Abstract
Disgust sensitivity refers to how unpleasant a disgusting experience is to an individual and is involved in the development of many psychiatric conditions. Given its link with food ingestion, there is an interest in understanding how an individual’s susceptibility to disgust relates to dietary habits. One possible mechanism giving rise to this association is through the effects negative emotions have on high-order cognitive processes, but few studies take this model into account. The aim of this study was to characterize general disgust sensitivity in a clinical binge eating disorder (BED) population, and explore whether disgust sensitivity relates to inhibitory control and eating pathology. Following a case-controlled study design, our results show that: (1) disgust sensitivity and its subscales do not differ between BED and healthy controls, (2) higher disgust sensitivity in BED relates to greater behavioural inhibition, (3) inhibitory control reaction times relate to aspects of eating pathology, and (4) inhibitory control does not mediate relationships between disgust sensitivity and BMI among participants with BED. Understanding the role of disgust sensitivity in BED may allow us to understand how negative emotion systems maintain dysregulated eating behaviours with the potential to inform emotion-regulation treatment approaches. Level of evidence: Level III: Evidence obtained from well-designed cohort or case–control analytic studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disgust sensitivity and inhibitory control
Disgust is a universally experienced primary emotion that serves to guide cognitive and behavioural functioning away from risk of infection and contamination by influencing eating cessation/food avoidance [1,2,3]. However, fairly little research has examined this construct to date. Behavioural components of disgust include modified facial expressions and actions that include stopping and dropping objects of disgust, shuddering or uttering “Ew!” [1, 2]. Its physiological components include nausea, gagging, lowered blood pressure and increased galvanic skin responses, which together can stop consummatory behaviours [4, 5]. Encompassing sensory and cognitive processes, disgust can influence eating cessation and avoidance of certain foods as well as other eating behaviours (i.e., anticipating how a certain food will taste, or the consequence of eating a certain food) [1], even without physical contact. For example, nausea, the most characteristic physiological manifestation of disgust, can influence food/eating avoidance without physical consumption [1]. Given this intimate link with food ingestion, there is an interest in understanding how an individual’s susceptibility to disgust relates to dietary habits.
One subfactor of disgust is disgust sensitivity—referring to how unpleasant a disgusting experience is to an individual [6]. With the capacity to rapidly link cognitive and affective processes, disgust sensitivity may also relate to the development and maintenance of psychiatric disorders [1]. To date, most research on disgust sensitivity has been in anxiety-related disorders [7,8,9,10,11,12,13,14,15,16,17,18], with additional investigations in avoidant behaviour [19], obsessive–compulsive behaviours [8, 20, 21] and social anxiety disorder [22, 23]. Very little research has investigated disgust sensitivity in eating disorders (EDs), and in binge eating disorder (BED) in particular [24]—one of the most commonly diagnosed EDs [25].
Given the universal nature of disgust sensitivity, this construct may be understood as a component of larger negative cognitive processes [1]. There is evidence that disgust sensitivity may be linked to both healthy and unhealthy eating [26]. Several disgust sensitivity theories suggest that this construct can serve as a protective mechanism preventing the consumption of risky foods with a potential high pathogen load (i.e., a rejection response surrounding eating) [3]. However, in the context of EDs, this construct may serve as an affective process associated with more restrictive eating behaviour (i.e., working in opposition to the hunger drive) [3, 26] driven by psychosocial factors influencing a person’s perspective of food and the body. Consistent with this second notion, disgust sensitivity relates to certain dysregulated eating behaviours, and eating pathology more generally [28,29,30]. Disgust sensitivity could move individuals away from a feared outcome different from infection—rather a fear of weight gain and/or feelings of fullness. While these hypotheses (protective anti-pathogen mechanism vs psychosocial affective process) are not mutually exclusive, they nevertheless represent different lenses for examining a possible (dys)functional role of disgust in eating behaviours—either through a general oversensitivity or acting as a defensive mechanism related to eating and weight domains.
Disgust sensitivity in eating disorders and links with eating pathology
Rather than a generic process, disgust sensitivity across EDs may pertain primarily to areas concerned with food and the body [31, 32]. Indeed, relationships seem to exist between anorexia nervosa (AN) and bulimia nervosa (BN) and disgust related to animal foodstuff, and body-related stimuli. More specifically, in healthy adults and patients with AN, heightened disgust sensitivity associates with greater Drive for Thinness, Bulimia, Body Dissatisfaction, Ineffectiveness, Eating Disorders Inventory (EDI) total scores, and Eating Attitudes Test (EAT) total scores [29, 31]. Related to this notion (but looking at more psychological variables, rather than diagnoses), there is some evidence for relationships between restraint/drive for thinness and disgust sensitivity (especially to food). For instance, in clinical ED populations (including AN-restricting subtype, AN-binge/purge subtype, BN, eating disorder not otherwise specified and obese binge eaters) symptoms of AN measured via the Drive for Thinness subscale of the EDI also positively correlate with disgust sensitivity to Food and Magical Contagion [31]. Furthermore, higher Bulimia subscale scores of the EDI are associated with increased disgust sensitivity to Animals, Death, Body Envelope Violation and Magical Contagion, and marginally with overall Disgust Sensitivity [31]. In another clinical ED sample (diagnoses not specified), higher Drive for Thinness correlates with increased Core Disgust, Animal Reminder, Contamination-Based Disgust, Disgust Sensitivity, and higher Body Dissatisfaction correlates with increased Core Disgust, Contamination-Based Disgust and Disgust Sensitivity [33]. Collectively, these results suggest that disgust sensitivity to food/body-related stimuli appear related to measures of disordered eating—both to BN (measuring fear of loss of control over eating and compensatory efforts) and Drive for Thinness.
There are some mixed findings linking disgust constructs with eating behaviours and clinical measures. In nonclinical populations, a higher body mass index (BMI) is linked with decreased Core Disgust and Contamination-Based Disgust levels; whereas higher reported disgust levels are associated with increased restrained eating behaviours [34]. In further support of this association, heightened Core Disgust sensitivity relates to measures of self-disgust, motivating restrained eating behaviours with high BMI in non-obese individuals [26]. However, one early study did not find associations between food-related disgust and the avoidance of high calorie/highly palatable foods in a nonclinical sample of women [35]. Nevertheless, participants with AN or BN diagnoses show significantly higher levels of disgust sensitivity on Foodstuff of Animal Origin, Human Body Products, and Gastro-enteric Products subscale of the Disgust Questionnaire compared to a matched, nonclinical control sample [29].
For BED, there is currently no evidence for differences between clinical and non-clinical BED groups in general or food/body-related disgust sensitivity [24]. This is supported by neuroimaging studies demonstrated significant activation of the amygdala, insula and lateral orbitofrontal cortex (OFC) when viewing disgusting stimuli in all participant groups (BED, BN, overweight control subject and normal-weight control subjects)—but no significant group differences [36], suggesting similar activations during generic disgust processing across groups rather than binge-specific differences.
