Abstract
Introduction
Biomarker testing is increasingly crucial for patients with early-stage non-small cell lung cancer (eNSCLC). We explored biomarker test utilization and subsequent treatment in eNSCLC patients in the real-world setting.
Methods
Using COTA’s oncology database, this retrospective observational study included adult patients ≥ 18 years old diagnosed with eNSCLC (disease stage 0–IIIA) between January 1, 2011 and December 31, 2021. Date of first eNSCLC diagnosis was the study index date. We reported testing rates by index year for patients who received any biomarker test within 6 months of eNSCLC diagnosis and by each molecular marker. We also evaluated treatments received among patients receiving the five most common biomarker tests.
Results
Among the 1031 eNSCLC patients included in the analysis, 764 (74.1%) received ≥ 1 biomarker test within 6 months of eNSCLC diagnosis. Overall, epidermal growth factor receptor (EGFR; 64%), anaplastic lymphoma kinase (ALK; 60%), programmed death receptor ligand 1 (PD-L1; 48%), ROS proto-oncogene 1 (ROS1; 46%), B-Raf proto-oncogene (40%), mesenchymal epithelial transition factor receptor (35%), Kirsten rat sarcoma viral oncogene (29%), RET proto-oncogene (22%), human epidermal growth factor receptor 2 (21%), and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (20%) were the 10 most frequently tested biomarkers. The proportion of patients undergoing biomarker testing rose from 55.3% in 2011 to 88.1% in 2021. The most common testing methods were Sanger sequencing for EGFR (244, 37%), FISH (fluorescence in situ hybridization) for ALK (464, 75%) and ROS1 (357, 76%), immunohistochemical assay for PD-L1 (450, 90%), and next-generation sequencing testing for other biomarkers. Almost all the 763 patients who received the five most common biomarker tests had a test before the initiation of a systemic treatment.
Conclusion
This study suggests a high biomarker testing rate among patients with eNSCLC in the US, with testing rates for various biomarkers increasing over the past decade, indicating a continuous trend towards the personalization of treatment decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The use of biomarker tests to guide treatment in patients with early-stage non-small cell lung cancer (eNSCLC) is not well understood in the real-world setting. |
This study fills a gap in knowledge by examining the real-world biomarker test utilization and subsequent treatment over 11 years in a national sample of adult patients with eNSCLC. |
What was learned from the study? |
This study suggests a high biomarker testing rate, with various biomarker testing rates increasing over the last decade in patients with eNSCLC in the US. |
In patients who received the five most commonly used biomarker tests, almost all received a test before the initiation of a systemic treatment. |
With the rapidly evolving treatment landscape and testing recommendations for eNSCLC, future research is needed to understand whether biomarker testing has improved optimal treatment decision making and long-term survival outcomes for patients with eNSCLC. |
Introduction
Lung cancer is the second most common cancer and the leading cause of cancer death in the United States (US) [1]. Approximately 236,740 new cases of lung cancer and 130,180 lung cancer-related deaths are estimated to have occurred by the end of 2022 [1]. Lung cancer is a heterogeneous disease [2,3,4], and 85% of patients diagnosed with lung cancer have non-small cell lung cancer (NSCLC) [2]. The main subtypes of NSCLC are adenocarcinoma (40%), squamous cell carcinoma (30%), and large cell carcinoma (10–15%) [5]. Approximately half of US patients with NSCLC are diagnosed at an advanced, metastatic stage (aNSCLC; stage IIIB or IV) [6]. The remaining half are diagnosed at an early, non-metastatic stage (eNSCLC; stage I, II, or IIIA) [6]. With an aging population and the introduction of low-dose computed tomography screenings for high-risk individuals, the number of patients diagnosed with eNSCLC is likely to increase [6,7,8].
The discovery of oncogenic driver mutations in NSCLC, which can be targeted by small molecule inhibitors, and the development of immunotherapies have transformed the treatment landscape for patients with NSCLC [9]. The treatment for NSCLC is becoming increasingly biomarker driven, with targeted therapies requiring testing using companion molecular diagnostics [10]. In fact, practical guidelines, such as the Clinical Practice Guidelines in Oncology (NCCN), the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology, recommend that all patients with aNSCLC should undergo, at a minimum, testing for the most prevalent biomarkers, including epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK), ROS proto-oncogene 1 (ROS1), B-Raf proto-oncogene (BRAF), and programmed death receptor ligand 1 (PD-L1) [11, 12].
Biomarker testing is also crucial for patients with eNSCLC [11]; for example, some clinical trials have reported survival benefits associated with adjuvant chemotherapy in eNSCLC [13, 14]. Information collected from biomarkers could help with identifying patients with eNSCLC who are most likely to benefit from adjuvant therapy [8, 15,16,17].
