Abstract
Introduction
Sarcopenia is defined by a loss of muscle mass and function associated with mortality, decreased physical performance, falls, and disability. Since chronic inflammation and decreased physical activity are risk factors for developing sarcopenia, it is critical to assess the role of sarcopenia in immune-mediated rheumatic diseases (IMRDs). Moreover, nutritional interventions are emerging as key modifiable and affordable options to improve physical performance in sarcopenia.
Objective
The aim of this review is to critically summarize current information on the evidence linking nutritional interventions and sarcopenia in IMRDs.
Methods
The search and selection of articles was performed in Medline, Dimensions.ai, Google Scholar, Cochrane Library, Epistemonikos, and Trip Database. The results were clustered into three areas: sarcopenia and IMRDs, sarcopenia and biological disease-modifying antirheumatic drugs (bDMARDs), and nutritional interventions for sarcopenia.
Findings
Several cross-sectional studies have shown a higher prevalence of sarcopenia in IMRDs, such as rheumatoid arthritis. Although not fully established, evidence linking sarcopenia and other IMRDs (ankylosing spondylitis and systemic sclerosis) has been also described. For secondary sarcopenia prevention and treatment, bDMARDs’ administration proved efficacy in patients with rheumatoid arthritis. Furthermore, there is growing evidence linking nutrition to the prevention and treatment of sarcopenia. Evidence linking unfavourable results in nutritional risk assessment, insufficient intake of protein, vitamin D, antioxidant nutrients, and long-chain polyunsaturated fatty acids and sarcopenia have been reported.
Conclusion
Given that sarcopenia and IMRDs have strong links, further research is needed to improve patient care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia is a generalized musculoskeletal disorder characterized by loss of muscle mass and function together with decreased physical performance. Loss of muscle mass and function leads to a higher risk of falls and hospitalization rates, decreases the ability to perform activities of daily living, increases functional impairment, worsens quality of life, and increases morbidity [1,2,3].
Sarcopenia is highly prevalent in older patients and is an important factor contributing to frailty and disability, generating a significant social and economic burden [4]. Sarcopenia prevalence in the community is highly variable (3–24%) as a result of the range of diagnostic criteria and definitions used [5].
Apart from age, sarcopenia-related risk factors include nutritional deficiencies, sedentarism, decreased protein synthesis and regeneration, inflammation, and hormonal and cytokine imbalance, among others [6, 7].
The definition, diagnosis, and assessment of sarcopenia is well described in the literature. The EWGSOP (European Working Group on Sarcopenia Older People) definition of sarcopenia put muscle strength to the forefront, as it is recognised that strength is better than mass in predicting adverse outcomes. In addition, it recommends an algorithm for case finding, diagnosis, and determination of the severity of sarcopenia [2, 3, 8, 9].
Methods
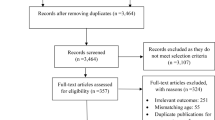
The literature search for this scoping review was conducted in the following databases since 2014 and in English: Medline, Dimensions.ai, Google Scholar, and Cochrane Library and the evidence-based medicine repositories: Epistemonikos and Trip Database, with the search completion date 11/29/2019. Search strings were performed on the above databases constructed from the term nutritional interventions and/or immune-mediated rheumatic diseases and/or sarcopenia and all their equivalents or synonyms as input terms into the MeSH (Medical Subject Headings) database, the NLM (National Library of Medicine) controlled vocabulary thesaurus. For screening, a restriction was made to those papers included older adults with sarcopenia and diagnosis immune-mediated rheumatic diseases (specifically rheumatoid arthritis, ankylosing spondylitis, and systemic sclerosis). A secondary manual literature search of the selected studies was also conducted to detect possible omissions that could be of interest. Articles were selected in pairs and reviewed in full text to give a detailed view of this complex field. The results were clustered into three areas: sarcopenia and immune-mediated rheumatic diseases (IMRDs); sarcopenia, immune-mediated rheumatic diseases and biological disease-modifying antirheumatic drugs (bDMARDs); and nutritional interventions for sarcopenia.
Sarcopenia and immuno-mediated rheumatic diseases
IMRDs are accompanied by inflammation, especially joint inflammation, causing pain, joint dysfunction, and destruction, decreased physical activity and quality-of-life impairment. Since decreased physical activity and chronic inflammation are risk factors for sarcopenia, it seems relevant to assess the prevalence of sarcopenia and its association with inflammatory markers, and rheumatic disease course and activity, among others, in patients with IMRDs.
Inflammatory markers in sarcopenia
Chronic inflammation is a risk factor for developing sarcopenia, because it facilitates muscle catabolism [10]. It is not clear which serum inflammatory molecules are associated with loss of muscle mass and strength and physical performance and which, as such, may be candidates for sarcopenia biomarkers [11].
A cross-sectional study exploring neuromuscular, peripheral pro‐inflammatory, and oxidative stress molecules as potential biomarkers associated with sarcopenia in old-aged people with hip fracture only found differences in peripheral TNF‐α levels and catalase activity. Probably, TNF‐α and catalase are markers of an early inflammatory reaction that is impaired in subjects with sarcopenia [12].
A randomized-controlled trial (RCT) published in 2019 evaluated the association between body composition and inflammatory markers in 1,121 healthy individuals between 65 and 79 years old. It found that muscle mass [assessed by skeletal muscle mass index (SMI): appendicular skeletal muscle mass (ASMM)/height2] negatively correlates with proinflammatory serum levels of C-reactive protein (CRP), leptin, and alpha-1-acid glycoprotein (AGP), and positively correlates with Ghrelin, in both men and women [13].
High levels of CRP have also been observed in sarcopenia patients in several cross-sectional studies. A systematic review and meta-analysis conducted in 2016 observed a correlation between significantly higher levels of CRP and sarcopenia (defined as muscle mass loss) [11]. In a cross-sectional study, Can et al. [14] showed that patients with sarcopenia (defined by EWGSOP criteria) had higher levels of CRP and adiponectin and a higher erythrocyte sedimentation rate (ESR). ESR was independently associated with sarcopenia (OR = 1.156; 95% CI 1.057–1.263; p = 0.001). In another cross-sectional study, van Atteveld et al. [15] also determined significant inverse correlations between ESR and muscle mass [relative skeletal muscle mass (RMM): skeletal muscle mass (SMM)/weight], muscle strength (grip strength and chair stand test), and physical performance [normal walking speed and timed up and go (TUG)]. Moreover, they observed an association between lower albumin levels and lower muscle strength and physical performance. Otzurk et al. [16] performed a cross-sectional study and observed higher ESR and higher CRP levels in patients with sarcopenia (defined by EWGSOP criteria) than in controls. These authors also analysed the neutrophil/lymphocyte ratio (NLR) and observed an independent association between NLR and sarcopenia (OR = 1.31, 95% CI 1.06–1.62, p = 0.013).
