Abstract
The identification of actionable biomarkers and development of targeted therapies have revolutionized the field of lung cancer treatment. In patients with advanced non-small cell lung cancer (NSCLC), biomarker testing can inform selection of effective targeted therapies as well as avoid therapies that are less likely to be effective in certain populations. A growing number of actionable targets, including those involving EGFR, ALK, ROS1, BRAF, MET, KRAS, NTRK, RET, HER2, and PD-L1, can be identified with biomarker testing. More than half of patients with advanced NSCLC have tumors that harbor genetic alterations that can be targeted. When these patients are treated with targeted therapy, survival and quality of life may be significantly improved. In addition, broad-based molecular testing may detect alterations identifying patients who are potentially eligible for current or future clinical trials. Comprehensive biomarker testing rates in communities are often low, and turnaround times for results can be unacceptably long. There is an unmet need for widespread, efficient, and routine testing of all biomarkers recommended by clinical guidelines. New testing techniques and technologies can make this an attainable goal. Panel-based sequencing platforms are becoming more accessible, and molecular biomarker analysis of circulating tumor DNA is becoming more common. In this podcast, we discuss the importance of biomarker testing in advanced NSCLC and explore topics such as testing methodologies, effect of biomarker testing on patient outcomes, emerging technologies, and strategies for improving testing rates in the United States.
Supplementary file1 (MP4 121301 KB)
Similar content being viewed by others
More than half of patients with advanced non-small cell lung cancer (NSCLC) have tumors that harbor an actionable biomarker. |
Early, broad-based biomarker testing is essential for determining optimal treatment for NSCLC and is recommended by guidelines. |
Biomarker testing rates and efficiency should be improved through the dissemination of information and advances in technology. |
This podcast is about the importance of biomarker testing in advanced NSCLC and includes discussion about testing methodologies and testing rates in the United States. |
Digital Features
This article is published with digital features, including a podcast audio, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.25352794.
Podcast Transcript
Welcome to the podcast. This podcast was supported by Pfizer Incorporated, with editorial support provided by Mark McCollum of Nucleus Global and funded by Pfizer.
FH: Hello everybody. My name is Dr. Fred Hirsch. I'm the Executive Director at the Tisch Cancer Institute at Mount Sinai, New York, and the Center of Thoracic Oncology there. And I’m also the Joe Lowe and Louis Price Professor of Medicine at Icahn School of Medicine at Mount Sinai.
CK: Hello. My name is Chul Kim. I'm an Associate Professor at the Division of Hematology and Oncology at the School of Medicine at Georgetown University.
In this podcast, Fred and I will be discussing predictive biomarkers and how biomarker testing informs targeted treatments in advanced non-small cell lung cancer or NSCLC. The topics we will cover include importance of biomarker testing, testing methodologies, the effect of biomarker testing on patient outcomes, emerging technologies, and opportunities to improve biomarker testing rates. Fred, why is biomarker testing important in patients with advanced non-small cell lung cancer?
FH: Well, step a little bit back in the history. Ten years ago, chemotherapy was a main option for patients with advanced lung cancer, and the median overall survival was less than 12 months [1]. Since then, the discovery of actionable biomarkers and the development of targeted therapies have revolutionized the field [2,3,4]. Biomarker testing and targeted therapies are based on oncogenic genomic alteration that include gene mutations, rearrangements, and amplifications [2]. In 2004, we had one actionable genomic alteration, the EGFR; today, we have more than ten, and we have even a greater number of US FDA [Food and Drug Administration]-approved targeted therapies [5, 6]. Approximately 60% of patients with advanced non-small cell lung cancer, especially adenocarcinoma, have tumors that harbor genetic mutations that can be targeted; if these patients are treated with a targeted therapy, the overall survival and the quality of life may be significantly improved [4, 7,8,9,10]. Patients who do not receive comprehensive biomarker testing may not receive optimal therapy [9, 10]. Biomarker testing for driver mutations that do not have an approved targeted therapy can help to identify patients eligible to enroll in clinical trials [11]. Chul, before we talk more about the utility of biomarker testing, would you please elaborate how often biomarker testing is being done in patients with advanced non-small cell lung cancer?