A growing number of biomarker-based treatments, along with companion diagnostic devices, tailored to patients with eNSCLC are now under development or have been approved by the US Food and Drug Administration (FDA) [8, 18]. For example, the 2022 update to the NCCN Guidelines recommended osimertinib as an option for adjuvant therapy in patients with resectable stage IIB–IIIA or high-risk stage IB–IIA NSCLC harboring EGFR mutations who have received previous adjuvant chemotherapy, or are ineligible to receive platinum-based chemotherapy [11, 19], based on the results of the ADAURA trial which showed an unprecedented disease-free survival benefit [16, 17]. In addition, the VENTANA PD-L1 (SP263) Assay (Ventana Medical Systems, Inc., a member of the Roche Group) was recently approved as a companion diagnostic device for adjuvant treatment with atezolizumab (Tecentriq, Genentech, Inc.) in patients with stage II to IIIA NSCLC whose tumors have PD-L1 expression on ≥ 1% of tumor cells [18].
However, little is known about how biomarker tests are conducted and used to guide treatments in patients with eNSCLC in the real-world setting. In this exploratory study, we aimed to understand the real-world utilization of biomarker tests and the subsequent treatment among patients newly diagnosed with eNSCLC. We also investigated the timing of biomarker testing and its relation to initiation of systemic treatment.
Methods
Study Design and Data Source
This retrospective, observational cohort study used COTA’s Real World Evidence (RWE) database, an electronic health records (EHR)-derived, de-identified oncology database [20]. The database includes data from 1.7 million patient records from over 1500 oncologists, of whom approximately 50% are from academic settings and 50% from community medical centers, representing diverse treatment settings. These treatment settings include academic, for-profit, community sites, and hospital systems in most of the US, with concentrations in the Northeast, Southeast, and South-Central regions of the US. Some examples of cancer centers include Miami Cancer Institute, Hackensack Meridian Health, John Theurer Cancer Center, Regional Cancer Care Associates, and Medstar Health.
COTA datasets contain individual patient data from the time of initial cancer diagnosis through to the most recent documentation in the EHR. Other available information includes patient demographics, cancer diagnosis, comorbidity, performance status, tumor histology, laboratory data, biomarker test methods and results, treatment information, and adverse events. All data available within the EHR at the time of abstraction were included in the RWE dataset. Where patients did not receive all of their care at a singular primary site, COTA reviewed and collected data from all available outside records that were scanned into the EHR and/or detailed by the treating physician. Patients who did not have sufficient documentation or had significant gaps in their patient journey within the EHR were excluded.
Compliance with Ethics Guidelines
All study data were fully compliant with US patient confidentiality requirements, including the Health Insurance Portability and Accountability Act (HIPAA) of 1996. The study used only de-identified patient records and, therefore, was exempted from institutional review board approval. Informed consent was not required, as this was not an interventional study, and routinely collected, anonymized data were used. This study complied with all relevant national regulations and was performed in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonization Guidelines on Good Clinical Practice. Full permission was received by COTA to access the study database.
Study Sample Selection
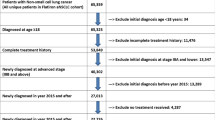
The study population included adult patients ≥ 18 years old with eNSCLC. A total of 1200 adult patients with a diagnosis of eNSCLC between January 1, 2000 and December 31, 2021 were initially identified by COTA, using the following patient identification and extraction criteria. Patients with a diagnosis of lung cancer were first identified based on having at least one international Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code or ICD-10-CM code for lung cancer. Medical abstractors then manually confirmed the diagnosis in the EHR and completed the full patient record extraction. Patients with NSCLC were then identified based on the histology codes for NSCLC. eNSCLC patients were included in the study cohort based on having the disease at stage 0–IIIA. Patients were excluded if they met the following criteria: (1) they were < 18 years of age at the time of diagnosis; (2) they did not have the malignancy of interest (i.e., NSCLC); (3) they had no date of diagnosis in the EHR; (4) they had no clinician note available; (5) they were not evaluated at the accessible provider site for the malignancy of interest; or (6) they had concurrent primary malignancies. In our analyses, we further excluded patients who: (1) had a diagnosis of eNSCLC before 2011; (2) had an unspecified cancer stage; and (3) received biomarker testing prior to having a NSCLC diagnosis.
Additionally, for the study analysis, we limited the biomarker test utilization to within 6 months or 182 days of the eNSCLC diagnosis date. The 6-month cut-off date was specified because the study clinical expert advised that the majority of patients with eNSCLC are typically treated within 6 months of diagnosis. Patients were further required to have at least one medical activity, defined as having at least one office visit or treatment, within 182 days after eNSCLC diagnosis. To ensure that patients were actively receiving care within the COTA Health Database, patients were excluded if they had no evidence of an interaction with the healthcare system within 90 days of diagnosis or a survival of less than 30 days after the diagnosis date. Patients were also excluded if they enrolled in clinical trials within 182 days of eNSCLC diagnosis. A total of 1031 patients with eNSCLC were included in this analysis after applying these study eligibility criteria (Table 1).
Three-month and 9-month cut-off dates were used for sensitivity analysis. Similar study sample sizes were found. The index date was the date of the first eNSCLC diagnosis. Patients were followed until death, the last medical activity date, or end of the study period, whichever occurred first.