A cross-sectional study included a multivariate analysis of 30 serum inflammatory markers in patients with sarcopenia and frailty, and observed a specific pattern of inflammatory markers, with higher levels of CRP, and lower levels of IL-8, myeloperoxidase (MPO), monocyte chemoattractant protein 1 (MCP1), and platelet-derived growth factor BB (PDGF-BB). This study also showed gender-specific pattern differences: for example, women had higher levels of selectin P and eotaxin, while men had lower levels of IFN-γ, IL-17, and TNF-α, among others [17].
Finally, CRP and IL-8 levels and adiponectin/leptin ratio may have prognostic value for the development of sarcopenia. A longitudinal study that included 336 adults aged 59–70 years of age, with an average follow-up period of 10.8 years, observed significant associations between higher levels of CRP, higher levels of IL-8, and a lower adiponectin/leptin ratio at baseline and the development of sarcopenia (defined by EGWSOP) at the follow-up visit [18].
Sarcopenia and rheumatoid arthritis
Loss of muscle strength in patients with RA may be seen frequently. Longer disease duration and higher disease activity should lead to development of sarcopenia due to chronic inflammation [19].
Several cross-sectional studies have shown a higher prevalence of sarcopenia in patients with rheumatoid arthritis (RA) compared to healthy controls [20,21,22,23,24,25]. The prevalence of sarcopenia described in studies in patients with RA ranges from 7.8% [26] to 87.5% [24]. One of the reasons for these differences is the different criteria and assessment methods for sarcopenia used in each study. Even so, it should be noted that in a cross-sectional study by Tournadre et al. [26] found the same sarcopenia prevalence in RA patients (low, 7.8%) using both the EWGSOP definition (muscle mass and function) and muscle mass alone (SMI: ASMM/height2).
Several studies have analysed factors associated with the development of sarcopenia in patients with RA. Although not fully established, these include, but are not limited to, age, sex, nutritional status, disease activity, and degree of disability.
Gender
Several studies have shown gender differences in the prevalence of sarcopenia in RA patients [23, 27]. In a cross-sectional study, Baker et al. [27] found that muscle mass [measured with appendicular lean mass index (ALMI): ALM/height2] was lower in men than in women (p < 0.0001) and they observed a 3–8 times higher probability of sarcopenia in men in one of the two study cohorts. Male sex was also associated with the development of sarcopenia in the correlation research of sarcopenia, skeletal muscle, and disease activity in RA [28].
Nutritional status
Although body mass index (BMI) has been associated with sarcopenia in previous publications [28,29,30,31,32], many studies show that muscle mass loss is not always associated with lower BMI. The low or no weight loss in these patients is explained by a stable or slightly increased fat mass, i.e., sarcopenic obesity. The concept of sarcopenic obesity is still an evolving one and has not been well studied in rheumatic diseases [33]. One observational study evaluated sarcopenia (defined by SMI) in women with RA vs. healthy controls and concluded that despite having a similar BMI, the prevalence of sarcopenia was significantly higher in patients with RA [20]. Accordingly, one transversal study in men and women with RA correlated sarcopenia (defined by SMI) to normal BMI (OR = 82.1, 95% CI 3.8–1733.3; p = 0.005) and over fat BMI (OR = 12.3; 95% CI 2.27–67.6; p = 0.004) [21]. A cross-sectional study by Vlietstra et al. [34] observed an association between sarcopenia (defined according to muscle mass) and higher fat content (OR = 1.1, 95% CI 1.0–1.2; p < 0.02), and use of glucocorticoids (OR = 1.08; 95% CI 1.0–1.2; p = 0.017) in patients with RA.
Disease activity
The relationship between the presence of sarcopenia and RA activity or severity is not clearly established. Some studies have found no association between sarcopenia and markers of disease activity such as Disease Activity Score 28 (DAS28) [20, 21, 32, 35]. In a cross-sectional study, Barone et al. [35] observed a prevalence of sarcopenia (muscle mass and strength) of about 20% in patients with RA, but no relationship with RA activity. In contrast, disability and age were positively associated in this study with sarcopenia.
Other studies in RA have positively correlated disease duration and activity with sarcopenia. In a longitudinal study of 294 RA patients, Park et al. [36] showed that sarcopenia (defined by SMI) has a prognostic value for increased disease activity (DAS28-ESR) at 3 years (OR = 4.477; 95% CI 1.661–12.067; p = 0.003). Another cross-sectional study in women with RA observed an association between inflammation levels and long-standing RA (CRP levels) and muscle mass (ALMI) [37]. In a case–control study, Reina et al. [30] found that BMI, SMI, and lean appendicular mass are inversely correlated, and that fat mass is directly correlated with disease duration in patients with RA, in both men and women. A cross-sectional study of 388 women with RA observed that disease duration (OR = 1.06; 95% CI 1.04–1.09), joint damage (Steinbrocker’s class, OR = 3.19, 95% CI 1.60–6.53), and age (OR = 1.64; 95% CI 1.26–2.17) were independent factors positively associated with sarcopenia [defined by muscle mass, strength, and function, according to the Asian Working Group on Sarcopenia (AWGS) definition]. However, bDMARDs use (OR = 0.51; 95% CI 0.28–0.93) and a good nutritional status (OR = 0.61; 95% CI 0.51–0.71) were negatively associated with sarcopenia [31].
Other studies have also observed an association between sarcopenia (defined by muscle mass, SMI) and radiographic joint damage (OR = 2.154; 95% CI 1.032–4.497; p = 0.041) [38] and bone erosion (OR = 0.057; 95% CI 0.006–0.532; p = 0.012) in patients with RA [21].
Disability and falls
A cross-sectional study of 240 patients with RA showed no significant relationship between a disability index or RA activity (determined by DAS28-ESR) and sarcopenia (defined by AWGS). Factors associated with sarcopenia in this study were age (OR = 1.08, p = 0.008), BMI (OR = 0.73, p < 0.001), CRP (OR = 1.76, p = 0.017), and hip bone mineral density (BMD) (OR = 0.61, p = 0.037) [32].
CHIKARA is a prospective, observational study that included 100 patients of both sexes with RA. Early analysis showed an independent correlation between sarcopenia (defined by the AWGS definition) and high body fat mass, low BMI, and high matrix metalloproteinase-3 (MMP3) [29]. In a subsequent study, univariate analysis observed that male sex, old age, glucocorticoid use > 5 mg/day, high levels of MMP3, and higher disability evaluated by the Health Assessment Questionnaire (HAQ) were associated with sarcopenia (defined by AWGS) development at 2 years in RA patients [28].
