Abstract
Background
Emotional eating is defined as a nonpathological eating behavior, whereas binge-eating disorder (BED) is defined as a pathological eating behavior. While different, both share some striking similarities, such as deficits in emotion regulation and inhibition. Previous research has suggested the existence of an “eating continuum” that might reflect the increased severity of overeating behaviors, that is, from nonpathological overeating to BED. The main aims of this scoping review were to explore in the literature the idea of a continuum between emotional eating and BED and to observe whether deficits in emotion regulation and inhibition follow this continuum in terms of severity. The other aims were to hopefully clarify the ill-defined concept of overeating, to question the potential role of positive emotions and to identify potential knowledge gaps.
Method
A systematic scoping review was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines. Two databases (PubMed/Medline and PsycINFO) were examined in complete accordance with the beforehand sharply defined eligibility and exclusion criteria. The main criteria included adults (≥ 18) with emotional eating, BED or overeating and emotion regulation and inhibition as exposure criteria.
Results
Thirty-two studies were included in this scoping review. If the results showed a link between emotional eating and BED, with the presence of inhibition and emotion regulation deficits in both eating behaviors, no mention of a continuum between emotional eating and BED was found.
Conclusion
In the absence of research directly comparing emotional eating and BED in the same studies and testing the potential increase in severity of emotion regulation and inhibition deficits along this continuum, there is currently no certainty that a continuum exists between emotional eating and BED. In the end, the idea of a continuum in terms of increased severity of overeating and in terms of emotion regulation and inhibition deficits between emotional eating and BED appears to be a gap in knowledge in the literature. This scoping review highlights the need for further research to identify knowledge gaps.
Plain English summary
Emotional eating (EE) is defined as a nonpathological eating behavior, whereas binge-eating disorder (BED) is defined as a pathological eating behavior. While different, both share some striking similarities, such as deficits in emotion regulation (ER) and inhibition. Previous research has suggested the existence of an “eating continuum” that might reflect the increased severity of overeating behaviors, that is, from nonpathological overeating to BED. The main aims of this scoping review were to explore in the literature the idea of a continuum between EE and BED and to observe whether deficits in ER and inhibition follow this continuum in terms of severity. A systematic scoping review was conducted, and thirty-two studies were included in this review. If the results showed a link between EE and BED, with the presence of inhibition and ER deficits in both eating behaviors, no mention of a continuum between EE and BED, or in relation to a continuum, was found. Thus, in the absence of research directly comparing EE and BED in the same studies and testing the potential increase in severity of ER and inhibition deficits along this continuum, there is currently no certainty about the existence or absence of such a continuum.
Similar content being viewed by others
Introduction
Our scoping review mainly focused on emotional eating (EE) and binge-eating disorder (BED). EE is an eating behavior that can be defined as “the tendency to overeat in response to negative emotions […]” ([1], p. 106) but in a nonpathological way. It differs from BED, which was formally indexed in 2013 in the DSM-5 as a discrete eating disorder. BED symptoms include recurrent binge-eating episodes (i.e., eating a larger amount of food than most people do during a discrete period of time, with at least one episode per week for three months), “a sense of lack of control over eating during the episode” and “marked distress regarding binge eating”, but without compensatory behaviors as in anorexia nervosa or bulimia nervosa [2].
Although different, both EE and BED appear to be affected by deficits in emotion regulation (ER) and inhibition [3,4,5,6,7,8,9,10]. Indeed, both individuals with EE and BED present with overeating behaviors caused by emotion regulation difficulties and a lack of inhibition/greater impulsivity. For example, it has been shown that negative emotions act as a trigger for binge-eating episodes in BED [7, 11, 12], and some data also suggest that positive emotions may increase food consumption [7]. Binge eating can be seen as a way to regulate negative emotions (but it is yet uncertain if this strategy successfully improves mood, see Leehr et al. and Stein et al. [7, 13]), and BED patients are more prone to use maladaptive strategies such as suppression or rumination [4].
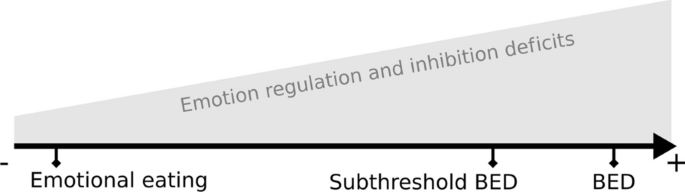
Davis [14] suggested the existence of an “(over) eating continuum”: in some way, on one end of the continuum are nonpathological overeating behaviors and at the other end is BED, which is a pathological and extreme state of overeating. The evolution on this continuum, therefore, reflects the “increased severity and compulsiveness” of overeating behaviors. It is also important to emphasize that this idea of a continuum in severity and compulsiveness between those eating behaviors is also reported by clinicians and physicians. It is therefore reasonable to think that the severity of ER and inhibition deficits could increase along this continuum between EE and BED, as shown in Fig. 1. Taken together, this information is a starting point to lead a systematic screening of the literature. Since our main goals are to clarify the concept of continuum and to identify knowledge gaps, we chose to conduct a scoping review following the guidelines of PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) [15].
The present scoping review aimed (1) to address the possible existence of a continuum between EE and BED; (2) to address the possibility of an increase in the severity of deficits in emotion regulation and inhibition; and (3) to address the ill-defined concept of overeating. Indeed, is overeating (OE) a symptom, an eating behavior, a synonymous concept of EE, or a synonym for binge eating? (4) The final aim was to potentially investigate whether positive emotions can, like negative emotions, trigger emotional eating episodes associated with emotion regulation and/or inhibition difficulties. Finally, this scoping review also aimed to identify gaps in knowledge.