Study Measures
Patients’ demographic and clinical characteristics were measured on or around the index date, including age at diagnosis, sex, race (e.g., white, African American, Asian, and other), ethnicity (Hispanic vs. non-Hispanic), cancer stage, Eastern Cooperative Oncology Group Performance Status Scale [21], personal history of cancer, history of tobacco usage, diagnosis method (i.e., biopsy, clinical, cytology, excisional biopsy, fine needle aspirate, surgical resection, other), and year of initial diagnosis.
The study database recorded details of the patients’ biomarker testing, such as the name of the molecular biomarker, test results (positive vs. negative), testing methods, specimen type, as well as dates of test collection and reporting. The specific testing methods included polymerase chain reaction, fluorescence in situ hybridization (FISH), immunohistochemistry (IHC), mutation-specific IHC, next-generation sequencing (NGS), ribonucleic acid (RNA) sequencing, Sanger sequencing, and unspecified. The specimen types included blood, tumor, and unspecified. The biomarker turnaround time was calculated as the difference between the date the specimen was collected in the laboratory and the date of the test result available to the provider.
Patients’ treatment information included surgery, radiation therapy, and systemic treatment regimens. We further categorized systemic treatment regimens into the following five categories: chemotherapies only, immunotherapies only, targeted therapies only, immunotherapy and chemotherapy (immuno-chemo), and targeted therapy and chemotherapy (targeted-chemo).
Statistical Analysis
Descriptive statistics were reported for the study, with the mean (median, minimum, maximum) used for continuous variables and the number (n) and proportion for categoric variables. The chi-squared test was used for categorical variables, and the t-test was performed for continuous variables to obtain p values.
To understand the biomarker test utilization over time, owing to the fact that biomarker testing rates were expected to change over the study time period between January 1, 2011 and December 31, 2021, we reported the biomarker testing rate by year of index diagnosis date for patients who received any biomarker test within 6 months of their eNSCLC diagnosis and by each molecular marker. We further evaluated the distribution of cancer stages, methods of testing, and specimen types among patients who received at least one biomarker test within 6 months of their eNSCLC diagnosis.
For treatment utilization, we reported the lines of therapy patients received within 1 year of their eNSCLC diagnosis. Additionally, in a subgroup of patients who received the five most commonly used biomarker tests, we reported the time from initial diagnosis to biomarker testing and the time from biomarker testing to first-line systemic treatment initiation. We further stratified our analysis by treatment type (i.e., chemotherapy vs. non-chemotherapy). All analyses were conducted using R version 4.2.0.
Results
Patient Demographic and Clinical Characteristics
Of the 1031 eNSCLC patients included in the study, the majority were aged 65 years and older (65–74 years: 39.4%; 75–84 years: 26.4%; 85+ years: 5.1%), female (52.9%), white (91.8%), and had a history of tobacco use (81.4%) (Table 2).
Most patients (n = 764, 74.1%) received at least one biomarker test within 6 months of their eNSCLC diagnosis, and a higher percentage of these patients were female, Hispanic or Latino, did not have a history of tobacco use, and received their cancer diagnosis after a surgical resection (p < 0.05) as compared with those who did not receive any biomarker test (n = 267, 25.9%).
Biomarker Test Utilization Over Time and Testing Methods
Overall, the 10 most frequently tested biomarkers were EGFR (64%), ALK (60%), PD-L1 (48%), ROS1 (46%), BRAF (40%), mesenchymal epithelial transition factor receptor (MET) (35%), Kirsten rat sarcoma viral oncogene (KRAS) (29%), RET proto-oncogene (RET) (22%), human epidermal growth factor receptor 2 (HER2) (21%), and PIK3CA (20%, Fig. 1). Most patients (n = 660, 64.0%) received more than one biomarker test within 6 months of diagnosis. The proportion of patients undergoing biomarker testing rose from 55.3% in 2011 to 88.1% in 2021 (Fig. 2). In particular, there was a significant increase in the proportion of patients who received PD-L1 testing after the index diagnosis year of 2016 (Fig. 2).
