Abstract
Background
Alterations in autonomic nervous system (ANS) activity might be involved in the pathophysiology of delirium. The aim was to explore autonomic cardiovascular control in older patients with and without delirium.
Methods
Fourteen patients (five with delirium) acutely admitted to the geriatric ward with an infection were enrolled in the study. Patients with atrial fibrillation, a pacemaker, or on treatment with beta-blockers, calcium channel blockers or acetylcholinesterase inhibitors were not eligible.
Continuous, non-invasive hemodynamic variables were measured during supine rest (5 min) and head-up tilt (HUT) to 15 degrees (10 min). Heart rate (HR), blood pressure (BP) and stroke volume (SV) were recorded beat-to-beat. Cardiac output (CO), total peripheral resistance (TPR), end-diastolic volume (EDV) and heart rate variability (HRV) values were calculated.
Results
Median age was 86 years. HR, BP, SV, CO, TPR and EDV were similar across the two groups at rest, but there was a trend towards a greater increase in systolic BP and HR during HUT in the delirium group. At rest, all HRV indices were higher in the delirium group, but the differences were not statistically significant. During HUT, the delirium group had higher power spectral density (PSD) (representing total variability) (p = 0.06) and a lower low frequency (LF)/high frequency (HF)-ratio (an index of sympathovagal balance) than the control group (p = 0.06). Also, delirious patients had a significantly greater reduction in standard deviation of RR-intervals (SDNN) (representing total variability) from baseline than controls (p = 0.01) during HUT.
Conclusions
This explorative pilot study on autonomic cardiovascular control in delirium suggests that there may be differences in HRV that should be further investigated in larger samples.
Similar content being viewed by others
Background
Delirium is a common disorder among hospitalised older patients, characterised by an acute onset and fluctuating course, altered arousal, inattention and cognitive problems [1]. Infections are among the most common precipitating causes of delirium. Despite its severity, the underlying pathophysiology of delirium is poorly understood [2]. The clinical features of delirium might suggest aberrations in acute stress responses, involving alterations in autonomic nervous system (ANS) activity [3].
ANS activity can be indirectly assessed by measuring heart rate variability (HRV). HRV refers to the beat-to-beat variations in the sinus rhythm and results from the constant interaction between sympathetic and parasympathetic activity [4]. When subjected to an orthostatic challenge (e.g., head-up tilt testing [HUT]), the ANS must compensate to maintain cardiovascular homeostasis.
Overall HRV decreases with age [5], is negatively associated with frailty status [6], and is inversely related to infection biomarkers such as C-reactive protein (CRP) [7, 8]. Further, there is evidence that reduced HRV is associated with cognitive impairment [9,10,11]. HRV in patients with delirium has been investigated previously in two studies, both in intensive care unit (ICU) patients [12, 13]. Zaal and co-workers did not find any significant differences in HRV parameters between ICU patients with (n = 12) and without (n = 13) delirium [12], whereas a recent study (n = 60) from South Korea found an association between delirium and increased HRV [13]. To our knowledge, HRV in delirium has not previously been studied outside the ICU, and especially not in older medical patients.
The aim of our study was to explore autonomic cardiovascular control in older medical patients with and without delirium, and particularly to assess possible differences in HRV according to delirium status. Due to the lack of previous knowledge about ANS activity during an episode of delirium, an explorative approach was chosen.
Methods
Patients
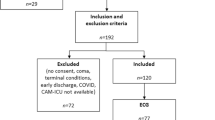
Patients admitted acutely with an infection to the acute geriatric ward at Oslo University Hospital were eligible for the study. We excluded patients with atrial fibrillation, pacemaker rhythm, or on current treatment with beta-blockers, calcium channel blockers or acetylcholinesterase inhibitors. The recruitment was pragmatic and took place whenever the investigator had the opportunity to be in the ward. If the patients did not fulfil any exclusion criteria, they were asked by the investigator (BEN) to participate in a head-up tilt-test (HUT) the next morning, between 9 and 10 a.m., performed by the same investigator. Written and oral information was given by BEN to the patient and to their relatives. Written consent was obtained the next day.
