Abstract
Background
Heart rate variability (HRV) is a method to assess the autonomic nervous system and reflects possibly central brain states. HRV has previously not been examined in patients with hip fracture and delirium.
Aims
To explore HRV parameters in hip fracture patients with and without delirium.
Methods
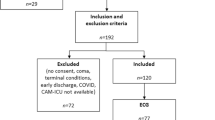
Patients admitted to Oslo University Hospital with hip fracture and sinus rhythm in electrocardiogram (ECG) were included. Delirium was diagnosed using the confusion assessment method. HRV was assessed preoperatively after a relaxing period of five minutes, by measuring an ECG signal over 5 min. Parameters in time domain (the standard deviation of the QRS distances—SDNN) and frequency domain (total power (TP), low frequency (LF), high frequency (HF) and LF/HF ratio) were calculated.
Results
Seventy-five patients were included in the study, and 21 of them had subsyndromal delirium and were excluded from the analysis. Fifty-four patients with a mean age of 83.5 years (SD 8.6, 78% females) were included. Twenty-six patients (48%) had preoperative delirium, 11 (20%) developed delirium postoperatively, whereas 17 (31%) never developed delirium. SDNN, TP and HF values were significantly higher in patients with delirium compared to patients without delirium, and LF and LF/HF were lower. Patients developing postoperative delirium had decreased LF and increased HF before symptom onset.
Discussion
Increased SDNN, TP and HF and decreased LF values might reflect an abnormal stress response in delirium.
Conclusion
HRV measurements in patients with hip fractures provide additional information beyond heart rate and might be used to identify relevant pathophysiological factors in delirium.



Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Benhamou D, Brouquet A (2016) Postoperative cerebral dysfunction in the elderly: diagnosis and prophylaxis. J Visc Surg 153:S27–s32. https://doi.org/10.1016/j.jviscsurg.2016.09.015
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. Lancet 383:911–922. https://doi.org/10.1016/s0140-6736(13)60688-1
Watne LO, Torbergsen AC, Conroy S et al (2014) The effect of a pre- and postoperative orthogeriatric service on cognitive function in patients with hip fracture: randomized controlled trial (Oslo Orthogeriatric Trial). BMC Med 12:63. https://doi.org/10.1186/1741-7015-12-63
Marcantonio ER, Flacker JM, Wright RJ et al (2001) Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc 49:516–522
Maldonado JR (2013) Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am J Geriatr Psychiatry 21:1190–1222. https://doi.org/10.1016/j.jagp.2013.09.005
Maclullich AM, Ferguson KJ, Miller T et al (2008) Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses. J Psychosom Res 65:229–238. https://doi.org/10.1016/j.jpsychores.2008.05.019
Shaffer F, McCraty R, Zerr CL (2014) A healthy heart is not a metronome: an integrative review of the heart's anatomy and heart rate variability. Front Psychol 5:1040. https://doi.org/10.3389/fpsyg.2014.01040
Ernst G (2017) Hidden signals-the history and methods of heart rate variability. Front Public Health 5:265. https://doi.org/10.3389/fpubh.2017.00265
Sassi R, Cerutti S, Lombardi F et al (2015) Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace 17:1341–1353. https://doi.org/10.1093/europace/euv015
Huikuri HV, Stein PK (2013) Heart rate variability in risk stratification of cardiac patients. Prog Cardiovasc Dis 56:153–159. https://doi.org/10.1016/j.pcad.2013.07.003
Lin K, Wei L, Huang Z et al (2017) Combination of Ewing test, heart rate variability, and heart rate turbulence analysis for early diagnosis of diabetic cardiac autonomic neuropathy. Medicine 96:e8296. https://doi.org/10.1097/md.0000000000008296
Tsuji H, Venditti FJ Jr, Manders ES et al (1994) Reduced heart rate variability and mortality risk in an elderly cohort The Framingham Heart Study. Circulation 90:878–883. https://doi.org/10.1161/01.cir.90.2.878
Huikuri HV, Makikallio TH, Airaksinen KE et al (1998) Power-law relationship of heart rate variability as a predictor of mortality in the elderly. Circulation 97:2031–2036
