Abstract
Purpose of Review
During the height of the coronavirus pandemic, the oral cavity was recognized as a critically important site for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection. The purpose of this review is to analyze the literature surrounding SARS-CoV-2 entry, replication, and transmission and the resulting impact on host tissues in the oral cavity.
Recent Findings
The detection of viral genetic material in saliva allows for widespread surveillance testing and emphasizes the importance of viral transmission through shed in saliva. As the cohort of patients who have recovered from acute SARS-CoV-2 infection grows, several questions remain about the long-term impacts of viral infection on the oral tissues, including whether the oral cavity may serve as a persistent viral reservoir. Therefore, a thorough understanding of the viral life cycle in the diverse tissues of the oral cavity is warranted. We conclude with a broad outlook on the long-term effects of SARS-CoV-2 infection in the oral cavity and how these effects may relate to the post-acute coronavirus syndrome sequelae experienced by recovered patients.
Summary
SARS-CoV-2 can enter and replicate in the oral cavity and be spread between individuals via shed in saliva. Several acute oral manifestations of infection have been reported, and the lingering effects of infection on oral tissues are an area of ongoing investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The oral cavity is a physiologic conduit between the external and internal environments connected not only to the respiratory and gastrointestinal tracts, but also to the systemic vasculature via lymphatic and blood vessels. As such, the oral cavity is a critical but understudied hub for viral infections, acting as a site of initial viral contact, entry, and replication allowing for viral transmission both within and between individuals. The emergence of the COVID-19 pandemic and the widespread use of salivary diagnostics for viral surveillance emphasize the epidemiologic significance of the oral cavity, which has been recognized as a site of SARS-CoV-2 entry and replication.
Since the onset of the pandemic, several reviews have outlined the acute oral manifestations of COVID-19 [1,2,3,4,5] and the use of saliva as a diagnostic tool [6, 7]. While studies have shown that oral tissues including the buccal mucosa, tongue, and salivary glands can support SARS-CoV-2 infection, viral persistence and long-term consequences of viral infections in these sites are not well understood. Further, there is a need for new perspectives on oral SARS-CoV-2 infection considering recent studies with cohorts of patients who have recovered from COVID-19 but continue to experience both persistent and new non-resolving symptoms, a phenomenon known as post-acute coronavirus syndrome, or “long COVID.” The purpose of this review is to (1) critically trace the path of SARS-CoV-2 infection in the oral cavity, from viral entry to egress, and (2) hypothesize on the long-term consequences of oral SARS-CoV-2 infection, including whether the oral cavity can serve as a reservoir for infectious virus and if history of SARS-CoV-2 infection can leave lasting signatures of viral infection.
Entry
SARS-CoV-2 is an enveloped positive single-strand RNA virus that is the etiologic agent of COVID-19. The virus primarily gains entry through infection of epithelial cells (e.g., mucosae) through inhalation of droplets or aerosols or ingestion of fomites. The most notable infection sites include those of the respiratory tract. Upon inoculation, the SARS-CoV-2 viral spike glycoprotein binds to the angiotensin-converting enzyme 2 (ACE2) receptor on host cells [8•]. Following receptor binding, the spike protein is cleaved by host proteases, including most specifically the transmembrane protease serine 2 (TMPRSS2), leading to the fusion of the viral and host membranes and facilitating viral entry [9]. In addition to principal entry factors, other mechanisms of entry have been described including alternate receptors (e.g., neuropilin-1, heparin sulfate), antibody-mediated endocytosis, and transcytosis of virions to adjacent cells [10]. Despite the existence of alternate receptors and entry mechanisms, the distribution of ACE2 and TMPRSS2 are consistent predictors of SARS-CoV-2 tissue tropism.
The early hypothesis that SARS-CoV-2 may infect the oral tissues was based on database mining for expression of the SARS-CoV-2 entry receptors in various oral tissues, which were eventually paired with studies in human biopsy specimens. In the early stages of the pandemic, Xu et al. (2020) analyzed bulk RNA sequencing (RNA-seq) data from TCGA and FANTOM5 CAGE databases and found that ACE2 was expressed in oral tissues, particularly the oral tongue, and a follow-up single-cell RNA-seq (scRNA-seq) library generated from buccal, gingival, and dorsal tongue tissues demonstrated high ACE2 expression in tongue tissue, specifically in epithelial cells [11]. Analysis of scRNA-seq datasets and immunohistochemistry in adjacent healthy tissues from patients diagnosed with oral squamous cell carcinoma showed that the majority of ACE2 expression was mostly restricted to epithelial cells, specifically in the basal layer, with appreciably less expression in fibroblasts and immune cells [12]. Since the TMPRSS2 protease also contributes to efficient SARS-CoV-2 entry, additional studies in human tissues analyzed ACE2 and TMPRSS2 co-expression and found that both factors were expressed in the dorsal tongue, mostly in the spinous layers of the stratified squamous epithelium, with ACE2 expressed in the cytoplasm and cell membrane and TMPRSS2 expressed predominantly on the cell membrane [13, 14]. ACE2 and TMPRSS were also expressed in other stratified squamous tissues including buccal, labial, and lingual mucosae [13, 14]. Notably, ACE2 and TMPRSS2 were almost exclusively expressed in epithelial tissues, with weak to undetectable expression in connective tissue layers. The distribution of SARS-CoV-2 entry receptors in the suprabasal epithelium supports the notion that the most superficial layer of the oral cavity is a readily accessible initial site of entry for virus particles. However, the suprabasal mucosa is relatively transcriptionally inert and rapidly sloughs into the oral cavity. While it is possible that SARS-CoV-2 infects and replicates in these cells, it raises the possibility that other proximal cell types may be vulnerable and contribute to viral infection and replication [15••].