Ethics
The study was approved by the Regional Committee for Ethics in Medical Research in Norway (REK 2011/2498) on 28 February 2012, and by the Data Protection Authorities. The study was undertaken in accordance with the Declaration of Helsinki. Patients were enrolled based either on written consent or on presumed consent in combination with written assent from the nearest relative.
Delirium assessments
Delirium was diagnosed by the researcher (BEN; physician trained in geriatrics) performing the HUT. The researcher visited the patient the day before HUT and spent time with the patient the next day. A structured patient interview, cognitive tests (Mini Mental State Examination [MMSE]) [14] and attention tests (digit span) were performed shortly after HUT. The Confusion Assessment Method (CAM) [15] was used for delirium screening, and “Months Of The Year Backwards” [16] and “Days Of The Week Backwards”, as well as DelApp [17] and the Observational Scale of Level of Arousal (OSLA) [18] were also used in the delirium assessment. All chart notes (nurses and doctors) were scrutinized for evidence of delirium symptoms during night-shifts, possible fluctuations, and resolution of symptoms. The delirium diagnosis was made according to the DSM-5 criteria [19], based on a comprehensive approach; observing and interviewing the patient, test results, and information from staff members and case notes. Delirium severity was assessed using the Memorial Delirium Assessment Scale (MDAS) [20].
Head-up tilt tests (HUT)
All HUTs were performed in the morning, between 9 and 10 a.m., in a quiet room with comfortable temperature, by the same investigator (BEN). The HUT took place a number of days after admission, to ensure that the patients were rehydrated and initial medical treatment had started. The patients had fasted overnight, but were allowed to drink (water, juice, milk) and to take their medicines. They were lying supine in their hospital bed, and were attached to a Task Force Monitor (TFM) (CNSystems Medizintechnik, Graz, Austria), a combined hardware and software device for noninvasive recording of cardiovascular variables. Baseline recordings were obtained for 5 min while the patients rested horizontally, before they were tilted head-up to 15 degrees for 10 min. The subjects were asked to relax and remain silent except for comments about discomfort. The low tilt angle chosen (15 degrees) is challenging for the cardiovascular system, but produces less discomfort than larger angles, and was the largest angle possible using the regular hospital beds.
Recordings
Four electrodes were placed for ECG recording, and three band electrodes were placed on the neck and upper abdomen for impedance cardiography (ICG). ICG is a method in which a small electrical potential is applied between the band electrodes (placed on the neck and upper abdomen). This method gives a continuous recording of the transthoracic impedance (dZ/dt) [21]. Blood pressure (BP) was recorded oscillometrically and continuously using the Finapres finger plethysmography technique, recorded from the second or middle finger of the right hand [22]. The continuous BP was calibrated against the oscillometric measurement.
Data analyses
All recordings were transferred online to the TFM for real-time data acquisition. Beat-to-beat stroke volume (SV) was calculated from the impedance signal, and beat-to-beat stroke index (SI) and cardiac index (CI) were obtained by dividing SV and cardiac output (CO) by body surface area (BSA), estimated from the subject’s height and weight. The total peripheral resistance index (TPRI) was calculated from the mean arterial blood pressure (MAP) divided by CO and BSA.
Two time series of 4 min were selected from each patient for analyses; 270–30 s prior to the 15o HUT and 120–360 s after the tilt. Delta-tilt values were calculated (HUT - rest). Ectopic beats, artifacts and their corresponding BP values were manually removed and replaced by linear interpolation. We then computed the median of all cardiovascular variables in all time periods and calculated the medians with total range for the two groups (delirium/no delirium).
Heart rate variability (HRV) analyses
The ECG signal was subjected to spectral analysis using an adaptive autoregressive algorithm that creates a time-varying spectrum [23] from consecutive segments of the biosignals [24, 25]. The length of these segments varies, as the biosignals are continuously monitored for departure from stationarity, and the segment boundaries placed accordingly. The power spectral density (PSD) is the power distribution across frequencies, representing total variability. For analysis of the power spectrum, we used fixed frequency bands, defined as: Very low frequency (VLF) < 0.04 Hz; low frequency (LF) 0.04–0.15 Hz, and high frequency (HF) 0.15–0.40 Hz. HF and LF power were converted to normalized units (nu); HFnu = HF/(total power - VLF)× 100. LF is considered to measure both parasympathetic and sympathetic modulation of the sine node; HF solely parasympathetic modulation, and the LF/HF-ratio to reflect the sympathovagal balance [4].
