplemental Table 1. Briefly, participants who developed multimorbidity tended to be female, older, overweight or obese, unemployed or retired, and report poorer self-rated health, disability, and shorter sleep duration at baseline compared to those without multimorbidity (all P < 0.05). Compared to those included in the current analyses, excluded participants were more likely to be female, older, overweight or obese, unemployed or retired, single, and report no formal education, poorer self-rated health, disability, and shorter sleep duration (Supplemental Table 2).
Exploratory factor analysis of latent multimorbidity patterns
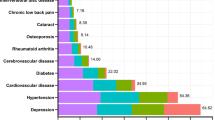
The exploratory factor analysis included 13 chronic diseases with a prevalence of > 1% in the current sample (Fig. 2). We identified four latent multimorbidity patterns: 1) a “Cardiometabolic” pattern characterized by high correlations with heart diseases, hypertension, diabetes, and dyslipidemia; 2) a “Brain” pattern characterized by stroke, memory-related disease, and emotional problems; 3) a “Digestive-arthritic” pattern which was strongly correlated with kidney disease, liver disease, digestive disease, and arthritis; and 4) a “Respiratory” pattern which was correlated with chronic lung diseases and asthma. We identified similar patterns using the cross-sectional data from 2013, 2015, and 2018 waves of CHARLS (Supplemental Figures 1–3), suggesting the robustness of the EFA.
Group-based multi-trajectory modeling of multimorbidity trajectories
Among mid to older age adults who developed multimorbidity, four distinct groups of multimorbidity trajectories were identified based on the joint trajectories of the four multimorbidity pattern scores (Fig. 3). The resulting trajectory groups were named according to the patterns with the most prominent increasing trend, indicating that the trajectory group was dominated by the disease growth of these multimorbidity patterns in the process of no multimorbidity to multimorbidity. Specifically, the first group showed the most prominent increasing trend in the “Cardiometabolic” multimorbidity pattern score, and therefore named “Cardiometabolic” trajectory (N = 821, 34.11%). Similarly, the second group was named “Digestive-arthritic” trajectory (N = 753, 31.28%), the third group was named “Cardiometabolic/Brain” trajectory (N = 618, 25.68%), and the fourth group was named “Respiratory” trajectory (N = 215, 8.93%). In a sensitivity analysis that restricted to participants with complete data for at least 3 waves, the multimorbidity trajectories were similar to those from the main analyses (Supplemental Fig. 4).
Baseline characteristics associated with multimorbidity trajectories
Table 1 presents the baseline characteristics by multimorbidity trajectory groups. There were significant differences in sex, age, self-rated health, education, BMI, occupation, disability, cigarette smoking, sleep duration, and location of residence across multimorbidity trajectories. Of particular note, participants with the “Digestive-arthritic” and the “Respiratory” trajectories were much more likely to report poor self-rated health, and participants with the “Cardiometabolic/Brain” and the “Cardiometabolic” trajectories were much more likely to have a BMI ≥ 27.5 kg/m2 (all P < 0.001).
Association between multimorbidity trajectories and incident disability
Table 2 summarizes the association between multimorbidity trajectory groups and incident disability using the GEE model. In the fully adjusted model, the “Cardiometabolic/Brain” (OR = 2.05, 95% CI: 1.55–2.70) trajectory group had the highest increased risk of disability, followed by the “Cardiometabolic” (OR = 1.96, 95% CI: 1.52 -2.53) and “Digestive-arthritic” (OR = 1.70, 95% CI: 1.31–2.20) trajectory groups, but no significant associations were observed with the “Respiratory” trajectory group.
Among excluded participants, those with multimorbidity had a significantly increased risk of disability compared to those without multimorbidity (OR = 1.64, 95% CI: 1.41–1.90). (Supplemental Table 3) In the analysis that only excluded participants with multimorbidity at baseline, the multimorbidity trajectories and their impact on incident disability were similar to those from the main analyses. (Supplemental Figure 5 and Table 4) In a sensitivity analysis evaluating the impact of single morbidity on the association between multimorbidity trajectories and incident disability, compared with participants without any morbidity, participants with single morbidity had a significantly increased risk of disability (OR = 1.33, 95% CI: 1.02 -1.73), and the multimorbidity trajectory groups were still significantly associated with a higher risk of disability. (Supplemental Table 5).
