Abstract
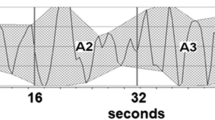
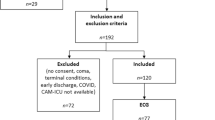
This study aimed to investigate the relationship between heart rate variability (HRV), a parameter of the autonomic nervous system activity (ANSA), and postoperative delirium and postoperative events. This retrospective cohort study included elderly patients aged 65 years or older who were admitted to the intensive care unit (ICU) after cardiovascular surgery. ANSA was measured using HRV parameters for 1 h at daytime and 1 h at night-time before ICU discharge. The primary endpoint was the effect of HRV parameters and delirium on mortality and readmission rates within 1 year after discharge, and the secondary endpoint was the association between HRV parameters and delirium. Cox proportional hazards models were used to examine the association between HRV parameters and postoperative events by adjusting for delirium and pre and postoperative information. A total of 71 patients, 39 without delirium and 32 with delirium, met the inclusion criteria. The incidence of death and readmission within 1 year was significantly higher in the delirium group and in the group with higher daytime HF (high frequency power) and r-MSSD (square root of the squared mean of the difference of successive NN intervals), parameters of the parasympathetic nervous system activity (PNSA), than that in other groups. Furthermore, the delirium group had significantly higher HF and r-MSSD than the nondelirium group. Even after adjusting for confounding factors in the multivariate analysis, a trend of higher daytime HF and r-MSSD was observed, indicating a significant effect on the occurrence of combined events within 1 year of discharge. ICU delirium has been associated with higher daytime HF and r-MSSD, parameters of PNSA. ICU delirium was a prognostic factor, and increased daytime PNSA may worsen the prognosis of elderly patients after cardiovascular surgery.


Similar content being viewed by others
References
Sakata R, Fujii Y, Kuwano H (2010) Thoracic and cardiovascular surgery in Japan during 2008: annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 58:356–383
Japanese Society of Intensive Care Medicine Early Rehabilitation Review Committee (2017) Early rehabilitation in intensive care: an evidence-based expert consensus. J Jpn Soc Intensive Care Med 24:255–303
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. The Lancet 383:911–922
Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, Jones RN (2012) Cognitive trajectories after postoperative delirium. N Engl J Med 367:30–39
Jooyoung Oh, Cho D, Kim J, Heo J, Park J, Na SH, Shin CS, Kim J-J, Park JY, Lee B (2017) Changes in heart rate variability of patients with delirium in intensive care unit. Annu Int Conf IEEE Eng Med Biol Soc 2017:3118–3121
Galinier M, Pathak A, Fourcade J, Androdias C, Curnier D, Varnous S, Boveda S, Massabuau P, Fauvel M, Senard JM, Bounhoure JP (2000) Depressed low frequency power of heart rate variability as an independent predictor of sudden death in chronic heart failure. Eur Heart J 21:475–482
Schmidt H, Müller-Werdan U, Hoffmann T, Francis DP, Piepoli MF, Rauchhaus M, Prondzinsky R, Loppnow H, Buerke M, Hoyer D, Werdan K (2005) Autonomic dysfunction predicts mortality in patients with multiple organ dysfunction syndrome of different age groups. Crit Care Med 33:1994–2002
Florea VG, Cohn JN (2014) The autonomic nervous system and heart failure. Circ Res 114:1815–1826
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, Simon AB, Rector T (1984) Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 311:819–823
Benedict CR, Johnstone DE, Weiner DH, Bourassa MG, Bittner V, Kay R, Kirlin P, Greenberg B, Kohn RM, Nicklas JM (1994) Relation of neurohumoral activation to clinical variables and degree of ventricular dysfunction: a report from the Registry of Studies of Left Ventricular Dysfunction. SOLVD Investigators. J Am Coll Cardiol 23:1410–1420
