Abstract
Introduction
Gastroenteropancreatic neuroendocrine tumors (GEP-NETs) can result in symptoms such as diarrhea, flushing, abdominal pain, and fatigue and are often associated with a significant disease burden and poor prognosis. This non-interventional, prospective, observational study evaluated the real-world safety and effectiveness of lanreotide depot, a somatostatin analog (SSA) used to treat GEP-NETs, in a community setting.
Methods
In this prospective, non-interventional study (NCT02730104), adult patients with locally advanced (inoperable), metastatic GEP-NETs treated with lanreotide depot were evaluated by their physician every 6 months from enrollment for 24 months. Clinically defined time to disease progression (TTDP) and overall survival (OS) were estimated for the total population and by primary tumor type (gastrointestinal [GI], pancreatic, unknown origin), and an exploratory analysis determined the rate of progression-free survival (PFS) at 12 and 24 months. Patient satisfaction was evaluated via the Treatment Satisfaction Questionnaire for Medication (TSQM-9), and safety information was recorded.
Results
Of 99 patients, the 24-month PFS rate was 73.7% (95% confidence interval [CI] 63.1–81.7) and 24-month OS rate was 84.2% (95% CI 74.0–90.7). Median TTDP was not reached because few patients experienced disease progression during the study period. The majority of responding patients expressed satisfaction with treatment on each domain of the TSQM-9. Treatment-related adverse events (AEs) occurred in 19.2% of patients, while no serious AEs (SAEs) were related to the study drug.
Conclusions
Lanreotide depot is an effective and well-tolerated treatment for GEP-NETs in the real-world community setting.
Trial registration
ClinicalTrials.gov identifier, NCT02730104.
Plain Language Summary
Gastroenteropancreatic neuroendocrine tumors (GEP-NETs) are rare tumors that develop in the gut or pancreas. GEP-NETs may lead to a reduced lifespan, and people with GEP-NETs may have symptoms such as fatigue, muscle weakness, diarrhea, stomach pain/cramping, and skin reactions. One approved treatment for patients whose tumor cannot be removed with surgery is lanreotide depot. Clinical trials have found lanreotide depot to be effective at prolonging survival and managing symptoms in people with GEP-NETs. However, clinical trials take place under very strict conditions and often do not represent all people with a certain disease in the ‘real world’. It is important to determine whether treatments are still effective when used outside of clinical trials. This study was conducted in the real world and followed 99 people with GEP-NETs whose physicians were treating them with lanreotide depot. Each person was monitored for 24 months and assessed during check-ups by their physician every 6 months. After 24 months, 73.7% of people did not have progression (worsening) of disease. The percentage of people who had not died by the end of the study was 84.2%. Most patients (91.6%) said they were satisfied with their treatment. Only 19.2% of patients experienced side effects, none of which were serious.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Gastroenteropancreatic neuroendocrine tumors (GEP-NETs) are rare malignancies frequently diagnosed as locally advanced or metastatic, which can substantially impact patients’ health and quality of life. |
Somatostatin analogs such as lanreotide depot are recommended as the first-line medical treatment for GEP-NETs and have demonstrated efficacy in clinical trials; however, real-world evidence studies, which provide a more accurate representation of the overall patient population and their clinical management, are limited. |
This prospective, observational study aimed to evaluate the effectiveness and tolerability of lanreotide depot to treat patients with GEP-NETs in a real-world, community setting. |
What was learned from the study? |
Patients with GEP-NETs receiving treatment with lanreotide depot had a high rate of progression-free survival and overall survival and no serious adverse events related to the study drug; the majority of patients expressed satisfaction with treatment. |
The findings from this real-world study align with data from clinical trials and provide unique insight into the use of lanreotide depot in clinical practice, indicating that lanreotide depot is an effective and well-tolerated treatment for managing GEP-NETs and associated symptoms in patients receiving care in a community setting. |
Introduction
Neuroendocrine tumors (NETs) are a group of rare malignancies arising from cells throughout the endocrine system, with an annual age-adjusted incidence of 6.98 per 100,000 people as of 2012 [1, 2]. Of all NETs, approximately 60% originate either in the gastrointestinal system (stomach, small and large intestine, colon, rectum, appendix) or the pancreas, and are known collectively as gastroenteropancreatic (GEP)-NETs [3, 4]. Approximately 30% of GEP-NETs are considered to be functional tumors, characterized by hypersecretion of bioactive peptides and neuroamines leading to a range of hormone-associated symptoms such as general fatigue and muscle weakness, diarrhea, abdominal pain/cramping, skin reactions such as flushing, and, in some cases, cardiac valve fibrosis [2, 5,6,7,8,9]. However, many GEP-NETs are asymptomatic or non-specifically symptomatic; as such, most are diagnosed as locally advanced or metastatic [8, 10,11,12,13]. There is a need for safe and effective treatments to manage tumor growth and prolong progression-free survival (PFS) in patients with unresectable, metastatic GEP-NETs.