The salivary glands are other viral ports of entry in the oral cavity. The salivary glands consist of three major glands (parotid, submandibular, and sublingual) as well as hundreds to thousands of minor salivary glands distributed throughout the mucosae of the oral cavity (e.g., labial and buccal mucosa, hard and soft palate, oro- and nasopharynx, and the tongue and floor of mouth). Analysis of bulk RNA-seq databases and the Human Protein Atlas demonstrated expression of both ACE2 and TMPRSS2 in the salivary glands [16, 17]. In further support of these findings, a novel single-cell atlas derived from human minor salivary glands revealed expression of ACE2 and TMPRSS2, with rates of co-expression comparable to levels in nasal and gastrointestinal sites [15••]. ACE2 and TMPRSS2 are also expressed in the major salivary glands (e.g., parotid, sublingual, and submandibular glands) (Fig. 1), present in the serous acini and ductal cells, but less in the mucous acinar cells [15, 18, 19]. Epithelial cells are continually shed into the oral cavity; it is possible that these infected cells could be shed into saliva serving as both a substrate for infection and a vehicle for viral spread [15••]. ACE2 and TMPRSS2 were detected in the acellular portion of saliva, and exogenous ACE2 and TMPRSS2 were able to adsorb to cultured oral epithelial cells [19], which may be a potential mechanism for viral spread between tissues of the oral cavity and to other individuals. However, whether secreted ACE2 can be bound to infectious viral particles remains to be determined.
Viral entry factors, ACE2 and TMPRSS2, are expressed in human salivary gland tissues. a, b mRNA expression of ACE2 (red) and TMPRSS2 (white) was analyzed using RNAscope fluorescence in situ hybridization (FISH). ACE2 and TMPRSS are expressed in pan-cytokeratin (pCTK) positive epithelial cells (green) in both minor salivary gland a and parotid gland b tissue sections from healthy volunteers. c, d Immunofluorescence (IF) imaging with confocal microscopy demonstrates ACE2 expression (green) in both acini and ducts of the minor salivary glands of healthy volunteers. Co-localization with aquaporin-5 (AQP5, purple) c or smooth muscle actin (SMA, purple) d and ACE2 is visualized in white indicating that acinar, ductal, and myoepithelial cells can express viral entry factors. Subject biopsies were obtained under NIH IRB-approved protocol: 15-D-0051-Characterization of Diseases With Salivary Gland Involvement [PI-Warner, NCT02327884]. The images shown are original, unpublished figures
Replication
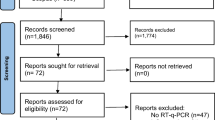
While the distribution of SARS-CoV-2 entry receptors were characterized early in the pandemic, further work was needed to determine whether the oral cavity could serve as a site of virus replication and virion production. Minimally invasive studies provided critical early insights into the sites of viral infection throughout the body. The gingival epithelium of the periodontium was one of the earliest oral sites in which SARS-CoV-2 RNA was detected by RT-qPCR, with accompanying histopathological findings observed in the tissues of the junctional epithelium [20]. Despite the high expression of ACE2/TMPRSS2 in the tongue, one study using in situ hybridization demonstrated relatively lower levels of SARS-CoV-2 RNA in tongue tissues as compared to tissues of the proximal airway [21]. Nevertheless, tongue scrapings from patients [22] and mucosal brush biopsies from autopsy tissues and acutely infected patients [15••] revealed cellular expression of SARS-CoV-2 spike RNA and protein, which suggests that like the distribution of ACE2/TMPRSS2, the virus localizes to the most superficial levels of the epithelium, layers which would be shed into the oral cavity and could facilitate interpersonal transmission of the virus. Cells isolated from buccal scrapings from patients infected with COVID-19 also exhibited cytopathic changes as compared to cells collected from healthy controls, including karyorrhexis, karyolysis, and micronucleation, though future studies are needed to determine if these effects are direct results of viral infection [23, 24].
The salivary glands are an additional site of interest for viral infections. Many viruses (e.g., hepatitis C virus, cytomegalovirus, Epstein Barr virus) infect the salivary glands, which then serve as short-term or chronic viral reservoirs. The salivary glands were predicted as SARS-CoV-2 targets early in the pandemic due to high ACE2/TMPRSS2 expression [13, 16, 17]. The hallmark finding that SARS-CoV-2 RNA was detectable in patients’ saliva [25••] further supported the notion that SARS-CoV-2 could infect the salivary glands. Two studies using salivary gland tissues recovered from acutely infected patients and autopsies from severe COVID-19 victims identified viral RNA at highly similar overall rates (57% and 60%) in major and minor salivary gland samples from infected patients [15, 18, 15, 18, 15, 18, 262).
SARS-CoV-2 replicates in the tissues of the human oral cavity. a, b Infection and replication of SARS-CoV-2 were demonstrated using RNAscope fluorescent in situ hybridization (FISH) in minor salivary glands from COVID-19 autopsy specimens (NIH COVID-19 Autopsy Consortium) or acutely infected ambulatory patients (NCT04348240: Transmissibility and Viral Load of SARS-CoV-2 Through Oral Secretions; PI-Warner). a SARS-CoV-2 genomes were detected in pan-cytokeratin (pCTK, green) positive epithelial cells in the acini and ducts of the minor salivary glands. Viral genomes (red) co-localized with ACE2 (white) in the glands. b Replication of SARS-CoV-2 in the salivary gland in the minor salivary gland acini and ducts was shown using probes to SARS-CoV-2 spike (white) and sense (replicative) strand (purple). c Immunohistochemistry (IHC) confirming expression of spike protein in the minor salivary glands in salivary glands from an autopsy specimen (NIH COVID-19 Autopsy Consortium). d FISH in dorsal tongue tissue demonstrates SARS-CoV-2 infection of pCTK-positive epithelial cells (green) with viral genomes visualized in red. ACE2 (white) is also expressed in the dorsal tongue epithelia from an acutely infected individual. The images shown are original, unpublished figures
Given the finding that SARS-CoV-2 can enter and replicate in oral tissues and induce histological abnormalities, the subsequent question is whether these pathological changes directly translate to oral manifestations. To date, numerous acute oral lesions that may be associated with SARS-CoV-2 infection have been described. Since early 2020, case reports of patients with oral lesions [27], dysgeusia [28, 29], xerostomia [30, 31], and salivary gland inflammation [32, 33], among other symptoms, have been published. The acute oral manifestations of COVID-19 have been reviewed extensively [1,2,3,4,5]. However, it is still not clear whether these symptoms are a direct result of tissue disruption due to viral infection (i.e., initiation of host shut-off mechanisms and viral hijacking of host translational machinery) or due to the triggering of an aberrant immune response with viral infection (i.e., immune cell infiltration and autophagy). Future studies are warranted to compare histopathological findings from SARS-CoV-2 infected tissues with clinical manifestations, and in vitro and in vivo mechanistic studies are needed to further understand viral pathophysiology in oral tissues.