We also measured HRV using time domain analyses [4]. Standard deviation of RR-intervals (SDNN) is the standard deviation of all normal RR-distances and correlates with PSD, representing total variability. pNN50 is the proportion of successive RR-intervals that differ by more than 50 ms. RMSSD is the square root of the mean square differences of successive RR-intervals. pNN50 and RMSSD correlate with HF and are assumed to measure parasympathetic modulation.
Background variables
Demographic data were collected at inclusion. Comorbidity was evaluated using the Cumulative Illness Rating Scale (CIRS) [26]. The American Society of Anesthesiologists (ASA) score [27] and the Acute Physiology and Chronic Health Evaluation version 2 (APACHE II) [28] score were used for assessment of physiological disruption. The proxy-based Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) [29] and the Clinical Dementia Rating scale (CDR) [30] were used to assess pre-existing cognitive impairment. Level of functioning was evaluated using the Barthel Activities of Daily Living Index [31], an index of primary activities of daily living. Venous blood samples were drawn and analysed, following standard hospital procedures. Body mass index (BMI) was calculated from height and weight. Weight was measured while standing or sitting on an electronic scale with light clothing, and height measured using a metric rule (patient either lying supine in bed or standing against a wall).
Statistical analysis
The data were exported from the TFM software to Microsoft Excel for further preparation and then transferred to SPSS Statistics version 24 (IBM, Armonk NY) for statistical analysis. We computed the median of the hemodynamic variables in all the epochs and calculated the medians with total range for the groups separately. We applied parametric (t-test) and non-parametric (Mann-Whitney test) analyses for group comparisons as appropriate. The Wilcoxon signed rank test was used for comparisons of paired observations. A p-value of < 0.05 was considered statistically significant.
Results
Fourteen participants (five with delirium) were included between March 2012 and January 2015 among patients admitted to the acute geriatric ward at Oslo University Hospital (Table 1). The patients had respiratory tract infections (n = 8), urinary tract infections (n = 4), erysipelas (n = 1) or cholecystitis (n = 1). Patients with delirium had higher CRP values at the time of HUT (median 174 [range 67–306] mg/L vs 62 [7–191] mg/L; p = 0.04). They were also older (median 89 [84–91] years vs 86 [74–91] years), had a higher CIRS score (median 14 [7–19] vs 10 [1–17]) and a lower Nottingham Extended Activities of Daily Living (NEADL) score (median 28 [9–30] vs 52 [13–66]), but these differences were not statistically significant. The percentage of patients with an IQCODE > 3.82 was similar in the delirium group (40%) and in the group without delirium (44%).
Autonomic response to HUT 15 degrees
Descriptive data for all patients during supine rest and HUT to 15 degrees show that HR and BP values were stable during tilt. There was a slight, but significant decrease in SI (p < 0.001) and an increase in TPRI (p < 0.001) during HUT (Table 2). Indices indicating increased sympathetic activity (LF-variables and LF/HF-ratio) also increased slightly, but these changes were not significant.
Hemodynamic regulation according to delirium status
At rest, values for HR, BP and indices for SV, CO, TPR and end diastolic volume were similar for patients with and without delirium (Table 3). There were also no significant differences between the groups in these conventional cardiovascular variables during HUT. However, there was a trend for both systolic BP and HR to increase more during tilt in the delirium group.
Heart rate variability according to delirium status
At rest, all HRV indices were higher in the delirium group, but the differences were not statistically significant (Table 4). In particular, there was a tendency in the delirium group to higher values for LFabs (p = 0.06), SDNN (p = 0.06) and pNN50 (p = 0.06). At 150 tilt, the delirious patients had a tendency to higher PSD (p = 0.06), lower LFnu and higher HFnu, and thus a lower LF/HF-ratio than the control group (p = 0.06). Delirious patients had a significantly more pronounced reduction in SDNN from baseline than the controls (p = 0.01). Patients with delirium also had a larger but non-significant reduction in PSD during HUT compared with the non-delirious group.