Effects of negative emotions on executive functioning
Multiple theories on the development and maintenance of eating disorders suggest that negative emotions trigger engagement in emotional eating and binge eating episodes in both non-clinical and clinical populations [37, 38] by acting on executive functioning abilities. Current evidence suggests that the onset of BN, characterized by cycles of binging and purging behaviours, co-occurs with periods of negative affect, suggesting associations between emotions and control over eating [39]. Furthermore, negative urgency—the tendency to act impulsively when feeling negative emotions—when combined with expectations that eating will alleviate negative affect, strongly characterises both BN [40, 41] and BED [42]. Based on a negative valence systems model of binge-type eating disorder risk [43], risk factors for binging behaviour (acting independently or in combination) include altered corticolimbic functioning, neuroendocrine dysregulation, and self-reported negative affect. Therefore, negative emotions like disgust may disrupt high-order cognitive processes like inhibitory control—a key feature in binge eating disorders [44,45,46]. For instance, emotions and inhibitory control share a ‘two-way connection’ between emotion processing and inhibitory control through shared brain networks (including the insula and inferior frontal gyrus) [47, 48], which allows emotions to disrupt inhibitory control and vice versa. The insula, which is heavily implicated in interoceptive awareness, emotional processing and response inhibition, may have the ability to ‘hijack’ self-control areas of the brain and affect inhibitory control via its projections that extend to various parts of the prefrontal cortex (housing numerous regions involved in inhibition) [49,50,51,52,53,54]. More specifically, the anterior insula acts as a “relay center” by receiving sensory information (from disgust-inducing stimuli), and subsequently modulates activity in response inhibition networks which consist of the left and right inferior and middle frontal gyri, right superior frontal gyrus, anterior cingulate cortex, anterior insula, subthalamic nucleus, pre-SMA, and dorsal aspects of the striatum [48, 49]. Therefore, disgust sensitivity may have the ability to indirectly influence eating behaviours via its effects on self-control processes; primarily by activating the anterior insula. Indeed, the effects of disgust sensitivity on BMI are mediated through reductions in food-specific inhibitory control [55].
Despite the effects negative emotions have on executive functioning, the relationship between inhibitory control and eating disorders is not straightforward. Response inhibition is generally assessed using validated stopping paradigms such as the Stop Signal Task and Go/No-Go tasks which require participants to withhold behavioural responses when a visual or auditory cue is presented. Impairments in inhibitory control across eating disorders differ between general and ‘disorder-salient’ stimuli (i.e., food/eating, body/shape). For generic stimuli, a meta-analysis of 5 Go/No-Go studies had non-significant effect sizes (Hedge’s g = − 0.39) across bulimic-type ED groups [56]. For food-specific inhibitory control stimuli, only one study showed significant inhibitory control deficits to food/eating stimuli (Hedges’ g = − 0.68, p = 0.042) but not to shape/weight stimuli (p = 0.699) in BN patients [56, 57]. Greater deficits in inhibitory control to food/eating-related stimuli may therefore suggest that inhibitory control specifically to consummatory actions, may underlie recurrent binge eating episode [56]. Response inhibition findings in binge-type eating disorders are also mixed. For food-related inhibitory control, several studies show inhibitory control deficits in BED relative to normal weight and obese controls [57,58,59] with two others showing similar Go/No-Go performance to obese controls [60, 61]. One study found inhibitory control deficits to both generic (non-food related) and food-specific Go/No-Go tasks in participants with BED [62].
Dual-process models [63] of eating proposes that eating behaviour can be understood as the outcome of two different but complementary systems: self-regulatory processes such as inhibitory control (top-down processes) and automatic processes such as automatic appraisal of appetitive stimulus acquired through affective properties (bottom-up processes). Studies have recently begun to take dual-process model into account, based on the premise that automatic affective processes moderate the relationship between inhibitory control and eating behaviour. For example, Liu and colleagues found negative associations between disgust sensitivity and BMI, suggesting that undergraduate students with higher BMIs have lower sensitivity to disgust. Although contradictory to the dual-process premise, the associations between disgust sensitivity and BMI appear to be fully mediated by inhibitory control and not the other way around [55]. Nevertheless, Spinelli and colleagues found no associations between disgust sensitivity, restrained eating and BMI in individuals with obesity. However, higher levels of disgust sensitivity were associated with higher BMI in their sample of non-obese individuals, and this association appeared to be fully mediated by restrained eating behaviours [26]. Both studies were conducted in community samples, therefore it is not clear whether these findings generalize to clinical ED populations. Furthermore, investigations into how response inhibition and disgust sensitivity relate to eating pathology and loss of control eating remain to be examined.
Current study
Considering that BED is the most common ED diagnosed, with lifetime prevalence ranging between 0.2 and 4.7%, and twelve-month prevalence estimates averaging 0.8% nationally [63], there is nevertheless a dearth of empirical studies examining disgust sensitivity in this population. The first aim of this study was to characterize disgust sensitivity in a clinical sample of patients with BED. Based on the findings that individuals with dysregulated eating behaviours exhibit similar levels of disgust to matched controls [28, 31, 36, 65], we hypothesized that individuals with BED would report similar levels of disgust sensitivity compared to healthy controls. If disgust sensitivity reflects more of an affective process associated with psychosocial aspects of eating behaviour or body image, then similar to previous AN and BN literature, we hypothesized that greater eating pathology (i.e., Restraint) would be associated with heightened (rather than lower) disgust sensitivity in our BED sample. In this way, aspects of disgust sensitivity would relate to attitudes around eating and body image domains, rather than BMI.
Given the links between disgust and inhibition, we also sought to explore whether disgust sensitivity might relate to inhibitory control in a BED population. Based on findings that disgust sensitivity is negatively correlated with inhibitory control in healthy controls [55] we hypothesized a similar relationship might exist in a BED sample. Next, we sought to extend associations between disgust sensitivity, behavioural inhibition and BMI to a clinical BED sample. Based on the finding that disgust sensitivity inversely related to BMI [34, 55], we also hypothesized that higher BMI would be significantly negatively associated with disgust sensitivity, and that behavioural inhibition would mediate the relationship.
Methods
Participants
Participants were 70 individuals (94.3% identifying as female gender) currently living in or around Hamilton Ontario, aged 20–64 (M = 41.35, SD = 13.01). Participants primarily identified as European (72.9%), with 4.3% identifying as South Asian (India, Sri Lanka, Pakistan, Nepal, Bangladesh), 5.7% as Native North American, 2.9% as Arab, 1.4% as Persian, and 12.9% as other. To take part in the study, participants were required to be at least 18 years of age. Healthy controls (n = 35) were required to have no current medical or psychiatric conditions, and no active or history of substance or alcohol use disorders. Participants with BED (n = 35) were recruited from the Eating Disorder Program at the St. Joseph’s Healthcare Hamilton West 5th campus in Hamilton, Ontario, Canada. Healthy control participants were recruited from community advertisements, and matched to BED participants on sex and gender. Nine participants were removed from the dataset due to missing Go/No-Go data. A total sample size of 61 participants was used for our analyses (HC N = 32; BED N = 29).