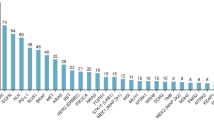
CK: Yes, sure, Fred. Unfortunately, data suggests that comprehensive biomarker testing rates in patients with lung cancer are low [3, 10]. For example, an analysis of electronic health records from community-based oncology practices shows that between 2018 and 2020, less than 50% of patients with metastatic non-small cell lung cancer received testing for five of the biomarkers most routinely recommended in guidelines, which are EGFR, ALK, ROS1, BRAF, and PD-L1. The median turnaround time between ordering the testing and receiving the results was approximately 2 weeks, and only 35% of patients had testing results for five biomarkers before initiation of first-line treatment [10]. Sometimes the testing is performed, but the results are not accessible in the patient's electronic health record. When comprehensive biomarker testing is not performed, or results are delayed, patients may not receive optimal therapy in a timely manner. So there is an opportunity to improve testing rates and turnaround times. Fred, what do current guidelines recommend regarding when biomarker testing should be performed and what testing methodology should be used?
FH: Well, the guidelines has of course evolved over time. According to the current guidelines, biomarker testing is recommended at the time of initial diagnosis for, I would say, all patients with metastatic lung cancer to determine if they are eligible for targeted therapies or immunotherapies [4, 10, 12,13,14]. It has been discussed, and it can still be discussed, whether all patients with squamous lung cancer need comprehensive biomarker testing. In my institution, we do comprehensive biomarker testing in all patients, because, particularly if you have a younger patient with squamous lung cancer and a never-smoker, Asian ethnicity,Footnote 1 you can find a driver mutation also in squamous histology. So, our recommendation today is comprehensive biomarker to all patients with advanced non-small cell lung cancer. Those recommendations are based on data showing clearly improved survival in patients who received biomarker-based therapies compared to traditional chemotherapy [3, 4, 8,9,10]. It is important that the clinicians wait for the results of biomarker testing before initiating treatment [15], unless in the rare situation where the patient is very much symptomatic and have a high disease burden. In those cases, it can be indicated to initiate therapy immediately, but as a rule, we should wait for the comprehensive biomarker testing before initiation of a therapy. Of course, if drug resistance develops and disease progress, which unfortunately still happens in almost all patients, additional biomarker testing may be performed to inform subsequent treatment [14]. We do have today several treatment options based on genomic alterations at time of treatment resistance in first-line therapy.
We have also most recently learned about early-stage lung cancer and the need of genomic knowledge profiling of tumors in early-stage non-small cell lung cancer [16]. We learned that in it first, with EGFR, through the ADAURA study as adjuvant EGFR therapy [17]. We most recently also learned results for ALINA study in ALK-positive patients using an adjuvant therapy [18]. So, even in early-stage disease, it is today recommended to do molecular profiling.
Current guidelines recommend a panel-based approach by next-generation sequencing, also known as “NGS” [19]. NGS has demonstrated broader detection of genomic regions of interest, with potential superior sensitivity and improved cost-effectiveness over single gene assays [10, 20, 21]. DNA-based NGS is the established approach to detect rearrangements that produce common oncogenic kinase fusions, including ALK, RET, ROS, MET exon 14 skipping mutations [22]. But, DNA-based NGS has certain challenges as well. First, some clinically relevant fusions result from rearrangement that occur within very long introns. Tiling probes for those long introns can be technically challenging and may significantly compromise the coverage of the remaining genes within the panel. Secondly, introns may have repetitive elements that exist elsewhere in the genome and cannot be assessed by short-read sequencing because given the difficulty of uniquely mapping such reads. This produce gaps in the coverage of certain introns and blind spots in the detection of potential rearrangement breakpoints. Thirdly, DNA-based NGS may detect fusions or rearrangements that are not actually expressed at the mRNA level. So, when we are talking fusions, RNA-based NGS probably is superior to DNA-based NGS [23, 24]. A retrospective analysis related to that showed that 14% of DNA-sequenced negative cases were positive for fusions and rearrangements by RNA sequencing [22]. That is one study. There might be other studies, and there are other studies out there. And false-negative DNA percentage can vary, but in general, fusions are best detected by RNA. The DNA that we use for testing can now come from sources other than the tissue biopsy. And that leads us to the next topic of discussion, discussing circulating tumor DNA or ctDNA in blood, also known as liquid biopsy. Chul, while tissue biopsy is our current gold standard for diagnosis, can you please explain the role of liquid biopsy in biomarker testing?