Method
The scoping review was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines [15].
The review protocol can be accessed at HAL (https://hal.science/hal-03643357v1—HAL Id/Registration number: hal-03643357) [16].
Eligibility criteria
Studies were selected based on the following criteria:
The PICOS framework was used to highlight the main criteria. PICOS criteria: Populations: People (adult human subjects ≥ 18) with binge-eating disorder (BED) (and meeting the full DSM-IV-TR or DSM-5 criteria for BED) or subthreshold BED and people (adult human subjects, 18 +) presenting with emotional eating (EE) or emotional overeating (EO). Interventions/Exposures: Our review focused on the impact of “emotion regulation” and “inhibitory control” on BED and EE. Comparisons: Our review did not focus on studies with specific comparisons. Outcomes: Our review considered all types of outcomes related to emotion regulation and inhibitory control in BED, EE, and EO (e.g., deficit, level of attention, response impairment, and degree of compulsivity). Studies: All types of journal articles published in peer-reviewed scientific journals, either written in English or in French. The exclusion criteria were all types of reviews, book chapters, abstracts, preprints, theses, and articles focusing on therapies/treatments.
Only papers published between January 2009 and January 2022 were eligible for consideration. Although the MeSH (Medical Subject Headings) terms for binge-eating disorder were not introduced until 2010, the year 2009 was chosen because it was a “transition year” between the previous indexing of binge-eating disorder as bulimia nervosa and the introduction of the MeSH term BED in 2010.
Information sources and search
Two electronic bibliographic databases, PubMed/Medline and PsycINFO, were searched to identify references related to the scoping review topic. The search focused on articles published between January 2009 and January 2022. The following search equation was used in both databases: ("Binge-Eating Disorder"[Mesh] OR BED OR Binge eater OR Emotional Eating OR Emotional Overeating OR Overeater OR Emotional eater OR Overeating) AND ("Emotional Regulation"[Mesh] OR Emotion regulation OR Reappraisal OR Rumination OR Attentional deployment OR Mood regulation OR "Inhibition, Psychological"[Mesh] OR Inhibitory control).
This database search stage was conducted by one of the authors, M. A. No additional references were added from other sources at this stage.
Selection of sources of evidence
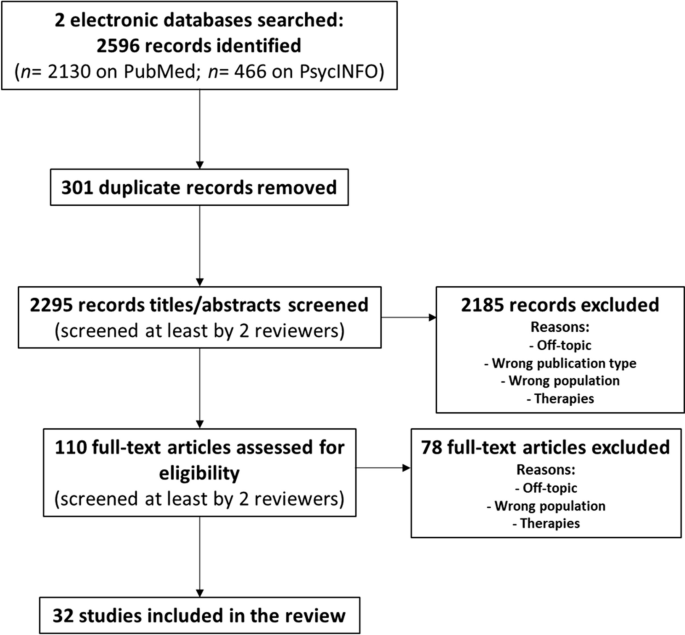
Duplicates were removed, and all references were imported into Rayyan, an online application for systematic reviews [17]. Figure 2 shows the flowchart of the literature search and screening/study selection process. During the successive screening stages, at least 2 authors (M. A., and P.-E. B. or S. C., up to 4 authors, M. A., P.-E. B., S. C. and M.-C. B.) screened each record. Disagreements regarding study selection were resolved by a third or even a fourth investigator, and discussions took place between the authors. In the first screening step, for each article, the inclusion criteria described in Sect. "Eligibility criteria" were applied to both titles and abstracts. In the second screening step (eligibility), for each article, the inclusion criteria described in Sect. "Eligibility criteria" were applied to the entire article (i.e., a complete reading of the article). Note that at this stage, we screened the bibliographic references of the included articles to identify potential new references. At the end of this screening, no new articles were included.
Data charting process and data items
Three investigators (authors M. A., P.-E. B., and S. C.) developed a data charting form to extract the relevant data from each of the 32 included studies. For each study, author M. A. extracted the data according to the following variables of the chart: authors, title, year of publication, country of the study, journal of publication, type of study, method/study design, participants and sample sizes, type of interventions, comparisons, and outcomes/results. Table 1 shows the final version of the chart with the main characteristics of the studies included in the scoping review. We did not include in Table 1 the journal of publication or type of study variables of the chart, as they were deemed irrelevant for this table. Note that we added in Table 1 a new column “Outcomes/Results highlight” with a simplified overview of the results, as well as a “Limitations” column.