Somatostatin analogs (SSAs) are recommended for the treatment of hormone-related symptoms associated with NETs, and as a first-line option for the treatment of unresectable, metastatic GEP-NETs, according to the National Comprehensive Care Network (NCCN) treatment guidelines [2]. Lanreotide depot is an SSA indicated for the treatment of patients with GEP-NETs, with an approved dosing regimen of 120 mg every 28 days by deep subcutaneous injections [14]. The randomized, phase 3 CLARINET study demonstrated that PFS was significantly prolonged in patients treated with lanreotide depot compared with placebo [15].
Although clinical trials provide valuable objective information on the efficacy and safety of therapeutic agents, they often have very specific eligibility criteria. As a result, patients enrolled in clinical trials may not be representative of patients in the community setting. Real-world evidence (RWE) demonstrates the effectiveness and tolerability of treatments when they are used in clinical practice. In recent years, the Food and Drug Administration (FDA) has explored the potential benefits of using RWE as a key part of regulatory decisions regarding drug product effectiveness and safety [16]. However, RWE currently available on SSA utilization in the US consists largely of retrospective data, leaving a need for prospective real-world data [17, 18]. This non-interventional, prospective, observational study investigated the real-world effectiveness of lanreotide depot in patients with locally advanced or metastatic well-differentiated GEP-NETs in a US community oncology setting.
Methods
Study Design and Endpoints
This prospective, non-interventional, observational study (NCT02730104) enrolled adult patients with locally advanced (inoperable), metastatic GEP-NETs treated with lanreotide depot 120 mg every 4 weeks in a US community oncology setting. Due to the observational nature of the study, the decision to prescribe lanreotide depot was required to have been made prior to, and independently from, the decision to enroll a patient in the study. Patients ≥ 18 years of age were enrolled in the study if they either planned to receive lanreotide depot or were already receiving lanreotide depot, provided that they had not experienced disease progression from the initiation of treatment. Patients were followed for a total duration of 24 months from the date of lanreotide depot initiation, regardless of whether treatment initiation occurred prior to or after enrollment in the study. Complete inclusion and exclusion criteria can be found in Supplementary Table 1.
The primary endpoint was clinically defined time to disease progression (TTDP). An exploratory analysis additionally assessed the PFS rates 12 and 24 months after lanreotide depot initiation, evaluated using Kaplan–Meier estimates. Progression was defined as at least one of the following: tumor growth (radiographic progression), new sites of metastatic disease, worsening clinical symptoms, or disease-related death, in conjunction with a treatment change: treatment modification (dose increase, regimen change), treatment discontinuation, or additional/other NET therapeutic intervention.
The secondary endpoints were rate of overall survival (OS) after 12 and 24 months and patient satisfaction with treatment via the Treatment Satisfaction Questionnaire for Medication (TSQM-9) [19]. TTDP, PFS, and OS were evaluated for the total study population as well as for subgroups based on primary tumor site. A safety analysis summarized treatment emergent adverse events (TEAEs) for all patients who received at least one dose of the study drug; all AEs considered to be related to lanreotide depot and all serious AEs (SAEs) were documented in the electronic case report form (eCRF) and reported to Ipsen Biopharmaceuticals. Patients were to be evaluated by their treating physician at a minimum of every 6 months from enrollment or initiation of lanreotide depot over a 24-month period, or more frequently, as best reflected routine clinical practice. If patients switched to a new anticancer therapy prior to disease progression or death (e.g., due to medication intolerance), they were censored and withdrawn from the study from the date of new treatment initiation. Patient demographics, including medical history, were collected at baseline upon study entry. Clinical characteristics were assessed and collected at each patient visit as appropriate; among these were radiologic assessment of disease progression, which was evaluated every 6 months, and AEs.