CK: Sure, Fred. This is an important topic. Liquid biopsy involves the acquisition of biomarkers from body fluids, mainly blood; plasma-derived ctDNA is the primary source of biomarkers in liquid biopsies [25]. Most guidelines state that liquid biopsy testing be considered when the patient is medically unfit for needle biopsy or tissue biopsy yields an insufficient sample for testing [10]. However, the routine use of liquid biopsies at diagnosis has several advantages. Liquid biopsies are noninvasive and may reduce costs and complications associated with multiple tissue biopsies [3]. Additionally, turnaround time may be shorter based on liquid biopsy; a study of molecular testing results in patients with advanced lung cancer found a turnaround time of 9 days with liquid biopsy versus 15 days with tissue biopsy [26]. Liquid biopsies can be serially repeated for therapeutic monitoring, but it is important to consider the potential cost implications of frequent testing, though [3]. Evidence supports the complementary use of liquid and tissue biopsies for molecular biomarker testing to increase detection and reduce time to treatment [8, 27, 28]. Recent studies have indicated that testing both liquid and tissue biopsies can increase the detection rate of actionable mutations, with detection rates for combination testing being 48% to 75% higher than rates for tissue biopsy alone [10]. Fred, would you please tell us which targetable biomarkers should be screened in patients with advanced lung cancer?
FH: Yeah, according to current guidelines, testing should be performed for the following biomarkers: EGFR mutation, which we have talked about previously, ALK rearrangements, BRAF, HER2/ERBB2 mutations, KRAS mutations, MET exon 14 skipping mutations, we have NTRK fusions, RET arrangements, and the ROS1 rearrangements [3, 4, 10]. Of course, testing for PD-L1 expression is also strongly advised, as we use PD-L1 as an indicator for whether we should give either immunotherapy alone or immunotherapy in combination with a chemotherapy [10]. Immunotherapy with or without chemotherapy is recommended as first-line therapy for patients without any actionable mutation [4]. However, when an actionable mutation is detected, effective treatment in first-line therapy is available, and targeted therapy should generally take precedence over immunotherapy even if the PD-L1 expression is elevated [4, 29]. Guidelines also recommend screening for emerging biomarkers, such as high-level MET amplification [4]. Broad molecular profiling, which can identify rare alterations without an approved therapy, is advised to identify clinical trials for which a patient may be eligible [3, 14, 29]. So again, a broader, comprehensive molecular profiling is recommended for every patient. The purpose of the biomarker guidelines is, of course, to promote practices that will lead to the best possible patient outcome.
In my institution, we have introduced more or less reflexive biomarker testing, both for patients with advanced non-small cell lung cancer as well as patients with early-stage non-small cell lung cancer. Of course, we are an academic institution, and some of the findings might currently have more academic interest than clinical practice interest. But again, using the principle that each patient should have comprehensive testing and no patients should be left behind, should justify broad testing for everyone. Dr. Kim, what is practiced in your institution?
CK: My practice and the practice here is quite similar to what you have just described, Fred. So, at the time of initial diagnosis of advanced non-small cell lung cancer, I utilize both tissue-based molecular profiling and plasma-based NGS simultaneously. I find that using both approaches, which have different advantages, is complementary and helps inform timely treatment decisions. And for, as you mentioned, early-stage non-small cell lung cancer, we also use NGS more often than before. And so, this is our practice pattern here, it's quite similar.
FH: So Chul, are there differences in patient outcomes when biomarker testing is used?
CK: Yes, evidence indicates that biomarker-directed therapy is associated with better patient outcomes [30]. For instance, a recent study using electronic health records showed that among 1260 patients with advanced non-small cell lung cancer and a targetable driver alteration, 48.3% received targeted therapy [31]. Patients who received targeted therapies experienced a longer median overall survival of 18.6 months versus 11.4 months in those who did not receive targeted therapy. Now, let's discuss important advances in this field that may improve testing efficiency. Fred, what emerging technologies do you think hold promise in the field of biomarker testing?
FH: Well, first of all, it is important to keep informed on the identification of new druggable oncogene drivers. The field of drug development in targeted therapies goes very fast, and it is important to keep up on all that information. For example, high-level MET amplification, NRG1 fusion, are emerging biomarkers with targeted drugs in development [14, 21]. When we are talking new biomarker techniques, of course, of high interest is: can we make early detection of lung cancer by using ctDNA genotyping? And is it possible to prove or have a high sensitivity and specificity based on liquid biopsy in that space? One platform for this purpose uses bisulfite sequencing and machine learning to detect abnormal ctDNA methylation in plasma, and clinical trials is undergoing to validate this technology [25].