Discussion
Based on a large, nationally representative sample of Chinese adults, we examined the joint developmental trajectories of multimorbidity among mid to older age adults. Four groups of multimorbidity trajectories were identified, which were characterized by the most prominent increasing trend in the factor scores of the “Cardiometabolic,” “Digestive-arthritic,” “Cardiometabolic/Brain,” and “Respiratory” multimorbidity patterns, respectively. For multimorbidity trajectory groups, compared to those who did not develop multimorbidity, except for the “Respiratory” trajectory group, the “Cardiometabolic,” “Digestive-arthritic,” and the “Cardiometabolic/Brain” trajectory groups had a significantly higher risk of disability. Our findings highlight the importance of the prevention and management of chronic diseases, especially cardiometabolic and brain diseases, in reducing disability in mid to older age adults.
Our findings confirm the complexity and heterogeneity of multimorbidity and its impact on functional health, suggesting the need to look beyond the count of chronic conditions to assess its effect on older adults’ health [40]. Our study contributes to the growing literature on the latent clustering of chronic conditions. For instance, in another study based on the CHARLS data, Yao et al. identified four multimorbidity patterns using factor analysis, including the respiratory, hepatic-renal-skeletal, cardio-metabolic, and arthritic-digestive-visual patterns. [36] Jackson et al. identified three multimorbidity patterns by factor analysis, including the neurological/mental health, cardiovascular, and musculoskeletal/somatic patterns, and found that older adults with the cardiovascular pattern showed the greatest decline in ADL over 6 years of follow-up [41]. However, few studies have examined the longitudinal change in disease clustering, which may be more efficient than studies of single disease. Our study fills in the gap by modeling the joint trajectories of multimorbidity pattern scores underlying chronic disease, which offers new insights into the dynamic accumulation process of multimorbidity.
Our findings suggest that the growing burden of cardiometabolic disease contributed most significantly to the risk of disability. This is consistent with previous studies showing a positive association of metabolic multimorbidity with a higher risk of disability [42], cardiovascular outcomes, and mortality [43]. Similar to our findings, a recent study based on the CHARLS suggested that the older adults who exhibited the “cardiometabolic” and the “stomach/arthritis” patterns of multimorbidity were at greater risk of function decline when developing a new chronic disease. However, this study did not examine the risk associated with specific types of newly-onset diseases [44]. In addition, our findings highlight a significantly increased risk of disability in adults with an increasing burden of arthritic, digestive, and brain diseases. Similar to these findings, a recent analysis based on the Health and Retirement Study suggested that a multimorbidity characterized by arthritis, hypertension, and depression may be associated with the highest risk of disabilities [12]. The accumulation of chronic diseases could be a result of aging-related physiological processes such as chronic inflammation, which may be the root causes leading to the disability [45]. It has been documented that the levels of inflammatory markers were different by multimorbidity patterns, with the highest level of inflammation in the cardiovascular pattern [46]. Other shared common etiologic mechanisms underlying the cardiometabolic, arthritic, digestive, and brain diseases may also explain the increased risk of disability, which warrants future research. The results of this study highlight the importance of developing and delivering interventions to manage multimorbidity to reduce the risk of ADL disability among mid to older age adults. Furthermore, since most chronic conditions could be due to unhealthy behaviors, such as smoking and lack of physical activity, more efforts are needed to promote healthy living among mid to older age adults.
To our knowledge, this is the first study to identify the latent developmental trajectory of multiple chronic diseases by leveraging the dimension-reducing capability of exploratory factor analysis. In addition, the current study estimated multimorbidity trajectory in mid to older age adults using a novel multi-trajectory approach. The GBMTM method accounted for the co-development of the multimorbidity pattern, which provides a greater understanding of the complexity of multimorbidity accumulation. Our findings reveal clinically meaningful patterns of multimorbidity development, which have important implications for the primary prevention of disability.