Sarcopenia is a risk factor for fall events. In a cross-sectional study, Vlietstra et al. [34] showed a weak association between sarcopenia (defined by muscle mass) and fatigue in patients with RA. Nevertheless, the analysis of CHIKARA data at 1 year did not show a significant relationship between the risk of fall events and sarcopenia (defined by AWGS). No relationship was observed between the risk of fall events and disease activity and CRP; but height and obesity levels showed a negative correlation with fall events [39].
Bone mineral density
Decreased muscle mass may appear together with decreased bone mass, in what has been named osteosarcopenia [40, 41], but the relationship of sarcopenia, low BMD, and osteoporosis in RA patients is not fully established understood [42].
Confavreux et al. [43] revised the systemic bone effects of biologic therapies in IMRDs (such as RA and ankylosing spondylitis). Feklistov et al. [22] observed osteoporosis (low BMD) in a cross-sectional study among 48% of women with RA versus 45% in healthy controls. Sarcopenia (muscle mass, strength, and physical performance) was observed in 25% of RA patients, and osteosarcopenia (sarcopenia + low BMD) was found in 15%, versus 12.5% and 5% in healthy controls, respectively. TOMORROW study was a prospective cohort that shows data from 208 patients with RA and 205 age- and sex-matched healthy controls [44, 45]. Okano et al. [44] showed lower muscle mass and lower BMD in patients with RA, and a positive correlation between both parameters. In a subsequent subanalysis of this cohort, Inui et al. analysed muscle mass and BMD in individuals > 65 years for a period of 7 years, and observed that muscle mass [determined by appendicular skeletal mass index (ASMI)] is an independent factor associated with BMD change (p = 0.0020) in patients with RA but not in healthy controls [45].
Frailty
Sarcopenia and frailty, defined as physical and cognitive function deterioration in older adults, often overlap [46]. Early detection of frailty and its risk factors, such as sarcopenia, is important for prevention and management. In a cross-sectional study of 282 patients with AR, prevalence of frailty was as high as 21.5%, and 42% of them were older than 65 years. Overall, 31% of patients had sarcopenia (defined by SMI) [47]. In a cross-sectional analysis of CHIKARA study data at 1 year, Tada et al. [48] observed a positive association between sarcopenia (defined by AWGS) and frailty (OR = 3.1; 95% CI 1.2–1.8; p < 0.024). Observed frailty and pre-frailty prevalences were 18.9% and 38.9%, respectively. In these groups, sarcopenia prevalence was 39% and 41%, respectively, and among patients without frailty, it was 18%. Other risk factors were MMP3 levels, age, disease severity, and joint dysfunction, whilst RA treatment was associated negatively with the onset of sarcopenia. Finally, a cross-sectional study of 210 patients with RA and 100 healthy controls found a higher prevalence of frailty among RA patients, showing 16.6% with frailty and 32.4% with pre-frailty. Risk factors associated with frailty were age (OR = 1.12; 95% CI 1.07–1.17; p < 0.0001), comorbidities (OR = 1.51; 95% CI 1.01–2.27; p = 0.0446), and disease activity (OR = 1.10; 95% CI 1.04–1.16; p = 0.0006) [49].
Sarcopenia and ankylosing spondylitis
Ankylosing spondylitis (AS) causes decreased bone mass, stiffness, and movement loss, which may be related to loss of muscle mass and the development of sarcopenia. However, the prevalence and impact of sarcopenia in AS patients has not yet been clearly established [35, 50].
A cross-sectional by Ibáñez et al. [51] observed a decrease in muscle mass (and fat mass) associated with disease activity in male patients with AS, but not in women with AS. In both men and women, disease activity [Ankylosing Spondylitis Disease Activity Score (ASDAS) CRP] correlated negatively with fat mass. In a cross-sectional study of 10 patients with AS and 10 healthy controls, Røren et al. [52] observed significantly lower appendicular lean body mass (but no total mass), lower muscle strength, and a reduced number of type II muscle fibres in patients with AS.
A cross-sectional carried out by El Maghraoui et al. [53], which included 67 males with AS and 67 healthy controls, observed lower muscle mass in patients with AS. Prevalences of pre-sarcopenia, sarcopenia (defined by EWGSOP), and cachexia in patients with AS were 50.4%, 34.3%, and 11.9%, respectively. Sarcopenia and cachexia were significant associated with higher disease activity (Bath Ankylosing Spondylitis Disease Activity Index [BASDAI]) and lower BMD. Finally, in a cross-sectional study by Barone et al. [35] also observed a high prevalence of sarcopenia among patients with AS, around 20%.
Sarcopenia and systemic sclerosis
Several studies have observed a high prevalence of sarcopenia among patients with systemic sclerosis (SS), higher than that of healthy individuals [35, 54,55,56,57].
In a large cohort of 141 patients with SS, the prevalence of sarcopenia (defined by SMI) was around 20.7%. Importantly, sarcopenia prevalence in malnourished patients was significantly higher [54]. In a pilot intervention study of 18 patients with SS and gastrointestinal involvement, the percentage of patients with sarcopenia (defined by muscle mass) was lower after 6-week nutritional intervention (54–39%, p < 0.02) [55].
However, the association between sarcopenia and disease duration in patients with SS has not been established [54, 56, 57].
These studies show an interesting relationship between IMRDs and sarcopenia, but are burdened by differences in sarcopenia-related terms definitions, especially those that only evaluate muscle mass, and those that use a modern definition of sarcopenia.
Sarcopenia, immune-mediated rheumatic diseases, and biological disease-modifying antirheumatic drugs
Treatment of IMRDs may have an impact on sarcopenia. However, only a few studies have reported on the links between drugs and sarcopenia in this setting.
The deleterious effects of glucocorticoid (GC) on muscles have been well described elsewhere [58]. Patients with IMRDs using GC are at high risk for fractures, due to both the direct and indirect negative effects of GC on bone mass, and bone and muscle strength, and due to activity of the underlying inflammatory disease [59]. In a cross-sectional analysis of CHIKARA in patients with RA, GC use was more frequent among patients with sarcopenia than in patients without sarcopenia. Univariate analysis showed that GC dose was significantly associated with sarcopenia onset [60]. However, few data are available on other drugs used to treat IMRDs.
A prospective cohort study by Hasegawa et al. [61] evaluated bDMARDs’ activity on sarcopenia in men and women with RA starting bDMARDs treatment for the first time. bDMARDs used in the study included certolizumab pegol (24.4%), adalimumab (17.1%), abatacept (17.1%), golimumab (14.6%), tocilizumab (12.2%), infliximab (7.3%), and etanercept (7.3%). After 6 months of treatment with bDMARDs, physical activity, nutritional status, and quality of life significantly improved, and disease activity also was significantly reduced. Although muscle mass did not increase notably, the proportion of patients with sarcopenia tended to decrease. In view of these data, the authors suggested that bDMARD administration may be useful for secondary sarcopenia prevention in patients with RA. Similarly, in a cross-sectional study by Torii et al. [31] observed a negative association between bDMARDs use and sarcopenia in women with RA.