When we're talking immunotherapy, we have had much discussion around tumor mutation burden (TMB) and the role of TMB for predicting efficacy of immunotherapy in lung cancer. TMB serves as a surrogate marker for tumor and neoantigen production, which trigger an immune response [32, 33]. In this way, TMB is thought to be correlated with the efficacy of immune checkpoint inhibitors. There are many current NGS platforms measuring TMB. My personal view is, in lung cancer, the TMB concept needs to be refined. Not all mutations are equally immunogenic. And we need to refine the concept, whether that is in combination with the HLA expression, other modifications of the TMB. But of course, there are studies looking into that. In addition, there are other body fluids which could be the source for liquid biopsy as well. Of interest is ctDNA assessment in cerebrospinal fluid, which could be used to profile brain metastases, which of course is a huge clinical problem in the lung cancer management [34], and there are studies ongoing also in that space.
Artificial intelligence, better known as “AI,” is today a very hot term and a very relevant, of course also, methodology, I would say. And deep learning algorithms are being developed to analyze DNA and RNA data and to discover new novel biomarkers [35]. AI-based predictive models may help us to identify patients who will derive clinical benefit from biomarker-based therapy [36]. By combining AI with well-known other, I would say, technologies or disciplines such as pathology, radiology, genomics, these combined technology methodologies may be able to predict better patient outcome resulting from immunotherapy or targeted therapy [36]. So, new technologies and techniques open the door for more efficient and widespread biomarker testing. In your opinion, Chul, how can biomarker testing rates be improved for patients with advanced lung cancer?
CK: Certainly. From the point of lung cancer diagnosis, patients and their care team are faced with a difficult journey that includes many complex steps. Incorporating biomarker testing early in the process can optimize patient outcomes [14]. As we previously mentioned, comprehensive biomarker testing is often not being performed, or the results are not received prior to initiating treatment. To improve biomarker testing rates, more medical education is needed. Healthcare providers that comprise an oncology team need to be fully informed on the importance and interpretation of biomarker data [14, 37]. Important information includes recognizing what biomarker testing resources are available at the practitioner's institution, the benefits and limitations of DNA- and RNA-based NGS, the advantages as well as limitations of plasma-based ctDNA, the need for consistent biomarker reporting in electronic health records, and best practices for sample collection. Case reviews by a molecular tumor board can help promote an interdisciplinary team approach [14, 38]. This board should be composed of a diverse set of medical specialists, with the common goal of determining the best diagnostic procedures and treatment regimens for a patient. This interdisciplinary team can provide comprehensive knowledge on emerging biomarkers that are clinically relevant and advise on associations with treatment outcomes. In addition, diagnostic testing in accordance with sample type and availability can also be discussed. Ultimately, this can help each patient receive a more customized diagnostic and treatment plan [38]. Also, the turnaround times with biomarker testing can also be improved [10, 14]. In cases where advanced lung cancer is confirmed or highly suspected, molecular testing should be ordered promptly to help guide treatment decisions [39].
Liquid biopsies may be useful in certain situations, for example, where tissue procurement or availability is a concern. Liquid biopsies can be obtained and analyzed early in the diagnostic pathway and may be associated with decreased turnaround times [26]. Finally, insurance is a well-known factor impacting cancer treatment. A recent study demonstrated that patients with the public insurance are less likely to receive biomarker testing and biomarker-driven therapy than those with private insurance [40]. Collectively, as practitioners in the treatment of lung cancer, if we can improve the dissemination of biomarker information, such as current guidelines, and promote cross-disciplinary dialogue about the utility of biomarkers, testing rates will increase. Fred, do you have any additional thoughts to add before closing?
