Abstract
Purpose of Review
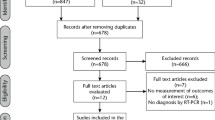
This systematic review addresses the question: Is the oral cavity a reservoir of SARS-CoV-2 in participants who tested positive for viral RNA in nasopharyngeal and oropharyngeal samples? Four databases and a complementary search on the reference list of included studies were consulted. Paired reviewers independently searched the literature, extracted data, and evaluated the risk of bias (Joanna Briggs Institute).
Recent Findings
A total of 3173 references were identified, and after a 2-phase selection, 24 studies were included. In total, 10 diagnostic test accuracy and 14 cross-sectional studies determined the presence of SARS-CoV-2 using real-time quantitative polymerase chain reaction (RT-qPCR) incorporating experimental and control samples. It was shown that saliva, gingival crevicular fluid, dental plaque, and gingival tissue harbored viral RNA. A high level of heterogenicity between studies was observed. The risk of bias analysis raised major concerns regarding the lack of clear criteria for inclusion, with most studies being of moderate to low quality. SARS-CoV-2 RNA is present in oral cavity samples, reinforcing the contribution of the oral cavity as a potential route of entry for infection and may offer a practical and affordable point-of-care platform for COVID-19 diagnosis. Furthermore, comprehending the oral cavity as a reservoir of SARS-CoV-2 may provide insight into its persistence and transmissibility.
Summary
The oral cavity can serve as a reservoir of SARS-CoV-2. Awareness of the significance of the oral cavity as a SARS-CoV-2 viral reservoir may help to shape COVID-19 containment measures and further potential therapeutic initiatives.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
WHO Director: General’s opening remarks at the media briefing on COVID-19 - March.11/2020. In: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 11 Dec 2021.
Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020. https://doi.org/10.1016/S0140-6736(20)30260-9.
WHO Coronavirus (COVID-19) Dasboard with vaccination data. In: https://covid19.who.int. Accessed 7 Feb 2024.
Kung S, Doppen M, Black M, Braithwaite I, Kearns C, Weatherall M, Beasley R, Kearns N. Underestimation of COVID-19 mortality during the pandemic. ERJ Open Res. 2021. https://doi.org/10.1183/23120541.00766-2020.
Cheng VC-C, Wong S-C, Chuang VW-M, So SY-C, Chen JH-K, Sridhar S, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. 2020;81(1):107–14. https://doi.org/10.1016/j.jinf.2020.04.024.
Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2022. https://doi.org/10.1016/j.ijid.2021.11.009.
Berger I, Schaffitzel C. The SARS-CoV-2 spike protein: balancing stability and infectivity. Cell Res. 2020. https://doi.org/10.1038/S41422-020-00430-4.
Örd M, Faustova I, Loog M. The sequence at Spike S1/S2 site enables cleavage by furin and phospho-regulation in SARS-CoV2 but not in SARS-CoV1 or MERS-CoV. Sci Rep. 2020. https://doi.org/10.1038/S41598-020-74101-0.
Lloyd-Jones G, Molayem S, Pontes CC, 2021. Chapple I The COVID-19 pathway: a proposed oral-vascular-pulmonary route of SARS-CoV-2 infection and the importance of oral healthcare measures. J Oral Med Dent Res. 2(1) 1–25. https://doi.org/10.52793/JOMDR.2020.2(1)-13
Sharma A, Ahmad Farouk I, Lal SK. COVID-19: a review on the novel coronavirus disease evolution, transmission, detection, control and prevention. Viruses. 2021. https://doi.org/10.3390/v13020202.
Kritika S, Mahalaxmi S, Srinivasan N, Krithikadatta J. Deciphering the role of saliva in COVID 19: a global cross-sectional study on the knowledge, awareness and perception among dentists. BMC Oral Health. 2023. https://doi.org/10.1186/s12903-023-03152-2.
Moher D, Liberati A, Tetzlaff J, Altman DG & PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009; https://doi.org/10.1371/journal.pmed.1000097
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016. https://doi.org/10.1186/s13643-016-0384-4.