de Castilho FM, Ribeiro ALP, Nobre V et al (2018) Heart rate variability as predictor of mortality in sepsis: a systematic review. PLoS One 13:e0203487. https://doi.org/10.1371/journal.pone.0203487
Nagendra H, Kumar V, Mukherjee S (2015) Cognitive behavior evaluation based on physiological parameters among young healthy subjects with yoga as intervention. Comput Math Methods Med 2015:821061. https://doi.org/10.1155/2015/821061
Kaikkonen KM, Korpelainen RI, Tulppo MP et al (2014) Physical activity and aerobic fitness are positively associated with heart rate variability in obese adults. J Phys Act Health 11:1614–1621. https://doi.org/10.1123/jpah.2012-0405
Heart rate variability (1996) Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J 17:354–381
McCraty R, Shaffer F (2015) Heart rate variability: new perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Glob Adv Health Med 4:46–61. https://doi.org/10.7453/gahmj.2014.073
Kleiger RE, Stein PK, Bigger JT Jr (2005) Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol 10:88–101. https://doi.org/10.1111/j.1542-474X.2005.10101.x
Ernst G (2014) Heart rate variability. Springer, London
Smith R, Thayer JF, Khalsa SS et al (2017) The hierarchical basis of neurovisceral integration. Neurosci Biobehav Rev 75:274–296. https://doi.org/10.1016/j.neubiorev.2017.02.003
Pontet J, Contreras P, Curbelo A et al (2003) Heart rate variability as early marker of multiple organ dysfunction syndrome in septic patients. J Crit Care 18:156–163
Ryan ML, Thorson CM, Otero CA et al (2011) Clinical applications of heart rate variability in the triage and assessment of traumatically injured patients. Anesthesiol Res Pract 2011:416590. https://doi.org/10.1155/2011/416590
Zaal IJ, van der Kooi AW, van Schelven LJ et al (2015) Heart rate variability in intensive care unit patients with delirium. J Neuropsychiatr Clin Neurosci 27:e112–e116. https://doi.org/10.1176/appi.neuropsych.13090213
Neerland BE, Wyller TB, Wyller VBB (2019) Autonomic cardiovascular control in older patients with acute infection and delirium: a pilot study of orthostatic stress responses. BMC Geriatr 19:23. https://doi.org/10.1186/s12877-019-1035-0
Wyller TB, Watne LO, Torbergsen A et al (2012) The effect of a pre- and post-operative orthogeriatric service on cognitive function in patients with hip fracture. The protocol of the Oslo Orthogeriatrics Trial. BMC Geriatr. https://doi.org/10.1186/1471-231812-36
Inouye SK, van Dyck CH, Alessi CA et al (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Inter Med 113:941–948. https://doi.org/10.7326/0003-4819-113-12-941
Organization WH The ICD-10 Classification of mental and behavioural disorders. Diagnostic criteria for research. World Health Organization (Available from: www.who.int/classifications/icd/en/GRNBOOK.pdf), Geneva. Accessed 26 Dec 2019
Alexopoulos GS, Abrams RC, Young RC et al (1988) Cornell scale for depression in dementia. Biol Psychiatry 23:271–284. https://doi.org/10.1016/0006-3223(88)90038-8
Wittling WW, Wittling RA (2012) Herzschlagvariabilität: Frühwarnsystem, Stress- und Fitnessindikator. Eichsfeld-Verlag, Heiligenstadt
Hillebrand S, Gast KB, de Mutsert R et al (2013) Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: meta-analysis and dose-response meta-regression. Europace 15:742–749. https://doi.org/10.1093/europace/eus341
de Bruyne MC, Kors JA, Hoes AW et al (1999) Both decreased and increased heart rate variability on the standard 10-second electrocardiogram predict cardiac mortality in the elderly: the Rotterdam Study. Am J Epidemiol 150:1282–1288. https://doi.org/10.1093/oxfordjournals.aje.a009959
Gerritsen J, Dekker JM, TenVoorde BJ et al (2001) Impaired autonomic function is associated with increased mortality, especially in subjects with diabetes, hypertension, or a history of cardiovascular disease: the Hoorn Study. Diabetes Care 24:1793–1798
Berntson G, Cacioppo J (2004) Heart rate variability: stress and psychiatric conditions. Dynamic Electrocardiography. Futura, New York
Hjortskov N, Rissen D, Blangsted AK et al (2004) The effect of mental stress on heart rate variability and blood pressure during computer work. Eur J Appl Physiol 92:84–89. https://doi.org/10.1007/s00421-004-1055-z