Kaye DM, Lefkovits J, Jennings GL, Bergin P, Broughton A, Esler MD (1995) Adverse consequences of high sympathetic nervous activity in the failing human heart. J Am Coll Cardiol 26:1257–1263
Barretto ACP, Santos AC, Munhoz R, Rondon MUPB, Franco FG, Trombetta IC, Roveda F, de Matos LNJ, Braga AMW, Middlekauff HR, Negrão CE (2009) Increased muscle sympathetic nerve activity predicts mortality in heart failure patients. Int J Cardiol 135:302–307
Cygankiewicz I, Zareba W (2013) Heart rate variability. Handb Clin Neurol 117:379–393
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Higuchi S, Kabeya Y, Matsushita K, Taguchi H, Ishiguro H, Kohshoh H, Yoshino H (2016) Barthel index as a predictor of 1-year mortality in very elderly patients who underwent percutaneous coronary intervention for acute coronary syndrome: better activities of daily living, longer life. Clin Cardiol 39:83–89
Bluhmki E, Chamorro A, Dávalos A, Machnig T, Sauce C, Wahlgren N, Wardlaw J, Hacke W (2009) Stroke treatment with alteplase given 3.0-4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 8:1095–1102
Di Monaco M, Castiglioni C, De Toma E, Gardin L, Giordano S, Tappero R (2015) Handgrip strength is an independent predictor of functional outcome in hip-fracture women: a prospective study with 6-month follow-up. Medicine (Baltimore) 94:e542
Gillman MW, Kannel WB, Belanger A, D’Agostino RB (1993) Influence of heart rate on mortality among persons with hypertension: the Framingham Study. Am Heart J 125:1148–1154
Hozawa A, Ohkubo T, Kikuya M, Ugajin T, Yamaguchi J, Asayama K, Metoki H, Ohmori K, Hoshi H, Hashimoto J, Satoh H, Tsuji I, Imai Y (2004) Prognostic value of home heart rate for cardiovascular mortality in the general population: the Ohasama study. Am J Hypertens 17:1005–1010
Fox K, Ford I, Steg PG, Tendera M, Ferrari R (2008) Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet 372:807–816
Marek M (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J 17:354–381
Chen I-C, Kor C-T, Lin C-H, Kuo J, Tsai J-Z, Ko W-J, Kuo C-D (2018) High-frequency power of heart rate variability can predict the outcome of thoracic surgical patients with acute respiratory distress syndrome on admission to the intensive care unit: a prospective, single-centric, case-controlled study. BMC Anesthesiol 18:34
Papaioannou VE, Maglaveras N, Houvarda I, Antoniadou E, Vretzakis G (2006) Investigation of altered heart rate variability, nonlinear properties of heart rate signals, and organ dysfunction longitudinally over time in intensive care unit patients. J Crit Care 21:95–103 (discussion 103-104)
Rollo E, Marotta J, Callea A, Brunetti V, Vollono C, Scala I, Imperatori C, Frisullo G, Broccolini A, Della Marca G (2022) Heart rate variability and delirium in acute non-cardioembolic stroke: a prospective, cross-sectional, cohort study. Neurol Sci 43:2423–2431
Norris PR, Ozdas A, Cao H, Williams AE, Harrell FE, Jenkins JM, Morris JA (2006) Cardiac uncoupling and heart rate variability stratify ICU patients by mortality: a study of 2088 trauma patients. Ann Surg 243:804–812 (discussion 812-814)
Bradley BD, Green G, Ramsay T, Seely AJE (2013) Impact of sedation and organ failure on continuous heart and respiratory rate variability monitoring in critically ill patients: a pilot study. Crit Care Med 41:433–444
Harris BR, Beesley SJ, Hopkins RO, Hirshberg EL, Wilson E, Butler J, Oniki TA, Kuttler KG, Orme JF, Brown SM (2021) Heart rate variability and subsequent psychological distress among family members of intensive care unit patients. J Int Med Res 49:3000605211057829
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y (2001) Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med 27:859–864
Kim S, Han H-S, Jung H, Kim K, Hwang DW, Kang S-B, Kim C-H (2014) Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg 149:633–640