Briot et al. [62] in a prospective open study analysed the effect of anti-TNF-α treatment in male and female patients with spondyloarthropathy. Drugs used in this study included infliximab (89.5%) and etanercept (10.5%). After 1 year of treatment, significant increases in body weight, BMD, bone markers, and IGF-1 were observed. Therefore, treatment with anti-TNF-α in AS improves bone resorption together with an increase in body weight, lean body mass, and IGF-1.
These limited data regarding bDMARDs therapy suggest that this treatment has the potential to improve sarcopenia. Hence, future studies exploring this outcome are of the outmost interest.
Nutritional interventions for sarcopenia
There is growing evidence linking nutrition to muscle mass, strength, and function, suggesting its important role in both the prevention and treatment of sarcopenia [63]. Appropriate quality dietary patterns that ensure sufficient intake of protein, vitamin D, antioxidant nutrients, and long-chain polyunsaturated fatty acids are key modifiable and affordable interventions to improve physical performance in older people and/or in patients with particular diseases, such as frailty or sarcopenia [64,65,66].
A systematic literature review evaluated the association between sarcopenia and nutritional status, and observed a relationship between sarcopenia and a poor nutritional status [67].
In another systematic review evaluated the quality of the diet and sarcopenia, studying muscle mass, strength and physical performance, and sarcopenia risk. Evidence showing a relationship between “healthier” diets and better results in muscle mass and strength was low. In contrast, a relationship between “healthier” diets and a lower risk of decreased physical performance and a reduced risk of sarcopenia were observed. This study, then, shows benefits associated with “high quality” diets for physical performance improvement in older patients [68].
An observational study called SarcoPhAge study assessed micronutrient and macronutrient intake in patients of both sexes with sarcopenia. Study results suggest an association between an unbalanced diet and sarcopenia and poor musculoskeletal health, although further prospective studies are needed to confirm these findings [64]. Current guidelines on sarcopenia management consider the role of nutritional intervention on sarcopenia, but overall evidence is weak [69].
Proteins
Dietary proteins provide essential amino acids for muscle protein synthesis, and of these, leucine is especially important. Moreover, dietary proteins may act as an anabolic trigger, playing a key role in muscle protein synthesis [66, 70]. Protein turnover is key to balancing catabolism and anabolism and to maintaining muscle mass balance. Several studies show that an adequate high-quality protein intake is essential to maintain muscle mass. However, studies linking protein/amino acid intake to muscle strength and mass and function show inconsistent results [65].
A critical review by Hickson [70] found that trials performed with complete protein supplementation did not show a consistent effect on muscle mass, strength, or function. This could be explained by differences in study design, protein supplement composition and failure to monitor voluntary food intake, compliance, and baseline nutritional status. However, a systematic review by Shad et al. [71] showed that administrating aminoacid/protein to young and old individuals induces muscle protein synthesis (MPS). Moreover, the amino acid/protein dose and leucine content should exceed a certain threshold to stimulate equivalent MPS rates in young and older adults. Below this threshold, age-related muscle anabolic resistance is observed.
A systematic review and meta-analysis evaluated the efficacy of dairy proteins in sarcopenia-related functions in middle-aged and older adults. Dairy protein supplementation significantly increased appendicular muscle mass in middle-aged and older adults, although it showed no effect on improving muscle strength [72]. Finally, a systematic review analysed the effects of leucine or leucine-enriched protein (range 1.2–6.0 g leucine/day) supplementation in sarcopenic patients. Results showed that leucine administration improved sarcopenia by improving lean muscle mass. The effect on muscle strength showed mixed results, and the effect on physical performance has been little studied [73].
In brief, there is significant evidence of the importance of protein intake as the main stimulus for muscle protein synthesis and for maintaining muscle mass and strength in old age. Several expert groups have proposed an increase in dietary protein recommendations for older age groups to 1.0–1.2 g/kg body weight per day. However, more studies are needed to understand the specific benefit of a high-protein diet on physical function [66].
Vitamin D
Muscle mass loss and vitamin D deficiency often occur concomitantly, and are linked to weakness, fall events, and frailty in older patients [66]. Vitamin D receptors are widely expressed in muscle cells; however, their expression decreases with age, contributing to sarcopenia. Indirectly, vitamin D regulates calcium levels in the muscle and muscle fibre atrophy. Vitamin D deficiency causes muscle weakness that can be reversed with external vitamin D administration. Several studies associate muscle mass with vitamin D levels, although this relationship has not been fully clarified [65, 74].
It is difficult to assess the role of vitamin D, because there are no studies of vitamin D alone without protein supplementation. An RCT named The PROVIDE study evaluated vitamin D and leucine-enriched diets in older adults with sarcopenia. After 13 weeks, an improvement in muscle mass and lower limb function was observed in sarcopenic patients, highlighting the value of nutritional supplementation among these patients [75]. In an RCT carried out by Bo et al. [76] also showed that combined supplementation with protein, vitamin D, and vitamin E can significantly improve muscle mass [relative skeletal mass index (RSMI)], muscle strength and anabolic markers such as IGF-I and IL-2 in older adults with sarcopenia.
In short, we found significant evidence of the benefits of vitamin D supplementation, when included in multicomponent oral nutritional supplements, in maintaining muscle mass, strength, and physical function in old age, and in preventing and treating sarcopenia [66].
Omega-3 fatty acids
It has been suggested that the anti-inflammatory properties of ω-3 fatty acids (ω-3) are beneficial for muscle mass, strength, and function, and that they can prevent the low-grade, age-related chronic inflammation that contributes to the development of sarcopenia. Although the mechanisms by which ω-3 exert their effect on muscle mass and function are still unclear, a growing number of studies demonstrate the potential beneficial effect of dietary supplementation with ω-3 in older sarcopenic individuals [77]. A review found that ω-3 supplementation seems to increase muscle mass and prevent muscle catabolism independent of anabolic stimuli or anti-inflammatory effects in patients with primary and secondary sarcopenia. However, one of the included studies failed to show any effect of supplementation on muscle mass [78].
β-Hydroxy-β-methylbutyrate
β-Hydroxy-β-methylbutyrate (HMB) has been shown to reduce protein degradation, increase protein synthesis, and increase cholesterol production in muscle cells, conferring more stability to cell membranes. Moreover, HMB is a leucine metabolite, and 5–10% of ingested leucine is converted into HMB. HMB administration has shown benefits in muscle mass loss, strength, and function in several studies [70].