Critical analysis
Two authors (M. A. and P.-E. B.) listed the possible limitations of each study. The limitations identified by both authors were retained, and the others were either eliminated or retained after discussion. A third author (S. C.) checked this list, and her comments were considered. The limitations are summarized in the "Limitations" column of Table 1 and are discussed in Sect. "Critical analysis".
Synthesis of results
Data were analyzed qualitatively. We first grouped the studies by the types of eating behaviors (emotional eating (EE), overeating (OE), and binge-eating disorder (BED)). Then, we addressed each of the topics formulated in our questions/hypotheses.
Results
Selection of sources of evidence
The source search in the electronic bibliographic databases retrieved 2596 records (2130 on PubMed/Medline and 466 on PsycINFO) (see Fig. 2). After removing 301 duplicate records, 2295 records were screened in the first screening step. During this first screening step, for each of the 2295 articles, the inclusion criteria described in the Eligibility criteria section of the Methods section were applied to both titles and abstracts, resulting in 110 records to be assessed for eligibility in the next step. Thus, in the second screening step (eligibility), for each of the 110 articles, the same inclusion criteria were applied to the entire article (i.e., a complete reading of the article). At the end of this second stage, 32 studies were selected to be included in the review. Table 1 shows the main characteristics of the 32 studies included in the scoping review, according to the variables described in Sect. "Data charting process and data items".
Regarding the types of populations (cf. PICOS criteria), 9 studies out of 32 focused on emotional eating (EE), 21 studies out of 32 focused on binge-eating disorder (BED), and 2 out of 32 focused on overeating (OE). Regarding the types of intervention/exposure (cf. PICOS criteria), namely, ER and inhibition/impulsivity, 19 studies out of 32 focused on emotion regulation (ER), 18 studies out of 32 focused on inhibition/impulsivity, and 5 out of 32 focused on both ER and inhibition/impulsivity. More than a third of the included studies (11 studies out of 32, ≈ 34%) were conducted in Germany. Moreover, more than half of the studies (17 studies out of 32, ≈ 53%) were conducted in Germany or in countries bordering Germany (i.e., France, Switzerland, Belgium and Poland).
Summary of findings
Emotional eating and emotion regulation
Studies confirm the existence of a link between ER and EE, including the fact that ER difficulties predict EE. For example, Stapleton and Whitehead [18] highlighted that “Emotion regulation difficulties was the greatest predictor of emotional eating, suggesting that individuals who have difficulty regulating their emotions are more likely to engage in emotional eating behavior”. Similarly, Crockett et al. [3] concluded that “In every model we tested, difficulties in emotion regulation predicted emotional eating”. Sultson and Akkermann [19] concluded that "Higher level of ER difficulties among obese and normal weight individuals with EE also lend further support for the assumption that emotion dysregulation might underlie EE". Kornacka et al. [20] highlighted the “[…] crucial role of ruminative thinking in the occurrence of emotional eating […]”. Regarding avoidance, Deroost and Cserjési [21] showed “[…] that people with a high degree of EM use avoidance as a primary coping strategy" and added that "avoidance coping also significantly predicted the level of EM” (EM = emotional eating).
Future studies focusing on EE and ER should separately test other specific types of emotional eating (e.g., EE in response to depression, to anxiety…). Indeed, Braden et al. [22] explained that “exploratory analyses suggest possible unique relationships between types of emotional eating and specific facets of emotion regulation”. The authors added that “[…] findings suggest that certain emotion regulation strategies may be more closely linked to various types of emotional eating”.
Emotional eating and inhibition
The studies included in this scoping review dealing with EE and inhibition/impulsivity confirmed the existence of an association between EE and some inhibition difficulties and impulsivity. For example, Wolz et al. [23] showed that “[…] emotional eating was not related to general inhibitory control deficits, but was associated with higher behavioral inhibitory control difficulties only while suppressing negative emotions. They added that “[…] the difficulty to inhibit behavioral responses while regulating negative emotions may contribute to disinhibited food intake while experiencing negative emotions”. Stapleton and Whitehead [18] revealed that emotional eating was related to high impulsivity and that impulsivity was the second greatest predictor of EE after emotion regulation difficulties. Regarding self-control, Wood et al. [24] showed “[…] an increase in activation across brain regions related to self-control and urges in response to high-calorie food associated with both emotional eating and routine restraint". Taken together, these findings confirm that emotional eaters are prone to inhibition impairments. Moreover, Wolz et al. [23] suggest that deficits in inhibition only appear when participants are regulating their emotions, highlighting an interesting link between ER and inhibition in EE.
BED and emotion regulation
Concerning BED and emotion regulation, most of the studies confirm the ER difficulties in BED. Leehr et al. [25] showed that individuals with BED have lower ER capacities. Limited access to ER strategies is also one of the ER difficulties met in BED [26, 27], as well as nonacceptance of emotional responses [27] and lack of emotional clarity [26, 27].
BED and inhibition
Overall, studies focusing on BED indicated a deficit in inhibition and increased impulsivity. Leehr et al. [25] concluded that “Overall, results support the assumption of inhibitory control deficiencies in BED on a behavioral level”. Grant and Chamberlain [28] underlined that “Binge-eating disorder was associated with impaired response inhibition and executive planning”. Schag et al. [29] said that “[…] BED represents a neurobehavioural phenotype of obesity that is characterized by increased impulsivity”, and Leehr et al. [30] showed that “the BED + sample showed higher trait and behavioural impulsivity”. Moreover, according to Aloi et al. [31], “[…] impaired self-monitoring metacognition and difficulties in impulse control are the central nodes in the psychopathological network of BED […]”.
