Abstract
Introduction
Ciltacabtagene autoleucel (cilta-cel), is a B-cell maturation antigen-directed, genetically modified autologous chimeric antigen receptor T-cell (CAR-T) immunotherapy. It is indicated for treatment for adult patients with relapsed or refractory multiple myeloma (RRMM) after four or more prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. The objective of this study was to estimate the per-patient US commercial healthcare costs related to cilta-cel (CARVYKTI®) CAR-T therapy (i.e., costs separate from cilta-cel therapy acquisition) for patients with RRMM.
Methods
US prescribing information for cilta-cel, publicly available data, and published literature were used with clinician input to identify the cost components and unit costs associated with administration of cilta-cel. Cost components included apheresis, bridging therapy, conditioning therapy, administration, and postinfusion monitoring for 1 year of follow-up. Adverse event (AE) management costs for all grades of cytokine release syndrome and neurologic toxicities, and additional AEs grade ≥ 3 occurring in > 5% of patients were included in the analysis.
Results
The estimated per-patient average costs of cilta-cel CAR-T therapy administered exclusively in an inpatient setting, excluding cilta-cel therapy acquisition costs, totaled US$160,933 over a 12 month period. Costs assuming different proportions of inpatient/outpatient administration (85%/15% and 70%/30%) were US$158,095 and US$155,257, respectively.
Conclusion
Cost estimates from this analysis, which disaggregates CAR-T therapy costs, provide a comprehensive view of the cost components of CAR-T therapy that can help healthcare decision-makers make informed choices regarding the use of cilta-cel. Real-world costs may differ with improved AE prevention and mitigation strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
This study sought to estimate the average per-patient US commercial healthcare costs related to cilta-cel (CARVYKTI®) chimeric antigen receptor T-cell (CAR-T) therapy (a complex, multi-step process taking up to several weeks from cell collection to administration) for patients with relapsed/refractory multiple myeloma (RRMM). |
Previously published studies have not examined the costs specific to cilta-cel CAR-T therapy, which was recently approved for use in patients with RRMM. |
What was learned from this study? |
The estimated per-patient average costs of cilta-cel therapy administered exclusively in an inpatient setting, excluding cilta-cel therapy acquisition costs, totaled US$160,933 over a 12 month period. |
Infusion of cilta-cel in an outpatient setting will reduce the per-patient average administration cost. |
A broad accounting of costs leads to a more comprehensive estimate of the cost of CAR-T therapy beyond drug acquisition costs. This information can aid in healthcare decision-making. |
Introduction
Ciltacabtagene autoleucel (cilta-cel), a chimeric antigen receptor T-cell (CAR-T) therapy, is a B-cell maturation antigen (BCMA)-directed genetically modified autologous T-cell immunotherapy indicated in the USA for the treatment of adult patients with relapsed or refractory multiple myeloma (RRMM) after four or more prior lines of therapy, including a proteasome inhibitor (PI), an immunomodulatory agent (IMiD), and an anti-CD38 monoclonal antibody [1].
While cilta-cel CAR-T therapy is administered as a single infusion [1], it is a complex, multi-step process taking up to several weeks from cell collection (apheresis) to administration. For many patients, bridging therapy, typically consisting of a combination of antimyeloma agents, is administered during the cell manufacturing period for stabilization of disease. In the days leading up to treatment, patients are given a conditioning regimen (lymphodepleting chemotherapy) to deplete existing T cells and enhance expansion and engraftment of CAR-T cells [2]. Administration of CAR-T is typically done in an inpatient setting; however, due to a delayed onset of cytokine release syndrome (CRS), cilta-cel CAR-T offers additional flexibility enabling administration in an outpatient setting with subsequent follow-up visits for monitoring [3].