Discussion
In this study, we explored possible differences in autonomic nervous activity between geriatric patients with and without delirium. Even within this small sample, there are some notable findings:
Firstly, there were no significant differences between patients with and without delirium with respect to the regulation of conventional cardiovascular variables, either at rest or during HUT. However, there was a non-significant trend for both HR and BP values to increase more during HUT in the delirious group. One possible explanation for this difference in MAP values is the existence of different central set-points of MAP between the groups. If patients in the delirium group have a higher MAP set-point, the HR and TPRI will increase more in these patients to reach this set-point during HUT [32].
Secondly, the resting values of HRV variables, both in frequency and time domains, indicate that the patients with delirium had a stronger autonomic modulation of the sinus node. At rest, patients with delirium tend to have higher HRV indices, in particular indices indicating parasympathetic control (such as HFabs, pNN50 and RMSSD), but sympathetic modulation might also be greater, as LFabs is a result of both sympathetic and parasympathetic activity. This results in higher values of PSD and SDNN (total variability) in the group with delirium. During tilt, the variability tends to fall in the delirium group (indicated by a larger reduction in PSD and SDNN) compared to the no delirium group.
Autonomic modulation will usually increase during head-up tilt. In contrast, the patients with delirium displayed a fall in many indices, resulting in a lower total variability in the delirium group. There was also no increase in the LF/HF-ratio (increased sympathovagal balance) in patients with delirium, as is normally seen during orthostatic stress. These results are difficult to interpret. One possible explanation for the lack of variability increase during tilt in the delirious patients might be that they are already using their maximal capacity for autonomic modulation at rest. They have already been brought to the fringe of their buffering capacity, and a further challenge (such as HUT) brings them “outside” the range of their homeostatic control systems, and thus variability does not increase as expected [32, 33].
Generally, high modulation is a sign of a healthy and robust regulatory system that can compensate adequately for external changes, to maintain normal homeostasis [33]. The decrease in ANS activity/modulation at tilt might indicate a less robust regulatory system/homeostatic mechanism in patients with delirium.
The patients in the delirium group had a lower functional level before hospitalisation (NEADL), as well as higher inflammatory markers (CRP and leukocytes) than the control group. This is to be expected, as older age, pre-existing cognitive impairment and functional decline are well-known predisposing factors, and infection is a common precipitating factor for delirium [1]. Frailty, cognitive impairment and infection have been previously shown to be negatively associated with HRV [6,7,8,9,10,11]. We would thus expect lower HRV in the delirium group than in the controls. However, our findings appear to indicate the opposite.
We are aware of two previous studies investigating HRV in patients with delirium [12, 13]. Zaal et al. analysed HRV measured in the frequency domain in 25 ICU patients (13 with delirium) and did not find any significant differences in HFnu and LF/HF-ratio. However, the direction of their results was such that mean HFnu was higher in patients with delirium (67 vs 57), particularly in the hypoactive state, while the LF/HF-ratio was lower in delirium. The direction of the changes was thus the same as in the present study. In addition, a recent study of HRV in ICU patients found that delirium was associated with high SDNN and RMSSD [13]. These results are also in line with those of our study.
Strengths of this study are that we have explored HRV in both the frequency domain and time domain, using a well-defined, standardized protocol including a tilt test. Our results (Table 2) indicate that the modified HUT to 15 degrees gave physiologically plausible results, even though the orthostatic challenge was small. There are also limitations to this work that should be noted. Our study is underpowered and too small to draw firm conclusions; the study is thus exploratory in nature. Many indices from the ANS were examined and, in principle, the issue of multiple comparisons should have been addressed. However, the sample size is too small to do so. The investigators who assessed the data were not blind to the patients’ delirium status. Due to multimorbidity, some patients in the ward were not eligible for the study, especially because of atrial fibrillation and the use of beta-blockers. Further, it is not clear if the HUT could be undertaken in hyperactive delirium. This may impair the generalizability of our findings.