Overeating and emotion regulation
One of the objectives of this scoping review was to clarify the ill-defined concept of overeating. In the eating disorders literature, overeating sometimes refers to a symptom of an eating disorder or as an eating behavior or is sometimes used as a synonym for emotional eating or binge eating.
Unfortunately, only two of the studies included in this scoping review focused on overeating [32, 33], so we could not address this specific question. Nevertheless, similar to EE and BED, those studies highlighted the links between overeating and emotion regulation.
Positive emotions and emotional eating
We questioned the possibility of positive emotions causing emotional eating episodes associated with emotion regulation and/or inhibition difficulties (in the same way as negative emotions). Based on the studies included in our review, opinions differ regarding this point. Indeed, while an article highlights that “[…] positive EE was associated with elevated levels of ER difficulties, suggesting that overeating in response to positive emotions might also include some features of emotion dysregulation” [19], another article concludes, on the contrary, that “[…] eating in response to positive emotions was not significantly related to poorer psychological well-being, greater eating disorder symptoms, or emotion dysregulation” [22]. Since there is yet no consensus on the subject, further research on emotional eating needs to be conducted to separately test and dissociate positive and negative emotions.
Positive emotions and BED
We wondered about positive emotions as a possible cause of emotional eating episodes associated with emotion regulation and/or inhibition difficulties. We checked whether the BED studies included in this scoping review addressed the question of positive emotions/affect/mood. Loeber et al. [34] showed that “[…] restrained eating and mood are factors that moderate response inhibition to food-associated stimuli in obese patients with BED” and that “[…] apart from negative mood, positive mood might as well be a trigger for loss of control over eating behaviour”.
Finally, it is worth mentioning that one study showed that negative and positive mood levels are different during binge days, with an increasing negative mood and a decreasing positive mood at the first binge-eating episode (see Munsch et al. [35]).
Emotional eating and weight profiles
Studies included in this scoping review tended to show that the relationships between EE and emotion dysregulation (and anxiety, depression, and rumination) might be different according to the weight profile (i.e., normal weight, overweight, and with moderate or severe obesity) (see, for example, Willem et al. [36] or Kornacka et al. [20]). Willem et al. [36] highlighted that “emotion dysregulation, anxiety and depression have different impacts on emotional eating (EE) depending on obesity severity", while Kornacka et al. [20] underlined that “the role of emotional eating in the link between rumination and uncontrolled eating is different in overweight vs. healthy individuals”.
Emotional eating, BED and rumination
According to three of the studies included in this scoping review, rumination, a maladaptive emotion regulation strategy, is encountered in both EE and BED. Indeed, in EE, Kornacka et al. [20] highlight that rumination is a predictor of EE (“[…] the results of the two studies confirm the crucial role of ruminative thinking in the occurrence of emotional eating […]”. Similarly, people with BED are more inclined than healthy people to use rumination as a negative emotion regulation strategy [27]. Wang et al. [37] also highlighted that “[…] rumination is an important cognitive process associated with severity of eating-disorder psychopathology”.
The idea of a possible continuum
We hypothesized that there would be a continuum between EE (nonpathological eating behavior) and BED (pathological eating behavior). Three studies focusing on BED mentioned this idea of a continuum in the severity of eating disorders. Leehr et al. [25] stated that “From a clinical perspective eating behavior of the three groups can be seen on a continuum from normal eating behavior, to overeating, to binge eating”. Mobbs et al. [38] highlighted that “[…] these cognitive deficits are more severe in obese patients with binge eating disorder, which indicates that there is a continuum of increasing inhibition and cognitive problems with increasingly disordered eating”. Moreover, Svaldi et al. [39] underlined that “[…] the magnitude of the inhibitory deficit was found to be related to the reported severity of eating pathology”, which is compatible with the idea of a continuum.
However, none of the reviewed studies directly compared EE to BED regarding ER or inhibition performances, neither in a longitudinal nor cross-sectional design. Thus, a gap can clearly be identified in this specific field since there is a complete lack of experimental data about an increased severity in ER and inhibition deficit between EE and BED.
Critical analysis
We identified some limitations between studies, and some of them were quite redundant in our corpus. First, half of the included studies recorded only self-reported data using scales, questionnaires, or interviews. These declarative measures often suffer from memory bias or social desirability concerns [40]. Moreover, these measures are often carried out for a particular purpose, and this purpose may differ from study to study, depending on the research question being asked [40]. Strikingly, 88.9% of papers addressing ER gathered only self-report measures (but only 11.8% for inhibition). Thus, there is a lack of experimental data to address the issue of ER in BED and EE.
Second, 43.8% of the articles with self-report measures only appeared to have rather small sample sizes and/or unbalanced groups and were therefore underpowered. Sample size is a critical issue for quantitative analysis. This sample size must be large enough to achieve the appropriate level of measurement precision. [41].
Third, most of the participants enrolled in these studies were women, compromising the generalizability to the global population (81.3% of studies had only women participants or an unbalanced sex ratio toward women). Eating disorders are more frequent among women, and for BED, the ratio varies between 1:2 and 1:6 [42]. Thus, while the lack of men in BED studies is understandable, future studies should consider recruiting more men to properly balance the experimental groups.
Finally, a recurring limitation emphasized by many authors of the included studies is that their research was cross-sectional. Indeed, given the short duration of these types of studies, it was impossible to reveal some causal links between different phenomena (e.g., between BED and impulsivity). However, in our opinion, this is not a limitation per se, as cross-sectional and longitudinal studies are two very different types of research. Therefore, we did not report this limitation in Table 1.