FH: Yeah, I think we have touched upon the most important things. The fact that real-world data tells us that maybe just half of the patients with advanced lung cancer get five or more genomic alterations recorded or studied before initiation of therapy is, in my opinion, alarmingly low level of participation [10]. And we need to figure out how can we increase number of patients undergoing molecular profiling before initial treatment is instituted. And for that, I think education is the key word. We need to come out in the communities and educate all the involved stakeholders on the importance of molecular testing. And it is a continuous process, as we talked about, Chul. There is a rapid development in molecular targeted therapies and new targets are discovered the whole time. So, a continuous, intensified education in the communities are important. I would also repeat that broad molecular testing give also the patients opportunity to identify potential clinical trials to be eligible for. We need more patients into clinical trials. We need more diversity into clinical trials. So, we need to reach out to communities, minority communities, to be sure that they are aware of molecular testing, they are aware of the benefit, potential benefit being a part of clinical trials. So, there is some work we have to do, but it needs to be done as soon as possible.
CK: Thank you, Fred. I would like to echo all your comments, and I cannot agree more. I also would like to emphasize the significant impact of comprehensive biomarker testing on patient outcomes. It really enables the selection of the most effective treatment for the patient, enhancing patient care [30]. Looking ahead, the integration of novel biomarker testing across various stages and settings in lung cancer care is a very promising and exciting development. In closing, we encourage the listener to help raise awareness about the importance of biomarker testing and keep informed on topics such as targeted therapies in development, emerging testing methods, and the use of liquid biopsy. Biomarker testing rates and efficiency should be improved through the dissemination of information and advances in technology. Thank you very much.
FH: And Chul, I would like to add also to these important conclusive remarks that education goes in many directions. It goes also in a multidisciplinary direction, meaning that we need to educate each other in the different, relevant disciplines. And medical oncologists, they might know a lot about molecular targeted therapies and biomarkers, but we need to also be sure that the other stakeholders like surgeons, radiotherapists, and pathologists, of course, they will know more. But we need to educate each other in multidisciplinary tumor boards. And that is important to expand on in the future management of lung cancer patients, in the current and future management of lung cancer patients.
CK: Very, very well said, Fred.
FH: Thank you.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Notes
People having origins in any of the original peoples of the Far East, Southeast Asia, or the Indian subcontinent.
References
Simeone JC, Nordstrom BL, Patel K, Klein AB. Treatment patterns and overall survival in metastatic non-small-cell lung cancer in a real-world US setting. Future Oncol. 2019;15(30):3491–502.
Camidge DR, Doebele RC, Kerr KM. Comparing and contrasting predictive biomarkers for immunotherapy and targeted therapy of NSCLC. Nat Rev Clin Oncol. 2019;16(6):341–55.
Pennell NA, Arcila ME, Gandara DR, West H. Biomarker testing for patients with advanced non-small cell lung cancer: real-world issues and tough choices. Am Soc Clin Oncol Educ Book. 2019;39:531–42.
Aisner DL, Riely GJ. Non-small cell lung cancer: recommendations for biomarker testing and treatment. J Natl Compr Cancer Netw. 2021;19(5.5):610–3.
American Cancer Society. 2023 [cited 2023 January 26]; Available from: https://www.cancer.org/cancer/lung-cancer/treating-non-small-cell/targeted-therapies.html
Rodak O, Peris-Díaz MD, Olbromski M, Podhorska-Okołów M, Dzięgiel P. Current landscape of non-small cell lung cancer: epidemiology, histological classification, targeted therapies, and immunotherapy. Cancers (Basel). 2021;13(18):4705.
Kris MG, Johnson BE, Kwiatkowski DJ, Iafrate AJ, Wistuba II, Aronson SL, et al. Identification of driver mutations in tumor specimens from 1,000 patients with lung adenocarcinoma: the NCI’s lung cancer mutation consortium (LCMC). J Clin Oncol. 2011;29:(18_Suppl). Abstract CRA7506.
Arbour KC, Riely GJ. Systemic therapy for locally advanced and metastatic non-small cell lung cancer: a review. JAMA. 2019;322(8):764–74.
VanderLaan PA, Rangachari D, Costa DB. The rapidly evolving landscape of biomarker testing in non–small cell lung cancer. Cancer Cytopathol. 2021;129(3):179–81.
Robert NJ, Espirito JL, Chen L, Nwokeji E, Karhade M, Evangelist M, et al. Biomarker testing and tissue journey among patients with metastatic non-small cell lung cancer receiving first-line therapy in the US oncology network. Lung Cancer. 2022;166:197–204.
Jain D. Lung molecular cytopathology: EGFR and beyond. J Cytol. 2019;36(2):124–7.