Conclusions
This explorative pilot study on autonomic cardiovascular control in delirium, suggests that there could be differences in HRV that should be further explored. A head-up tilt test is feasible in older medical patients, also in patients with hypoactive and mixed delirium.
Abbreviations
- ANS:
-
Autonomic nervous system
- BP:
-
Blood pressure
- BSA:
-
Body surface area
- CI:
-
Cardiac index
- CO:
-
Cardiac output
- EDV:
-
End-diastolic volume
- HF (nu):
-
High frequency (normalized units)
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- HUT:
-
Head-up tilt
- ICG:
-
Impedance cardiography
- LF (nu):
-
Low frequency (normalized units)
- MAP:
-
Mean arterial blood pressure
- pNN50:
-
The proportion of successive RR-intervals that differ by more than 50 ms
- PSD:
-
Power spectral density
- RMSSD:
-
Square root of the mean square differences of successive RR-intervals
- SDNN:
-
Standard deviation of RR-intervals
- SI:
-
Stroke index
- SV:
-
Stroke volume
- TFM:
-
Task Force Monitor
- TPR:
-
Total peripheral resistance
- TPRI:
-
Total peripheral resistance index
- VLF:
-
Very low frequency
References
Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22.
Maldonado JR. Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am J Geriatr Psychiatry. 2013;21(12):1190–222.
Maclullich AM, Ferguson KJ, Miller T, de Rooij SE, Cunningham C. Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses. JPsychosomRes. 2008;65(3):229–38.
Malik M. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task force of the European Society of Cardiology and the north American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17(3):354–81.
Almeida-Santos MA, Barreto-Filho JA, Oliveira JL, Reis FP, da Cunha Oliveira CC, Sousa AC. Aging, heart rate variability and patterns of autonomic regulation of the heart. Arch Gerontol Geriatr. 2016;63:1–8.
Parvaneh S, Howe CL, Toosizadeh N, Honarvar B, Slepian MJ, Fain M, Mohler J, Najafi B. Regulation of cardiac autonomic nervous system control across frailty statuses: a systematic review. Gerontology. 2015;62(1):3–15.
Huang C, Alamili M, Rosenberg J, Gogenur I. Heart rate variability is reduced during acute uncomplicated diverticulitis. J Crit Care. 2016;32:189–95.
Papaioannou VE, Dragoumanis C, Theodorou V, Gargaretas C, Pneumatikos I. Relation of heart rate variability to serum levels of C-reactive protein, interleukin 6, and 10 in patients with sepsis and septic shock. J Crit Care. 2009;24(4):625 e621–627.
Zeki Al Hazzouri A, Haan MN, Deng Y, Neuhaus J, Yaffe K. Reduced heart rate variability is associated with worse cognitive performance in elderly Mexican Americans. Hypertension. 2014;63(1):181–7.
Kim DH, Lipsitz LA, Ferrucci L, Varadhan R, Guralnik JM, Carlson MC, Fleisher LA, Fried LP, Chaves PH. Association between reduced heart rate variability and cognitive impairment in older disabled women in the community: Women's health and aging study I. J Am Geriatr Soc. 2006;54(11):1751–7.
Zulli R, Nicosia F, Borroni B, Agosti C, Prometti P, Donati P, De Vecchi M, Romanelli G, Grassi V, Padovani A. QT dispersion and heart rate variability abnormalities in Alzheimer's disease and in mild cognitive impairment. J Am Geriatr Soc. 2005;53(12):2135–9.
Zaal IJ, van der Kooi AW, van Schelven LJ, Oey PL, Slooter AJ. Heart rate variability in intensive care unit patients with delirium. J Neuropsychiatry Clin Neurosci. 2014:41(12);2130-7.
Jooyoung O, Dongrae C, Jongin K, Jaeseok H, Jaesub P, Se Hee N, Cheung Soo S, Jae-Jin K, Jin Young P, Boreom L. Changes in heart rate variability of patients with delirium in intensive care unit. Conf Proc IEEE Eng Med Biol Soc. 2017;2017:3118–21.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI: Clarifying confusion: the confusion assessment method. A new method for detection of delirium. AnnInternMed 1990, 113(12):941–948.