Spread
While nasopharyngeal (NP) swabs remained the gold standard for SARS-CoV-2 detection and surveillance, saliva was quickly recognized for its diagnostic potential. In the first months of the pandemic, it was reported that SARS-CoV-2 RNA could be detected in 11 out of 12 patients who also tested positive via NP swabs [34]. Subsequent papers reported a high concordance between NP swabs and samples derived from the oral cavity and oropharynx, including oropharyngeal swabs and saliva samples [15, 35,36,37,38,39], and several groups have published systematic reviews on this topic [6, 7]. Most importantly, detection of viral genetic material in both cellular and acellular portions of saliva provided strong initial evidence that the virus may be orally transmissible (Fig. 3). In 2021, Huang et al. showed that saliva contained infectious virus particles, as incubation of cells with the acellular fraction of saliva from SARS-CoV-2 positive individuals was sufficient to induce cytopathic effect in Vero cells, and supernatants from these cells could be used to establish infectivity titers [15••]. The authors also demonstrated the ability of cellular portions of saliva to induce a cytopathic effect in cultured cells. This indicates that viral particles could be released directly into the salivary ducts from the salivary glands and/or that viral particles in saliva are derived from infected oral mucosal cells. Both mechanisms, which likely occur simultaneously, support the notion that the oral cavity is a reservoir of infectious virus, and that saliva is an epidemiologically relevant route of viral spread.
SARS-CoV-2-infected cells are shed into saliva and facilitate COVID-19 transmission and viral spread. a RNAscope fluorescent in situ hybridization (FISH) on the cellular fractions of saliva from acutely infected COVID-19 subject (NCT04348240: Transmissibility and Viral Load of SARS-CoV-2 Through Oral Secretions; PI-Warner) show SARS-CoV-2 genomes in ACE2 expressing sloughed epithelial cells, which contains a mixture of both squamous epithelial cells and salivary-derived epithelial cells (data not shown). a, b Immunohistochemistry (IHC) confirming expression of spike protein in sloughed epithelial cells in two acutely infected subjects (NCT04348240: Transmissibility and Viral Load of SARS-CoV-2 Through Oral Secretions; PI-Warner). Both cellular and acellular saliva has been shown to be infectious in ex vivo assays [15••]. The images shown are original, unpublished figures
While saliva is a route of spread between individuals via viral shed in nasal and oropharyngeal droplets, the oral cavity may also serve as a gateway to systemic spread. Anatomically, the oral cavity and oropharyngeal region are entryways to the respiratory, digestive, immune, and vascular systems. There are several potential routes of viral spread between the oral cavity and other tissues. First, SARS-CoV-2 RNA has been detected in an interconnected region of the oral cavity both in oropharyngeal swabs [34] and in the tonsillar tissues [40, 41, 41, 40,41,42], although these findings have not yet been independently replicated. It has been suggested that microaspiration of periodontal bacteria can be linked to aspiration pneumonia and chronic obstructive pulmonary disease [43]; similar phenomenon may occur for other infectious viruses. The periodontal tissues are sites of SARS-CoV-2 infection [15, 20], and infectious virus has been detected in gingival crevicular fluid [44]. The oral-systemic connection is well-established for bacterial pathogens which can traffic from the highly vascularized periodontal pockets to the cardiovascular system to cause infective endocarditis [45]. Given the COVID-19 pulmonary vascular symptoms, it has been proposed that SARS-CoV-2 transits to the lungs via the blood vessels in the periodontal pockets [46], and several studies linking periodontal disease to severe COVID-19 corroborate these findings [47, 48].
Host Response
Even after SARS-CoV-2 has entered, replicated, and shed from oral tissues, the oral cavity can still serve as a readout for host response to SARS-CoV-2 infection via antibody titers. Anti-SARS-CoV-2 antibodies have been detected in saliva from convalescent patients for weeks to months after recovery from viral infection, and often correlate with serum antibody levels [49,50,51,52]. Although anti-SARS-CoV-2 antibodies were present in saliva, they were often non-neutralizing compared to serum IgG [53,54,55], suggesting alternative mechanisms of host defense to SARS-CoV-2 infection in the oral cavity and a possible way in which the virus may escape persist in this tissue type and shed in saliva for extended periods. Moreover, the inflammatory status in the saliva appears more muted as compared to serum samples, with some groups only showing slight increases in proinflammatory cytokines as compared to healthy controls [53, 56, 57]. Interestingly, one study found that certain cytokines, including TNFɑ, IL10, CXCL5, CD40L, and HGF were expressed at lower levels in patients with mild to moderate disease versus healthy controls or patients with severe disease [57]. This may represent a titer-dependent response wherein viral immune evasion mechanisms dominate in moderate infection, but in severe disease, higher viral loads may lead to aberrant activation of the immune system and subsequent tissue destruction.