This analysis has several limitations. First, our measurement of multimorbidity was limited to 14 chronic conditions that were self-reported by study participants, which may not be reliable or comprehensive. Findings could be different if a wide scope of chronic conditions were considered along with detailed parameters of the conditions (e.g. severity or duration). Second, some trajectory groups were relatively small, which may lead to limited power. Third, functional assessments in the CHARLS study were self-reported, which may have led to an inaccurate estimate of the true prevalence of disability. Future studies should evaluate disability using more objective measurements, such as walking speed and the grip strength test. Finally, because this study selected participants who participated in all four waves of CHARLS, the results are not free from selection bias and influences of attrition. Compared to those excluded from the current analyses, included participants were healthier. Therefore, findings should be interpreted with caution with full consideration of sample characteristics and the potential for selection bias. However, in the sensitivity analysis that only excluded participants with multimorbidity at baseline, the results were similar to those from the main analyses, suggesting that our findings are robust.
Conclusions
There was great heterogeneity in the development of multimorbidity among mid to older age adults in China. For mid to older age adults, multimorbidity trajectory groups are characterized by high increases in the “Cardiometabolic,” “Digestive-arthritic,” and “Cardiometabolic/Brain” multimorbidity patterns were associated with a significantly increased risk of disability. Findings from this study highlight the importance of developing and providing interventions for managing and preventing multimorbidity to reduce disability among mid to older age adults.
Availability of data and materials
The analytical dataset used in this study is a publicly available dataset released by the CHARLS. Information about the data source and available data are found at https://charls.charlsdata.com/pages/data/111/zh-cn.html. Researchers can obtain these data after submitting a data use agreement to the CHARLS team.
Abbreviations
- CHARLS:
-
China Health and Retirement Longitudinal Study
- ADL:
-
Activities of daily living
- IADL:
-
Instrumental activities of daily living
- BIC:
-
Bayesian information criterion
- AIC:
-
Akaike’s information criterion
- EFA:
-
Exploratory factor analysis
- GBMTM:
-
Group-based multi-trajectory modeling
- WLSMV:
-
Weighted least squares means and variance
- CFI:
-
Comparative fit index
- TLI:
-
Tucker and lewis index
- RMSEA:
-
Root mean squared error of approximation
- SRMR:
-
Standardized root mean square residual
- GEE:
-
Generalized estimating equation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Ferraro KF, Su Y-P, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: a 20-year panel study. Am J Public Health. 2002;92(5):834–40.
Schoeni RF, Martin LG, Andreski PM, Freedman VA. Persistent and growing socioeconomic disparities in disability among the elderly: 1982–2002. Am J Public Health. 2005;95(11):2065–70.
Guralnik JM, Ferrucci L, Balfour JL, Volpato S, Di Iorio A. Progressive versus catastrophic loss of the ability to walk: implications for the prevention of mobility loss. J Am Geriatr Soc. 2001;49(11):1463–70.
Millán-Calenti JC, Tubío J, Pita-Fernández S, González-Abraldes I, Lorenzo T, Fernández-Arruty T, Maseda A. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr. 2010;50(3):306–10.
Department of Economic and Social Affairs. Ageing and disability. UN 2015. https://www.un.org/development/desa/disabilities/disability-and-ageing Accessed.
Rizzuto D, Melis RJF, Angleman SB, Qiu C, Marengoni A. Effect of chronic diseases and multimorbidity on survival and functioning in elderly adults. J Am Geriatr Soc. 2017;65(5):1056–60.
Guido D, Perna S, Peroni G, Guerriero F, Rondanelli M. A comorbidity prognostic effect on post-hospitalization outcome in a geriatric rehabilitation setting: the pivotal role of functionality, assessed by mediation model, and association with the Brass index. Aging Clin Exp Res. 2015;27(6):849–56.
Fortin M, Hudon C, Haggerty JL, Akker Mvd, Almirall J. Prevalence estimates of multimorbidity: a comparative study of two sources. BMC Health Serv Res. 2010;10(1):1–6.