Discussion
The main objectives of this scoping review were to explore the idea of a continuum between EE and BED as well as explore the idea of a gradation in emotion regulation and inhibition deficits along this continuum. This hypothesis is supported by some authors and is widely discussed in Davis [14]. He developed the concept of an “eating continuum”, ranging from homeostatic eating (energy balance) to food addiction, with different levels of “overeating”, including BED-like symptoms and diagnosed BED. It should also be noted that this idea of a continuum is shared by many physicians in their daily clinical practice and that this idea needs to be verified.
The most striking result of our scoping review is that there are strong similarities between EE and BED, with emotional eaters and BED patients sharing the same difficulties in emotion regulation and inhibition. Some of the included studies seem to be compatible with the idea of a gradation of ER and inhibition deficits following this continuum. For instance, Mobbs et al.’s [38] conclusions strengthened the idea of a continuum of inhibition impairment, with BED patients living with obesity having more difficulties inhibiting their responses compared to controls living with obesity. Indeed, the authors concluded that “[…] these cognitive deficits are more severe in obese patients with binge eating disorder, which indicates that there is a continuum of increasing inhibition and cognitive problems with increasingly disordered eating”. Concerning EE, the results of Sultson and Akkermann [19] showed that participants with EE have more binge eating behaviors than participants without EE but do not meet all the DSM-5 criteria to be diagnosed with BED. These results suggest that EE could lead to BED and thus support the idea of a continuum. It is, however, crucial to remember that none of the articles included in this review directly compared EE and BED in the same study, neither in a longitudinal nor cross-sectional design. To ascertain the existence of a continuum between EE and BED, the increased severity of ER and inhibition deficits between EE and BED still need to be proven. One of the main goals of this scoping review was also to identify knowledge gaps, and indeed, we found a gap in the literature regarding the increased severity in ER and inhibition impairments from EE to BED. Such a lack of experimental work is truly surprising given the feelings shared by many caregivers in the field of eating disorders as well as the thoughts shared by some authors [14, 25, 38, 39].
Among the thirty-two articles reviewed, only one focused on the relationship between ER and inhibition in EE. Indeed, Wolz et al. [23] showed that EE was associated with higher behavioral inhibitory control difficulties only while participants were suppressing negative emotions. This outcome should be taken into account in further studies, since ER and inhibition deficits are often studied separately [7, 43, 44]. Indeed, the direct relationship between ER and inhibition remains poorly studied in BED, as well as in EE, but is an important question to explore the idea of a continuum.
The third objective of this scoping review was to address the ill-defined concept of overeating. Unfortunately, only two studies focused on overeating [32, 33], and it is thus difficult to clearly define this concept. For both authors, overeating is not an eating disorder per se since participants were healthy volunteers with no prior diagnosis of an eating disorder. However, in both studies, overeating is measured with questionnaires widely used in medical contexts to assess eating disorders, such as the Eating Disorder Examination-Questionnaire (EDE-Q) or the Binge Eating Scale (BES). Thus, overeating may be seen as pathological eating. Moreover, Racine and Horvath [33] used the Eating Disorder Diagnostic Scale and the Questionnaire on Eating and Weight Patterns-5 (QEWP-5) to determine experimental groups. Women included in the “overeating” group reported consuming an “unusually large amount of food unaccompanied by loss of control over the past 3 months” on both questionnaires. Thus, this inclusion criterion could be a suitable definition of the concept of overeating, but it must be emphasized that there is too little information to properly define this concept.
The fourth aim of this review was to determine whether positive emotions could trigger emotional eating or binge eating episodes associated with emotion regulation and/or inhibition difficulties. Most of the studies only measured EE and binge eating episodes in response to negative emotions. However, few articles specifically focused on positive mood or emotions. Due to a lack of consensus among studies, it was impossible to strongly conclude that positive emotions can affect eating behaviors. Indeed, some data support this idea [19, 34], and others are less affirmative [22, 35].
Last, concerning the weight profile, it was not one of the aims of this scoping review, but our results showed that emotion regulation deficits were more severe in obese participants than in normal weight or overweight volunteers. Thus, the weight profile seems to be an important parameter when addressing the question of an increased severity in ER deficits between EE and BED.
Limitations
This scoping review presents some limitations. First, regarding the selection phase, not all relevant studies may have been indexed in the two searched databases (PsycINFO and PubMed/Medline). Second, the examination was based on a list of terms describing emotional eating, binge-eating disorder, emotion regulation and inhibition. The possibility that additional articles would have been identified by adding other terms cannot be completely excluded, although the search was intended to be as extensive as possible. Third, a possible limitation of our scoping review is that we did not mention explicitly in our search equation the terms “positive emotions”. Indeed, given that one of our questions was about the possibility that positive emotions can, like negative emotions, trigger emotional eating episodes, we could have perhaps included it in our search equation. Nevertheless, given that we used the inclusive terms “Emotional Regulation”[Mesh]” and “Emotion regulation”, it is likely that we did not miss some interesting records focusing on positive emotions. Finally, in this review, only studies in French or English were included, which did not allow us to be exhaustive in our conclusions.