Saliva also serves as a primary source of defense against infections in the oral cavity as it contains antimicrobial peptides. SARS-CoV-2 infection of the salivary glands and subsequent damage of the glandular tissue may hinder the host antimicrobial defenses in the oral cavity. In support of this notion, Alfaifi et al. (2022) followed a patient with recurrent symptoms of dysesthesia and burning mouth following COVID-19 recovery and discovered significantly reduced levels of the antimicrobial peptide histatin-5 in the patient’s saliva [58]. Histatin-5 has a known role in defense against fungal infections such as Candida albicans, and histatin-5 deficient saliva was ineffective at inhibiting growth of C. albicans in vitro [58]. Several groups have shown a shift in the balance of the oral bacterial microbiome following SARS-CoV-2 infection. The alpha diversity of the salivary microbiome was found to decrease as severity of COVID-19 disease increased [57, 59]. Several groups noted an increased abundance of Streptococcus in saliva samples from infected individuals, but generally, these shifts had no resulting difference in clinical characteristics [60, 61]. Finally, in a cohort of patients diagnosed with myeloencephalitis/chronic fatigue syndrome, COVID-19 infection led to elevated levels of antiviral antibodies against human herpesviruses 1–6, human endogenous retroviruses, and adenovirus in saliva as compared to otherwise healthy patients who had recovered COVID-19 [62, 63]. In both the myeloencephalitis/chronic fatigue syndrome COVID-19 group and the control COVID-19 group, SARS-CoV-2 infection led to an apparent reactivation of latent viruses. While the exact mechanism is still unknown, it is possible that SARS-CoV-2 infection may lead to a suppression of the immune system, creating an environment supportive of replication of other viruses.
Outlook: The Long-Term Impact of COVID-19 on the Oral Cavity
As the number of individuals infected with and recovered from COVID-19 grows, there are increasing reports of lingering symptoms following infection. Some of the symptoms reported by patients include chronic fatigue, muscle weakness, and dyspnea [64]. Despite evidence of the involvement of the oral cavity in the context of SARS-CoV-2 infection, few studies have analyzed the long-term impact of viral infection in oral tissues. Preliminary studies, however, provide evidence that oral manifestations may be a part of the long COVID complex. In a follow-up of 122 patients who had been hospitalized with COVID-19, several had residual oral symptoms an average of 3 months after recovery, including salivary gland ectasia (38%) and xerostomia (30%) [65]. Recently, it has been shown that patients with mild symptomatic and asymptomatic infection continue to have increased inflammation in their salivary glands up to 6 months after infection [66•]. While neither study investigated the presence of the virus in the salivary glands at the time of follow-up, these findings could be the result of persistent low-level infection with SARS-CoV-2 in salivary gland tissue, irreparable damage of salivary gland structures, and/or the result of persistently altered immune responses to initial viral infection. These data are partially supported by autopsy evidence showing detection of virus in salivary tissues 76 days after hospitalization [26••].
Though SARS-CoV-2 has a known tropism for the salivary gland epithelium and known acute effects on the salivary gland architecture, the long-term impact of infection on salivary gland tissue structure and function has not been fully elucidated. Studies in murine models recently demonstrated that infection with SARS-CoV-2 leads to a long-term decrease in salivary flow and an increase in autoantibody production, along with an increased prevalence of lymphocytic infiltration in murine salivary glands [66•]. These findings are consistent with a phenotype reminiscent of Sjӧgren’s disease, an autoimmune disease characterized by dry mouth and dry eyes secondary to immune-mediated destruction of salivary and lacrimal glands. Convalescent sera from patients who had recovered from COVID-19 contained elevated levels of the autoantibodies ANA and SSA/Ro52, which are elevated in patients with Sjӧgren’s disease, as well as an increase in lymphocytic infiltration of the minor salivary glands [66•]. Coupled with the clinical finding of patient-reported dry mouth following clearance of SARS-CoV-2 [65], these results suggest that SARS-CoV-2 infection has long-lasting clinical implications beyond initial infection, which will likely continue to be uncovered in the years following the COVID-19 pandemic.
Conclusions
SARS-CoV-2 interfaces the oral cavity at all stages of infection, from initial entry and replication to the release of viral particles into saliva. Throughout the viral life cycle, there are acute pathologic effects on infected tissues, and the many oral manifestations reported in SARS-CoV-2 infected individuals may be a direct result of virus infection. As the years since the start of the pandemic increase, ongoing research has shifted to the chronic impacts of COVID-19 infection, and follow-ups of patients with long COVID-19 should consider the impacts on the tissues of the oral cavity and effects upon patient quality of life and associated clinical sequela (e.g., recurrent candidiasis infection, dental caries, oral sensation). Further, oral tissues should be studied as a reservoir of viral infections, as current studies rely predominantly on autopsy tissues which do not fully reveal the dynamics of viral shedding. While this review focused on SARS-CoV-2, the overall concept of the oral cavity as a site of viral infections is translatable across diverse pathogen challenges.
Data Availability
NA and BMW contributed to the conception, drafting, and critical revision of the manuscript. PP contributed to the data acquisition for the images presented in the figures. BM and KMB contributed to the editing and critical revision of the manuscript. All authors gave approval for the final manuscript and agree to be accountable for all aspects of the work.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gutierrez-Camacho JR, Avila-Carrasco L, Martinez-Vazquez MC, Garza-Veloz I, Zorrilla-Alfaro SM, Gutierrez-Camacho V, et al. Oral lesions associated with COVID-19 and the participation of the buccal cavity as a key player for establishment of immunity against SARS-CoV-2. Int J Environ Res Public Health. 2022;19(18). https://doi.org/10.3390/ijerph191811383.