Abasiyanik MF, Flood B, Lin J, Ozcan S, Rouhani SJ, Pyzer A, Trujillo J, Zhen C, Wu P, Jumic S, Wang A, Gajewski TF, Wang P, Hartley M, Ameti B, Niemiec R, Fernando M, Aydogan B, Bethel C, Matushek S, Izumchenko E Sensitive detection and quantification of SARS-CoV-2 in saliva. medRxiv. 2020; https://doi.org/10.1101/2020.12.04.20241059
Al Suwaidi H, Senok A, Varghese R, Deesi Z, Khansaheb H, Pokasirakath S, Chacko B, Abufara I, Loney T, Alsheikh-Ali A. Saliva for molecular detection of SARS-CoV-2 in school-age children. Clin Microbiol Infect. 2021;27(9):1330–5. https://doi.org/10.1016/j.cmi.2021.02.009.
Andrade LM, Lau-Junior W, Oliveira RAM, Rodrigues ES, Santos EV, Borges JS, Evaristo M, Marques AA, Baccarin AD, Milhomens J, Garibaldi PMM, Ferreira NN, Moraes GR, Macedo LD, Calado RT, Borges M, Sabbaga MCE, Vessoni SCS, Covas DT, Kashima S. Uso da saliva como amostra biológica no diagnóstico da COVID-19 por RT-PCR. Hematol Transfus Cell Ther. 2022;44:S681-2. https://doi.org/10.1016/j.htct.2022.09.1171.
Barat B, Das S, De Giorgi V, Henderson DK, Kopka S, Lau AF, Miller T, Moriarty T, Palmore TN, Sawney S, Spalding C, Tanjutco P, Wortmann G, Zelazny AM, Frank KM. Pooled saliva specimens for SARS-CoV-2 testing. J Clin Microbiol. 2021. https://doi.org/10.1128/JCM.02486-20.
Bhattacharya D, Parai D, Rout UK, Dash P, Nanda RR, Dash GC, Kanungo S, Palo SK, Giri S, Choudhary HR, Kshatri JS, Turuk J, Mishra BK, Lenka RK, Dash S, Pati S. Saliva for diagnosis of SARS-CoV-2: first report from India. J Med Virol. 2021. https://doi.org/10.1002/jmv.26719.
Congrave-Wilson Z, Lee Y, Jumarang J, Perez S, Bender JM, Bard JD, Pannaraj PS. Change in saliva RT-PCR sensitivity over the course of SARS-CoV-2 infection. JAMA. 2021. https://doi.org/10.1001/jama.2021.13967.
Connor MC, Copeland M, Curran T. Investigation of saliva, tongue swabs and buccal swabs as alternative specimen types to nasopharyngeal swabs for SARS-CoV-2 testing. J Clin Virol. 2022. https://doi.org/10.1016/j.jcv.2021.105053.
Cornette M, Decaesteker B, Martens GA, Vandecandelaere P, Jonckheere S. From Delta to Omicron SARS-CoV-2 variant: switch to saliva sampling for higher detection rate. J Clin Virol Plus. 2022. https://doi.org/10.1016/j.jcvp.2022.100090.
Fernandes PADC, Ferreira FADC, Morais OM, Ramos CMT, Fernandes ÉMR, Rocha SAAD, Rocha RJA, Monteiro VJP, Vilar PSG, Romão AM, Alves MRA. Performance of saliva as a specimen to detect SARS-CoV-2. J Clin Virol. 2021. https://doi.org/10.1016/j.jcv.2021.104913.
Poukka E, Mäkelä H, Hagberg L, Vo T, Nohynek H, Ikonen N, Liitsola K, Helve O, Savolainen-Kopra C, Dub T. Detection of SARS-CoV-2 infection in gargle, spit, and sputum specimens. Microbiol Spectr. 2021. https://doi.org/10.1128/Spectrum.00035-21.
Abdollahi A, Salarvand S, Ghalehtaki R, Jafarzadeh B, Beigmohammadi MT, Ghiasvand F, Shakoori A, Khoshnevis H, Arabzadeh M, Nateghi S, Mehrtash V. The role of saliva PCR assay in the diagnosis of COVID-19. J Infect Dev Ctries. 2022. https://doi.org/10.3855/jidc.15239.
Alkhateeb KJ, Cahill MN, Ross AS, Arnold FW, Snyder JW. The reliability of saliva for the detection of SARS-CoV-2 in symptomatic and asymptomatic patients: insights on the diagnostic performance and utility for COVID-19 screening. Diagn Microbiol Infect Dis. 2021. https://doi.org/10.1016/j.diagmicrobio.2021.115450.
Altawalah H, AlHuraish F, Alkandari WA, Ezzikouri S. Saliva specimens for detection of severe acute respiratory syndrome coronavirus 2 in Kuwait: a cross-sectional study. J Clin Virol. 2020. https://doi.org/10.1016/j.jcv.2020.104652.