Procedure
The current study consists of data from part of a larger ongoing multi-session study examining reward and stress effects on decision-making and motivation. After obtaining informed consent, participants completed a battery of questionnaires including the MINI Psychiatric Assessment, the Disgust Scale-Revised, the Eating Disorders Examination Questionnaire, and the Beck Anxiety Inventory (descriptions below). Study sessions ended by completing the Go/No-Task. Study procedures were approved by the Hamilton Integrated Research Ethics Board (HiREB, Project 1600).
Measures
Mini-International neuropsychiatric interview (MINI) [66, 67]
The Mini-International Neuropsychiatric Interview is a widely used structured clinical interview to assess major psychiatric disorders in the Diagnostic and Statistics Manual 3rd edition revised (DSM-III-TR), 4th edition (DSM-IV), 5th edition (DSM-V), and the International Classification of Disease 10th Revision (ICD-10). The MINI demonstrates excellent concordance with other structured clinical interviews including the Structured Clinical Interview for Diagnostic and Statistical Manual—patient version diagnoses (SCID-P) [68], and the Composite International Diagnostic Interview (CIDI) [64]. The MINI also demonstrates excellent interrater and retest reliability with Cohen’s kappa values ranging from 0.52 to 1.0 [66].
Disgust scale-revised (DS-R) [69]
The Disgust Scale-Revised is a 27-item self-report inventory modified from the initial 32-item Disgust Scale (DS) [27] designed to measure individual differences in disgust sensitivity. The DS-R assesses sensitivity to three disgust-eliciting domains including Core Disgust, Animal Reminder Disgust, and Contamination-Based Disgust. The DS-R demonstrates good internal validity (α = 0.87) with average inter-item correlations of 0.23. Internal consistency between the DS-R subscales is acceptable; with Core Disgust (α = 0.80, inter-item correlation = 0.23), Animal Reminder Disgust (α = 0.82, inter-item correlation = 0.34), and Contamination-Based Disgust (α = 0.71, inter-item correlation = 0.31). The DS-R also demonstrates good convergent and discriminant validity, with results suggesting that the three DS-R subscales are correlated, but not redundant [70]. Within the current sample, the DS-R demonstrated good overall internal consistency (α = 0.79), in addition to moderate internal consistencies in its Core Disgust (α = 0.51), Animal Reminder Disgust (α = 0.67), and Contamination-Based Disgust (α = 0.61) subscales.
Eating disorder examination questionnaire (EDE-Q) [71]
The Eating Disorder Examination Questionnaire is a self-report version of the Eating Disorder Examination (EDE), and was designed to measure the attitudinal and behavioural features of patients with EDs. Primarily used for diagnostic purposes, subjects are required to report how frequently they engage in a certain pathological eating behaviour based on a 7-point scale from 0 (no days) to 6 (every day) within the past 28 days. The EDE-Q examines eating pathology across four subscales include Restraint, Eating Concern, Shape Concern and Weight Concern. A Global score is also calculated as a mean across all four subscales. The EDE-Q has good concurrent validity, and acceptable criterion validity, with correlations between EDE-Q and EDE subscales ranging between 0.68 and 0.78 [72]. Test–retest reliability ranged from 0.66 to 0.94 for scores on the four subscales, and from 0.51 to 0.92 for items addressing the frequency of behavioural engagement. The EDE-Q demonstrates acceptable internal consistency, with alpha’s ranging from 0.70 to 0.93 [73]. Internal consistency for the EDE-Q in the current sample was high, with an alpha of 0.92.
Beck anxiety inventory (BAI) [74]
The Beck Anxiety Inventory (BAI) is a widely used 21-item self-report measure of anxiety severity in adolescents and adults. Items are scored in a Likert scale fashion ranging from 0 (not at all) to 3 (severely, I could barely stand it). The BAI shows high internal consistency (α = 0.92) and test–retest reliability over one week [r(81) = 0.75] [74]. The BAI also shows good concurrent and discriminant validity. In the current sample, the BAI demonstrated a high internal consistency with an alpha of 0.95.
Body mass index (BMI)
BMI was calculated based on participants self-reported height (in metres) and weight (in kg) using the standard formula (BMI = kg/m2 where kg is a participant’s weight in kilograms, and m2 is the participants height in metres squared). Participants BMIs ranged from underweight to obese (M[SD] = 33.98 [11.42]; range = 16.2–69.1), with 2.8% of participants having a BMI in the underweight range (BMI < 18.5), 18.3% in the normal weight range (BMI = 18.5–24.99), 19.7% of participants in the overweight range (BMI = 25.0–29.99), and 56.3% in the obese range (BMI > 30.0) (missing data N = 2). Height was recorded in centimeters using a stadiometer located in a dietitian’s office, and weight was recorded using a yearly calibrated digital bariatric scale.
Go/No-Go task
The Go/No-Go task is cognitive task aimed at determining the ability of an individual to inhibit a prepotent response. The experimental paradigm requires participants to make responses when they see a ‘Go’ signal, and withhold a response when they see a ‘No-Go’ signal. The main dependent variable in the Go/No-Go task are commission errors (making a ‘Go’ response on ‘No-Go’ trials); fewer errors signify better response inhibition [75].
Statistical analysis
Data were screened for outliers and normality. A one-way ANOVA was conducted with the EDE-Q and its subscales (DV: EDE-Q Total Score, Restraint subscale, Eating Concern subscale, Shape Concern subscale and Weight Concern subscale; IV: participant group) to test group differences in eating pathology. To test for group differences in disgust sensitivity and behavioural inhibition, we conducted two separate one-way ANCOVAs, while controlling for anxiety. The first ANCOVA tested group differences on the Disgust Sensitivity Total Scores; the second ANCOVA tested for group differences on Commission Errors, the primary dependent variable of the Go/No-Go task. Next, we conducted two exploratory MANOVAs with each of the DS-R subscales as well as Go/No-Go parameters between our samples (MANOVA 1 DVs: Core Disgust score, Animal Reminder score, Contamination-Based score; MANOVA 2 DVs: Omission Errors, Trial Reaction Times and ‘Go’ Reaction Time; IV: participant group). Given the high prevalence of anxiety-related symptoms in BED [76], the current study controlled for anxiety symptomatology with the BAI. Although the primary aim of our study was to test the relationship between eating pathology and associations with behavioural and emotional measures of inhibition, we explored each subscale that may be driving effects in instances where significant differences emerged. To assess whether eating pathology is associated with behavioural and/or emotional inhibition in our BED sample, Pearson Correlations were conducted between the EDE-Q subscales and total score, the DS-R subscales and total scores and each parameter of the Go/No-Go task. To adjust for anxiety, Partial Correlations were run using the same measures as our Pearson Correlations, but controlling for BAI scores. Lastly, to test whether BMI was associated with cognitive and/or behavioural inhibition, correlational analyses were conducted between BMI, DS-R and parameters from the Go/No-Go task first within, then between groups. A mediation model was also tested using Model 4 in Hayes’ PROCESS macro for SPSS [77]. The significance of the indirect effect of disgust sensitivity on BMI through inhibitory control was evaluated using the 95% confidence intervals calculated from 5000 bootstrapped samples. Four models tested the following: (1) the indirect effect of Disgust Sensitivity total score on BMI via number of Commission Errors, (2) the indirect effect of Core Disgust on BMI via number of Commission Errors, (3) the indirect effect of Animal Reminder on BMI via number of Commission Errors, and (4) the indirect effect of Contamination-Based Disgust on BMI via number of Commission Errors. Analyses were conducted using IBM SPSS 26.0 (IBM Corp. Armonk, NY).