Biomarker tests received within 6 months of diagnosis among the 1031 patients with eNSCLC during the entire study period between 2011–2021. ALK anaplastic lymphoma kinase, BRAF B-Raf proto-oncogene, DDR2 discoidin-domain receptor 2, EGFR epidermal growth factor receptor, eNSCLC early non-small cell lung cancer, ERBB2 erythroblastic oncogene B, FGFR1 fibroblast growth factor receptor 1, HER2 human epidermal growth factor receptor 2, KEAP1 Kelch-like ECH-associated protein 1, KRAS Kirsten rat sarcoma viral oncogene, LKB1 liver kinase B1, MAP 2k1 mitogen-activated protein kinase 1, MAP 2k2 mitogen-activated protein kinase 2, MEK1 mitogen-activated protein kinase 1, MEK2 mitogen-activated protein kinase 2, MET mesenchymal epithelial transition factor receptor, MLH1 MutL protein homolog 1, MSH2 MutS homolog 2, MSH6 MutS homolog 6, MSI microsatellite instability, NRAS neuroblastoma ras viral oncogene, NTRK1 neurotrophic tyrosine kinase receptor 1, NTRK2 neurotrophic receptor tyrosine kinase 2, NTRK3 neurotrophic receptor tyrosine kinase 3, PD-L1 programmed death receptor ligand 1, PIK3CA phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha, PMS2 mismatch repair endonuclease, RET RET proto-oncogene, ROS1 ROS proto-oncogene 1, STK11 serine/threonine kinase 11, TMB tumor mutational burden
Trends in receipt of the top 10 biomarker tests within 6 months of diagnosis over time (2011−2021). ALK anaplastic lymphoma kinase, BRAF B-Raf proto-oncogene, EGFR epidermal growth factor receptor, HER2 human epidermal growth factor receptor 2, KRAS Kirsten rat sarcoma viral oncogene, MET mesenchymal epithelial transition factor receptor, PD-L1 programmed death receptor ligand 1, PIK3CA phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha, RET RET proto-oncogene, ROS1 ROS proto-oncogene 1
The most commonly performed testing methods were Sanger sequencing for EGFR (n = 244, 37%), FISH for ALK (n = 464, 75%) and ROS1 (n = 357, 76%), IHC for PD-L1 (n = 450, 90%), and NGS testing for other biomarkers (Fig. 3). Most biomarker tests were conducted using tumor samples rather than blood samples (Fig. 4). The test turnaround time was shortest for IHC testing (median [interquartile range [IQR]]: 9 [7–22] days) and longest for RNA sequencing (median [IQR]: 59 [36–68.8] days) (Table 3). NGS testing had the second-longest turnaround time (median [IQR]: 30 [16–50.5] days) (Table 3).
Distribution of biomarker testing methods among 764 patients with eNSCLC who received biomarker tests within 6 months of diagnosis. ALK anaplastic lymphoma kinase, BRAF B-Raf proto-oncogene, DDR2 discoidin-domain receptor 2, EGFR epidermal growth factor receptor, eNSCLC early non-small cell lung cancer, FISH fluorescence in situ hybridization, FGFR1 fibroblast growth factor receptor 1, HER2 human epidermal growth factor receptor 2, IHC immunohistochemistry, KEAP1 Kelch-like ECH-associated protein 1, KRAS Kirsten rat sarcoma viral oncogene, MEK1 mitogen-activated protein kinase 1, MEK2 mitogen-activated protein kinase 2, MET mesenchymal epithelial transition factor receptor, MLH1 MutL protein homolog 1, MSH2 MutS homolog 2, MSH6 MutS homolog 6, MSI microsatellite instability, NGS next-generation sequencing, NRAS neuroblastoma ras viral oncogene, NTRK1 neurotrophic tyrosine kinase receptor 1, NTRK2 neurotrophic receptor tyrosine kinase 2, NTRK3 neurotrophic receptor tyrosine kinase 3, PCR polymerase chain reaction, PD-L1 programmed death receptor ligand 1, PIK3CA phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha, PMS2 mismatch repair endonuclease, RET RET proto-oncogene, RNA ribonucleic acid, ROS1 ROS proto-oncogene 1, STK11 serine/threonine kinase 11, TMB tumor mutational burden
Distribution of specimen types among 764 patients with eNSCLC who received biomarker tests within 6 months of diagnosis. ALK anaplastic lymphoma kinase, BRAF B-Raf proto-oncogene, DDR2 discoidin-domain receptor 2, EGFR epidermal growth factor receptor, eNSCLC early non-small cell lung cancer, FGFR1 fibroblast growth factor receptor 1, HER2 human epidermal growth factor receptor 2, KEAP1 Kelch-like ECH-associated protein 1, KRAS Kirsten rat sarcoma viral oncogene, MEK1 mitogen-activated protein kinase 1, MEK2 mitogen-activated protein kinase 2, MET mesenchymal epithelial transition factor receptor, MLH1 MutL protein homolog 1, MSH2 MutS homolog 2, MSH6 MutS homolog 6, MSI microsatellite instability, NRAS neuroblastoma ras viral oncogene, NTRK1 neurotrophic tyrosine kinase receptor 1, NTRK2 neurotrophic receptor tyrosine kinase 2, NTRK3 neurotrophic receptor tyrosine kinase 3, PD-L1 programmed death receptor ligand 1, PIK3CA phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha, PMS2 mismatch repair endonuclease, RET RET proto-oncogene, ROS1 ROS proto-oncogene 1, STK11 serine/threonine kinase 11, TMB tumor mutational burden
Treatment Utilization and Time to Treatment
Among the 1031 eNSCLC patients included in this analysis, most of the patients (n = 696, 67.5%) received surgery as their first-line treatment, followed by chemotherapy (n = 182, 17.7%), and radiation therapy (n = 133, 12.9%) (Fig. 5). Only 14 patients (1.4%) received immunotherapy or targeted therapy as their first-line treatment (Fig. 5). Ten out of these 14 patients had non-positive gene alterations. In addition, among the 566 patients who received systemic therapies, the median time from diagnosis to the first-line systemic therapy was around 50 days for chemotherapy, 44.5 days for immuno-chemo combination therapy, 75 days for immunotherapy, 95 days for targeted therapies, and 294 days for targeted-chemo combination therapy (Table 4).