Bemquerer LM, de Arruda JAA, Soares MPD, Mesquita RA, Silva TA. The oral cavity cannot be forgotten in the COVID-19 era: is there a connection between dermatologic and oral manifestations? J Am Acad Dermatol. 2021;84(3):e143–5. https://doi.org/10.1016/j.jaad.2020.11.034.
Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, Acevedo AC, De Luca Canto G, Sugaya N, et al. Oral manifestations in patients with COVID-19: a living systematic review. J Dent Res. 2021;100(2):141–54. https://doi.org/10.1177/0022034520957289.
• Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, Acevedo AC, De Luca Canto G, Sugaya N, et al. Oral manifestations in patients with COVID-19: a 6-month update. J Dent Res. 2021;100(12):1321–9. https://doi.org/10.1177/00220345211029637. A comprehensive systemic review covering 183 studies and over 60,000 patients that outlines the prevalence of oral signs and symptoms in SARS-CoV-2 infection.
Lin W, Gao F, Wang X, Qin N, Chen X, Tam KY, et al. The oral manifestations and related mechanisms of COVID-19 caused by SARS-CoV-2 infection. Front Cell Neurosci. 2022;16:1006977. https://doi.org/10.3389/fncel.2022.1006977.
Faruque MRJ, Bikker FJ, Laine ML. Comparing SARS-CoV-2 viral load in human saliva to oropharyngeal swabs, nasopharyngeal swabs, and sputum: a systematic review and meta-analysis. Can J Infect Dis Med Microbiol. 2023;2023:5807370. https://doi.org/10.1155/2023/5807370.
Caixeta DC, Paranhos LR, Blumenberg C, Garcia-Júnior MA, Guevara-Vega M, Taveira EB, et al. Salivary SARS-CoV-2 RNA for diagnosis of COVID-19 patients: a systematic revisew and meta-analysis of diagnostic accuracy. Jpn Dent Sci Rev. 2023;59:219–38. https://doi.org/10.1016/j.jdsr.2023.06.004.
• Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271-80.e8. https://doi.org/10.1016/j.cell.2020.02.052. This was a hallmark study that was the first to show that SARS-CoV-2 uses a similar mechanism for cellular entry as SARS-CoV, with the spike protein primed by TMPRSS2 and then binding to the ACE2 receptor.
V’Kovski P, Kratzel A, Steiner S, Stalder H, Thiel V. Coronavirus biology and replication: implications for SARS-CoV-2. Nat Rev Microbiol. 2021;19(3):155–70. https://doi.org/10.1038/s41579-020-00468-6.
Zhang Q, Xiang R, Huo S, Zhou Y, Jiang S, Wang Q, et al. Molecular mechanism of interaction between SARS-CoV-2 and host cells and interventional therapy. Signal Transduct Target Ther. 2021;6(1):233. https://doi.org/10.1038/s41392-021-00653-w.
Xu J, Li Y, Gan F, Du Y, Yao Y. Salivary glands: potential reservoirs for COVID-19 asymptomatic infection. J Dent Res. 2020;99(8):989. https://doi.org/10.1177/0022034520918518.
Zhong M, Lin B, Pathak JL, Gao H, Young AJ, Wang X, et al. ACE2 and furin expressions in oral epithelial cells possibly facilitate COVID-19 infection via respiratory and fecal-oral routes. Front Med (Lausanne). 2020;7:580796. https://doi.org/10.3389/fmed.2020.580796.
• Sakaguchi W, Kubota N, Shimizu T, Saruta J, Fuchida S, Kawata A, et al. Existence of SARS-CoV-2 Entry Molecules in the Oral Cavity. Int J Mol Sci. 2020;21(17). https://doi.org/10.3390/ijms21176000. This study used patient tissues from various sites in the oral cavity to demonstrate the expression of SARS-CoV-2 entry receptor and protease ACE2 and TMPRSS, respectively.
Sawa Y, Ibaragi S, Okui T, Yamashita J, Ikebe T, Harada H. Expression of SARS-CoV-2 entry factors in human oral tissue. J Anat. 2021;238(6):1341–54. https://doi.org/10.1111/joa.13391.
•• Huang N, Pérez P, Kato T, Mikami Y, Okuda K, Gilmore RC, et al. SARS-CoV-2 infection of the oral cavity and saliva. Nat Med. 2021;27(5):892–903. https://doi.org/10.1038/s41591-021-01296-8. This paper provided single-cell atlases of both the salivary glands and gingival epithelium to demonstrate the specific cell types in which ACE2 was expressed, demonstrated SARS-CoV-2 replication in the tissues of the oral cavity, and was the first to demonstrate that saliva from infected individuals contains infectious virus.
Pascolo L, Zupin L, Melato M, Tricarico PM, Crovella S. TMPRSS2 and ACE2 coexpression in SARS-CoV-2 salivary glands infection. J Dent Res. 2020;99(10):1120–1. https://doi.org/10.1177/0022034520933589.
Song J, Li Y, Huang X, Chen Z, Li Y, Liu C, et al. Systematic analysis of ACE2 and TMPRSS2 expression in salivary glands reveals underlying transmission mechanism caused by SARS-CoV-2. J Med Virol. 2020;92(11):2556–66. https://doi.org/10.1002/jmv.26045.
•• Matuck BF, Dolhnikoff M, Duarte-Neto AN, Maia G, Gomes SC, Sendyk DI, et al. Salivary glands are a target for SARS-CoV-2: a source for saliva contamination. J Pathol. 2021;254(3):239–43. https://doi.org/10.1002/path.5679. A study in post-mortem biopsies that showed SARS-CoV-2 infection of the minor and major salivary glands by immunohistochemistry and also showed particles consistent in size and shape with Coronaviridae in the salivary glands by electron microscopy.