Results
Demographics and descriptive statistics
Table 1 presents the demographic characteristics of our sample, followed by mean scores on the EDE-Q between our participant groups. As expected, the BED group had a significantly higher BMI compared to our control group and differed in ED pathology, with significantly higher EDE-Q total scores compared to controls. Our sample with BED scored significantly higher on Eating Concern, Shape Concern and Weight Concern compared to our healthy control group, but not on the Restraint subscale.
Disgust sensitivity
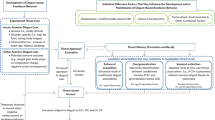
No significant group difference emerged following our one-way ANCOVA, controlling for anxiety, between healthy controls (M = 49.84, SD = 11.26) and participants with BED (M = 52, SD = 15.84) on mean Disgust Sensitivity Total Scores [f(58) = 0.225, p > 0.05] (Fig. 1). An additional exploratory MANCOVA revealed no significant differences on the Core Disgust subscale [f(58) = 0.595, p > 0.05], on the Animal Reminder Disgust subscale [f(58) = 0.001, p > 0.05], nor the Contamination-Based Disgust subscale [f(58) = 0.047, p > 0.05].
Mean scores on the revised Disgust Sensitivity Questionnaire by participant group. Mean scores are shown for Disgust Sensitivity Total Score, Core Disgust Subscale, Animal Reminder Subscale and Contamination-Based Subscales of the DS-R for binge eating disorder (BED, n = 29) and healthy control (HC, n = 32) participants
Behavioural inhibition
No significant group difference on commission errors emerged following our one-way ANCOVA between healthy controls (M = 3.78, SD = 2.51) and participants with BED (M = 4.03, SD = 2.64) on the Go/No-Go [f(58) = 0.673, p > 0.05] after controlling for anxiety. An additional exploratory MANCOVA of secondary Go/No-Go measures revealed no significant differences on the mean omission errors [f(58) = 0.421, p > 0.05], on Trial reaction time [f(58) = 1.117, p > 0.05], nor ‘Go’ mean reaction times [f(58) = 0.480, p > 0.05].
Associations between disgust sensitivity and behavioural inhibition
Within our BED participants, a negative association between Disgust total score and Commission Errors was trending significance in our BED sample (r = − 0.365, p = 0.052), suggesting that BED with higher disgust sensitivity are better at making accurate responses on the Go/No-Go task. Further examinations into the different Disgust subscales demonstrated that Contamination-Based Disgust Subscale scores significantly negatively correlated with Commission Errors on the Go/No-Go Task (r = − 0.435, p = 0.018), suggesting that BED with higher Contamination-Based disgust sensitivity have better response inhibition (Fig. 2). No significant correlations emerged in our sample of healthy controls, nor after collapsing groups together. Results remained the same after removing male subjects from our analyses.
Associations between disgust sensitivity, behavioural inhibition and eating pathology
Pearson correlation tests showed no significant associations between EDE-Q Total Scores and measures of disgust sensitivity, or behavioural inhibition within our BED participants (Table 2). Exploring the EDE-Q subscales showed a positive correlation between the Restraint subscale and the ‘Go’ Mean Reaction Time of the Go/No-Go task (r = 0. 386, p < 0.05; Table 2), suggesting participants with higher restraint took longer to make behavioural responses on ‘Go’ trials. After controlling for anxiety, this correlation remained significant. Restraint and ‘Trial’ Reaction Time (r = 0.38, p < 0.05) also became significantly positively associated suggesting that participants with higher restraint took longer to make behavioural responses on every trial (‘Go’ and ‘No-Go’ trial; Table 3). Shape Concern and Core Disgust (r = 0.394, p < 0.05; Table 3) additionally became significantly positively correlated after controlling for anxiety, suggesting that BED participants with greater shape concerns experience greater sensitivity to disgust based on the offensiveness and the threat of disease (e.g. arising from rotten foods and waste products). In our sample of healthy controls, EDE-Q total score significantly correlated with Disgust Total Score (r = − 0.35, p < 0.05), further subscale exploration showed that the Restraint subscale of the EDE-Q significantly correlated with Disgust Total Score (r = − 0.436, p < 0.05) and Contamination-Based Disgust (r = − 0.478, p < 0.05). Results remained the same after removing male subjects from our analyses.
Associations between disgust sensitivity, behavioural inhibition and BMI
Within the HC group, Pearson correlation coefficients showed no significant associations between BMI, disgust sensitivity or its subscales, or Go/No-Go parameters. Similarly, no significant associations emerged between BMI, disgust sensitivity and Go/No-Go parameters in our participants with BED. Results from our mediation models show that inhibitory control does not mediate any relationships between disgust sensitivity and BMI (Table 4).
Discussion
The aim of this study was to characterize general disgust sensitivity in a clinical BED population. We found no group differences in self-reported disgust sensitivity levels between individuals with BED and healthy controls. Nevertheless, within the BED group, higher disgust sensitivity related to greater behavioural inhibition, driven by contamination-based disgust levels with commission errors. Further exploration of the behavioural data showed positive associations between Go/No-Go reaction times and Restraint levels on the EDE-Q. No associations were found between disgust sensitivity and eating pathology in our sample of BED participants. Lastly, a mediation model did not find that inhibitory control, as measured via commission errors on the Go/No-Go task, mediated any relationships between disgust sensitivity and BMI among participants with clinical BED.
Our results suggest that individuals with BED do not differ from healthy controls in overall levels of disgust sensitivity. Further analyses of disgust subscales revealed similar levels of on all three disgust domains (Core Disgust, Animal Reminder Disgust, and Contamination-Based Disgust) as our healthy participants. While previous relationships between disgust sensitivity and EDs have been examined (in AN, [28, 32]; in BN, [32, 68]; in restrictive eating and obesity [34]; and in ARFID [78]), our study is the first to investigate disgust sensitivity in a clinical sample of BED patients. This study also replicates and extends findings from Schienle and colleagues [36] who found similar disgust sensitivity levels to healthy individuals in a community sample of individuals with BED. Our results are, therefore, consistent with previous findings of disgust sensitivity in other EDs, in both clinical and nonclinical samples. Moreover, these findings support the idea that most EDs are not characterized by a disgust over- or under-sensitivity. If disgust sensitivity reflected affective process associated with psychosocial aspects of eating behaviour or body image, we would have expected to see greater eating pathology associated with heightened disgust sensitivity in our BED sample; our null results suggest that neither diagnosis nor severity of symptoms in BED patients (eating or body image) are related to disgust stimuli that are not specific to ED concerns. Future studies examining more food- and shape-specific disgust may shed light on particular aspects of disgust more directly related to ED pathology, and allow examination of possible links with dysregulated eating behaviours.