Recent studies estimated additional costs associated with CAR-T therapy beyond the treatment acquisition costs of the CAR-T treatment (e.g., costs of conditioning therapy and apheresis) that need to be considered; however, these estimates either capture a partial accounting of the costs associated with CAR-T therapy [4, 5] or lack the granularity [6] necessary for healthcare payers and other stakeholders to make informed healthcare decisions. In addition, previously published studies have not examined the costs specific to cilta-cel CAR-T therapy, which was recently approved for use in patients with RRMM.
This study estimated per-patient average US healthcare costs related to cilta-cel therapy (i.e., costs separate from cilta-cel acquisition) for patients with RRMM beginning with pre-infusion cost components through 1 year of postinfusion monitoring. We examined costs when cilta-cel is administered in an inpatient setting and scenarios assuming inpatient/outpatient infusion rates of 85%/15% and 70%/30%. Additional scenarios examined the impact of varying the percentage of patients receiving bridging therapy. Details of the costing can be utilized in additional CAR-T pharmacoeconomic studies.
Methods
Study Population
The patient population was based on the CARTITUDE-1 trial (registered at ClinicalTrials.gov as NCT03548207), a phase IB/II clinical trial evaluating the efficacy and safety of cilta-cel CAR-T among patients with RRMM, who received cilta-cel CAR-T infusion, i.e., a modified intention-to-treat (mITT) population. A total of 113 patients with RRMM with prior exposure to a PI, an IMiD, and an anti-CD38 monoclonal antibody underwent apheresis [intention-to-treat (ITT) population] and 97 (85.8%) received cilta-cel CAR-T therapy. Sixteen patients with RRMM underwent apheresis but did not ultimately receive CAR-T therapy. Primary reasons for not receiving therapy included pre-infusion mortality, disease progression, and patient/physician decision [3]. Micromedex RED BOOK, a commercially licensed database [11] and the CMS 2021 Physician Fee Schedule, a publicly available database [10], were used to calculate costs in this study. No patient level data were used in the analyses and no institutional review board (IRB) approval was needed.
Costs and Resource Utilization
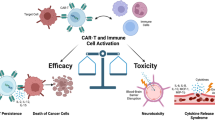
Costs are presented in 2021 US dollars (USD) from the perspective of a commercial payer with Medicare-eligible members and are limited to direct medical costs. Cost components were identified for three phases of CAR-T therapy: pre-, peri-, and postinfusion (Fig. 1). Management of adverse events (AEs) associated with cilta-cel infusion were considered as a separate cost component. US prescribing information (USPI) for cilta-cel [1], clinical trial data [7], publicly-available medical cost databases (discussed in detail below) [8,9,10,11], and published literature [12] were used to identify the cost components and unit costs.
To address gaps in the literature surrounding healthcare resource utilization (HCRU) in the treatment of RRMM with CAR-T, a double blinded Delphi panel of clinical experts was convened [13, 14]. One of the primary objectives of the panel (Study Delphi Panel) was to gain consensus on HCRU associated with CAR-T therapy for RRMM. The method used a two-phase process, following established Delphi methods [13, 14]. The details of the methodology are described in the supplementary materials (Supplementary Materials Table 1).
Pre-infusion
Pre-infusion costs included apheresis, bridging therapy, and conditioning chemotherapy costs (Table 1). We assumed outpatient site of care for all pre-infusion procedures. The cost of apheresis was sourced from the CMS 2021 Physician Fee Schedule, a publicly available database [10].
There is no single standard of care for bridging therapy, with chosen treatments generally based on physician choice and specific to patient needs [2]. In our base case analysis, the proportion of patients receiving bridging therapy, 75.26%, is based on the CARTITUDE-1 trial. In all analyses, bridging therapy costs were accrued for 3 weeks based on clinician expert opinion from the Study Delphi Panel. Weekly bridging therapy costs were based on the average of ten non-CAR-T RRMM regimens weighted by market share [11].