Zhu F, Zhong Y, Ji H, Ge R, Guo L, Song H, et al. ACE2 and TMPRSS2 in human saliva can adsorb to the oral mucosal epithelium. J Anat. 2022;240(2):398–409. https://doi.org/10.1111/joa.13560.
Fernandes Matuck B, Dolhnikoff M, Maia GVA, Isaac Sendyk D, Zarpellon A, Costa Gomes S, et al. Periodontal tissues are targets for Sars-Cov-2: a post-mortem study. J Oral Microbiol. 2020;13(1):1848135. https://doi.org/10.1080/20002297.2020.1848135.
Nakayama T, Lee IT, Jiang S, Matter MS, Yan CH, Overdevest JB, et al. Determinants of SARS-CoV-2 entry and replication in airway mucosal tissue and susceptibility in smokers. Cell Rep Med. 2021;2(10):100421. https://doi.org/10.1016/j.xcrm.2021.100421.
Marques BBF, Guimarães TC, Fischer RG, Tinoco JMM, Pires FR, Lima Junior JDC, et al. Morphological alterations in tongue epithelial cells infected by SARS-CoV-2: a case-control study. Oral Dis. 2022;28(Suppl 2):2417–22. https://doi.org/10.1111/odi.13988.
Fernández-Rojas MA, Ávila G, Romero-Valdovinos M, Plett-Torres T, Salazar AM, Sordo M, et al. Elevated levels of cytotoxicity, cytokines, and anti-SARS-CoV-2 antibodies in mild cases of COVID-19. Viral Immunol. 2023. https://doi.org/10.1089/vim.2023.0012.
Pinto TG, Alpire MES, Ribeiro DA. Cytogenetic biomonitoring in buccal mucosa cells of COVID-19 patients: preliminary findings. In Vivo. 2021;35(6):3495–9. https://doi.org/10.21873/invivo.12651.
•• To KK, Tsang OT, Yip CC, Chan KH, Wu TC, Chan JM, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71(15):841–3. https://doi.org/10.1093/cid/ciaa149. One of the first papers published during the pandemic that demonstrated the presence of SARS-CoV-2 genetic material in 91.7% of specimens from self-collected saliva samples from SARS-CoV-2 positive patients.
•• Stein SR, Ramelli SC, Grazioli A, Chung JY, Singh M, Yinda CK, et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature. 2022;612(7941):758–63. https://doi.org/10.1038/s41586-022-05542-y. This study conducted autopsies in 44 patients who passed following SARS-CoV-2 infection and demonstrated the persistent presence of SARS-CoV-2 genetic material weeks to months following infection, including in salivary gland tissues, revealing potential reservoirs of the virus.
Jimenez-Cauhe J, Ortega-Quijano D, de Perosanz-Lobo D, Burgos-Blasco P, Vañó-Galván S, Fernandez-Guarino M, et al. Enanthem in Patients With COVID-19 and Skin Rash. JAMA Dermatol. 2020;156(10):1134–6. https://doi.org/10.1001/jamadermatol.2020.2550.
Menni C, Valdes AM, Freidin MB, Ganesh S, Moustafa JSE-S, Visconti A, et al. Loss of smell and taste in combination with other symptoms is a strong predictor of COVID-19 infection. medRxiv. 2020:2020.04.05.20048421. https://doi.org/10.1101/2020.04.05.20048421.
Weir EM, Exten C, Gerkin RC, Munger SD, Hayes JE. Transient loss and recovery of oral chemesthesis, taste and smell with COVID-19: a small case-control series. Physiol Behav. 2023;271:114331. https://doi.org/10.1016/j.physbeh.2023.114331.
Fathi Y, Hoseini EG, Atoof F, Mottaghi R. Xerostomia (dry mouth) in patients with COVID-19: a case series. Future Virol. 2021. https://doi.org/10.2217/fvl-2020-0334.
Gebretsadik HG. An update on oral clinical courses among patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a clinical follow-up (a prospective prevalent cohort) study. PLoS ONE. 2022;17(10):e0275817. https://doi.org/10.1371/journal.pone.0275817.
Chern A, Famuyide AO, Moonis G, Lalwani AK. Sialadenitis: a possible early manifestation of COVID-19. Laryngoscope. 2020;130(11):2595–7. https://doi.org/10.1002/lary.29083.
Friedrich RE, Droste TL, Angerer F, Popa B, Koehnke R, Gosau M, et al. COVID-19-associated parotid gland abscess. In Vivo. 2022;36(3):1349–53. https://doi.org/10.21873/invivo.12837.
To KK, Tsang OT, Leung WS, Tam AR, Wu TC, Lung DC, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20(5):565–74. https://doi.org/10.1016/s1473-3099(20)30196-1.
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–9. https://doi.org/10.1038/s41586-020-2196-x.
Wyllie AL, Fournier J, Casanovas-Massana A, Campbell M, Tokuyama M, Vijayakumar P, et al. Saliva or nasopharyngeal swab specimens for detection of SARS-CoV-2. N Engl J Med. 2020;383(13):1283–6. https://doi.org/10.1056/NEJMc2016359.
Jacob AA, C CC, Mohan G, Mathew R, Matteethra GC, M A, et al. Evaluation of the efficacy of tongue swab and saliva as samples for testing COVID-19 infection in symptomatic cases in comparison with nasopharyngeal swab. J Med Microbiol. 2023;72(8). https://doi.org/10.1099/jmm.0.001743.
Azzi L, Carcano G, Gianfagna F, Grossi P, Gasperina DD, Genoni A, et al. Saliva is a reliable tool to detect SARS-CoV-2. J Infect. 2020;81(1):e45–50. https://doi.org/10.1016/j.jinf.2020.04.005.