Statistical Analysis
Statistical analyses were performed by US Oncology Research in accordance with International Conference on Harmonization (ICH E9) guidelines, based on the pooled data from individual study sites. The planned sample size, 100 patients, was based on prior experience in conducting similar studies [20, 21]. Descriptive statistics, including mean, standard deviation, median, minimum, and maximum values, are presented for continuous variables, while numbers and percentages are presented for categorical variables. The Kaplan–Meier estimate was used for median TTDP, PFS, and OS, where the index date was the initiation of treatment with lanreotide depot, with patients then followed for a duration of 24 months. At each study visit, patients were given the opportunity to use the TSQM-9 to self-report treatment satisfaction on a seven-point scale from ‘Extremely Dissatisfied’ to ‘Extremely Satisfied’ across nine domains, covering aspects of treatment including convenience, effectiveness, and overall satisfaction with the medication. The scores were summarized using the worst score for each patient (in case a patient completed multiple questionnaires during a single visit) across all study visits, and descriptive statistics were applied. AEs were graded according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE version 4.03) [22]. Incidence and type of AEs, including SAEs, were tabulated and summarized using descriptive statistics. All statistical analyses were performed using Statistical Analysis System (SAS) version 9.4 (Cary, NC, USA) [23].
Compliance with Ethics Guidelines
This study was non-interventional and therefore fell outside the scope of the European Union (EU) Directive 2001/20/EC and the EU Directive 2005/28/EC. As required by applicable local regulations, all legal regulatory aspects were covered, and approval was obtained from the appropriate regulatory bodies prior to study initiation. This study adhered to all local regulatory requirements applicable to non-interventional studies. Before initiating the study, written and dated approval/favorable opinion were obtained from the Independent Ethics Committee (IEC)/Institutional Review Board (IRB).
This study complied with the EU Directive 95/46/EC of the European Parliament, and of the Council of 24 October 1995 on the protection of individuals with regards to the processing of personal data and on the free movement of such data. This study also followed the recommendations from the International Society for Pharmacoepidemiology (ISPE), Good Pharmacoepidemiological Practice (GPP) Guidelines, April 2007.
Participants were given a full explanation, in lay terms, of the nature and purpose of this data collection at the enrollment visit. All assessments and procedures were conducted in accordance with routine medical practice, and therefore participation in the study did not convey any additional risk or burden for patients. However, participants were provided with information on the benefits and risks of their medical treatment. Participants were required to provide written informed consent to confirm that they allowed their medical data to be collected, analyzed, and shared with regulatory authorities. Informed consent was obtained prior to participant enrollment and prior to any data collection. Sufficient time was allowed for participants to discuss any questions with investigators.
Results
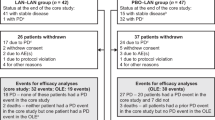
A total of 100 patients were recruited to the study; 99 patients received at least one dose of study drug and were included in the analyses. Among all patients who received study treatment, 62.6% completed their treatment over the course of the study and 16.2% went off treatment due to progression of disease. The remaining 21.1% discontinued treatment due to the following reasons: patient request (5.1%), AEs (4.0%), investigator request (4.0%), lost to follow-up (3.0%), death (2.0%), and other reasons (3.0%). The mean age of included patients was 64.5 years, with men comprising 54.5% of the study population. Over half of patients (59.6%) had already started lanreotide treatment prior to enrollment in the study. At baseline, 21.2% and 37.0% of patients presented with flushing and diarrhea, respectively. Complete patient demographics and medical history are shown in Table 1. A list of prescribed concomitant medications is presented in Supplementary Table 2.
Overall, 24 patients experienced clinically defined progression. Too few patients experienced progression over the course of the study to reach the median TTDP; therefore, median TTDP is not reported. The 12-month and 24-month PFS rates were 88.2% (95% CI 79.6–93.3) and 73.7% (95% CI 63.1–81.7), respectively (Fig. 1a). OS rates were 92.3% (95% CI 84.6−96.3) at 12 months and 84.2% (95% CI 74.0−90.7) at 24 months (Fig. 1b). A total of 13 (13.1%) patients died over the course of the study. A complete summary of causes of death is presented in Supplementary Table 3.