Naso J, Lo YC, Sholl LM. Updates in pathology and molecular diagnostics to inform the evolving landscape of thoracic surgery and oncology. J Surg Oncol. 2023;127(2):244–57.
Planchard D, Popat S, Kerr K, Novello S, Smit EF, Faivre-Finn C, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl 4):iv192–237.
Gregg JP, Li T, Yoneda KY. Molecular testing strategies in non-small cell lung cancer: optimizing the diagnostic journey. Transl Lung Cancer Res. 2019;8(3):286–301.
Mileham KF, Schenkel C, Bruinooge SS, Freeman-Daily J, Basu Roy U, Moore A, et al. Defining comprehensive biomarker-related testing and treatment practices for advanced non-small-cell lung cancer: results of a survey of US oncologists. Cancer Med. 2022;11(2):530–8.
McGuire AL, McConechy MK, Melosky BL, English JC, Choi JJ, Peng D, et al. The clinically actionable molecular profile of early versus late-stage non-small cell lung cancer, an individual age and sex propensity-matched pair analysis. Curr Oncol. 2022;29(4):2630–43.
Tsuboi M, Herbst RS, John T, Kato T, Majem M, Grohe C, et al. Overall survival with osimertinib in resected EGFR-mutated NSCLC. N Engl J Med. 2023;389(2):137–47.
Solomon BJ, Ahn JS, Dziadziuszko R, Barlesi F, Nishio M, Lee DH, et al. ALINA: efficacy and safety of adjuvant alectinib versus chemotherapy in patients with early-stage ALK+ non-small cell lung cancer (NSCLC). Ann Oncol. 2023;34:S1295–6. Abstract LBA2.
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, et al. Non-small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20(5):497–530.
Kerr KM, Bibeau F, Thunnissen E, Botling J, Ryška A, Wolf J, et al. The evolving landscape of biomarker testing for non-small cell lung cancer in Europe. Lung Cancer. 2021;154:161–75.
Guo H, Zhang J, Qin C, Yan H, Liu T, Hu H, et al. Biomarker-targeted therapies in non-small cell lung cancer: current status and perspectives. Cells. 2022;11(20):3200.
Benayed R, Offin M, Mullaney K, Sukhadia P, Rios K, Desmeules P, et al. High yield of RNA sequencing for targetable kinase fusions in lung adenocarcinomas with no mitogenic driver alteration detected by DNA sequencing and low tumor mutation burden. Clin Cancer Res. 2019;25(15):4712–22.
Solomon JP, Linkov I, Rosado A, Mullaney K, Rosen EY, Frosina D, et al. NTRK fusion detection across multiple assays and 33,997 cases: diagnostic implications and pitfalls. Mod Pathol. 2020;33(1):38–46.
Heydt C, Wölwer CB, Velazquez Camacho O, Wagener-Ryczek S, Pappesch R, Siemanowski J, et al. Detection of gene fusions using targeted next-generation sequencing: a comparative evaluation. BMC Med Genom. 2021;14(1):62.
Gray J, Thompson JC, Carpenter EL, Elkhouly E, Aggarwal C. Plasma cell-free DNA genotyping: from an emerging concept to a standard-of-care tool in metastatic non-small cell lung cancer. Oncologist. 2021;26(10):e1812–21.
Leighl NB, Page RD, Raymond VM, Daniel DB, Divers SG, Reckamp KL, et al. Clinical utility of comprehensive cell-free DNA analysis to identify genomic biomarkers in patients with newly diagnosed metastatic non-small cell lung cancer. Clin Cancer Res. 2019;25(15):4691–700.
Choudhury Y, Tan MH, Shi JL, Tee A, Ngeow KC, Poh J, et al. Complementing tissue testing with plasma mutation profiling improves therapeutic decision-making for patients with lung cancer. Front Med (Lausanne). 2022;9:758464.
Rolfo C, Mack P, Scagliotti GV, Aggarwal C, Arcila ME, Barlesi F, et al. Liquid biopsy for advanced NSCLC: a consensus statement from the international association for the study of lung cancer. J Thorac Oncol. 2021;16(10):1647–62.
Villaruz LC, Socinski MA, Weiss J. Guidance for clinicians and patients with non-small cell lung cancer in the time of precision medicine. Front Oncol. 2023;13:1124167.