Bordi L, Sberna G, Lalle E, Fabeni L, Mazzotta V, Lanini S, et al. Comparison of SARS-CoV-2 detection in nasopharyngeal swab and saliva samples from patients infected with Omicron variant. Int J Mol Sci. 2023;24(5). https://doi.org/10.3390/ijms24054847
Xu Q, Milanez-Almeida P, Martins AJ, Radtke AJ, Hoehn KB, Oguz C, et al. Adaptive immune responses to SARS-CoV-2 persist in the pharyngeal lymphoid tissue of children. Nat Immunol. 2023;24(1):186–99. https://doi.org/10.1038/s41590-022-01367-z.
• Lima TM, Martins RB, Miura CS, Souza MVO, Cassiano MHA, Rodrigues TS, et al. Tonsils are major sites of persistence of SARS-CoV-2 in children. Microbiol Spectr. 2023:e0134723. https://doi.org/10.1128/spectrum.01347-23. This recent study analyzed tonsillar tissue samples from 48 patients aged 3 to 11 years old and found that 27% of samples were positive for SARS-CoV-2, some even months after the child had been exposed to the virus, indicating a persistent infection in this tissue type.
Silva J, Lucas C, Sundaram M, Israelow B, Wong P, Klein J, et al. Saliva viral load is a dynamic unifying correlate of COVID-19 severity and mortality. medRxiv. 2021. https://doi.org/10.1101/2021.01.04.21249236.
Bansal M, Khatri M, Taneja V. Potential role of periodontal infection in respiratory diseases - a review. J Med Life. 2013;6(3):244–8.
Gupta S, Mohindra R, Chauhan PK, Singla V, Goyal K, Sahni V, et al. SARS-CoV-2 detection in gingival crevicular fluid. J Dent Res. 2021;100(2):187–93. https://doi.org/10.1177/0022034520970536.
Bumm CV, Folwaczny M. Infective endocarditis and oral health-a narrative review. Cardiovasc Diagn Ther. 2021;11(6):1403–15. https://doi.org/10.21037/cdt-20-908.
Lloyd-Jones G, Molayem S, Pontes CC, Chapple I. The COVID-19 pathway: a proposed oral-vascular-pulmonary route of SARS-CoV-2 infection and the importance of oral healthcare measures. J Oral Med Dent Res. 2021;2:1–25. https://doi.org/10.52793/JOMDR.2020.2(1)-13.
Marouf N, Cai W, Said KN, Daas H, Diab H, Chinta VR, et al. Association between periodontitis and severity of COVID-19 infection: a case-control study. J Clin Periodontol. 2021;48(4):483–91. https://doi.org/10.1111/jcpe.13435.
Gupta S, Mohindra R, Singla M, Khera S, Sahni V, Kanta P, et al. The clinical association between periodontitis and COVID-19. Clin Oral Investig. 2022;26(2):1361–74. https://doi.org/10.1007/s00784-021-04111-3.
Isho B, Abe KT, Zuo M, Jamal AJ, Rathod B, Wang JH, et al. Persistence of serum and saliva antibody responses to SARS-CoV-2 spike antigens in COVID-19 patients. Sci Immunol. 2020;5(52). https://doi.org/10.1126/sciimmunol.abe5511
Seaman WT, Keener O, Mei W, Mollan KR, Jones CD, Pettifor A, et al. Oral SARS-CoV-2 host responses predict the early COVID-19 disease course. Res Sq. 2023. https://doi.org/10.21203/rs.3.rs-3154698/v1. PubMed PMID: 37645853; PubMed Central PMCID: PMCPMC10462189 manufacturer of the N-antigen and anti-SARS-CoV-2 Spike RBD protein IgG/IgM LFA cartridges used in this study. No other authors declare any conflicts of interest.
Chellamuthu P, Angel AN, MacMullan MA, Denny N, Mades A, Santacruz M, et al. SARS-CoV-2 specific IgG antibodies persist over a 12-month period in oral mucosal fluid collected from previously infected individuals. Front Immunol. 2021;12:777858. https://doi.org/10.3389/fimmu.2021.777858.
Vilela ACS, Costa CA, Oliveira SA, Souza M, Fiaccadori FS, Leles CR, et al. Validity and reliability of immunochromatographic IgM/IgG rapid tests for COVID-19 salivary diagnosis. Oral Dis. 2022;28(Suppl 2):2465–73. https://doi.org/10.1111/odi.14059.
Wadhwa S, Yoon AJ, Kister K, Bolin I, Chintalapudi N, Besmer A, et al. Detection of SARS-CoV-2 IgG antibodies and inflammatory cytokines in saliva-a pilot study. J Oral Biol Craniofac Res. 2023;13(2):267–71. https://doi.org/10.1016/j.jobcr.2023.02.008.
Faustini SE, Cook A, Hill H, Al-Taei S, Heaney J, Efstathiou E, et al. Saliva antiviral antibody levels are detectable but correlate poorly with serum antibody levels following SARS-CoV-2 infection and/or vaccination. J Infect. 2023;87(4):328–35. https://doi.org/10.1016/j.jinf.2023.07.018.
Jang H, Choudhury S, Yu Y, Sievers BL, Gelbart T, Singh H, et al. Persistent immune and clotting dysfunction detected in saliva and blood plasma after COVID-19. Heliyon. 2023;9(7):e17958. https://doi.org/10.1016/j.heliyon.2023.e17958.
Saulle I, Garziano M, Cappelletti G, Limanaqi F, Strizzi S, Vanetti C, et al. Salivary miRNA profiles in COVID-19 patients with different disease severities. Int J Mol Sci. 2023;24(13). https://doi.org/10.3390/ijms241310992
Alqedari H, Altabtbaei K, Espinoza JL, Bin-Hasan S, Alghounaim M, Alawady A, et al. Host-microbiome associations in saliva predict COVID-19 severity. bioRxiv. 2023. https://doi.org/10.1101/2023.05.02.539155
Alfaifi A, Sultan AS, Montelongo-Jauregui D, Meiller TF, Jabra-Rizk MA. Long-term post-COVID-19 associated oral inflammatory sequelae. Front Cell Infect Microbiol. 2022;12:831744. https://doi.org/10.3389/fcimb.2022.831744.