Among 763 patients who received the five most commonly used biomarker tests (i.e., EGFR, ALK, PD-L1, ROS1, and BRAF), the time from initial diagnosis to biomarker testing and from biomarker testing to first-line systemic treatment initiation was investigated (Fig. 6). The average times from eNSCLC diagnosis to biomarker testing ranged from 5.3 days for PD-L1 to 8.7 days for BRAF. More than 97% of the patients received these biomarker tests before the initiation of a systemic treatment. The times between biomarker testing and systemic treatment initiation varied with both biomarker and treatment type, ranging between 49 and 56 days on average for chemotherapy and between 94 and 113 days for non-chemotherapy.
Time from diagnosis to the five most commonly used biomarker tests and time from the five most commonly biomarker tests to systemic treatment initiation within 1 year of eNSCLC diagnosis. Note: of the 763 patients who received these five biomarker tests, 20 had biomarker tests after their initial systemic treatment and were excluded from this figure. Chemo chemotherapy, eNSCLC early non-small cell lung cancer, Non-chemo non-chemotherapy
Discussion
Broad molecular profiling is essential for improving the care of patients with NSCLC [22]. Our study fills a gap in knowledge by examining the real-world biomarker test utilization and subsequent treatment over a period of 11 years in a national sample of adult patients diagnosed with eNSCLC. Our results show that the biomarker testing rate was high in the overall study sample, with 74.1% patients receiving at least one biomarker test within 6 months of their eNSCLC diagnosis. There was an increased adoption of biomarker testing over time, from 55.3% in 2011 to 88.1% in 2021. Among 763 patients who received the five most commonly used biomarker tests, almost all of them received a biomarker test before the initiation of a systemic treatment.
The overall high biomarker testing rate in eNSCLC patients observed in our study is comparable with the rates reported in aNSCLC patients, which range from 80 to 90% [23]. The approval and favorable results of a number of biomarker-based treatments, along with companion diagnostic devices, particularly for aNSCLC patients, may have promoted the increased adoption of biomarker testing during our study period. In our study, we observed a rapid uptake of PD-L1 testing after 2016, following the approval of pembrolizumab in October 2015 for patients with previously treated metastatic NSCLC whose tumors express PD-L1 as determined by an FDA-approved companion diagnostic [24]. A similar pattern of PD-L1 testing was also observed in patients with aNSCLC. For instance, a study focusing on patients with metastatic NSCLC reported an almost 10% increase in PD-L1 testing rate, from 3.0% in the second quarter of 2015 to 12.8% in the first quarter of 2016, following the approval of pembrolizumab in October 2015 [25]. A more recent study found that PD-L1 testing increased from 7.2% in 2015 to 73.2% in 2018 among patients with advanced NSCLC [26].
Regardless of the test results (positive or negative) of patients who received EGFR, ALK, PD-L1, ROS1, and BRAF testing, the five most commonly used biomarker tests in our study, the majority of them received chemotherapy, the recommended primary systemic treatment following eNSCLC diagnosis [19]. The adoption of targeted and immunotherapy agents for eNSCLC in guidelines or practice has been relatively recent. For instance, the first FDA approval for neoadjuvant therapy (i.e., nivolumab) for eNSCLC only occurred in 2022 [27]. This may explain the low use of immunotherapy or targeted therapy observed in our study. Additionally, the varied range of times between biomarker testing and chemotherapy initiation, an average 49- to 56-day gap, was consistent with clinical practice, as the majority of these patients had undergone surgery and typically needed to wait at least 6–8 weeks after resection to be considered for systemic chemotherapy. For patients who initiated non-chemotherapy treatment, the 94- to 113-day gap may be because these patients had to have completed adjuvant chemotherapy first. The recent FDA approvals of adjuvant therapies (i.e., osimertinib and atezolizumab) for eNSCLC will change practices in biomarker testing; testing for PD-L1 and EGFR mutations is vital for determining whether patients need these adjuvant therapies after their lung resections [28].
Our results also show that different biomarkers were tested via a wide variety of testing techniques or platforms. For example, Sanger sequencing and polymerase chain reaction (PCR) were the main methods used to test for EGFR, while FISH was the most frequently used testing method for detecting ALK. For most patients (90%), IHC tests were used for determining PD-L1 status. Additionally, we found that NGS testing was frequently used for testing for other biomarkers, especially for less commonly observed but emerging actionable biomarkers, such as KRAS, HER2, and neurotrophin receptor tyrosine kinase (NTRK). This is consistent with prior studies on biomarker testing in advanced settings, indicating that NGS technologies can increase efficiency by substituting for other tests used for biomarker testing, thus enabling testing for a wide range of genes simultaneously [29]. This also aligns with our finding that patients tend to be tested for multiple biomarkers rather than one single biomarker. Single-gene tests such as Sanger sequencing, IHC, and a range of in situ hybridization tests are usually less expensive per test than multigene methods. However, two decision analytical models suggested that using NGS or multi-gene panel sequencing as the initial test can lead to cost savings compared with a single-marker genetic testing approach [12, 30].