Aydin S, Benk IG, Geckil AA. May viral load detected in saliva in the early stages of infection be a prognostic indicator in COVID-19 patients? J Virol Methods. 2021. https://doi.org/10.1016/j.jviromet.2021.114198.
Azzi L, Carcano G, Gianfagna F, Grossi P, Gasperina DD, Genoni A, Fasano M, Sessa F, Tettamanti L, Carinci F, Maurino V, Rossi A, Tagliabue A, Baj A. Saliva is a reliable tool to detect SARS-CoV-2. J Infect. 2020. https://doi.org/10.1016/j.jinf.2020.04.005.
Chen L, Zhao J, Peng J, Li X, Deng X, Geng Z, Shen Z, Guo F, Zhang Q, Jin Y, Wang L, Wang S. Detection of SARS-CoV-2 in saliva and characterization of oral symptoms in COVID-19 patients. Cell Prolif. 2020;53(12):12923. https://doi.org/10.1111/cpr.12923.
Chua GT, Wong JSC, To KKW, Lam ICS, Yau FYS, Chan WH, Ho PPK, Duque JSR, Yip CCY, Ng ACK, Wong WHS, Kwong JHY, Leung KFS, Wan PT, Lam K, Wong ICK, Kwok J, Ho MHK, Chan GCF, Lau YL, Kwan MYW. Saliva viral load better correlates with clinical and immunological profiles in children with coronavirus disease 2019. Emerg Microbes Infect. 2020. https://doi.org/10.1080/22221751.2021.1878937.
Gupta S, Mohindra R, Chauhan PK, Singla V, Goyal K, Sahni V, Gaur R, Verma DK, Ghosh A, Soni RK, Suri V, Bhalla A, Singh MP. SARS-CoV-2 Detection in gingival crevicular fluid. J Den Res. 2020. https://doi.org/10.1177/0022034520970536.
Gomes SC, da Fonseca JG, Miller LM, Manenti L, Angst PDM, Lamers ML, Brum IS, Nunes LN. SARS-CoV-2 RNA in dental biofilms: supragingival and subgingival findings from inpatients in a COVID-19 intensive care unit. J Periodontol. 2022. https://doi.org/10.1002/JPER.21-0623.
•• Gomes SC, Fachin S, da Fonseca JG, Angst PDM, Lamers ML, da Silva ISB, & Nunes LN Dental biofilm of symptomatic COVID-19 patients harbours SARS-CoV-2. J Clin Periodontol. 2021; https://doi.org/10.1111/jcpe.13471. This evidence is crucial because it supports the hypothesis that the oral cavity can serve as a source of viral infection. By addressing the oral route of transmission, public health initiatives can more comprehensively tackle the multifaceted nature of SARS‐CoV‐2 transmission.
Hanege FM, Kocoglu E, Kalcioglu MT, Celik S, Cag Y, Esen F, Bayindir E, Pence S, Alp Mese E, Agalar C. SARS-CoV-2 Presence in the saliva, tears, and cerumen of COVID-19 patients. Laryngoscope. 2021. https://doi.org/10.1002/lary.29218.
Matuck BF, Dolhnikoff M, Duarte-Neto AN, Maia G, Gomes SC, Sendyk DI, Zarpellon A, de Andrade NP, Monteiro RA, Pinho JRR, Gomes-Gouvêa MS, Souza SC, Kanamura C, Mauad T, Saldiva PHN, Braz-Silva PH, Caldini EG, da Silva LFF. Salivary glands are a target for SARS-CoV-2: a source for saliva contamination. J Pathol. 2021. https://doi.org/10.1002/path.5679.
Miyake S, Ashikari K, Kato S, Takatsu T, Kuwashima H, Kaneko H, Nagai K, Watari I, Sato T, Yamaoka Y, Yamamoto T. Severe acute respiratory syndrome coronavirus 2 prevalence in saliva and gastric and intestinal fluid in patients undergoing gastrointestinal endoscopy in coronavirus disease 2019 endemic areas: prospective cross-sectional study in Japan. Dig Endosc. 2022; https://doi.org/10.1111/den.13945
Perret P, Cecilia Abarca, Katia Solari, Sandra Aguilera, Pablo García-Huidobro, Diego Olivares, Felipe Palma, Carlos Contreras, María Ana, Martínez-Valdebenito Constanza, Ferrés Marcela. Detección del SARS-CoV-2 mediante RT-qPCR utilizando saliva en pacientes ambulatorios con estudio de COVID-19. Rev Chil Infect. 2022;39(4):372–81. https://doi.org/10.4067/s0716-10182022000400372.
Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, Bleicker T, Brünink S, Schneider J, Schmidt ML, Mulders DG, Haagmans BL, van der Veer B, van den Brink S, Wijsman L, Goderski G, Romette JL, Ellis J, Zambon M, Peiris M, Drosten C. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045. https://doi.org/10.2807/1560-7917.ES.2020.25.3.2000045.
Azzi L, Maurino V, Baj A, Dani M, d’Aiuto A, Fasano M, Lualdi M, Sessa F, Alberio T. Diagnostic salivary tests for SARS-CoV-2. J Dent Res. 2021;100(2):115–23. https://doi.org/10.1177/0022034520969670.
Lee RA, Herigon JC, Benedetti A, Pollock NR, Denkinger CM. Performance of saliva, oropharyngeal swabs, and nasal swabs for SARS-CoV-2 molecular detection: a systematic review and meta-analysis. J Clin Microbiol. 2021;59(5):10–128. https://doi.org/10.1128/JCM.02881-20.
Li Y, Liang M, Gao L, Ayaz Ahmed M, Uy JP, Cheng C, et al. Face masks to prevent transmission of COVID-19: a systematic review and meta-analysis. Am J Infect Control. 2021. https://doi.org/10.1016/J.AJIC.2020.12.007.
Nagura-Ikeda M, Imai K, Tabata S, Miyoshi K, Murahara N, Mizuno T, Horiuchi M, Kato K, Imoto Y, Iwata M, Mimura S, Ito T, Tamura K, Kato Y. Clinical evaluation of self-collected saliva by quantitative reverse transcription-PCR (RT-qPCR), direct RT-qPCR, reverse transcription-loop-mediated isothermal amplification, and a rapid antigen test to diagnose COVID-19. J Clin Microbiol. 2020. https://doi.org/10.1128/JCM.01438-20.
Sri Santosh T, Parmar R, Anand H, Srikanth K, Saritha M. A review of salivary diagnostics and its potential implication in detection of COVID-19. Cureus. 2020. https://doi.org/10.7759/CUREUS.7708.
Fernandes LL, Pacheco VB, Borges L, Athwal HK, de Paula EF, Bezinelli L, Correa L, Jimenez M, Dame-Teixeira N, Lombaert IMA, Heller D. Saliva in the diagnosis of COVID-19: a review and new research directions. J Dent Res. 2020. https://doi.org/10.1177/0022034520960070.
Subbarao KC, Nattuthurai GS, Sundararajan SK, Sujith I, Joseph J, Syedshah YP. Gingival crevicular fluid: an overview. J Pharm Bioallied Sci. 2019;11:135. https://doi.org/10.4103/JPBS.JPBS_56_19.
Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD, van der Voort PH, Mulder DJ, van Goor H. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol. 2020;251(3):228–48. https://doi.org/10.1002/path.5471.
Essalmani R, Jain J, Susan-Resiga D, Andréo U, Evagelidis A, Derbali RM, Huynh DN, Dallaire F, Laporte M, Delpal A, Sutto-Ortiz P, Coutard B, Mapa C, Wilcoxen K, Decroly E, Nq Pham T, Cohen ÉA, Seidah NG. Distinctive roles of furin and TMPRSS2 in SARS-CoV-2 infectivity. J Virol. 2022. https://doi.org/10.1128/jvi.00128-22.
Huang N, Pérez P, Kato T, et al. SARS-CoV-2 infection of the oral cavity and saliva. Nat Med. 2021. https://doi.org/10.1038/s41591-021-01296-8.
González-Olmo MJ, Delgado-Ramos B, Ruiz-Guillén A, Romero-Maroto M, Carrillo-Díaz M. Oral hygiene habits and possible transmission of COVID-19 among cohabitants. BMC Oral Health. 2020. https://doi.org/10.1186/s12903-020-01274-5.
Author information
Authors and Affiliations
Contributions
SCG was the study coordinator and took part in all stages of the manuscript, except for the selection of studies. FVB and LM did this and helped write the manuscript. LX helped with data extraction. All authors worked editing the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gomes, S.C., Miller, L.M., Xavier, L. et al. The Mouth as a Reservoir of SARS-CoV-2. Curr Oral Health Rep 11, 144–166 (2024). https://doi.org/10.1007/s40496-024-00369-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-024-00369-0