O'Regan NA, Ryan DJ, Boland E, Connolly W, McGlade C, Leonard M, Clare J, Eustace JA, Meagher D, Timmons S. Attention! A good bedside test for delirium? J Neurol Neurosurg Psychiatry. 2014;85(10):1122–31.
Tieges Z, Stiobhairt A, Scott K, Suchorab K, Weir A, Parks S, Shenkin S, MacLullich A. Development of a smartphone application for the objective detection of attentional deficits in delirium. International psychogeriatrics / IPA. 2015;27(8):1251-62.
Tieges Z, McGrath A, Hall RJ, Maclullich AM. Abnormal level of arousal as a predictor of delirium and inattention: an exploratory study. Am J Geriatr Psychiatry. 2013;21(12):1244–53.
AmericanPsychiatricAssociation. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington DC: American Psychiatric Association; 2013.
Breitbart W, Rosenfeld B, Roth A, Smith MJ, Cohen K, Passik S. The memorial delirium assessment scale. J Pain Symptom Manag. 1997;13(3):128–37.
Denniston JC, Maher JT, Reeves JT, Cruz JC, Cymerman A, Grover RF. Measurement of cardiac output by electrical impedance at rest and during exercise. JApplPhysiol. 1976;40(1):91–5.
Parati G, Casadei R, Groppelli A, Di RM, Mancia G. Comparison of finger and intra-arterial blood pressure monitoring at rest and during laboratory testing. Hypertension. 1989;13(6 Pt 1):647–55.
Fortin J, Habenbacher W, Gruellenberger R, Wach P, Skrabal F: Real-time monitor for hemodynamic beat-to-beat parameters and power spectra analysis of the biosignals. In: Proceedings of the 20th Annual International Conference of the IEEE Engineering in Medicine and Biology Society Vol20 Biomedical Engineering Towards the Year 2000 and Beyond (Cat No98CH36286): 29 Oct-1 Nov 1998 1998. 360–363 vol.361.
Cerutti S, Bianchi AM, Mainardi LT. Advanced spectral methods for detecting dynamic behaviour. Auton Neurosci. 2001;90(1–2):3–12.
Barlow JS. Methods of analysis of nonstationary EEGs, with emphasis on segmentation techniques: a comparative review. J Clin Neurophysiol. 1985;2(3):267–304.
Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, Spazzafumo L, Mancinelli L, Espinosa E, Rappelli A, et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. JAmGeriatrSoc. 2008;56(10):1926–31.
American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24(111).
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Jorm AF. A short form of the informant questionnaire on cognitive decline in the elderly (IQCODE): development and cross-validation. PsycholMed. 1994;24(1):145–53.
Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Maryland state medical journal. 1965;14:61–5.
Stauss HM. Baroreceptor reflex function. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002;283(2):R284–6.
Goldstein DS. The autonomic nervous system in health and disease. New York: MarcelDekker; 2001.
Acknowledgements
We thank the Department of Cardiology at Oslo University Hospital, Ullevål, for kindly giving us permission to use their Task Force Monitor.
Funding
This study was funded by the University of Oslo. The sponsors had no role in the design, methods, subject recruitment, data collection, analysis or preparation of the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
VBW and TBW conceived the study. BEN carried out all experimental procedures, clinical assessments, collected data and wrote the first manuscript draft. All authors contributed to data interpretation and further revisions of the manuscript. The final paper has been approved by all authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Regional Committee for Ethics in Medical Research in Norway (REK 2011/2498) on 28 February 2012, and by the Data Protection Authorities. All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Patients were enrolled based either on written consent or on presumed consent in combination with written assent from the nearest relative.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no conflicts of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Neerland, B.E., Wyller, T.B. & Wyller, V.B.B. Autonomic cardiovascular control in older patients with acute infection and delirium: a pilot study of orthostatic stress responses. BMC Geriatr 19, 23 (2019). https://doi.org/10.1186/s12877-019-1035-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-019-1035-0