Furthermore, in most cases, single-gene tests have a shorter turnaround time than multigene methods. As shown in our results, IHC tests had the shortest turnaround time (median: 9 days) among all testing techniques, while NGS testing can take around 30 days from receiving specimens at a laboratory to the date of obtaining test results. The turnaround times for FISH and Sanger sequencing tests are consistent with previous studies [29]. However, the turnaround times for FISH, PCR, and NGS tests are longer than those reported by Hess et al., where median turnaround times of ≤ 10 days for all testing modalities including NGS were reported [23]. We noted that their definition of turnaround time was the time taken to receive results from the time that the specimen was received in the laboratory that performed the test, which did not account for the time taken to prepare and send the sample to the laboratory conducting the test. Moreover, Hess et al. evaluated a smaller subset of biomarkers (EGFR, ROS1, ALK, and BRAF) than those included in this study. These differences are likely to have played a role in the discrepancies between the two studies. In a survey of medical oncologists in the US, most providers considered 1 or 2 weeks an acceptable turnaround time [31]. Delays could occur at any point along the timeline, including biopsy, pathology sent out, testing, and analysis. Therefore, future studies should take into account the various steps in the process, starting at the time of specimen collection. Strategies can be employed to shorten the time to receipt of results, such as coordinating efforts between pathologists and surgeons to standardize procedures and decreasing the turnaround time within biomarker testing companies [31]. Prolonged turnaround times can influence oncologists to delay the decision to start treatment [31].
Although this study indicated high rates of biomarker testing in eNSCLC patients, there are several factors at play which can limit the utilization of such tests in the administration of targeted therapies. Poor quality and/or availability of tissue samples that prevent sufficient biomarker testing have been noted as significant constraints [32, 33]. Rapid on-site evaluation can help to ensure that the sample quality and quantity are sufficient; biomarker-specific processing methods and tissue-sparing techniques can all be implemented to limit this [32]. A previous study indicated that 49.7% of advanced NSCLC patients are lost to precision oncology due to factors associated with getting biomarker results [33]. In addition to insufficient sampling methods, the study also noted inadequate processing and interpretation of biomarker tests results as factors impeding the administration of appropriate targeted treatment [33]. Furthermore, many patients do not undergo biomarker testing due to factors such as cost concerns, test accessibility, lack of awareness of testing options, and low confidence of the ordering physician or the patient in the test value [33]. Removing the barriers that exist between biomarker testing and precision oncology will begin with furthering our understanding of these clinical gaps and the implementation of standardized protocols to support clinicians with the use of predictive biomarker testing in eNSCLC and wider oncology.
A limitation of our study may be that it is likely that the frequent NGS testing for less commonly used biomarkers observed in our study, such as KRAS, HER2, and NTRK, was performed in academic centers, as previous studies have suggested that academic practices tend to adopt NGS testing earlier than community practices [23]. However, we were not able to assess this due to a lack of information about community versus academic settings in our study base. Future studies should investigate this and find out how much of the increased PD-L1 testing was being driven by academic centers in our dataset, as routine PD-L1 testing for eNSCLC was not considered clinically relevant until 2021, when regulatory approval for PD-L1-driven adjuvant therapy with atezolizumab occurred. Additionally, it is worthwhile noting that emerging biomarkers, such as HER2, RET, and MET, are reimbursed by few payers [34]. Due to a lack of patients’ insurance or payment data in our study database, we do not know how various biomarker tests or procedures were paid for in this study. Third, our study database included patients with eNSCLC representing the Northeast, Southeast, and South-Central regions of the US. Therefore, our results might not be generalizable to patients from other regions. Future studies should be conducted using a larger, real-world database representing all regions of the US. Furthermore, there is a lack of diversity in the race distribution in the database, with most of the included patients being white (91.8%). Test utilization and subsequent treatment may vary across different race subgroups. For instance, a previous study reported that 50.1% of white patients versus 39.9% of Black/African Americans ever received NGS testing (p < 0.0001) [35].
Conclusion
This is the first real-world study to assess the biomarker test utilization and subsequent treatment in patients with eNSCLC. The study suggests a high biomarker testing rate among patients with eNSCLC in the US, with testing rates for various biomarkers increasing over time during the past decade, indicating a continuous trend towards the personalization of treatment decisions. Timely biomarker testing is essential for patients with NSCLC to ensure that patients receive the appropriate treatment at the right time. With the rapidly evolving treatment landscape and testing recommendations for eNSCLC, future research is needed to understand whether biomarker testing has improved optimal treatment decision making and long-term survival outcomes for patients with eNSCLC.
References
American Cancer Society. Cancer facts & figures 2022. 2022. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2022.html. Accessed 6 June 2023.
Inamura K. Lung cancer: understanding its molecular pathology and the 2015 WHO classification. Front Oncol. 2017;7:193. https://doi.org/10.3389/fonc.2017.00193.
The Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511(7511):543–50. https://doi.org/10.1038/nature13385.
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. WHO classification of tumours of the lung, pleura, thymus and heart. Lyon: IARC; 2015.