Conclusion and further directions
In conclusion, this scoping review fully confirmed the presence of inhibition and emotion regulation deficits in both EE and BED, showing strong similarities between these two eating behaviors. However, the lack of experimental data coming from direct comparisons between EE and BED did not make it possible either to confirm the existence or the absence of a possible continuum between EE and BED or an increased severity in ER and inhibition deficits between EE and BED. Thus, this scoping review helped to identify a knowledge gap, and the question of the existence of a continuum still needs to be addressed in further research.
If such a continuum exists, we think it could greatly impact the clinical care of eating disorders. Indeed, if EE can become BED, early care of emotional eaters becomes essential, and early diagnoses could be made. Additionally, prevention could be improved in emotional eaters and even in the general population to avoid progression to an eating disorder (i.e., subthreshold BED and BED) and could also reduce the risk of developing obesity and its comorbidities often associated with BED. Given the variety of symptoms (psychological and physical), monitoring of emotional eaters could be performed by a multidisciplinary medical team, especially for children and adolescents.
The existence of a continuum between EE and BED could also have implications for eating disorder research. In our view, this could lead to further research to develop more specific screening instruments, such as scales and questionnaires. Such instruments might indeed be helpful to classify emotional eater participants into more relevant experimental groups that take into account the severity of EE. To go even further, one could imagine a new scale that would assess the level of eating behaviors across the entire continuum. Moreover, regarding data analysis, data could be analyzed in a discrete way in addition to group comparisons between EE and BED. Last, if such a continuum was verified, it could guide the focus on future research, especially studies on the etiology of BED, and help to better define the concept of “emotional overeating”.
Moreover, to test the idea of a continuum from a different angle, it could be interesting to see if there is an evolution of some other markers between EE and BED, such as biomarkers. Some of them are well known in BED but remain rather poorly studied in EE. Several fMRI studies have shown that brain activation patterns are different in BED patients, especially in the reward system, which explains why this eating disorder is often associated with food addiction [14]. For example, the ventral striatum and the medial prefrontal cortex seem to be underactivated during a rewarding task. Moreover, the ventral putamen, orbitofrontal cortex, amygdala, and insula respond less in BED patients than in controls [8]. EEG studies have also provided a valuable understanding of neurophysiological markers. In their narrative review, Berchio et al. [45] found that behavioral traits of BED and bulimia nervosa, such as loss of control over eating and emotional eating, are associated with an increased attentional reactivity (P300 wave) to visual food stimuli. Finally, animal studies allow us to better understand the functioning of some molecules. For example, the role of dopamine, oxytocin, and opiate in eating disorders is well understood [46], and this could be an interesting focus to measure the gradation between EE and BED.
Availability of data and materials
Two electronic bibliographic databases, PubMed/Medline and PsycINFO, were searched to identify references related to the scoping review topic. The search focused on articles published between January 2009 and January 2022. Original records (before screening) can be found using the search equation that was used in both databases: ("Binge-Eating Disorder"[Mesh] OR BED OR Binge eater OR Emotional Eating OR Emotional Overeating OR Overeater OR Emotional eater OR Overeating) AND ("Emotional Regulation"[Mesh] OR Emotion regulation OR Reappraisal OR Rumination OR Attentional deployment OR Mood regulation OR "Inhibition, Psychological"[Mesh] OR Inhibitory control). The 32 articles included after the screening steps are listed in the References section.
Abbreviations
- EE:
-
Emotional eating
- BED:
-
Binge-eating disorder
- ER:
-
Emotion regulation
- PRISMA-ScR:
-
Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews
- PICOS criteria:
-
Populations, interventions, comparisons, outcomes, studies
- DSM-IV-TR, or DSM-5:
-
Diagnostic and statistical manual of mental disorders Text Revision, or 5th edition
- EEG:
-
Electroencephalography
- MEG:
-
Magnetoencephalography
- NWC:
-
Normal weight controls
- FST:
-
Food stroop task
- BMI:
-
Body mass index
- BIS-11:
-
Barratt impulsiveness scale
- EMA:
-
Ecological momentary assessment
- BN:
-
Bulimia nervosa
- HC:
-
Healthy controls
- ED:
-
Eating disorders
- DERS:
-
Difficulties in emotion regulation scale
- BED + :
-
People living with BED (or subthreshold BED, depending on the studies)
- BED-:
-
People living without BED (or subthreshold BED, depending on the studies)
- LOC:
-
Loss of control
- OBE:
-
Objective binge episode
- LPP:
-
Late positive potential
- SST:
-
Stop signal task
- SSRT:
-
Stop signal reaction time
- fMRI:
-
Functional magnetic resonance imaging
- HV:
-
Healthy volunteers
- GoRT:
-
Go-trial reaction time
- NW-BED:
-
Normal-weight people living with BED
- OW-BED:
-
Overweight people living with BED
- EF:
-
Executive functioning
- OB:
-
Non-BED obese individuals
- LC:
-
Lean comparison
- vmPFC:
-
Ventromedial prefrontal cortex
- IFG:
-
Inferior frontal gyrus
- AN-R:
-
Anorexia nervosa-restricting type
- AN-BP:
-
Anorexia nervosa–binge/purge type
- EDNOS:
-
Eating disorder, not otherwise specified
- EM:
-
Emotional eating/eaters (depending on the studies)
- ECT:
-
Exogenous cueing task
- NA:
-
Network analysis
- OE:
-
Overeating
- EO:
-
Emotional overeating
- MeSH:
-
Medical subject headings
- EM:
-
Emotional eating (used in some of the included articles)
- EDE-Q:
-
Eating disorder examination-questionnaire (EDE-Q)
- BES:
-
Binge eating scale
- QEWP-5:
-
Eating disorder diagnostic scale and the questionnaire on eating and weight patterns-5
References
van Strien T, van de Laar FA, van Leeuwe JFJ, Lucassen PLBJ, van den Hoogen HJM, Rutten GEHM, et al. The dieting dilemma in patients with newly diagnosed type 2 diabetes: does dietary restraint predict weight gain 4 years after diagnosis? Health Psychol. 2007;26(1):105–12.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington: American psychiatric association; 2013.