We also support our second hypothesis that disgust sensitivity is negatively correlated with general inhibitory control by demonstrating a negative trending association between Total Disgust, particularly driven by Contamination-Based Disgust Subscale scores and Commission Errors on the Go/No-Go Task in our sample of BED patients. These results extend previous reports in undergraduate students and non-obese individuals using food-related stimuli demonstrating an inverse relationship between disgust sensitivity and behavioural inhibition [26, 55] suggesting that general, non-food-related disgust sensitivity may have the ability to indirectly influence eating behaviours via its effects on self-control processes. Taking a closer look at associations between behavioural inhibition and eating pathology, our results suggest that BED participants with higher EDE-Q Restraint scores also took significantly longer to make ‘Go’ and ‘No-Go’ responses suggesting a possible high-order conscientious influence on self-control processes. Interestingly, no associations were observed between disgust sensitivity and measures of eating pathology among BED participants. Other studies assessing the effects of negative affect on cognitive functioning in binge eating disorders have also demonstrated that in individuals with binge-type eating disorders (namely, BED and BN) have greater impairments in decision-making abilities following negative affect compared to healthy controls [79, 80]. Disgust is unique in this study as it is a negative emotion that also incorporate elements of arousal considering its close ties with anxiety-related disorder, and our results may support theories of binging as a way to escape/avoid negative emotions. Nonetheless, understanding the interaction of emotional and cognitive processes is important to better understand the development and maintenance of binge eating disorder, and foster the development of improved clinical interventions. Future research examining disgust stimuli that is more relevant to BED (i.e., larger body image, more decadent and palatable foods) may shed light onto stronger relationships between disgust sensitivity, eating pathology, and impulse control.
In contrast to our hypothesis and previous research in non-BED groups, our results suggest that higher BMI is not associated with disgust sensitivity levels in BED. Despite Houben and Havermans [34] proposing lower disgust sensitivity encouraging overeating behaviours, the lack of association between high BMI and disgust sensitivity is consistent with the idea that disgust may be more closely linked to affective processes. Our findings nevertheless suggest a relationship between disgust sensitivity and eating attitudes; in particular a role for the severity of body image concerns in BED, a factor known to be associated with greater distress and poor treatment outcomes in BED [81]. Research in a nonclinical population showed that the desire to binge is greater when experiencing higher levels of body dissatisfaction/distress [82]. These findings highlight the cognitive-affective link with emotion regulation whereby different disgust-related eating features may have a unique maintenance function on eating attitudes, including the severity of shape and weight concerns. In contrast to previous studies [26, 55], we found no mediating role of behavioural inhibition when further examining associations between disgust sensitivity and BMI, suggesting differentials roles between cognitive and behavioural inhibition across EDs. Indeed, whereas Spinelli and colleagues [26] found no associations between disgust sensitivity, restrained eating and BMI in individuals with obesity, they did find associations between higher levels of disgust sensitivity and higher BMI in their sample of non-obese individuals, which appeared to be fully mediated by restrained eating behaviours [26, 55]. While BMI may be a marker for more dysregulated eating and/or less restriction, our sample is mostly obese and dysregulated in their eating, and as such we may be looking at a limited restricted range. Relationship between BMI, disgust and impulse control may only arise in a broader non-obese samples.
Strengths and limitations
This is the first study to assess disgust sensitivity in a clinical sample of individuals with BED. We extended findings of disgust sensitivity patterns previously reported in AN and BN to BED, while controlling for baseline anxiety. Specifically, we replicated associations between disgust sensitivity (related to contamination-based disgust), and behavioural inhibition. The current study did not find a relationship between BMI and disgust sensitivity, nor did it find a mediating role of behavioural inhibition. Additionally, despite using different measures of disgust sensitivity and eating pathology (namely the revised Disgust Scale and the EDE-Q), we found similarities in our results with previous ED research, therefore extending the validity between measures to the reproducibility of consistent results. This study is also unique in examining general traits and processes (i.e., generalized disgust and inhibitory control), rather than food or disorder-specific stimuli.
Our findings should be considered in light of some limitations. First, although double the size of the first study examining disgust sensitivity in a community BED sample [36], our sample size is still relatively small and powered to only detect medium to large effect size relationships; nevertheless, we have replicated and extended previous findings from other ED studies to a clinical BED sample. Second, the individual DS-R subscales show lower internal consistency, which may be due to the sample size or type (i.e., clinical) or from different versions of the measure. Future revisions of these subscale seems warranted. Third, although sex differences in disgust sensitivity are evident [83], these could not be addressed as our sample had a higher representation of females compared to males (with only 4 males included altogether). This is important to highlight as cognitive-affect processes may also differ between sexes and could be examined with a larger and more diverse sample. Future research could assess disgust sensitivity in a community sample of males with dysregulated eating behaviours as a preliminary way to assess sex differences in a large sample, as males are often underrepresented in eating disorder treatment settings. Furthermore, our cross-sectional study makes it difficult to assess temporal interrelationships between disgust sensitivity and eating pathology. Although disgust sensitivity is often conceptualized as a trait, state-dependent testing will also be important for future research to assess affective processes, including craving, loss of control eating and body image triggers, linked to immediate states. Lastly, given the characteristics of our sample, matching healthy control participants to BED patients on BMI was not possible. As such, differences in body muscle/fat compositions exist between individuals within each group, which may relate to other between-group differences and our underlying constructs of interest. Our sample sex-ratio is also a limitation; our study was also conducted only with females, and differences may emerge with males in our sample or an all-male study.
Future directions
Future research should consider replicating these findings in larger clinical samples and further differentiating between food and non-food items using a food-specific disgust measure, as disgust sources may have an effect on the development and maintenance of eating disorders. Additionally, future studies could assess the extent of food-related disgust in the context of different levels of body image distress/dissatisfaction, or after an experience of loss of control over eating. Future studies should also consider further differentiating between moral aspects of disgust. For example, examining self-disgust and behavioural disgust, as feelings of disgust towards the self is a DSM-5 characteristic required for a BED diagnosis [84], and appears elevated in individuals with binging behaviours (ex; BN) [85]. Furthermore, a study in an undergraduate population suggests that negative body image relates to higher self-disgust scores, heightened disgust propensity and disgust sensitivity, and that people who experience disgust more readily are more likely to experience disgust directed towards themselves [86]. Importantly, von Spreckelsen and colleagues [86] found that only disgust sensitivity (as opposed to self-disgust or disgust propensity) appeared independently related to a negative body image—further substantiating a link between these two constructs. However, associations stemming from this approach may be context dependent; if you’ve violated your eating rules versus general self-disgust. Additionally, examining food-related inhibitory control, for example through an affective Go/No-Go task, can also test whether stronger associations exist with disgust. Further replication and extension of these results with greater sample sizes in clinical disordered eating populations will be valuable, particularly as they relate to persistent body dissatisfaction and changes over treatment.