In an RCT conducted by Cramer et al. [79] evaluated high-protein oral + HMB nutritional supplementation in malnourished adult patients. Nutritional supplementation improved strength outcomes in malnourished older patients with sarcopenia. In patients with mild–moderate sarcopenia, nutritional supplementation + HMB improved strength and muscle quality in lower limbs compared to controls.
Oktaviana et al. [80] performed a systematic review to determine HMB effects on sarcopenic or fragile individuals. The results showed increased lean body mass and preserved muscle strength and function after HMB supplementation. The main limitation was the reduced number of currently available studies with HMB. In this respect, the effect of HMB supplementation on the mass, strength, and muscle function of older people with sarcopenia or frailty may be underestimated. A review evaluated the effect of oral HMB-enriched protein-rich nutritional supplements and found that they mitigated the decline of muscle mass and preserved muscle function, especially during hospital rehabilitation and recovery [81].
Therefore, more randomized clinical studies evaluating HMB administration in different clinical settings are needed to determine the benefits of supplementation.
Other micronutrients
It has been suggested that the antioxidant elements (vitamins C, E, and carotenoids and trace elements: Cu, Mn, Se, and Zn) intervene in muscle mass and strength, while minerals (Mg) intervene in muscle function and performance, and particular biocomponents, such as phenols, in muscle strength and mass [65].
The SarcoPhAge study assessed the micronutrient and macronutrient intake of patients of both sexes with sarcopenia. The adjusted analysis showed that sarcopenic patients consumed significantly lower amounts of two macronutrients (protein, lipids) and five micronutrients (potassium, magnesium, phosphorus, iron, and vitamin K) compared to non-sarcopenic participants (p < 0.005) [64].
Combined nutritional interventions
A systematic review evaluated the effect of nutritional intervention combined with physical activity on muscle mass and function in individuals over 60 years of age. Physical activity affected muscle mass and function positively; however, the results of interactive effects with the nutritional intervention were limited [82]. A systematic review evaluated the effect of nutritional intervention, physical activity, and the combined effect. The results highlight the importance of physical exercise (with and without concomitant nutritional interventions) for improving physical performance in patients with frailty and sarcopenia. In these patients, muscle strength improved with multidisciplinary treatment and physical exercise [83].
Immune-mediated rheumatic diseases and nutritional interventions
Nutritional abnormalities are prevalent in patients with IMRDs, and affect prognosis, quality of life, autonomy, independence, and even mortality. The aetiology of nutritional alterations is multifactorial, and malnutrition can be associated with chronic inflammatory processes (cachexia), acute inflammatory processes (protein-calorie malnutrition), and low food intake [84].
Nutrition plays an important role in both the progression and clinical outcomes of inflammatory diseases such as RA. Although the effect of nutrition on musculoskeletal diseases is not well studied, several clinical studies have linked supplementation with fatty acids and probiotics, and anti-inflammatory diets with improved symptoms and activities of daily living in patients with RA [85]. One case–control study in patients with RA showed that oral administration of creatine improves muscle mass, but no effect on muscle strength or function was observed [86]. The integrated management of IMRDs should include prevention, identification, and management of nutritional disorders [84].
Hugo et al. [87] performed an observational study to evaluate energy expenditure and nutritional complications in RA patients with metabolic syndrome and rheumatoid cachexia. They found that low levels of physical activity and GC use are associated with nutritional complications in patients with RA, suggesting a potential strategy for therapeutic intervention.
Conclusions and future research directions
The link between sarcopenia and rheumatoid diseases is an interesting growing area of study; however, it requires more in-deep studies (Table 1). To better understand the interaction between these two groups of diseases and its potential treatment, geriatricians and rheumatologists need to work closely. Finally, it would be helpful to use modern definitions of sarcopenia, and not just muscle mass definition, to get comparable and universal results.
References
Beaudart C, Zaaria M, Pasleau F et al (2017) Health outcomes of sarcopenia: a systematic review and meta-analysis. PLoS ONE 12:e0169548–e0169548. https://doi.org/10.1371/journal.pone.0169548
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia. Lancet (London, England) 393:2636–2646. https://doi.org/10.1016/S0140-6736(19)31138-9
Vellas B, Fielding RA, Bens C et al. (2018) Implications of ICD-10 for sarcopenia clinical practice and clinical trials: report by the international conference on frailty and sarcopenia research task force. J Frailty Aging 7:2–9. https://doi.org/10.14283/jfa.2017.30
Tournadre A, Vial G, Capel F et al (2019) Sarcopenia. Jt Bone Spine 86:309–314. https://doi.org/10.1016/j.jbspin.2018.08.001
Fuggle N, Shaw S, Dennison E et al (2017) Sarcopenia. Best Pract Res Clin Rheumatol 31:218–242. https://doi.org/10.1016/j.berh.2017.11.007
Bauer J, Morley JE, Schols AMWJ et al (2019) Sarcopenia: a time for action. An SCWD position paper. J Cachexia Sarcopenia Muscle 10:956–961. https://doi.org/10.1002/jcsm.12483
Beaudart C, Rolland Y, Cruz-Jentoft AJ et al (2019) Assessment of muscle function and physical performance in daily clinical practice: a position paper endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Calcif Tissue Int 105:1–14. https://doi.org/10.1007/s00223-019-00545-w