Cancer Treatment Centers of America. Lung cancer types. 2022. https://www.cancercenter.com/cancer-types/lung-cancer/types. Accessed 6 June 2023.
Ganti KA, Klein AB, Cotarla I, Seal B, Chou E. Update of incidence, prevalence, survival, and initial treatment in patients with non-small cell lung cancer in the US. JAMA Oncol. 2021;7(12):1824–32. https://doi.org/10.1001/jamaoncol.2021.4932.
McDonald F, De Waele M, Hendriks LEL, Faivre-Finn C, Dingemans A-MC, Van Schil PE. Management of stage I and II nonsmall cell lung cancer. Euro Respir J. 2017;49(1):1600764. https://doi.org/10.1183/13993003.00764-2016.
Rodríguez M, Ajona D, Seijo LM, et al. Molecular biomarkers in early stage lung cancer. Transl Lung Cancer Res. 2021;10(2):1165–85. https://doi.org/10.21037/tlcr-20-750.
Yang SR, Schultheis AM, Yu H, Mandelker D, Ladanyi M, Büttner R. Precision medicine in non-small cell lung cancer: current applications and future directions. Semin Cancer Biol. 2022;84:184–98. https://doi.org/10.1016/j.semcancer.2020.07.009.
Kerr KM, Bibeau F, Thunnissen E, et al. The evolving landscape of biomarker testing for non-small cell lung cancer in Europe. Lung Cancer. 2021;154:161–75. https://doi.org/10.1016/j.lungcan.2021.02.026.
Aisner DL, Riely GJ. Non–small cell lung cancer: recommendations for biomarker testing and treatment. J Natl Compr Canc Netw. 2021;19(5.5):610–3. https://doi.org/10.6004/jnccn.2021.5020.
Pennell NA, Arcila ME, Gandara DR, West H. Biomarker testing for patients with advanced non-small cell lung cancer: real-world issues and tough choices. Am Soc Clin Oncol Educ Book. 2019;39:531–42. https://doi.org/10.1200/edbk_237863.
Douillard JY, Rosell R, De Lena M, et al. Adjuvant vinorelbine plus cisplatin versus observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer (Adjuvant Navelbine International Trialist Association [ANITA]): a randomised controlled trial. Lancet Oncol. 2006;7(9):719–27. https://doi.org/10.1016/s1470-2045(06)70804-x.
Pignon JP, Tribodet H, Scagliotti GV, et al. Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE Collaborative Group. J Clin Oncol. 2008;26(21):3552–9. https://doi.org/10.1200/jco.2007.13.9030.
Burotto M, Thomas A, Subramaniam D, Giaccone G, Rajan A. Biomarkers in early-stage non-small-cell lung cancer: current concepts and future directions. J Thorac Oncol. 2014;9(11):1609–17. https://doi.org/10.1097/jto.0000000000000302.
Herbst RS, Tsuboi M, John T, et al. Osimertinib as adjuvant therapy in patients (pts) with stage IB–IIIA EGFR mutation positive (EGFRm) NSCLC after complete tumor resection: ADAURA. J Clin Oncol. 2020;38(18 Suppl.):Abstract LBA5. https://doi.org/10.1200/JCO.2020.38.18_suppl.LBA5.
Wu YL, Tsuboi M, He J, et al. Osimertinib in resected EGFR-mutated non-small-cell lung cancer. N Engl J Med. 2020;383(18):1711–23. https://doi.org/10.1056/NEJMoa2027071.
US Food & Drug Administration (FDA). FDA approves atezolizumab as adjuvant treatment for non-small cell lung cancer. Published October 15, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-atezolizumab-adjuvant-treatment-non-small-cell-lung-cancer.
National Comprehensive Cancer Network. Non-small cell lung cancer. Version 5.2022. 2022. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 6 June 2023.
COTA. Bringing clarity to cancer. 2022. https://cotahealthcare.com/. Accessed 6 June 2023.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Ettinger DS, Wood DE, Aisner DL, et al. Non–small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20(5):497–530. https://doi.org/10.6004/jnccn.2022.0025.
Hess LM, Krein PM, Haldane D, Han Y, Sireci AN. Biomarker testing for patients with advanced/metastatic nonsquamous NSCLC in the United States of America, 2015 to 2021. JTO Clin Res Rep. 2022;3(6):100336. https://doi.org/10.1016/j.jtocrr.2022.100336.
National Cancer Institute. FDA approves pembrolizumab for patients with non-small cell lung cancer. 2015. https://www.cancer.gov/news-events/cancer-currents-blog/2015/pembrolizumab-nsclc. Accessed 6 June 2023.
Khozin S, Abernethy AP, Nussbaum NC, et al. Rates of PD-L1 expression testing in U.S. community-based oncology practices (USCPs) for patients with metastatic non-small cell lung cancer (mNSCLC) receiving nivolumab (N) or pembrolizumab (P). J Clin Oncol. 2017;35(15 Suppl.):Abstract 11596. https://doi.org/10.1200/JCO.2017.35.15_suppl.11596.