Conclusion
This study is the first to preliminarily assess disgust sensitivity in a clinical BED sample and examine subsequent associations with behavioural inhibition. Findings from our study support relationships between disgust sensitivity and inhibitory control, and further suggest potential cognitive-affective linkages formed in maintaining BED pathology. We replicated associations between disgust sensitivity and eating pathology reported in other EDs—specifically on similarities in overall disgust sensitivity between BED patients and healthy controls. Examining disgust sensitivity in BED can shed light on how affective processing and inhibitory control systems might maintain dysregulated eating behaviours.
What is already known on this subject?
Disgust is a universally experienced emotion that has strong ties with consummatory behaviour. Evidence suggests that relationships exist between anorexia nervosa and bulimia nervosa and disgust related to food and body-related stimuli, as well as between restraint/drive for thinness and disgust sensitivity (particularly to food stimuli). For binge eating disorder, there is currently no evidence for differences between clinical and non-clinical BED groups in general or food/body-related disgust sensitivity, nor a clear understanding of how self-regulatory processes and affective processes influence binge eating behaviours.
What does this study add?
To the best of our knowledge, this is the first study to characterize general disgust sensitivity in a clinical binge eating disorder population. We add to the existing disgust in eating disorders literature by demonstrating that general disgust sensitivity does not differ between BED patients and healthy individuals, and that behavioural inhibition relates to disgust sensitivity but does not mediate relationships between disgust sensitivity and BMI in patients with BED.
References
Rozin P, Fallon AE (1987) A perspective on disgust. Psychol Rev 94(1):23–41. https://doi.org/10.1037/0033-295X.94.1.23
Curtis V, Aunger R, Rabie T (2004) Evidence that disgust evolved to protect from risk of disease. Proc Biol Sci 271(Suppl 4):S131–S133. https://doi.org/10.1098/rsbl.2003.0144
Egolf A, Siegrist M, Hartmann C (2018) How people’s food disgust sensitivity shapes their eating and food behaviour. Appetite 127:28–36. https://doi.org/10.1016/j.appet.2018.04.014
Levenson RW, Ekman P, Friesen WV (1990) Voluntary facial action generates emotion-specific autonomic nervous system activity. Psychophysiology 27:363–384. https://doi.org/10.1111/j.1469-8986.1990.tb02330.x
Levenson RW (1992) Autonomic nervous system differences among emotions. Psychol Sci 3(1):23–27. https://doi.org/10.1111/j.1467-9280.1992.tb00251.x
van Overveld WJM, De Jong PJ, Peters ML, Cavanagh K, Davey GCL (2006) Disgust propensity and disgust sensitivity: separate constructs that are differentially related to specific fears. Personal Individ Differ 41(7):1241–1252. https://doi.org/10.1016/j.paid.2006.04.021
Muris P, Merckelback H, Schmidt H, Tierney S (1999) Disgust sensitivity, trait anxiety and anxiety disorders symptoms in normal children. Behav Res Ther 37(10):953–961. https://doi.org/10.1016/s0005-7967(99)00045-5
Thorpe SJ, Patel SP, Simonds LM (2003) The relationship between disgust sensitivity, anxiety and obsessions. Behav Res Ther 41(12):1397–1409. https://doi.org/10.1016/s0005-7967(03)00058-5
Tolin DF, Lohr JM, Sawchuk CN, Lee TC (1997) Disgust and disgust sensitivity in blood-injection-injury and spider phobia. Behav Res Ther 35(10):949–953. https://doi.org/10.1016/s0005-7967(97)00048-x
Koch MD, O’Neill HK, Sawchuk CN, Connolly K (2002) Domain-specific and generalized disgust sensitivity in blood-injection-injury phobia: the application of behavioural approach/avoidance tasks. J Anxiety Disord 16(5):511–527. https://doi.org/10.1016/s0887-6185(02)00170-6
Sawchuk CN, Lohr JM, Westendorf DH, Meunier SA, Tolin DF (2002) Emotional responding to fearful and disgusting stimuli in specific phobics. Behav Res Ther 40(9):1031–1046. https://doi.org/10.1016/s0005-7967(01)00093-6
Sawchuk CN, Lohr JM, Tolin DF, Lee TC, Kleinknecht RA (2000) Disgust sensitivity and contamination fears in spider and blood-injection-injury phobias. Behav Res Ther 28(8):753–762. https://doi.org/10.1016/s0005-7967(99)00093-5
De Jong PJ, Andrea H, Muris P (1997) Spider phobia in children: disgust and fear before and after treatment. Behav Res Ther 35(6):559–562. https://doi.org/10.1016/s0005-7967(97)00002-8
Mulken SA, De Jong PJ, Merckelbach H (1996) Disgust and spider phobia. J Abnorm Psychol 105(3):464–468. https://doi.org/10.1037/0021-843x.105.3.464
De Jong PJ, Peters M, Vanderhallen I (2002) Disgust and disgust sensitivity in spider phobia: facial EMG in response to spider and oral disgust imagery. J Anxiety Disord 16(5):477–493. https://doi.org/10.1016/s0887-6185(02)00167-6
Davey GCL (1994) Self-reported fears to common indigenous animals in an adult UK population: the role of disgust sensitivity. Br J Psychol 85(pt. 4):541–545. https://doi.org/10.1111/j.2044-8295.1994.tb02540.x
Ware J, Jain K, Burgess I, Davey GCL (1994) Disease-avoidance model: factor analysis of common animal fears. Behav Res Ther 32(1):57–63. https://doi.org/10.1016/0005-7967(94)90084-1
Matchett G, Davey GCL (1991) A test of a disease-avoidance model of animal phobias. Behav Res Ther 29(1):91–94. https://doi.org/10.1016/s0005-7967(09)80011-9
Woody SR, Tolin DF (2002) The relationship between disgust sensitivity and avoidant behaviour: studies of clinical and nonclinical sample. J Anxiety Disord 16(5):543–559. https://doi.org/10.1016/s0887-6185(02)00173-1
Berle D, Phillips ES (2006) Disgust and obsessive-compulsive disorder: an update. Psychiatry 69(3):228–238. https://doi.org/10.1521/psyc.2006.696.3.228
Olatunji BO, Lohr JM, Sawchuk CN, Tolin DF (2007) Multimodal assessment of disgust in contamination-related obsessive-compulsive disorder. Behav Res Ther 45(2):263–276. https://doi.org/10.1016/j.brat.2006.03.004
Amir N, Najmi S, Bomyea J, Burns M (2010) Disgust and anger in social anxiety. Int J Cogn Ther. https://doi.org/10.1521/ijct.2010.3.1.3
Montagne B, Schutters S, Westenberg HGM, van Honk J, Kessels RPC, de Haan EHF (2006) Reduced sensitivity in the recognition of anger and disgust in social anxiety disorder. Cogn Neuropsychiatry 11(4):389–401. https://doi.org/10.1080/13546800444000254