It was assumed all patients received lymphodepleting chemotherapy in an outpatient setting as a conditioning therapy. Conditioning therapy comprised 30 mg/m2 fludarabine and 300 mg/m2 cyclophosphamide infusions administered for 3 days based on the cilta-cel clinical trial protocol [7], consistent with the USPI for CARVYKTI® [1]. Baseline surface area (BSA) was assumed to be 1.87 m2 [15].
The acquisition costs of bridging therapy and conditioning chemotherapy were the wholesale acquisition cost prices sourced from Micromedex RED BOOK, a commercially licensed database [11]. Infusion costs were sourced from the CMS 2021 Physician Fee Schedule [10].
Peri-infusion
Peri-infusion costs included inpatient hospital days and outpatient visits (Table 1). The primary analysis assumed 100% inpatient administration of cilta-cel. Average length of inpatient stay was assumed to be 7 days, and any extended inpatient stays resulting from CRS are accounted for in AE costs, which are separately costed. In CARTITUDE-1, the median number of days to onset of CRS symptoms in patients who received a cilta-cel CAR-T infusion and subsequently developed CRS was 7 days [1].
Scenario analyses were also conducted assessing 85%/15% and 70%/30% inpatient/outpatient cilta-cel infusion administration. For the outpatient dosing in each scenario, it was assumed patients incurred 1 day of hospitalization costs for the day of the infusion. Additional hospitalization time and costs would be associated with AEs (discussed below). The number of outpatient visits immediately following infusion in both administration settings (7 visits in the inpatient setting and 11 visits in the outpatient setting; Table 1) were based on clinician expert opinion from the Study Delphi Panel.
Cost per inpatient day was sourced from an Agency for Healthcare Resource and Quality (AHRQ) statistical brief [9], as cited in a published evaluation of CAR-T therapies [16], and inflated to 2021 values using the medical care component of the Consumer Price Index (CPI) from the US Bureau of Labor Statistics (BLS) [17]. Cost per outpatient visit was from the CMS physician fee schedule, the standard source use for outpatient costs [10].
Postinfusion
Postinfusion costs included 100-day postinfusion monitoring costs and additional infusion monitoring costs required in the remainder of the first year (Table 1). Utilization of 100-day and subsequent first-year monitoring resources was based on clinician expert opinion from the Study Delphi Panel. Briefly, the analysis assumed 100-day monitoring comprised twice weekly outpatient visits, laboratory testing frequency of two to three times per week for the first month followed by less frequent testing, and one bone marrow biopsy. Subsequent first-year monitoring comprised once-monthly outpatient visits and laboratory testing. Monitoring resource costs were sourced from the CMS 2021 physician fee schedule [10]. Resource use and unit costs are detailed in Supplementary Materials Table 2. Postinfusion monitoring cost components with unit costs and resource utilization are also presented in Supplementary Materials Table 2.
Adverse Events
Adverse event costs included costs of managing AEs of interest associated with cilta-cel therapy, including hospitalization when required (Table 2). All grades of cytokine release syndrome (CRS) and neurologic toxicity AEs were included in the analysis. Additional AEs of interest included in the analysis were grade ≥ 3 AEs occurring in > 5% of patients receiving a cilta-cel infusion sourced from the cilta-cel USPI, which reflected a median duration of follow-up of 18 months [1]. CRS and neurologic toxicity AE costs were derived from a published study, using the assumption that grade ≥ 3 CRS events with hemophagocytic lymphohistiocytosis/macrophage activation syndrome (HLH) had similar costs to grade 4 CRS [12]. All other AE costs were retrieved from the AHRQ Healthcare Cost and Utilization Project website [8]. All costs were inflated to 2021 values using the medical care component of the US BLS CPI [17].
Additional Scenario Analysis
Two sets of scenarios were explored in addition to the scenarios varying cilta-cel administration setting. In scenario A, the percent of patients receiving bridging therapy was increased to 100%. All other assumptions were identical to the base case.