Marconcin P, Peralta M, Ferrari G et al (2020) The association of grip strength with depressive symptoms among middle-aged and older adults with different chronic diseases. Int J Environ Res Public Health 17:1–10. https://doi.org/10.3390/ijerph17196942
Wilson D, Jackson T, Sapey E et al (2017) Frailty and sarcopenia: the potential role of an aged immune system. Ageing Res Rev 36:1–10. https://doi.org/10.1016/j.arr.2017.01.006
Bano G, Trevisan C, Carraro S et al (2017) Inflammation and sarcopenia: a systematic review and meta-analysis. Maturitas 96:10–15. https://doi.org/10.1016/j.maturitas.2016.11.006
Sánchez-Castellano C, Martín-Aragón S, Bermejo-Bescós P et al (2020) Biomarkers of sarcopenia in very old patients with hip fracture. J Cachexia Sarcopenia Muscle 11:478–486. https://doi.org/10.1002/jcsm.12508
Santoro A, Guidarelli G, Ostan R et al (2019) Gender-specific association of body composition with inflammatory and adipose-related markers in healthy elderly Europeans from the NU-AGE study. Eur Radiol 29:4968–4979. https://doi.org/10.1007/s00330-018-5973-2
Can B, Kara O, Kizilarslanoglu MC et al (2017) Serum markers of inflammation and oxidative stress in sarcopenia. Aging Clin Exp Res 29:745–752. https://doi.org/10.1007/s40520-016-0626-2
van Atteveld VA, Van Ancum JM, Reijnierse EM et al (2019) Erythrocyte sedimentation rate and albumin as markers of inflammation are associated with measures of sarcopenia: a cross-sectional study. BMC Geriatr 19:1–8. https://doi.org/10.1186/s12877-019-1253-5
Öztürk ZA, Kul S, Türkbeyler İH et al (2018) Is increased neutrophil lymphocyte ratio remarking the inflammation in sarcopenia? Exp Gerontol 110:223–229. https://doi.org/10.1016/j.exger.2018.06.013
Marzetti E, Picca A, Marini F et al (2019) Inflammatory signatures in older persons with physical frailty and sarcopenia: the frailty “cytokinome” at its core. Exp Gerontol 122:129–138. https://doi.org/10.1016/j.exger.2019.04.019
Westbury LD, Fuggle NR, Syddall HE et al (2018) Relationships between markers of inflammation and muscle mass, strength and function: findings from the hertfordshire cohort study. Calcif Tissue Int 102:287–295. https://doi.org/10.1007/s00223-017-0354-4
Tekgoz E, Colak S, Ozalp F, et al (2020) FRI0059 Sarcopenia in patients with rheumatoid arthritis. Ann Rheum Dis 79:606. https://ard.bmj.com/content/79/Suppl_1/606.2
Doğan SC, Hizmetli S, Hayta E et al (2015) Sarcopenia in women with rheumatoid arthritis. Eur J Rheumatol 2:57–61. https://doi.org/10.5152/eurjrheum.2015.0038
Ngeuleu A, Allali F, Medrare L et al (2017) Sarcopenia in rheumatoid arthritis: prevalence, influence of disease activity and associated factors. Rheumatol Int 37:1015–1020. https://doi.org/10.1007/s00296-017-3665-x
Feklistov A, Demin N, Toroptsova N (2018) AB0330 Osteoporosis, sarcopenia and osteosarcopenia in women with rheumatoid arthritis. Ann Rheum Dis 77:1340. https://doi.org/10.1136/annrheumdis-2018-eular.6141
Aminov K (2017) AB0842 Sarcopenia and osteoporosis in patients with rheumatoid arthritis. Ann Rheum Dis 76:1351. https://doi.org/10.1136/annrheumdis-2017-eular.3165
Yatsyshyn R, Stoika I (2018) AB0358 Phenotypes of secondary sarcopenia in patients with rheumatoid arthritis. Ann Rheum Dis 77:1351. https://doi.org/10.1136/annrheumdis-2018-eular.2305
Clausen J, Dietzel R, Armbrecht G (2019) OP0285-Pare sarcopenia in patients with rheumatic diseases. Ann Rheum Dis 78:224. https://doi.org/10.1136/annrheumdis-2019-eular.2072
Tournadre A, Jaffeux P, Frayssac T et al (2017) SAT0682 Prevalence of sarcopenia in patients with chronic inflammatory rheumatic diseases. Ann Rheum Dis 76:1033. https://doi.org/10.1136/annrheumdis-2017-eular.5122
Baker JF, Long J, Ibrahim S et al (2015) Are men at greater risk of lean mass deficits in rheumatoid arthritis? Arthritis Care Res 67:112–119. https://doi.org/10.1002/acr.22396
Yamada Y, Tada M, Mandai K et al (2019) THU0159 Risk factors for developing sarcopenia in patients with rheumatoid arthritis at 2 years: from the CHIKARA study. Ann Rheum Dis 78:352–353. https://doi.org/10.1136/annrheumdis-2019-eular.1399
Tada M, Yamada Y, Mandai K et al (2018) Matrix metalloprotease 3 is associated with sarcopenia in rheumatoid arthritis—results from the CHIKARA study. Int J Rheum Dis 21:1962–1969. https://doi.org/10.1111/1756-185X.13335
Reina D, Gómez-Vaquero C, Díaz-Torné C et al (2019) Assessment of nutritional status by dual X-Ray absorptiometry in women with rheumatoid arthritis: a case-control study. Medicine (Baltimore) 98:e14361–e14361. https://doi.org/10.1097/MD.0000000000014361
Torii M, Hashimoto M, Hanai A et al (2019) Prevalence and factors associated with sarcopenia in patients with rheumatoid arthritis. Mod Rheumatol 29:589–595. https://doi.org/10.1080/14397595.2018.1510565
Mochizuki T, Yano K, Ikari K et al (2019) Sarcopenia-associated factors in Japanese patients with rheumatoid arthritis: a cross-sectional study. Geriatr Gerontol Int 19:907–912. https://doi.org/10.1111/ggi.13747
Donini LM, Busetto L, Bauer JM et al (2019) Critical appraisal of definitions and diagnostic criteria for sarcopenic obesity based on a systematic review. Clin Nutr 39:2368–2388. https://doi.org/10.1016/j.clnu.2019.11.024
Vlietstra L, Stebbings S, Meredith-Jones K et al (2019) Sarcopenia in osteoarthritis and rheumatoid arthritis: the association with self-reported fatigue, physical function and obesity. PLoS ONE 14:1–13. https://doi.org/10.1371/journal.pone.0217462
Barone M, Viggiani M, Anelli M et al (2018) Sarcopenia in patients with rheumatic diseases: prevalence and associated risk factors. J Clin Med 7:504. https://doi.org/10.3390/jcm7120504
Park D-J, Kang J-H, Xu H et al (2019) THU0152 Sarcopenia is associated with persistent disease activity during follow-up of rheumatoid arthritis. Ann Rheum Dis 78:349. https://doi.org/10.1136/annrheumdis-2019-eular.3412
Carvalho GD, Bonfiglioli K, Caparbo VF et al (2019) Changes to body composition in women with long-standing established rheumatoid arthritis: differences by level of disease activity. J Clin Densitom S1094–6950:30070–30078. https://doi.org/10.1016/j.jocd.2019.06.002