Akker Mvd, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity: what’s in a name ? A review of literature. Eur J Gen Prac. 1996;2(2):65–70.
Griffith LE, Gilsing AMJ, Mangin D, Patterson CJ, van den Heuvel ER, Sohel N, St John PD, van den Akker M, Raina P. Multimorbidity frameworks impact prevalence and relationships with patient important outcomes. J Am Geriatr Soc. 2019;67(8):1632–40.
Jindai K, Nielson CM, Vorderstrasse BA, Quiñones AR. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005–2012. Prev Chronic Dis. 2016;13:E151.
Quiñones AR, Markwardt S, Botoseneanu A. Multimorbidity combinations and disability in older adults. J Gerontol A Biol Sci Med Sci. 2016;71(6):823–30.
Bleijenberg N, Zuithoff NPA, Smith AK, de Wit NJ, Schuurmans MJ. Disability in the individual ADL, IADL, and mobility among older adults: A prospective cohort study. J Nutr Health Aging. 2017;21(8):897–903.
Hajek A, König HH. Longitudinal predictors of functional impairment in older adults in Europe–evidence from the survey of health, ageing and retirement in Europe. PLoS One. 2016;11(1):e0146967.
Rivera-Almaraz A, Manrique-Espinoza B, Avila-Funes JA, Chatterji S, Naidoo N, Kowal P, Salinas-Rodríguez A. Disability, quality of life and all-cause mortality in older Mexican adults: association with multimorbidity and frailty. BMC Geriatr. 2018;18(1):1–9.
Pati S, Swain S, Hussain MA, van den Akker M, Metsemakers J, Knottnerus JA, Salisbury C. Prevalence and outcomes of multimorbidity in South Asia: a systematic review. BMJ Open. 2015;5(10):e007235.
Gu J, Chao J, Chen W, Xu H, Zhang R, He T, Deng L. Multimorbidity and health-related quality of life among the community-dwelling elderly: a longitudinal study. Arch Gerontol Geriatr. 2018;74:133–40.
Prince MJ, Wu F, Guo Y, Robledo LMG, o Donnell M, Sullivan R, Yusuf S. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–62.
Wister AV, Li L, Mitchell BA. A Study of social isolation, multimorbidity and multiple role demands among middle-age adults based on the Canadian longitudinal study on aging. Int J Aging Hum Dev. 2021;94(3):312–43.
Sakib MN, Shooshtari S, St John PD, Menec VH. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: an analysis of Canadian Longitudinal Study on Aging data. BMC Public Health. 2019;19(1):1–13.
Bowling CB, Deng L, Sakhuja S, Morey MC, Jaeger BC, Muntner PM. Prevalence of Activity Limitations and Association with Multimorbidity Among US Adults 50 to 64 Years Old. J Gen Intern Med. 2019;34(11):2390–6.
Marengoni A, Angleman SB, Fratiglioni L. Prevalence of disability according to multimorbidity and disease clustering: a population-based study. J Comorbidity. 2011;1(1):11–8.
Grande G, Marengoni A, Vetrano DL, Roso-Llorach A, Rizzuto D, Zucchelli A, Qiu C, Fratiglioni L, Calderón-Larrañaga A. Multimorbidity burden and dementia risk in older adults: The role of inflammation and genetics. Alzheimers Dement. 2021;17(5):768–76.
Marengoni A, Akugizibwe R, Vetrano DL, Roso-Llorach A, Onder G, Welmer A-K, Calderón-Larrañaga A. Patterns of multimorbidity and risk of disability in community-dwelling older persons. Aging Clin Exp Res. 2021;33(2):457–62.
Zhao Y, Hu Y-S, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Marengoni A, Rizzuto D, Wang H-X, Winblad B, Fratiglioni L. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. 2009;57(2):225–30.
Kriegsman DMW, Penninx BWJH, van Eijk JTM, Boeke AJP, Deeg DJH. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol. 1996;49(12):1407–17.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–9.