Currently, there are two CAR-T therapies (cilta-cel and ide-cel) approved for patients with RRMM, and these two clinical trials reported different bridging therapy rates [7, 18]. In scenario B, we estimated the impact of changing the bridging therapy rate on cilta-cel administration cost by increasing the rate from 75.26% in the cilta-cel trial to 82.20%, the weighted average of the bridging therapy use rates from the two CAR-T clinical trials [7, 18].
The impact of 15% and 30% of patients receiving outpatient infusions were also explored in scenarios A and B.
Results
The estimated per-patient average costs of CAR-T therapy with cilta-cel administered exclusively in an inpatient facility (excluding cilta-cel therapy acquisition costs) in our primary (base case) analysis totaled $160,933, which included the 12-month follow-up period postinfusion (Fig. 2). Pre-infusion costs including apheresis, bridging therapy, and conditioning therapy totaled $18,268. Peri-infusion costs exclusive of drug acquisition, totaled $23,154. Postinfusion monitoring costs through the end of the first year following CAR-T therapy totaled $4584. The cost of AE management totaled $114,928 (Table 3).
The per-patient cost of cilta-cel infusion in an outpatient setting was estimated to be $18,922 lower ($4232 versus $23,154) than inpatient infusion cost (Table 1), which would lead to an estimated total per-patient cost of $142,012. Total costs assuming 85%/15% and 70%/30% inpatient/outpatient administration were $158,095 and $155,257, respectively (Table 3). Cost reductions were driven solely by reductions in peri-infusion costs, which were attributable to lower per-patient inpatient days.
Scenarios that increased the percent of patients receiving bridging therapy increased the estimated total cost of CAR-T therapy. Assuming 100% of patients received bridging therapy increased the estimated per-patient average costs of CAR-T cilta-cel therapy to $165,861 (Supplementary Materials Table 3). Assuming 82.2% bridging therapy, the average bridging therapy use in RRMM clinical trials for two CAR-T products [7, 18], increased the estimated per-patient average costs of CAR-T cilta-cel therapy to $162,316. Administering a proportion of cilta-cel infusions in an outpatient setting lowered the average per-patient costs in each of these scenarios by $2838 assuming 85%/15% inpatient/outpatient administration and $5677 assuming 70%/30% inpatient/outpatient administration (Supplementary Materials Table 3).
Discussion
This study analyzed non-CAR-T components that contribute to the cost of cilta-cel CAR-T therapy over three phases of the CAR-T process: pre-infusion, peri-infusion, and postinfusion. Postinfusion included monitoring costs for 1 year following initiation of CAR-T therapy. The cost analysis also included management of AEs following CAR-T therapy (Fig. 1). We used publicly available information and input from an internal Delphi panel of clinical experts for this study to inform our analyses.
Pre-infusion costs were driven by the cost of bridging therapy, which is administered to prevent or treat rapid clinical progression while awaiting CAR-T infusion [2]. The length of bridging therapy administration varies but generally takes 2–4 weeks, although it can extend longer based on factors related to product cell expansion rate during manufacturing and logistical factors such as treatment planning [19]. Our analysis assumed 3 weeks of bridging therapy from the Study Delphi Panel for a total estimated costs of $19,915. A longer interval of bridging therapy would lead to higher costs. Increasing the proportion of patients that receive bridging therapy also leads to higher costs. If the percentage of patients using bridging therapy was similar to the average of patients with RRMM using bridging therapy in two CAR-T trials (82.2%) [7, 18], the estimated average per patient total cost of CAR-T therapy would increase by $1382. If all patients received bridging therapy, the estimated average per patient total cost of CAR-T cilta-cel therapy would increase by $4927; however, similar costs would likely also be incurred by patients with RRMM who receive standard of care.