Lin J-Z, Wang Y-Y, Liu P-J et al (2018) SAT0099 Sarcopenia is associated with joint damage in rheumatoid arthritis: a cross-sectional study. Ann Rheum Dis 77:911–912. https://doi.org/10.1136/annrheumdis-2018-eular.6085
Tada M, Yamada Y, Mandai K et al (2018) AB0373 Sarcopenia could not predict falls in patients with rheumatoid arthritis from the CHIKARA study. Ann Rheum Dis 77:1356–1357. https://doi.org/10.1136/annrheumdis-2018-eular.2562
Nielsen BR, Abdulla J, Andersen HE et al (2018) Sarcopenia and osteoporosis in older people: a systematic review and meta-analysis. Eur Geriatr Med 9:419–434. https://doi.org/10.1007/s41999-018-0079-6
Hirschfeld HP, Kinsella R, Duque G (2017) Osteosarcopenia: where bone, muscle, and fat collide. Osteoporos Int 28:2781–2790. https://doi.org/10.1007/s00198-017-4151-8
Radkowski MJ, Sławiński P, Targowski T (2020) Osteosarcopenia in rheumatoid arthritis treated with glucocorticosteroids—essence, significance, consequences. Reumatologia 58:101–106. https://doi.org/10.5114/reum.2020.95363
Confavreux CB, Chapurlat RD (2011) Systemic bone effects of biologic therapies in rheumatoid arthritis and ankylosing spondylitis. Osteoporos Int 22(4):1023–1036. https://doi.org/10.1007/s00198-010-1462-4
Okano T, Inui K, Tada M et al (2017) Loss of lean body mass affects low bone mineral density in patients with rheumatoid arthritis–results from the TOMORROW study. Mod Rheumatol 27:946–952. https://doi.org/10.1080/14397595.2017.1289645
Inui K, Koike T, Sugioka Y et al (2018) SAT0144 Effect of aging on bone mass and skeletal muscle mass in elderly patients with rheumatoid arthritis: TOMORROW study. Ann Rheum Dis 77:934. https://doi.org/10.1136/annrheumdis-2018-eular.1780
Cruz-Jentoft AJ, Kiesswetter E, Drey M et al (2017) Nutrition, frailty, and sarcopenia. Aging Clin Exp Res 29:43–48. https://doi.org/10.1007/s40520-016-0709-0
Trujillo E, Garcia-Marrero MR, Fuentes MI et al (2018) AB0339 Sarcopenia and early frailty syndrome in rheumatoid arthritis. Ann Rheum Dis 77:1343. https://doi.org/10.1136/annrheumdis-2018-eular.3519
Tada M, Yamada Y, Mandai K et al (2019) Correlation between frailty and disease activity in patients with rheumatoid arthritis: data from the CHIKARA study. Geriatr Gerontol Int 19:1220–1225. https://doi.org/10.1111/ggi.13795
Salaffi F, Di Carlo M, Farah S et al (2019) Prevalence of frailty and its associated factors in patients with rheumatoid arthritis: a cross-sectional analysis. Clin Rheumatol 38:1823–1830. https://doi.org/10.1007/s10067-019-04486-5
Valido A, Crespo CL, Pimentel-Santos FM (2019) Muscle evaluation in axial spondyloarthritis—the evidence for sarcopenia. Front Med 6:1–10. https://doi.org/10.3389/fmed.2019.00219
Ibáñez S, Visman IM, van Denderen C et al (2017) Muscle wasting in male TNF-α blocker naïve ankylosing spondylitis patients: a comparison of gender differences in body composition. Rheumatol (United Kingdom) 56:1566–1572. https://doi.org/10.1093/rheumatology/kex187
Røren Nordén K, Dagfinrud H, Løvstad A et al (2016) Reduced appendicular lean body mass, muscle strength, and size of type II muscle fibers in patients with spondyloarthritis versus healthy controls: a cross-sectional study. Sci World J 2016:6507692. https://doi.org/10.1155/2016/6507692
EI Maghraoui A, Ebo’O FB, Sadni S et al (2016) Is there a relation between pre-sarcopenia, sarcopenia, cachexia and osteoporosis in patients with ankylosing spondylitis? BMC Musculoskelet Disord 17:1–8. https://doi.org/10.1186/s12891-016-1155-z
Caimmi C, Caramaschi P, Venturini A et al (2018) Malnutrition and sarcopenia in a large cohort of patients with systemic sclerosis. Clin Rheumatol 37:987–997. https://doi.org/10.1007/s10067-017-3932-y
Doerfler B, Allen TS, Southwood C et al (2017) Medical nutrition therapy for patients with advanced systemic sclerosis (MNT PASS): a pilot intervention study. J Parenter Enter Nutr 41:678–684. https://doi.org/10.1177/0148607115597883
Corallo C, Fioravanti A, Tenti S et al (2019) Sarcopenia in systemic sclerosis: the impact of nutritional, clinical, and laboratory features. Rheumatol Int 39:1767–1775. https://doi.org/10.1007/s00296-019-04401-w
Siegert E, March C, Otten L et al (2018) Prevalence of sarcopenia in systemic sclerosis: assessing body composition and functional disability in patients with systemic sclerosis. Nutrition 55–56:51–55. https://doi.org/10.1016/j.nut.2018.03.046
Martín AI, Priego T, López-Calderón A (2018) Hormones and muscle atrophy. Adv Exp Med Biol 1088:207–233. https://doi.org/10.1007/978-981-13-1435-3_9
Güler-Yüksel M, Hoes JN, Bultink IEM et al (2018) Glucocorticoids, inflammation and bone. Calcif Tissue Int 102:592–606. https://doi.org/10.1007/s00223-017-0335-7
Yamada Y, Tada M, Mandai K et al (2020) Glucocorticoid use is an independent risk factor for developing sarcopenia in patients with rheumatoid arthritis: from the CHIKARA study. Clin Rheumatol 39:1757–1764. https://doi.org/10.1007/s10067-020-04929-4
Hasegawa E, Ito S, Kurosawa Y et al (2019) AB0328 Secondary sarcopenia in rheumatoid arthritis patients treated by biologic disease modifying anti-rheumatic drugs. Ann Rheum Dis 78:1622. https://doi.org/10.1136/annrheumdis-2019-eular.4572
Briot K, Garnero P, Le Henanff A et al (2005) Body weight, body composition, and bone turnover changes in patients with spondyloarthropathy receiving anti-tumour necrosis factor alpha treatment. Ann Rheum Dis 64:1137–1140. https://doi.org/10.1136/ard.2004.028670
Ganapathy A, Nieves JW (2020) Nutrition and sarcopenia-what do we know? Nutrients 12:1755. https://doi.org/10.3390/nu12061755
Beaudart C, Locquet M, Touvier M et al (2019) Association between dietary nutrient intake and sarcopenia in the SarcoPhAge study. Aging Clin Exp Res 31:815–824. https://doi.org/10.1007/s40520-019-01186-7
Abiri B, Vafa M (2019) Nutrition and sarcopenia: a review of the evidence of nutritional influences. Crit Rev Food Sci Nutr 59:1456–1466. https://doi.org/10.1080/10408398.2017.1412940
Robinson SM, Reginster JY, Rizzoli R et al (2018) Does nutrition play a role in the prevention and management of sarcopenia? Clin Nutr 37:1121–1132. https://doi.org/10.1016/j.clnu.2017.08.016