Lestari SK, Ng N, Kowal P, Santosa A. Diversity in the factors associated with ADL-related disability among older people in six middle-income countries: a cross-country comparison. Int J Environ Res Public Health. 2019;16(8):1341.
Adeyemi OJ, Gill TL, Paul R, Huber LRB. Evaluating the association of self-reported psychological distress and self-rated health on survival times among women with breast cancer in the U.S. PLoS One. 2021;16(12):e0260481.
Nishida C. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet. 2004;363:157–63.
Muthén B. A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika. 1984;49(1):115–32.
Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods Research. 1992;21(2):230–58.
Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55.
Brown TA. Confirmatory factor analysis for applied research. 2nd ed. New York: The Guilford Press; 2015.
Yao S, Cao G, Han L, Huang Z, Chen Z, Su H, Hu Y, Xu B. Associations between somatic multimorbidity patterns and depression in a longitudinal cohort of middle-aged and older Chinese. J Am Med Dir Assoc. 2020;21(9):1282–7.
Lee SA, Joo S, Chai HW, Jun HJ. Patterns of multimorbidity trajectories and their correlates among Korean older adults. Age Ageing. 2021;50(4):1336–41.
Nagin DS, Jones BL, Passos VL, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018;27(7):2015–23.
Jones BL, Nagin DS. A note on a Stata plugin for estimating group-based trajectory models. Sociological Methods & Research. 2013;42(4):608–13.
Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. 2009;265(2):288–95.
Jackson CA, Jones M, Tooth L, Mishra GD, Byles J, Dobson AJ. Multimorbidity patterns are differentially associated with functional ability and decline in a longitudinal cohort of older women. Age Ageing. 2015;44(5):810–6.
Zhao Y, Zhang P, Lee JT, Oldenburg B, van Heusden A, Haregu TN, Wang H. The prevalence of metabolic disease multimorbidity and its associations with spending and health outcomes in middle-aged and elderly Chinese adults. Front Public Health. 2021;9:456.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, Rinfret S, Schiffrin EL, Eisenberg MJ. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32.
Liu H, Zhang X, Chen B, Fang B, Lou VWQ, Hu J. The Differential Impact of Multimorbidity Patterns and Subsequent Accumulation on Longitudinal Trajectories of Physical Function Decline in a Population-based Cohort of Older People. J Gerontol A Biol Sci Med Sci. 2022;77(8):1629–36.
Ferrucci L, Gonzalez-Freire M, Fabbri E, Simonsick EM, Tanaka T, Moore ZA, Salimi S, Sierra F, de Cabo R. Measuring biological aging in humans: A quest. Aging Cell. 2020;19(2):e13080.
Marengoni A, Roso-Llorach A, Vetrano DL, Fernández S, Guisado-Clavero M, Violán C, Calderón-Larrañaga A. Patterns of multimorbidity in a population-based cohort of older people: sociodemographic, lifestyle, clinical, and functional differences. J Gerontol A Biol Sci Med Sci. 2020;75(4):798–805.
Acknowledgements
The authors would like to thank China Health and Retirement Longitudinal Study participants and researchers for their contributions to this important study.
Funding
This work was supported by the National Natural Science Foundation of China (Grant number 81973144 and 82103951). The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Z. S. and Z. Z. conceived the study. Z. S., Z. Z., and Y. F. developed the analytic plan. Z.S., Z. Z., K. S., B. Y., Z. J., L.Y., and J. L. obtained data and performed data analyses. Z. S., and Y.F. obtained funding for the study. All authors provided critical input on the interpretation of the results. Z. S., and Z. Z. drafted the initial manuscript. All authors critically revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. The ethical approvement and experimental protocols were approved by the institutional review board of Peking University (IRB00001052-11015). Informed consent has been acquired from all participants before the participation.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, Z., Zhang, Z., Shi, K. et al. Association between multimorbidity trajectories and incident disability among mid to older age adults: China Health and Retirement Longitudinal Study. BMC Geriatr 22, 741 (2022). https://doi.org/10.1186/s12877-022-03421-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03421-9