Peri-infusion costs were driven by inpatient hospitalization costs. In the primary analysis, we assumed that 100% of patients were administered cilta-cel in an inpatient setting. We presented scenario analyses assuming variable outpatient administration of CAR-T (15% and 30% of patients) to demonstrate the impact of administration setting on overall costs for the CAR-T components. Cilta-cel provides flexibility for outpatient administration due to delayed onset of CRS events. Outpatient CAR-T administration with frequent monitoring and early intervention can provide a mechanism to decrease healthcare costs by reducing the length of inpatient hospitalization following CAR-T therapy [20]. These analyses demonstrate that outpatient administration of cilta-cel CAR-T therapy could lead to decreased per patient peri-infusion costs ($4232 for outpatient administration versus $23,154 inpatient administration per patient; Table 1), and lower overall costs of CAR-T therapy, as well as reduced HCRU associated with hospitalization during the peri-infusion phase.
The estimated cost to treat CRS and neurologic toxicity AEs related to cilta-cel CAR-T therapy based on the weighted average of all grades of events contributed $35,103 (30.5%) of the AE management costs. The cumulative costs of other grade ≥ 3 AEs occurring at > 5% in patients receiving cilta-cel included in our analysis ($79,825) were higher than CRS and neurotoxicity events of any grade, demonstrating the importance of including a more complete accounting of severe AE management. Of note is that the AE rates used in this estimation were obtained from the CARTITUDE-1 trial as reported in the USPI [1] and may not be a reflection of real-world AEs. Additionally, once physicians have a better understanding of how to prevent some AEs and/or monitor and manage these events more proactively at a lower level of severity, HCRU and AE costs may be lowered [21]. For example, a recent publication on the incidence and management of CAR-T neurotoxicity in patients in the cilta-cel program documented the success of implementation of monitoring and patient strategies on movement and neurocognitive treatment events (MNTs), which had a median time of onset of 27 days in CARTITUDE-1. After implementation of proactive strategies to monitor and manage patients with MNTs, the overall incidence of MNTs decreased to < 1% among 150 patients subsequently dosed across the cilta-cel program (from 5% reported in CARTITUDE-1) [22].
Our estimated per-patient average costs of cilta-cel CAR-T therapy totaled $160,933, excluding the acquisition cost of cilta-cel, which had a 2022 wholesale acquisition cost of $465,000 [23]. The estimated $160,933 costs exclusive of acquisition costs correspond to 25.7% of the total costs ($160,933 + $465,000 = $625,933). The average per-patient US commercial healthcare costs related to cilta-cel therapy presented in this study are reflective of patients who actually receive cilta-cel, i.e., an mITT population. In the CARTITUDE-1 trial, 16 of 113 patients (14.2%) did not receive cilta-cel therapy. Based on trial data, these patients would incur apheresis costs ($112), and a subset would receive bridging therapy (75.3% of $19,915) and conditioning therapy (25.0% of $3168) costs. The average per-patient costs would total $15,891 for patients not receiving cilta-cel therapy. These are real additional costs from the healthcare payer’s perspective, and reflect additional costs associated with utilization of cilta-cel therapy not included in the study results. Note that patients who had apheresis and did not continue to CAR-T therapy would likely experience costs similar to the bridging therapy costs in the absence of intention to treat with CAR-T.
Several other studies have estimated costs associated with CAR-T immunotherapies for other indications [4,5,6]. Our estimated costs of CAR-T therapy are higher than costs of CAR-T therapy reported by both Hernandez et al. [4] and Lyman et al. [5]. Hernandez et al. [4] reports costs of CAR-T therapy exclusive of drug acquisition cost of $30,000 to $56,000 per patient; Lyman et al. [5] reports costs of $23,526 to $53,360 per patient, depending on the site of care. Similar to our study, both studies included conditioning costs and administration costs associated with CAR-T. Hernandez et al. [4] also included apheresis costs. Neither study, however, included bridging therapy. More significantly, both studies focused on more limited AE management costs (primarily focusing on CRS and/or neurotoxicity); however, AE profiles of all RRMM treatments include other grade ≥ 3 AEs. Our base case analysis included costs associated with the management of all grades of CRS and neurologic toxicity AEs. In addition, we included all grade ≥ 3 AEs that occurred in more than 5% of patients treated with cilta-cel in the CARTITUDE-1 trial reported in the prescribing information [1], which increased the estimated cost of this CAR-T therapy in our study.