TTDP and OS in the total study population. A TTDP: Rates of PFS for the study population were 88.2% (95% CI 79.6%—93.3%) at 12 months and 73.7% (95% CI 63.1%—81.7%) at 24 months. TTDP was evaluated using Kaplan–Meier estimates. Vertical lines represent censored events. a‘Patients at risk’ refers to the number of patients at each timepoint who had neither experienced the event of interest (in this case, disease progression) nor been censored for any other reason (e.g., withdrew from the study, switched to a different treatment, completed their final study visit); therefore, the number ‘at risk’ at 24 months is substantially lower than the total number of patients who did not experience disease progression over the course of the study. CI confidence interval, PFS progression-free survival, TTDP time to disease progression. B OS: Rates of OS for the study population were 92.3% (95% CI 84.6%−96.3%) at 12 months and 84.2% (95% CI 74.0%−90.7%) at 24 months. OS was evaluated using Kaplan–Meier estimates. Vertical lines represent censored events. a ‘Patients at risk’ refers to the number of patients at each timepoint who had neither experienced the event of interest (in this case, death) nor been censored for any other reason (e.g., withdrew from the study, switched to a different treatment, completed their final study visit); therefore, the number ‘at risk’ at 24 months is substantially lower than the total number of patients who did not die over the course of the study. CI confidence interval, OS overall survival
The analysis by primary tumor sites demonstrated 24-month PFS rates of 77.5% (95% CI 63.7–86.6) for gastrointestinal (GI) tumors (n = 63), 60.8% (95% CI 39.3–76.8) for pancreatic tumors (n = 27) and 88.9% (95% CI 43.3–98.4) for tumors of unknown origin (n = 9; Fig. 2a). The 24-month rates of OS by subgroup were 79.0% (95% CI 64.7–88.0) for GI tumors, 91.6% (95% CI 70.4–97.8) for pancreatic tumors, and 100% for tumors of unknown origin (Fig. 2b).
TTDP and OS evaluated by primary tumor type. A TTDP: Rates of PFS for GI NETs were 89.3% (95% CI 77.7%−95.1%) at 12 months and 77.5% (95% CI 63.7%−86.6%) at 24 months; for pancreatic NETs, PFS was 81.5% (95% CI 61.1%−91.8%) at 12 months and 60.8% (95% CI 39.3%−76.8%) at 24 months; for unknown primary NETs, PFS was 100% at 12 months and 88.9% (95% CI 43.3%−98.4%) at 24 months. TTDP was evaluated using Kaplan–Meier estimates. Vertical lines represent censored events. a‘Patients at risk’ refers to the number of patients at each timepoint who had neither experienced the event of interest (in this case, disease progression) nor been censored for any other reason (e.g., withdrew from the study, switched to a different treatment, completed their final study visit); therefore, the number ‘at risk’ at 24 months is substantially lower than the total number of patients who did not experience disease progression over the course of the study. CI confidence interval, GI gastrointestinal, NET neuroendocrine tumor, PFS progression-free survival, TTDP time to disease progression. B OS: Rates of OS for GI NETs were 89.8% (95% CI 78.6%−95.3%) at 12 months and 79.0% (95% CI 64.7%−88.0%) at 24 months; for pancreatic NETs, OS was 96.0% (95% CI 74.8%−99.4%) at 12 months and 91.6% (95% CI 70.4%−97.8%) at 24 months; for unknown primary NETs, OS was 100% at 12 months and 100% at 24 months. OS was evaluated using Kaplan–Meier estimates. Vertical lines represent censored events. a‘Patients at risk’ refers to the number of patients at each timepoint who had neither experienced the event of interest (in this case, death) nor been censored for any other reason (e.g., withdrew from the study, switched to a different treatment, completed their final study visit); therefore, the number ‘at risk’ at 24 months is substantially lower than the total number of patients who did not die over the course of the study. CI confidence interval, GI gastrointestinal, NET neuroendocrine tumor, OS overall survival
A total of 83 patients answered the TSQM-9. The majority of patients (76/83; 91.6%) who answered the survey expressed at least some degree of satisfaction with the overall treatment. Of the 83 patients, 88.0% were somewhat, very, or extremely confident that the study medication was good for them (Table 2). Treatment-related AEs were experienced by 19/99 (19.2%) of patients; the majority were grades 1 and 2, with one patient experiencing grade 3 diarrhea (Table 3). Sixteen patients experienced SAEs, none of which were determined to be related to the study drug (Table 3). Treatment was discontinued in four patients due to AEs (abdominal cramps, anorexia, nausea, and paroxysmal atrial fibrillation), two of whom died; one from cardiac arrest and one from progressive disease.
Discussion
This prospective, observational study aimed to evaluate the effectiveness of lanreotide depot in patients with locally advanced, metastatic GEP-NETs. Patients treated with lanreotide depot demonstrated extended PFS and a high rate of OS, highlighting the effectiveness of lanreotide depot for the treatment of patients with GEP-NETs in a real-world setting. While previous RWE studies have evaluated the effectiveness of lanreotide depot retrospectively [24, 25], few observational studies have prospectively evaluated the safety and effectiveness of lanreotide depot as a treatment for GEP-NETs. The design of our study likely minimized bias and increased the robustness of our data, as study outcomes were predetermined, and investigators were able to collect accurate and complete datasets in accordance with a protocol.