Eijsvogels TMH, Maessen MFH, Bakker EA, Meindersma EP, van Gorp N, Pijnenburg N, Thompson PD, Hopman MTE (2020) Association of cardiac rehabilitation with all-cause mortality among patients with cardiovascular disease in the Netherlands. JAMA Netw Open 3:e2011686
Salata K, Hussain MA, de Mestral C, Greco E, Aljabri BA, Mamdani M, Forbes TL, Bhatt DL, Verma S, Al-Omran M (2019) Comparison of outcomes in elective endovascular aortic repair vs open surgical repair of abdominal aortic aneurysms. JAMA Netw Open 2:e196578
Buckley U, Shivkumar K, Ardell JL (2015) Autonomic regulation therapy in heart failure. Curr Heart Fail Rep 12:284–293
Li M, Zheng C, Sato T, Kawada T, Sugimachi M, Sunagawa K (2004) Vagal nerve stimulation markedly improves long-term survival after chronic heart failure in rats. Circulation 109:120–124
Vaseghi M, Shivkumar K (2008) The role of the autonomic nervous system in sudden cardiac death. Prog Cardiovasc Dis 50:404–419
Tindle J, Tadi P (2021) Neuroanatomy, parasympathetic nervous system. In: StatPearls. StatPearls Publishing, Treasure Island
Eckberg DL, Drabinsky M, Braunwald E (1971) Defective cardiac parasympathetic control in patients with heart disease. N Engl J Med 285:877–883
Brubaker PH, Kitzman DW (2011) Chronotropic incompetence: causes, consequences, and management. Circulation 123:1010–1020
Dimopoulos S, Anastasiou-Nana M, Sakellariou D, Drakos S, Kapsimalakou S, Maroulidis G, Roditis P, Papazachou O, Vogiatzis I, Roussos C, Nanas S (2006) Effects of exercise rehabilitation program on heart rate recovery in patients with chronic heart failure. Eur J Cardiovasc Prev Rehabil 13:67–73
Jin L, Min G, Wei C, Min H, Jie Z (2017) Exercise training on chronotropic response and exercise capacity in patients with type 2 diabetes mellitus. Exp Ther Med 13:899–904
Zaal IJ, van der Kooi AW, van Schelven LJ, Oey PL, Slooter AJC (2015) Heart rate variability in intensive care unit patients with delirium. J Neuropsychiatry Clin Neurosci 27:e112-116
Neerland BE, Wyller TB, Wyller VBB (2019) Autonomic cardiovascular control in older patients with acute infection and delirium: a pilot study of orthostatic stress responses. BMC Geriatr 19:23
Alamili M, Rosenberg J, Gögenur I (2015) Day-night variation in heart rate variability changes induced by endotoxaemia in healthy volunteers. Acta Anaesthesiol Scand 59:457–464
Okada K, Kurita A, Takase B, Otsuka T, Kodani E, Kusama Y, Atarashi H, Mizuno K (2009) Effects of music therapy on autonomic nervous system activity, incidence of heart failure events, and plasma cytokine and catecholamine levels in elderly patients with cerebrovascular disease and dementia. Int Heart J 50:95–110
Sinha M, Behera AK, Sinha R, Parganiha A, Pande B, Sharma R, Pati AK (2021) Circadian rhythmicity of heart rate variability and its impact on cardiac autonomic modulation in asthma. Chronobiol Int 38:1631–1639
Evrengul H, Tanriverdi H, Kose S, Amasyali B, Kilic A, Celik T, Turhan H (2006) The relationship between heart rate recovery and heart rate variability in coronary artery disease. Ann Noninvasive Electrocardiol 11:154–162
Acknowledgements
We would like to thank the cardiac rehabilitation team of Shinshu University for their cooperation in data collection and the patients who underwent cardiovascular surgery at Shinshu University for participating in this study.
Funding
This research was supported by a research grant from the Japanese Physical Therapy Association (No. 20-A19).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsukakoshi, D., Yamamoto, S., Nojima, I. et al. Association between postoperative delirium and heart rate variability in the intensive care unit and readmissions and mortality in elderly patients with cardiovascular surgery. Heart Vessels 38, 438–447 (2023). https://doi.org/10.1007/s00380-022-02173-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02173-1