Our costs are slightly lower than estimates presented by Sahli et al. [6] of the nondrug portion of total cost of care associated with CAR-T therapy indicated for relapsed or refractory B-cell lymphoma ($184,337). The estimates presented by Sahli et al. are based on an integrated pharmacy and medical commercial claims data analysis. Sahli et al. [6], however, only present aggregated costs for the nondrug component of CAR-T therapy. Since nondrug costs are not further disaggregated it is not possible to compare the results of Sahli et al. to the component costs of our study.
There are some limitations to our analyses. Because there are limited published real-world data on resource use associated with CAR-T therapy for RRMM, we used inputs from a Delphi survey and panel to inform our analysis. We assumed an outpatient site of care for all pre-infusion procedures. The Study Delphi Panel noted that during the COVID pandemic, patients received lymphodepleting conditioning therapy in an inpatient setting to decrease infection risk, which would lead to slightly higher total costs. In addition, our analysis did not include the costs of patients identified as potential CAR-T therapy patients who undergo apheresis but do not eventually receive CAR-T therapy. AE rates used in our analysis were based on USPI-reported clinical trial data [1] and may not be reflective of real-world rates with additional AE mitigation strategies [21], which could lead to lower costs. In addition, we assume each event occurs and is costed independently; however, there may be a single treatment or hospitalization for concurrent AEs that could lead to lower costs. We did not include costs associated with AEs that may occur during apheresis or conditioning therapy that manifest prior to CAR-T therapy.
Our analysis focuses on the average per-patient US commercial healthcare costs related to cilta-cel therapy for RRMM. CAR-T therapies for other indications or used in different countries, may have differences in the proportion of the patients using bridging therapy, different conditioning therapies, or differences in administration setting that contribute to cost differences. In addition, difference in AE rates among different CAR-T therapies and patient populations may also lead to cost differences. Our scenario analyses demonstrate the cost sensitivity of varying two of the parameters, bridging therapy and administration setting. Although our focus is on cilta-cel therapy in the USA, we believe our study is holistic and of value broadly to healthcare decision-makers because the approach used in our analysis, with detailed cost categories across phases of therapy, can be used to calculate costs of comparators or cilta-cel therapy in other markets.
Conclusion
This analysis estimated per-patient costs associated with the use of cilta-cel CAR-T treatment in patients with RRMM from pre-infusion through 1 year of postinfusion monitoring. Our broad accounting of healthcare costs associated with cilta-cel leads to a more comprehensive estimate of the cost of CAR-T therapy beyond drug acquisition. Results from this holistic analysis provide detailed information that can be used by healthcare decision-makers to make more informed choices specific to cilta-cel CAR-T.
References
Janssen Pharmaceutical Companies. CARVYKTI® (ciltacabtagene autoleucel) suspension for intravenous infusion. US Prescribing Information. [Internet]. 2022. https://carvyktirems.com/ResourceDownloadRaw/PrescribingInformation/attachment. Accessed 1 July 2022.
Amini L, Silbert SK, Maude SL, Nastoupil LJ, Ramos CA, Brentjens RJ, et al. Preparing for CAR T cell therapy: patient selection, bridging therapies and lymphodepletion. Nat Rev Clin Oncol. 2022;19:342–55.
Berdeja JG, Madduri D, Usmani SZ, Jakubowiak A, Agha M, Cohen AD, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398:314–24.
Hernandez I, Prasad V, Gellad WF. Total costs of chimeric antigen receptor T-cell immunotherapy. JAMA Oncol. 2018;4:994–6.