Nadler E, Vasudevan A, Wang Y, Ogale S. Real-world patterns of biomarker testing and targeted therapy in de novo metastatic non-small cell lung cancer patients in the US oncology network. Cancer Treat Res Commun. 2022;31:100522.
Singal G, Miller PG, Agarwala V, Li G, Kaushik G, Backenroth D. et al. Association of patient characteristics and tumor genomics with clinical outcomes among patients with non-small cell lung cancer using a clinicogenomic database. JAMA. 2019;321(14):1391–9.
Kim ES, Velcheti V, Mekhail T, Yun C, Shagan SM, Hu S, et al. Blood-based tumor mutational burden as a biomarker for atezolizumab in non-small cell lung cancer: the phase 2 B-F1RST trial. Nat Med. 2022;28(5):939–45.
Sholl LM, Hirsch FR, Hwang D, Botling J, Lopez-Rios F, Bubendorf L, et al. The promises and challenges of tumor mutation burden as an immunotherapy biomarker: a perspective from the international association for the study of lung cancer pathology committee. J Thorac Oncol. 2020;15(9):1409–24.
Wu J, Liu Z, Huang T, Wang Y, Song MM, Song T, et al. Cerebrospinal fluid circulating tumor DNA depicts profiling of brain metastasis in NSCLC. Mol Oncol. 2022;17(5):810–24.
Park MK, Lim JM, Jeong J, Jang Y, Lee JW, Lee JC, et al. Deep-learning algorithm and concomitant biomarker identification for NSCLC prediction using multi-omics data integration. Biomolecules. 2022;12(12):1839.
Yin X, Liao H, Yun H, Lin N, Li S, Xiang Y, et al. Artificial intelligence-based prediction of clinical outcome in immunotherapy and targeted therapy of lung cancer. Semin Cancer Biol. 2022;86(Pt 2):146–59.
Smeltzer MP, Wynes MW, Lantuejoul S, Soo R, Ramalingam SS, Varella-Garcia M, et al. The international association for the study of lung cancer global survey on molecular testing in lung cancer. J Thorac Oncol. 2020;15(9):1434–48.
De Maglio G, Pasello G, Dono M, Fiorentino M, Follador A, Sciortino M, et al. The storm of NGS in NSCLC diagnostic-therapeutic pathway: how to sun the real clinical practice. Crit Rev Oncol Hematol. 2022;169:103561.
Lindeman NI, Cagle PT, Aisner DL, Arcila ME, Beasley MB, Bernicker EH, et al. Updated molecular testing guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors: guideline from the college of american pathologists, the international association for the study of lung cancer, and the association for molecular pathology. J Thorac Oncol. 2018;13(3):323–58.
Gross CP, Meyer CS, Ogale S, Kent M, Wong WB. Associations between medicaid insurance, biomarker testing, and outcomes in patients with advanced NSCLC. J Natl Compr Cancer Netw. 2022;20(5):479–87.e2.
Authorship.
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Editorial Assistance.
Editorial support was provided by Mark McCollum, PhD, of Nucleus Global and was funded by Pfizer.
Funding
The podcast and the journal's rapid service fee was funded by Pfizer.
Author information
Authors and Affiliations
Contributions
Fred R. Hirsch and Chul Kim made substantial contributions to the development of the podcast, critically reviewed and revised the podcast, and provided final approval of the podcast as submitted.
Corresponding author
Ethics declarations
Conflict of Interest
Fred Hirsch reports participation on advisory boards for Amgen, AstraZeneca, Blueprint, BMS, G1 Therapeutics, Genentech, Merus, NextCure, Novartis, Novocure, Regeneron, and Sanofi. Chul Kim reports institutional grants from AstraZeneca, BMS, Daiichi Sankyo, Debiopharm, Genentech, Janssen, Karyopharm, Lyell Immunopharma, Novartis, and Regeneron; and consulting fees from Arcus Biosciences, AstraZeneca, Daiichi Sankyo, Diffusion Pharmaceuticals, Eisai, Janssen, Jazz Pharmaceuticals, Mirati, Novartis, PierianDx, Regeneron, and Sanofi.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hirsch, F.R., Kim, C. The Importance of Biomarker Testing in the Treatment of Advanced Non-Small Cell Lung Cancer: A Podcast. Oncol Ther (2024). https://doi.org/10.1007/s40487-024-00271-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40487-024-00271-w