Bektas S, Keeler JL, Anderson LM, Mutwalli H, Himmerich H, Treasure J (2022) Disgust and self-disgust in eating disorders: a systematic review and meta-analysis. Nutrients 14:1728. https://doi.org/10.3390/nu14091728
Santomauro DF, Melen S, Mitchison D, Vos T, Whiteford H, Ferrari AJ (2021) The Hidden burden of eating disorders: an extension of estimates from the global burden of disease study 2019. Lancet Psychiatry 8(4):320–328. https://doi.org/10.1016/S2215-0366(21)00040-7
Spinelli S, Cunningham C, Pierguidi L, Dinnella C, Monteleone E, White TL (2021) The relationship between disgust sensitivity and BMI: is the food disgusting or am I? Food Qual Prefer 92:104222. https://doi.org/10.1016/j.foodqual.2021.104222
Haidt J, McCauley C, Rozin P (1994) Individual differences in sensitivity to disgust: a scale sampling seven domains of disgust elicitors. Personal Individ Differ 16:701–713
Aharoni R, Hertz MM (2011) Disgust sensitivity and anorexia nervosa. Eur Eat Disord Rev. https://doi.org/10.1002/erv.1124
Davey GCL, Buckland G, Tantow B, Dallos R (1998) Disgust and eating disorders. Eur Eat Disord Rev 6:201–211
Troop NA, Treasure JL, Serpell L (2002) A further exploration of disgust in eating disorders. Eur Eat Disord Rev 10:218–226. https://doi.org/10.1002/erv.444
Troop NA, Murphy F, Bramon E, Treasure JL (2000) Disgust sensitivity in eating disorders: a preliminary investigation. Int J Eat Disord 27(4):446–451. https://doi.org/10.1002/(SICI)1098-108X(200005)27:4%3c446::AID-EAT9%3e3.0.CO;2-W
Troop N, Baker A (2009) Food, body, and soul: The role of disgust in eating disorders. In: Olatunji BO, McKay D (eds) Disgust and its disorders: theory, assessment, and treatment implications. American Psychological Association, Washington, DC, US, pp 229–251. https://doi.org/10.1037/11856-011
Lobera IJ, Rio PB (2011) Disgust sensitivity and eating behaviour. Revista Espanola de Nutriion Humana y dietetica 15(1):4–9. https://doi.org/10.1016/S2173-1292(11)70002-3
Houben K, Havermans RC (2012) A delivious fly in the soup. The relationship between disgust, obesity, and restraint. Appetite 58(3):827–830. https://doi.org/10.1016/j.appet.2012.01.018
Griffiths J, Troop NA (2006) Disgust and fear ratings of eating disorder-relevant stimuli: associations with dieting concerns and fat intake. Anxiety Stress Coping 19(4):421–433. https://doi.org/10.1080/10615800601066771
Schienle A, Schäfer A, Hermann A, Vaitl D (2009) Binge-eating disorder: reward sensitivity and brain activation to images of food. Biol Psychiat 65(8):654–661. https://doi.org/10.1016/j.biopsych.2008.09.028
Gross JJ, Jazaieri H (2014) Emotion, emotion regulation, and psychopathology: an affective science perspective. Clin Psychol Sci 2(4):387–401. https://doi.org/10.1177/2167702614536164
Litwin R, Goldbacher EM, Cardaciotto L, Gambrel LE (2017) Negative emotions and emotional eating: the mediating role of experiential avoidance. Eat Weight Disord 22(1):97–104
Dreyfuss MFW, Riegel ML, Pedersen GA, Cohen AO, Silverman MR, Dyke ML et al (2017) Patients with bulimia nervosa do not show typical neurodevelopment of cognitive control under emotional influences. Psychiatry Res Neuroimaging 266:59–65. https://doi.org/10.1016/j.pscychresns.2017.05.001
Anestis MD, Smith AR, Fink EL, Joiner TE (2009) Dysregulated eating and distress: examining the specific role of negative urgency in a clinical sample. Cogn Ther Res 33:390–397. https://doi.org/10.1007/s10608-008-9201-2
Hayaki J (2009) Negative reinforcement eating expectancies, emotion dysregulation, and symptoms of bulimia nervosa. Int J Eat Disord 42:552–556. https://doi.org/10.1002/eat.20646
Fischer S, Settles R, Collins B, Gunn R, Smith GT (2012) The role of negative ur- gency and expectancies in problem drinking and disordered eating: testing a model of comorbidity in pathological and at-risk samples. Psychol Addict Behav 26:112–123. https://doi.org/10.1037/a0023460
Vannucci A, Nelson EE, Bongiorno DM, Pine DS, Yanovski JA, Tanofsky-Kraff M (2015) Behavioral and neurodevelopmental precursors to binge-type eating disorders: support for the role of negative valence systems. Psychol Med 45(14):2921–2936. https://doi.org/10.1017/S003329171500104X
Manasse SM, Forman EM, Ruocco AC, Butryn ML, Juarascio AS, Fitzpatrick KK (2015) Do executive functioning deficits underpin binge eating disorder? A comparison of overweight women with and without binge eating pathology. Int J Eat Disord 48(6):677–683
Miller EK, Cohen JD (2001) An integrative theory of prefrontal cortex function. Ann Rev Neurosci 24:167–202. https://doi.org/10.1146/annurev.neuro.24.1.167
Tiego J, Testa R, Bellgrove MA, Pantelis C, Whittle S (2018) A hierarchical model of inhibitory control. Front Psychol 9:1339. https://doi.org/10.3389/fpsyg.2018.01339
Kalanthroff E, Cohen N, Henik A (2013) Stop feeling: inhibition of emotional interference following stop-signal trials. Front Hum Neurosci 7:78. https://doi.org/10.3389/fnhum.2013.00078
Steward T, Berner LA (2020) The neurobiological basis of executive function alterations in binge eating populations. In: Frank G, Berner L (eds) Binge eating. Springer, Cham. https://doi.org/10.1007/978-3-030-43562-2_10
Flynn FG, Benson DF, Ardila A (1999) Anatomy of the insula – functional and clinical correlates. Aphasiology 13:55–78. https://doi.org/10.1080/026870399402325
Droutman V, Read SJ, Bechara A (2015) Revisiting the role of the insula in addiction. Trends Cogn Sci 19:414–420. https://doi.org/10.1016/j.tics.2015.05.005
Naqvi NH, Rudrauf D, Damasio H, Bechara A (2007) Damage to the insula disrupts addiction to cigarette smoking. Science 315:531–534. https://doi.org/10.1126/science.1135926
Craig AD (2009) How do you feel - now? The anterior insula and human awareness. Nat Rev Neurosci 10:59–70. https://doi.org/10.1038/nrn2555
Naqvi NH, Bechara A (2009) The hidden island of addiction: the insula. Trends Neurosci 32:56–67. https://doi.org/10.1016/j.tins.2008.09.009
Naqvi NH, Bechara A (2010) The insula and drug addiction: an interoceptive view of pleasure, urges, and decision-making. Brain Struct Funct 214:435–450. https://doi.org/10.1007/s00429-010-0268-7
Liu X, Li J, Turel O, Chen R, He Q (2019) Food-specific inhibitory control mediates the effect of disgust sensitivity on body mass index. Front Psychol 10:2391. https://doi.org/10.3389/fpsyg.2019.02391
Wu M, Hartmann M, Skunde M, Herzog W, Friederich H-C (2013) Inhibitory control in bulimic-type eating disorders: a systematic review and meta-analysis. PLOS One 8(12):e83412. https://doi.org/10.1371/journal.pone.0083412