Lyman GH, Nguyen A, Snyder S, Gitlin M, Chung KC. Economic evaluation of chimeric antigen receptor T-cell therapy by site of care among patients with relapsed or refractory large B-cell lymphoma. JAMA Netw Open. 2020;3: e202072.
Sahli B, Eckwright D, Darling E, Gleason PP, Leach JW. Chimeric antigen receptor T-cell therapy real-world assessment of total cost of care and clinical events for the treatment of relapsed or refractory lymphoma. JCO. 2021;39:e19500.
Madduri D, Bredeja J, Usmani SZ, Jakubowiak AJ, Agha M, Cohen A, et al. CARTITUDE-1: phase 1b/2 study of ciltacabtagene autoleucel, a B-cell maturation antigen–directed chimeric antigen receptor T cell therapy, in relapsed/refractory multiple myeloma. ASH; 2020 [cited 2021 July 8]. https://ash.confex.com/ash/2020/webprogram/Paper136307.html. Accessed 8 July 2021
Agency for Healthcare Research and Quality (AHRQ). Healthcare cost and utilization project (HCUPnet) [Internet]. 2021 [cited 2021 Aug 3]. https://hcupnet.ahrq.gov/#setup. Accessed 3 Aug 2021.
Agency for Healthcare Research and Quality (AHRQ). Statistical brief #125: cancer hospitalizations for adults, 2009. [Internet]. 2012 [cited 2021 Aug 31]. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb125.jsp. Accessed 31 Aug 2021.
Centers for Medicare and Medicaid Services (CMS). Physician fee schedule search [Internet]. 2021 [cited 2021 June 29]. https://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx. Accessed 29 June 2021.
Truven Health Analytics. RED BOOK Online® 2021 Pricing [Internet]. 2021 [cited 2021 June 29]. http://www.micromedexsolutions.com. Accessed 29 June 2021.
Hari P, Nguyen A, Pelletier C, McGarvey N, Gitlin M, Parikh K. Healthcare resource utilization and economic burden of cytokine release syndrome (CRS) and neurologic events (NE) in patients (pts) with relapsed/refractory multiple myeloma (RRMM) receiving idecabtagene vicleucel (ide-cel, bb2121) in KarMMa. JCO. 2020;38:61.
Hsu C-C, Sandford B. The Delphi technique: making sense of consensus. Practical assessment, research, and evaluation [Internet]. 2019;12. https://scholarworks.umass.edu/pare/vol12/iss1/10. Accessed 6 May 2022.
Nasa P, Jain R, Juneja D. Delphi methodology in healthcare research: how to decide its appropriateness. World J Methodol. 2021;11:116–29.
Fau J-B, El-Cheikh R, Brillac C, Koiwai K, Mace N, Campana F, et al. Drug-disease interaction and time-dependent population pharmacokinetics of isatuximab in relapsed/refractory multiple myeloma patients. CPT Pharmacomet Syst Pharmacol. 2020;9:649–58.
Institute for Clinical and Economic Review. Anti B-cell maturation antigen CAR T-cell and antibody drug conjugate therapy for heavily pre-treated relapsed and refractory multiple myeloma: final report. [Internet]. 2021 [cited 2021 Aug 31]. https://icer.org/wp-content/uploads/2020/10/ICER_Multiple-Myeloma_Final-Report_Update_09102021.pdf. Accessed 31 Aug 2021.
US Bureau of Labor Statistics. Consumer Price Index (CPI) for all urban consumers, US city average, medical care [Internet]. [cited 2021 July 21]. https://www.bls.gov/data/. Accessed 21 July 2021.
Munshi NC, Anderson LD, Shah N, Madduri D, Berdeja J, Lonial S, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384:705–16.
Perica K, Curran KJ, Brentjens RJ, Giralt SA. Building a CAR garage: preparing for the delivery of commercial CAR T cell products at Memorial Sloan Kettering Cancer Center. Biol Blood Marrow Transplant. 2018;24:1135–41.