Crockett AC, Myhre SK, Rokke PD. Boredom proneness and emotion regulation predict emotional eating. J Health Psychol. 2015;20(5):670–80.
Dingemans A, Danner U, Parks M. Emotion regulation in binge eating disorder: a review. Nutrients. 2017;9(11):1274.
Ferrell EL, Watford TS, Braden A. Emotion regulation difficulties and impaired working memory interact to predict boredom emotional eating. Appetite. 2020;144:104450.
Giel KE, Teufel M, Junne F, Zipfel S, Schag K. Food-related impulsivity in obesity and binge eating disorder-a systematic update of the evidence. Nutrients. 2017;9(11):1170.
Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE. Emotion regulation model in binge eating disorder and obesity–a systematic review. Neurosci Biobehav Rev. 2015;49:125–34.
Steward T, Menchon JM, Jiménez-Murcia S, Soriano-Mas C, Fernandez-Aranda F. Neural network alterations across eating disorders: a narrative review of fMRI studies. Curr Neuropharmacol. 2018;16(8):1150–63.
Waltmann M, Herzog N, Horstmann A, Deserno L. Loss of control over eating: a systematic review of task based research into impulsive and compulsive processes in binge eating. Neurosci Biobehav Rev. 2021;129:330–50.
Zhang P, Wu GW, Yu FX, Liu Y, Li MY, Wang Z, et al. Abnormal regional neural activity and reorganized neural network in obesity: evidence from resting-state fMRI. Obes Silver Spring Md. 2020;28(7):1283–91.
Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. J Consult Clin Psychol. 2000;68(1):95–102.
Nicholls W, Devonport TJ, Blake M. The association between emotions and eating behaviour in an obese population with binge eating disorder: emotions and binge eating disorder. Obes Rev. 2016;17(1):30–42.
Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What’s driving the binge in binge eating disorder?: a prospective examination of precursors and consequences. Int J Eat Disord. 2007;40(3):195–203.
Davis C. From passive overeating to « food addiction »: a spectrum of compulsion and severity. ISRN Obes. 2013;2013:435027.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Arexis M, Feron G, Brindisi MC, Billot PE, Chambaron S. Impacts of emotional regulation and inhibition on Emotional Eating (EE) and Binge Eating Disorder (BED): Protocol for a scoping review. Hal-03643357. 2022.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Stapleton P, Whitehead M. Dysfunctional eating in an Australian community sample: the role of emotion regulation, impulsivity, and reward and punishment sensitivity. Aust Psychol. 2014;49(6):358–68.
Sultson H, Akkermann K. Investigating phenotypes of emotional eating based on weight categories: a latent profile analysis. Int J Eat Disord. 2019;52(9):1024–34.
Kornacka M, Czepczor-Bernat K, Napieralski P, Brytek-Matera A. Rumination, mood, and maladaptive eating behaviors in overweight and healthy populations. Eat Weight Disord EWD. 2021;26(1):273–85.
Deroost N, Cserjési R. Attentional avoidance of emotional information in emotional eating. Psychiatry Res. 2018;269:172–7.
Braden A, Musher-Eizenman D, Watford T, Emley E. Eating when depressed, anxious, bored, or happy: are emotional eating types associated with unique psychological and physical health correlates? Appetite. 2018;125:410–7.
Wolz I, Biehl S, Svaldi J. Emotional reactivity, suppression of emotions and response inhibition in emotional eaters: a multi-method pilot study. Appetite. 2021;161:105142.
Wood SMW, Schembre SM, He Q, Engelmann JM, Ames SL, Bechara A. Emotional eating and routine restraint scores are associated with activity in brain regions involved in urge and self-control. Physiol Behav. 2016;165:405–12.
Leehr EJ, Schag K, Dresler T, Grosse-Wentrup M, Hautzinger M, Fallgatter AJ, et al. Food specific inhibitory control under negative mood in binge-eating disorder: evidence from a multimethod approach. Int J Eat Disord. 2018;51(2):112–23.
Gianini LM, White MA, Masheb RM. Eating pathology, emotion regulation, and emotional overeating in obese adults with Binge Eating Disorder. Eat Behav. 2013;14(3):309–13.
Walenda A, Kostecka B, Santangelo PS, Kucharska K. Examining emotion regulation in binge-eating disorder. Borderline Personal Disord Emot Dysregulation. 2021;8(1):25.
Grant JE, Chamberlain SR. Neurocognitive findings in young adults with binge eating disorder. Int J Psychiatry Clin Pract. 2020;24(1):71–6.
Schag K, Teufel M, Junne F, Preissl H, Hautzinger M, Zipfel S, et al. Impulsivity in binge eating disorder: food cues elicit increased reward responses and disinhibition. PLoS ONE. 2013;8(10):e76542.
Leehr EJ, Schag K, Brückmann C, Plewnia C, Zipfel S, Nieratschker V, et al. A putative association of COMT Val(108/158)met with impulsivity in binge eating disorder. Eur Eat Disord Rev J Eat Disord Assoc. 2016;24(2):169–73.