Armstrong AJS, Horton DB, Andrews T, Greenberg P, Roy J, Gennaro ML, et al. Saliva microbiome in relation to SARS-CoV-2 infection in a prospective cohort of healthy US adults. EBioMedicine. 2023;94:104731. https://doi.org/10.1016/j.ebiom.2023.104731.
Sekaran K, Varghese RP, Doss CG, Alsamman AM, Zayed H, El Allali A. Airway and Oral microbiome profiling of SARS-CoV-2 infected asthma and non-asthma cases revealing alterations-a pulmonary microbial investigation. PLoS One. 2023;18(8):e0289891. https://doi.org/10.1371/journal.pone.0289891.
Miller EH, Annavajhala MK, Chong AM, Park H, Nobel YR, Soroush A, et al. Oral microbiome alterations and SARS-CoV-2 saliva viral load in patients with COVID-19. Microbiol Spectr. 2021;9(2):e0005521. https://doi.org/10.1128/Spectrum.00055-21.
Apostolou E, Rizwan M, Moustardas P, Sjögren P, Bertilson BC, Bragée B, et al. Saliva antibody-fingerprint of reactivated latent viruses after mild/asymptomatic COVID-19 is unique in patients with myalgic-encephalomyelitis/chronic fatigue syndrome. Front Immunol. 2022;13:949787. https://doi.org/10.3389/fimmu.2022.949787.
Hannestad U, Apostolou E, Sjögren P, Bragée B, Polo O, Bertilson BC, et al. Post-COVID sequelae effect in chronic fatigue syndrome: SARS-CoV-2 triggers latent adenovirus in the oral mucosa. Front Med (Lausanne). 2023;10:1208181. https://doi.org/10.3389/fmed.2023.1208181.
Bowe B, Xie Y, Al-Aly Z. Postacute sequelae of COVID-19 at 2 years. Nat Med. 2023;29(9):2347–57. https://doi.org/10.1038/s41591-023-02521-2.
Gherlone EF, Polizzi E, Tetè G, De Lorenzo R, Magnaghi C, Rovere Querini P, et al. Frequent and persistent salivary gland ectasia and oral disease after COVID-19. J Dent Res. 2021;100(5):464–71. https://doi.org/10.1177/0022034521997112.
• Shen Y, Voigt A, Goranova L, Abed MA, Kleiner DE, Maldonado JO, et al. Evidence of a Sjögren’s disease-like phenotype following COVID-19 in mice and human. JCI Insight. 2023. https://doi.org/10.1172/jci.insight.166540. This recent paper used a mouse model to demonstrate a decrease in salivary flow, increase in production of auto-antibodies, and increase in inflammation in the salivary glands following infections with SARS-CoV-2, while in convalescent patients, there was a slight increase in serum auto-antibodies as well as histological signs of salivary gland pathology.
Acknowledgements
The supporting evidence (e.g., microscopic images) depicted in figures in this review (e.g., microscopic data) were published in Huang et al., Nature Medicine, 2021 (15). For the purposes of this review, the authors used additional unpublished original microscopic images and sections as supporting data for the new figures. The authors would like to thank the NIH COVID-19 Autopsy Consortium COVID-19 for access to affected tissues and data which were first published in Huang et al. (2021).
Funding
BMW has Cooperative Research Award and Development Agreements [CRADA] from Pfizer, Inc., and Mitobridge, Inc., (a subsidiary of Astellas Pharma, Inc.). The work presented is unrelated to the research funded under these agreements. This research was principally supported through research awards to BMW from the Division of Intramural Research (DIR) Program of the National Institute of Dental and Craniofacial Research of the National Institutes of Health (NIH/NIDCR ZIA: DE000704). NA is funded as a Dental Clinical Research Fellow through the NIH/NIDCR Office of the Clinical Director.
Author information
Authors and Affiliations
Contributions
NA and BMW contributed to the conception, drafting, and critical revision of the manuscript. PP contributed to the data acquisition for the images presented in the figures. BM and KMB contributed to the editing and critical revision of the manuscript. All authors gave approval for the final manuscript and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
For the images shown in Fig. 1, subject’s biopsies were obtained under NIH IRB-approved protocol: 15-D-0051-Characterization of Diseases With Salivary Gland Involvement [PI-Warner, NCT02327884]. For the images shown in Fig. 2, samples were obtained as part of the NIH COVID-19 Autopsy Consortium. For the images shown in Fig. 3, subject’s biopsies were obtained under NIH IRB-approved protocol NCT04348240: Transmissibility and Viral Load of SARS-CoV-2 Through Oral Secretions (PI-Warner). The NIH single institutional review board (IRB) conducts ethical reviews for human research studies as required by Department of Health and Human Services regulations for the Protection of Human Subjects. All patients seen at the author’s (B.M.W.) institute (NIH/NIDCR) reported herein provided informed consent prior to participation in IRB-approved research protocols (NIH IRB: 20-D-0094, NCT04348240; NIH IRB: 15-D-0051, NCT02327884). In autopsy tissues, consent for autopsies (reported previously in Huang & Perez, et al., 2021) of COVID-19 victims was coordinated by the NIH COVID-19 Autopsy Consortium and obtained from family members. Autopsies were performed in the National Cancer Institute (NCI) Laboratory of Pathology, and tissues were recovered per family wishes for histopathological and other downstream analyses.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Atyeo, N., Perez, P., Matuck, B. et al. The Mouth as a Site of SARS-CoV-2 Infection. Curr Oral Health Rep 11, 167–176 (2024). https://doi.org/10.1007/s40496-024-00367-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-024-00367-2