McGann M, Davis JA, Gaffney KJ, Smith D, Edwards K, Hess BT, et al. Real-world experience and optimization of outpatient chimeric antigen receptor T cell therapy. Transplant Cell Ther. 2022;28:583–85.
Alexander M, Culos K, Roddy J, Shaw JR, Bachmeier C, Shigle TL, et al. Chimeric antigen receptor T cell therapy: a comprehensive review of clinical efficacy, toxicity, and best practices for outpatient administration. Transplant Cell Ther. 2021;27:558–70.
Cohen AD, Parekh S, Santomasso BD, Gállego Pérez-Larraya J, van de Donk NWCJ, Arnulf B, et al. Incidence and management of CAR-T neurotoxicity in patients with multiple myeloma treated with ciltacabtagene autoleucel in CARTITUDE studies. Blood Cancer J. 2022;12:32.
National Cancer Institute. Carvykti approval marks second CAR T-cell therapy for multiple myeloma [Internet]. [cited 2022 Dec 15]. https://www.cancer.gov/news-events/cancer-currents-blog/2022/fda-carvykti-multiple-myeloma.
Acknowledgements
Funding
Sponsorship for this study and its publication, including the journal’s Rapid Service Fee, were funded by Janssen Scientific Affairs, LLC and Legend Biotech, Inc. Medical writing and editorial support were funded by Janssen Scientific Affairs, LLC and Legend Biotech, Inc.
Medical Writing/Editorial Assistance
Medical writing and editorial support were provided by Pamela Martin of Medical Decision Modeling Inc., and were funded by Janssen Scientific Affairs, LLC and Legend Biotech, Inc.
Author Contributions
All named authors (Sundar Jagannath, Nedra Joseph, Concetta Crivera, Akshay Kharat, Carolyn C. Jackson, Satish Valluri, Patricia Cost, Hilary Phelps, Rafal Slowik, Timothy Klein, Lee Smolen, Xueting Yu, and Adam D. Cohen) contributed to concept, design, and data interpretation. All named authors contributed to drafting of the manuscript. All named authors meet the International Committee of Medical Journal (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Sundar Jagannath is an employee of Icahn School of Medicine at Mount Sinai, New York, NY, USA, who received funding from Janssen to assist in the study. Nedra Joseph, Concetta Crivera, and Akshay Kharat are employees of Janssen Scientific Affairs, LLC, and current equity holders in a publicly traded company. Carolyn C. Jackson is an employee of Janssen R&D and a physician consultant at Memorial Sloan Kettering Cancer Center, New York, NY, USA. Satish Valluri, Patricia Cost, and Rafal Slowik are employees of Janssen Global Services, LLC, and current equity holders in a publicly traded company. Hilary Phelps was an employee of Janssen Global Services, LLC during the project and is now an independent contractor. Timothy Klein, Lee Smolen, and Xueting Yu are employees of Medical Decision Modeling Inc., who received funding from Janssen to conduct the study. Adam D. Cohen is an employee of University of Pennsylvania, Philadelphia, PA, USA, and reports receiving consulting/advisory board fees from Janssen, Takeda, GSK, Genentech/Roche, BMS/Celgene, AstraZeneca, Oncopeptides, Pfizer, Abbvie, Ichnos, Arcellx; research support (personal) from GSK and Novartis; research support (institutional) from Janssen; and patents/royalties from Novartis.
Compliance with Ethics Guidelines
Micromedex RED BOOK, a commercially licensed database [11] and the CMS 2021 Physician Fee Schedule, a publicly available database [10], were used to calculate costs in this study. No patient level data were used in the analyses and no IRB approval was needed.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jagannath, S., Joseph, N., Crivera, C. et al. Component Costs of CAR-T Therapy in Addition to Treatment Acquisition Costs in Patients with Multiple Myeloma. Oncol Ther 11, 263–275 (2023). https://doi.org/10.1007/s40487-023-00228-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-023-00228-5