Mobbs O, Iglesias K, Golay A, Van der Linden M (2011) Cognitive deficits in obese persons with and without binge eating disorder. Investigation using a mental flexibility task. Appetite 57(1):263–271. https://doi.org/10.1016/j.appet.2011.04.023
Schag K, Schönleber J, Teufel M, Zipfel S, Giel KE (2013) Food-related impulsivity in obesity and binge eating disorder – a systematic review. Obes Rev 14(6):477–495. https://doi.org/10.1111/obr.12017
Córdova ME, Schiavon CC, Busnello FM, Reppold CT (2017) Nutritional and neuropsychological profile of the executive functions on binge eating disorder in obese adults. Nutr Hosp 34:1448–1454. https://doi.org/10.20960/nh.1151
Kollei I, Rustemeier M, Schroeder S, Jongen S, Herpertz S, Loeber S (2018) Cognitive control functions in individuals with obesity with and without binge-eating disorder. Int J Eat Disord 51(3):233–240
Hege MA, Stingl KT, Kullmann S, Schag K, Giel KE, Zipfel S, Preissl H (2015) Attentional impulsivity in binge eating disorder modulates response inhibition performance and frontal brain networks. Int J Obes (2005) 39(2):353–360. https://doi.org/10.1038/ijo.2014.99
Ames SL, Kisbu-Sakarya Y, Reynolds KD, Boyle S, Cappelli C, Cox MG, Dust M, Grenard JL, Mackinnon DP, Stacy AW (2014) Inhibitory control effects in adolescent binge eating and consumption of sugar-sweetened beverages and snacks. Appetite 81:180–192. https://doi.org/10.1016/j.appet.2014.06.013
Strack F, Deutsch R (2004) Reflective and impulsive determinants of social behavior. Pers Soc Psychol Rev 8(3):220–247. https://doi.org/10.1207/s15327957pspr0803_1
Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, de Graaf R, Maria Haro J, Kovess-Masfety V, O’Neill S, Posada-Villa J, Sasu C, Scott K, Viana MC, Xavier M (2013) The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry 73(9):904–914. https://doi.org/10.1016/j.biopsych.2012.11.020
Schienle A, Stark R, Schafer A, Walter B, Kirsch P, Vaitl D (2004) Disgust and disgust sensitivity in bulimia nervosa: an fMRI study. Eur Eat Disord Rev 12(1):42–50. https://doi.org/10.1002/erv.562
Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(suppl 20):22–33
Lecrubier Y, Sheehan DV, Weiller E et al (1997) The mini-international neuro- psychiatric interview (M.I.N.I.): a short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry 12:224–231
Sheehan DV, Lecrubier Y, Harnett-Sheehan K et al (1997) The validity of the mini-international neuropsychiatric interview (M.I.N.I.) according to the SCID-P and its reliability. Eur Psychiatry 12:232–241
Olatunji BO, Williams NL, Tolin DF, Abramowitz JS, Sawchuck CN, Lohr JM, Elwood LS (2007) The disgust scale: item analysis, factor structure, and suggestions for refinement. Psychol Assess 19(3):281–297. https://doi.org/10.1037/1040-3590.19.3.281
van Overveld WJM, De Jong PJ, Peters ML, Shouten E (2011) The disgust scale-R: a valid and reliable index to investigating separate disgust domains? Personal Individ Differ 51:325–330. https://doi.org/10.1016/j.paid.2011.03.023
Fairburn CG, Beglin SJ (1994) Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord 16(4):363–370
Mond JM, Hay PJ, Rodgers B, Owen C, Beaumont PJV (2004) Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther 42:551–567. https://doi.org/10.1016/S0005-7967(03)00161-X
Berg KC, Peterson CB, Frazier P, Croz SJ (2012) Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. Int J Eat Disord 45(3):428–438. https://doi.org/10.1002/eat.20931
Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 56(6):893–897
Verbruggen F, Logan GD (2008) Response inhibition in the stop-signal paradigm. Trends Cogn Sci 12(11):418–424. https://doi.org/10.1016/j.tics.2008.07.005
Rosenbaum DL, White KS (2013) The role of anxiety in binge eating behavior: a critical examination of theory and empirical literature. Health Psychol Res 1(2):e19. https://doi.org/10.4081/hpr.2013.e19
Hayes AF. Model templates for PROCESS for SPSS and SAS. 2013. Retrieved from http://www.afhayes.com/public/templates.pdf. Accessed July 2022
Harris AA, Romer AL, Hanna EK, Keeling LA, LaBar KS, Sinnott-Armstrong W, Strauman TJ, Wagner HR, Marcus MD, Zucker NL (2019) The central role of disgust in disorders of food avoidance. Int J Eat Disord 52(2):543–553. https://doi.org/10.1002/eat.23047
Kittle R, Braudhardt A, Hilbert A (2015) Cognitive and emotional functioning in binge eating disorder: a systematic review. Int J Eat Disord 48(6):353–554
Danner UN, Evers C, Sternheim L, van Meer F, van Elburg AA, Geerets TA et al (2012) Influence of negative affect on choice behaviour in individuals with binge eating pathology. Psychiatry Res 207:100–106
Lloyd-Richardson EE, King TK, Forsyth LH, Clark MM (2000) Body image evaluations in obese females with binge eating disorder. Eat Behav 1(2):161–171. https://doi.org/10.1016/S1471-0153(00)00016-7
Andrés A, Saldaña C (2014) Body dissatisfaction and dietary restraint influence binge eating behavior. Nutr Res (New York, N.Y.) 34(11):944–950. https://doi.org/10.1016/j.nutres.2014.09.003
Tybur JM, Bryan AD, Lieberman D, Caldwell Hooper AE, Merriman LA (2011) Sex differences and sex similarities in disgust sensitivity. Personality Individ Differ 51:343–348
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. Author, Washington, DC
Bell K, Coulthard H, Wildbur D (2017) Self-disgust within eating disordered groups: associations with anxiety, disgust sensitivity and sensory processing. Eur Eat Disord Rev 25(5):373–380
von Spreckelsen P, Glashouwer KA, Bennik EC, Wessel I, De Jong PJ (2018) Negative body image: Relationships with heightened disgust propensity, disgust sensitivity, and self-directed disgust. PLOS One 13(6):e0198532. https://doi.org/10.1371/journal.pone.0198532
Funding
This research was supported from the Peter Boris Centre for Addictions Research at McMaster University and from the Constantine Douketis Award at the Research Institute of St. Joe’s Hamilton (IB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical and informed consent
Study procedures were approved by the Hamilton Integrated Research Ethics Board (HiREB, Project 1600). All participants provided informed consent prior to participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brassard, S.L., Laliberte, M., MacKillop, J. et al. Disgust sensitivity and behavioural inhibitory systems in binge eating disorder: associations with eating pathology. Eat Weight Disord 28, 15 (2023). https://doi.org/10.1007/s40519-023-01544-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40519-023-01544-5