Tharion E, Parthasarathy S, Neelakantan N (2009) Short-term heart rate variability measures in students during examinations. Natl Med J India 22:63–66
Taelman J, Vandeput S, Vlemincx E et al (2011) Instantaneous changes in heart rate regulation due to mental load in simulated office work. Eur J Appl Physiol 111:1497–1505. https://doi.org/10.1007/s00421-010-1776-0
Castaldo R, Melillo P, Bracale U et al (2015) Acute mental stress assessment via short term HRV analysis in healthy adults: A systematic review with meta-analysis. Biomed Signal Proc Control 18:370–377. https://doi.org/10.1016/j.bspc.2015.02.012
Schubert C, Lambertz M, Nelesen RA et al (2009) Effects of stress on heart rate complexity—a comparison between short-term and chronic stress. Biol Psychol 80:325–332. https://doi.org/10.1016/j.biopsycho.2008.11.005
Molina PE (2005) Neurobiology of the stress response: contribution of the sympathetic nervous system to the neuroimmune axis in traumatic injury. Shock 24:3–10
Maldonado JR (2018) Delirium pathophysiology: an updated hypothesis of the etiology of acute brain failure. Int J Geriatr Psychiatry 33:1428–1457. https://doi.org/10.1002/gps.4823
de Rooij SE, van Munster BC, Korevaar JC et al (2007) Cytokines and acute phase response in delirium. J Psychosom Res 62:521–525. https://doi.org/10.1016/j.jpsychores.2006.11.013
Thayer JF, Loerbroks A, Sternberg EM (2011) Inflammation and cardiorespiratory control: the role of the vagus nerve. Respir Physiol Neurobiol 178:387–394. https://doi.org/10.1016/j.resp.2011.05.016
Groves DA, Brown VJ (2005) Vagal nerve stimulation: a review of its applications and potential mechanisms that mediate its clinical effects. Neurosci Biobehav Rev 29:493–500. https://doi.org/10.1016/j.neubiorev.2005.01.004
Sternberg EM (2006) Neural regulation of innate immunity: a coordinated nonspecific host response to pathogens. Nat Rev Immunol 6:318–328. https://doi.org/10.1038/nri1810
Kemp AH, Quintana DS (2013) The relationship between mental and physical health: insights from the study of heart rate variability. Int J Psychophysiol 89:288–296. https://doi.org/10.1016/j.ijpsycho.2013.06.018
Jooyoung O, Dongrae C, Jongin K et al (2017) Changes in heart rate variability of patients with delirium in intensive care unit. Conference proceedings : Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Annual Conference 2017:3118–3121. https://doi.org/10.1109/embc.2017.8037517
da Silva VP, Ramalho Oliveira BR, Tavares Mello RG et al (2018) Heart Rate Variability Indexes in Dementia: a systematic review with a quantitative analysis. Curr Alzheimer Res 15:80–88. https://doi.org/10.2174/1567205014666170531082352
Kasanuki K, Iseki E, Fujishiro H et al (2015) Impaired heart rate variability in patients with dementia with Lewy bodies: efficacy of electrocardiogram as a supporting diagnostic marker. Parkinsonism Relat Dis 21:749–754. https://doi.org/10.1016/j.parkreldis.2015.04.024
Frenneaux MP (2004) Autonomic changes in patients with heart failure and in post-myocardial infarction patients. Heart 90:1248–1255. https://doi.org/10.1136/hrt.2003.026146
Funding
The study was funded by the Research Council of Norway and the Norwegian Association for Public Health. The sponsors had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Gernot Ernst and Leiv Otto Watne. The first draft of the manuscript was written by Gernot Ernst, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was reviewed and accepted by the Regional Committee for Medical and Health Research Ethic in South-East Norway (REK 2009/450).
Informed consent
Informed consent was obtained from the patients or substitute decision-makers if the patients did not have the capacity to consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ernst, G., Watne, L.O., Rostrup, M. et al. Delirium in patients with hip fracture is associated with increased heart rate variability. Aging Clin Exp Res 32, 2311–2318 (2020). https://doi.org/10.1007/s40520-019-01447-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01447-5