Aloi M, Rania M, Carbone EA, Caroleo M, Calabrò G, Zaffino P, et al. Metacognition and emotion regulation as treatment targets in binge eating disorder: a network analysis study. J Eat Disord. 2021;9(1):22.
Görlach MG, Kohlmann S, Shedden-Mora M, Rief W, Westermann S. Expressive suppression of emotions and overeating in individuals with overweight and obesity. Eur Eat Disord Rev J Eat Disord Assoc. 2016;24(5):377–82.
Racine SE, Horvath SA. Emotion dysregulation across the spectrum of pathological eating: comparisons among women with binge eating, overeating, and loss of control eating. Eat Disord. 2018;26(1):13–25.
Loeber S, Rustemeier M, Paslakis G, Pietrowsky R, Müller A, Herpertz S. Mood and restrained eating moderate food-associated response inhibition in obese individuals with binge eating disorder. Psychiatry Res. 2018;264:346–53.
Munsch S, Meyer AH, Quartier V, Wilhelm FH. Binge eating in binge eating disorder: a breakdown of emotion regulatory process? Psychiatry Res. 2012;195(3):118–24.
Willem C, Gandolphe MC, Doba K, Roussel M, Verkindt H, Pattou F, et al. Eating in case of emotion dys-regulation, depression and anxiety: different pathways to emotional eating in moderate and severe obesity. Clin Obes. 2020;10(5):e12388.
Wang SB, Lydecker JA, Grilo CM. Rumination in patients with binge-eating disorder and obesity: associations with eating-disorder psychopathology and weight-bias internalization. Eur Eat Disord Rev J Eat Disord Assoc. 2017;25(2):98–103.
Mobbs O, Iglesias K, Golay A, Van der Linden M. Cognitive deficits in obese persons with and without binge eating disorder. Investigation using a mental flexibility task. Appetite. 2011;57(1):263–71.
Svaldi J, Naumann E, Trentowska M, Schmitz F. General and food-specific inhibitory deficits in binge eating disorder. Int J Eat Disord. 2014;47(5):534–42.
Kimberlin CL, Winterstein AG. Validity and reliability of measurement instruments used in research. Am J Health-Syst Pharm AJHP Off J Am Soc Health-Syst Pharm. 2008;65(23):2276–84.
Frost MH, Reeve BB, Liepa AM, Stauffer JW, Hays RD. Mayo/FDA patient-reported outcomes consensus meeting group; What is sufficient evidence for the reliability and validity of patient-reported outcome measures? Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2007;10(Suppl 2):S94-105.
Raevuori A, Keski-Rahkonen A, Hoek HW. A review of eating disorders in males. Curr Opin Psychiatry. 2014;27(6):426–30.
Carr MM, Wiedemann AA, Macdonald-Gagnon G, Potenza MN. Impulsivity and compulsivity in binge eating disorder: a systematic review of behavioral studies. Prog Neuropsychopharmacol Biol Psychiatry. 2021;12:110318.
Saruco E, Pleger B. a systematic review of obesity and binge eating associated impairment of the cognitive inhibition system. Front Nutr. 2021;8:609012.
Berchio C, Cambi S, Pappaianni E, Micali N. EEG biomarkers in children and adolescents with feeding and eating disorders: current evidence and future directions. Front Psychiatry. 2022;13:882358.
Turton R, Chami R, Treasure J. Emotional eating, binge eating and animal models of binge-type eating disorders. Curr Obes Rep. 2017;6(2):217–28.
Acknowledgements
Not applicable.
Funding
This scoping review was supported by grants from the French National Research Agency [Agence Nationale de la Recherche (ANR): ImplicEAT project ANR-17-CE21-0001].
Author information
Authors and Affiliations
Contributions
All authors participated in the conception of the study. Three investigators (authors MA, P-EB, and SC) developed a data charting form to extract the relevant data from each of the 32 included studies. For each study, author MA extracted the data according to the following variables of the chart: authors, title, year of publication, country of the study, journal of publication, type of study, method/study design, participants and sample sizes, type of interventions, comparisons, and outcomes/results. Two authors (MA and P-EB) listed the possible limitations of each study. The limitations identified by both authors were retained, and the others were either eliminated or retained after discussion. Two authors (SC and M-CB) checked this list, and their comments were considered. MA wrote the first draft of the article and MA, P-EB, SC and M-CB contributed to the final version. All authors proofread the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This scoping review did not involve animals or human participants, and we did not use personal information. All data used in this review were extracted from published articles.
Consent for publication
This scoping review did not involve human participants, and we did not use personal information. Thus, consent for publication was unnecessary for this scoping review.
Competing interests
The authors declare that they have no competing interests.
Protocol
The review protocol can be accessed at HAL (https://hal.science/hal-03643357v1—HAL Id/Registration number: hal-03643357). Protocol reference: Arexis, M., Feron, G., Brindisi, M.-C., Billot, P.-E., & Chambaron, S. (2022). Impacts of emotional regulation and inhibition on Emotional Eating (EE) and Binge Eating Disorder (BED): Protocol for a scoping review. Hal-03643357.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Arexis, M., Feron, G., Brindisi, MC. et al. A scoping review of emotion regulation and inhibition in emotional eating and binge-eating disorder: what about a continuum?. J Eat Disord 11, 197 (2023). https://doi.org/10.1186/s40337-023-00916-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40337-023-00916-7