Leapman MS, Presley CJ, Zhu W, et al. Association of programmed cell death ligand 1 expression status with receipt of immune checkpoint Inhibitors in patients with advanced non-small cell lung cancer. JAMA Netw Open. 2020;3(6):e207205. https://doi.org/10.1001/jamanetworkopen.2020.7205.
US Food & Drug Administration (FDA). FDA approves neoadjuvant nivolumab and platinium-doublet chemotherapy for early-stage non-small cell lung cancer. Published 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-neoadjuvant-nivolumab-and-platinum-doublet-chemotherapy-early-stage-non-small-cell-lung. Accessed 6 June 2023.
Yanagawa J. Non-small cell lung cancer: managment of patients with resectable disease. In: National Comprehensive Cancer Network (NCCN) 2022 Annual Conf; 2022 Oct 14–15; virtual.
van de Ven M, Koffijberg H, Retèl V, et al. Real-world utilization of biomarker testing for patients with advanced non-small cell lung cancer in a tertiary referral center and referring hospitals. J Mol Diagn. 2021;23(4):484–94. https://doi.org/10.1016/j.jmoldx.2021.01.004.
Steuten L, Goulart B, Meropol NJ, Pritchard D, Ramsey SD. Cost effectiveness of multigene panel sequencing for patients with advanced non-small-cell lung cancer. JCO Clin Cancer Inform. 2019;3:1–10. https://doi.org/10.1200/cci.19.00002.
Mileham KF, Schenkel C, Bruinooge SS, et al. Defining comprehensive biomarker-related testing and treatment practices for advanced non-small-cell lung cancer: results of a survey of U.S. oncologists. Cancer Med. 2022;11(2):530–8. https://doi.org/10.1002/cam4.4459.
Penault-Llorca F, Kerr KM, Garrido P, et al. Expert opinion on NSCLC small specimen biomarker testing—part 1: tissue collection and management. Virchows Arch. 2022;481(3):335–50. https://doi.org/10.1007/s00428-022-03343-2.
Sadik H, Pritchard D, Keeling DM, et al. Impact of clinical gaps on the implementation of personalized medicine in advanced non-small cell lung cancer. JCO Precis Oncol Oncol. 2022. https://doi.org/10.1200/PO.22.00246.
American Cancer Society Cancer Action Network and LUNGevity Foundation. Payer coverage policies of tumor biomarker testing. 2020. https://www.fightcancer.org/sites/default/files/ACS%20CAN%20and%20LUNGevity_Payer%20Coverage%20Policies%20of%20Tumor%20Biomarker%20Testing.pdf. Accessed 6 June 2023.
Peck P. Precision medicine: it’s all about biomarker testing. 2022. https://www.physiciansweekly.com/precision-medicine-its-all-about-biomarker-testing. Accessed 6 June 2023.
Acknowledgements
Funding
This study and its publication, including the journal’s Rapid Service Fee, as well as medical editing support, was funded by Roche Diagnostics International Ltd (Rotkreuz, Switzerland).
Medical Writing, Editorial, and Other Assistance
Editorial support for this manuscript was provided by Aisling Minard, PhD, of Ashfield MedComms (Manchester, UK), an Inizio company, and was funded by Roche Diagnostics International Ltd.
Author Contributions
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship. Jessie T. Yan, Yue Jin, Ernest Lo, Yilin Chen, Amy E. Hanlon Newell, Ying Kong, and Landon J. Inge contributed to the study concept and design, the interpretation of the data, and to the drafting and critical review of the manuscript. Yue Jin and Yilin Chen further contributed to the analysis of the data. This manuscript has been approved by all authors.
Prior Presentation
The poster was presented at ISPOR 2023, Boston, MA, USA, May 7-10, 2023 (MT51) https://www.ispor.org/heor-resources/presentations-database/presentation/intl2023-3669/125655.
Disclosures
Jessie T. Yan, Yue Jin, and Ernest Lo are employees of Roche Diagnostics, Santa Clara, and hold Roche stocks; Ying Kong and Landon J. Inge are employees of Roche Diagnostics Solutions, Tucson, and hold Roche stocks; Yilin Chen was a summer intern at Roche Diagnostics during the conduct of the study; Amy E. Hanlon Newell was an employee of Roche Diagnostics Solutions, Tucson, at the time of analysis and holds Roche stock.
Compliance with Ethics Guidelines
All study data were fully compliant with US patient confidentiality requirements, including the HIPAA of 1996. The study used only de-identified patient records and, therefore, was exempted from institutional review board approval. Informed consent was not required as this was not an interventional study, and routinely collected, anonymized data were used. This study complied with all relevant national regulations and was performed in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonization Guidelines on Good Clinical Practice. Full permission was received by COTA to access the study database.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available, as individual data cannot be shared, per HIPAA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yan, J.T., Jin, Y., Lo, E. et al. Real-World Biomarker Test Utilization and Subsequent Treatment in Patients with Early-Stage Non-small Cell Lung Cancer in the United States, 2011−2021. Oncol Ther 11, 343–360 (2023). https://doi.org/10.1007/s40487-023-00234-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-023-00234-7