Eglseer D, Eminovic S, Lohrmann C (2016) Association between sarcopenia and nutritional status in older adults: a systematic literature review. J Gerontol Nurs 42:33–41. https://doi.org/10.3928/00989134-20160613-03
Bloom I, Shand C, Cooper C et al (2018) Diet quality and sarcopenia in older adults: a systematic review. Nutrients 10:308. https://doi.org/10.3390/nu10030308
Dent E, Morley JE, Cruz-Jentoft AJ et al (2018) International Clinical Practice Guidelines for Sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging 22:1148–1161. https://doi.org/10.1007/s12603-018-1139-9
Hickson M (2015) Nutritional interventions in sarcopenia: a critical review. Proc Nutr Soc 74:378–386. https://doi.org/10.1017/S0029665115002049
Shad BJ, Thompson JL, Breen L (2016) Does the muscle protein synthetic response to exercise and amino acid-based nutrition diminish with advancing age? A systematic review. Am J Physiol Endocrinol Metab 311:E803–E817. https://doi.org/10.1152/ajpendo.00213.2016
Hanach NI, McCullough F, Avery A (2019) The impact of dairy protein intake on muscle mass, muscle strength, and physical performance in middle-aged to older adults with or without existing sarcopenia: a systematic review and meta-analysis. Adv Nutr 10:59–69. https://doi.org/10.1093/advances/nmy065
Martínez-Arnau FM, Fonfría-Vivas R, Cauli O (2019) Beneficial effects of leucine supplementation on criteria for sarcopenia: a systematic review. Nutrients 11:2504. https://doi.org/10.3390/nu11102504
Wimalawansa SJ (2018) Non-musculoskeletal benefits of vitamin D. J Steroid Biochem Mol Biol 175:60–81. https://doi.org/10.1016/j.jsbmb.2016.09.016
Bauer JM, Verlaan S, Bautmans I et al (2015) Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc 16:740–747. https://doi.org/10.1016/j.jamda.2015.05.021
Bo Y, Liu C, Ji Z et al (2019) A high whey protein, vitamin D and E supplement preserves muscle mass, strength, and quality of life in sarcopenic older adults: a double-blind randomized controlled trial. Clin Nutr 38:159–164. https://doi.org/10.1016/j.clnu.2017.12.020
Dupont J, Dedeyne L, Dalle S et al (2019) The role of omega-3 in the prevention and treatment of sarcopenia. Aging Clin Exp Res 31:825–836. https://doi.org/10.1007/s40520-019-01146-1
Buoite Stella A, Gortan Cappellari G, Barazzoni R et al (2018) Update on the impact of omega 3 fatty acids on inflammation, insulin resistance and sarcopenia: a review. Int J Mol Sci 19:218. https://doi.org/10.3390/ijms19010218
Cramer JT, Cruz-Jentoft AJ, Landi F et al (2016) Impacts of high-protein oral nutritional supplements among malnourished men and women with sarcopenia: a multicenter, randomized, double-blinded, controlled trial. J Am Med Dir Assoc 17:1044–1055. https://doi.org/10.1016/j.jamda.2016.08.009
Oktaviana J, Zanker J, Vogrin S et al (2019) The effect of β-hydroxy-β-methylbutyrate (HMB) on sarcopenia and functional frailty in older persons: a systematic review. J Nutr Health Aging 23:145–150. https://doi.org/10.1007/s12603-018-1153-y
Sanz-Paris A, Camprubi-Robles M, Lopez-Pedrosa JM et al (2018) Role of oral nutritional supplements enriched with β-Hydroxy-β-methylbutyrate in maintaining muscle function and improving clinical outcomes in various clinical settings. J Nutr Health Aging 22:664–675. https://doi.org/10.1007/s12603-018-0995-7
Beaudart C, Dawson A, Shaw SC et al (2017) Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int 28:1817–1833. https://doi.org/10.1007/s00198-017-3980-9
Lozano-Montoya I, Correa-Pérez A, Abraha I et al (2017) Nonpharmacological interventions to treat physical frailty and sarcopenia in older patients: a systematic overview—the SENATOR Project ONTOP Series. Clin Interv Aging 12:721–740. https://doi.org/10.2147/CIA.S132496
Hurtado-Torres GF, González-Baranda LL, Abud-Mendoza C (2015) Caquexia reumatológica y otras alteraciones nutricionales en las enfermedades reumatológicas. Reumatol Clin 11:316–321. https://doi.org/10.1016/j.reuma.2015.03.005
Cutolo M, Nikiphorou E (2018) Don’t neglect nutrition in rheumatoid arthritis! RMD open 4:e000591. https://doi.org/10.1136/rmdopen-2017-000591
Wilkinson TJ, Lemmey AB, Jones JG et al (2016) Can creatine supplementation improve body composition and objective physical function in rheumatoid arthritis patients? A randomized controlled trial. Arthritis Care Res (Hoboken) 68:729–737. https://doi.org/10.1002/acr.22747
Hugo M, Mehsen-Cetre N, Pierreisnard A et al (2016) Energy expenditure and nutritional complications of metabolic syndrome and rheumatoid cachexia in rheumatoid arthritis: an observational study using calorimetry and actimetry. Rheumatology (Oxford) 55:1202–1209. https://doi.org/10.1093/rheumatology/kew038
Funding
This paper was financed by Fresenius-Kabi Spain. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to the literature search, and drafted and/or critically revised the work. Literature search and data analysis were performed by all the authors: AJC-J, SR-Y, ECC, and JMN. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Cruz-Jentoft reports research grants from Abbott Nutrition, Fresenius Kabi and Nutricia, and speaking fees from Abbott Nutrition, Fresenius Kabi, Nestlé, Nutricia, Sanofi and Pfizer. Dra. Romero-Yuste has no conflict of interest to declare. Dr. Chamizo has no conflict of interest to declare. Dr. Nolla has received consulting fees and speaking fees from AbbVie, Amgen, Bristol-Myers Squibb, Fresenius Kabi, Gebro, Kern, Eli Lilly, MSD, Novartis, Pfizer, Roche, Sanofi, and UCB, and research support from AbbVie, Amgen, Biogen, Bristol-Myers Squibb, Gebro, Eli Lilly, MSD, Roche, Sandoz, Sanofi, and UCB.
Ethical approval
For this type of study, ethics approval is not required.
Consent to participate
For this type of study, informed consent is not required.
Consent for publication
For this type of study, consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cruz-Jentoft, A.J., Romero-Yuste, S., Chamizo Carmona, E. et al. Sarcopenia, immune-mediated rheumatic diseases, and nutritional interventions. Aging Clin Exp Res 33, 2929–2939 (2021). https://doi.org/10.1007/s40520-021-01800-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01800-7