In line with our findings, several published RWE studies have suggested that lanreotide depot treatment is effective at controlling symptoms and disease progression in patients with NETs. One retrospective study evaluating patients with metastatic midgut NETs and carcinoid syndrome reported that lanreotide depot provided a reduction in daily frequency of diarrhea and flushing symptoms in 74% of patients, and 70% of patients demonstrated no radiological tumor progression throughout the study period [25]. Another study prospectively evaluated lanreotide treatment in patients with multiple endocrine neoplasia type 1 (MEN1) syndrome with one or more pancreatic NETs. Compared to patients not receiving lanreotide depot treatment, those receiving lanreotide depot had significantly longer median PFS (p < 0.001) [26]. An Italian retrospective database study investigated the effectiveness and tolerability of the four main therapeutic sequences recommended for grade 1 and 2 NETs: SSA standard dose to SSA high dose; SSA to everolimus; SSA to chemotherapy; and SSA to peptide receptor radionuclide therapy (PRRT) [27]. The study found that while PFS did not differ significantly between the groups, the sequences with SSA high dose or PRRT were better tolerated than those with everolimus or chemotherapy. A significantly lower number and severity of side effects (p = 0.04) and rate of dose reduction/discontinuation (p = 0.03) were observed in the SSA high dose and PRRT groups, suggesting that SSAs should be one of the preferred treatment options for NETs. Our study builds on these previous findings, demonstrating the effectiveness of an SSA, lanreotide depot, as a treatment for patients with a range of primary tumor sites.
Furthermore, the high rates of PFS observed in this study (88.2% and 73.7% after 12 and 24 months, respectively) are broadly consistent with the results of previous clinical trials evaluating lanreotide depot. For example, the CLARINET phase 3 clinical trial reported a 24-month PFS rate of 65.1% for patients treated with lanreotide depot versus 33.0% for patients treated with placebo [15]. The CLARINET open-label extension (OLE) study and the CLARINET FORTE phase 2 study provided further evidence of the efficacy and safety of lanreotide treatment in this population. In CLARINET OLE, median (95% CI) PFS for patients receiving lanreotide depot was 38.5 months (95% CI 30.9–59.4), versus 19.0 months (95% CI 10.1–26.7) in placebo-treated patients [28]. The CLARINET FORTE study reported no treatment-related SAEs and no deterioration in quality of life for patients with progressive midgut or pancreatic NETs receiving an increased dosing frequency of lanreotide depot (every 14 days versus every 28 days), affirming the tolerability of lanreotide depot even when administered at shorter intervals [29]. Compared with real-world studies, data from clinical trials are considered to be more robust because their highly controlled design, including stricter eligibility criteria and data collection methods, reduces the risk of confounding factors. For example, the CLARINET trial excluded patients who had undergone surgery related to their NET within 3 months of study entry or had received chemotherapy within 6 months of entry, while these exclusion criteria were not present in our study. In addition, clinical trials typically use the response evaluation criteria in solid tumors (RECIST) as a standardized method for defining disease progression [30]. By contrast, our study introduced a more flexible definition of disease progression that identified worsening clinical symptoms, tumor growth without a specified increase in diameter, and treatment change as additional indications of progression beyond those described by RECIST. While clinical trial data are more robust, real-world studies can provide a more accurate representation of the patient population and their clinical management in the community. Notably, the rate of PFS observed in our study was comparable to the rates reported in clinical trials, indicating that lanreotide depot is effective in treating a broad range of patients in a real-world setting.
The mortality rate and safety profile of our study were comparable to those of other studies evaluating lanreotide depot as a treatment for NETs. The low mortality rate was expected due to the slow-growing nature of GEP-NETs, with patients generally having prolonged survival even after disease progression has occurred. Other studies investigating SSAs to treat NETs have shown that median survival after disease progression can range from 12 to over 60 months [31,32,33,34]. Furthermore, treatment-related AEs were experienced by 19.2% of patients, the majority of which were mild or moderate (grades 1 or 2), and no SAEs were determined to be treatment-related. The phase 3 ELECT study, which evaluated the efficacy and safety of lanreotide depot, found that 26% of patients in the lanreotide depot group experienced TEAEs [35]. In the CLARINET study, a higher proportion of patients receiving lanreotide depot (50%) experienced treatment-related AEs; however, the low rate of SAEs (3%) is consistent with our findings [15]. Additionally, a review of 40 publications evaluating the safety and tolerability of lanreotide depot determined that the most frequently reported AEs were abdominal pain, diarrhea, and cholelithiasis [36]. This is in line with our study, which found that abdominal pain/cramping and diarrhea were the most frequently experienced treatment-related AEs. Finally, in our analysis, 4.0% of patients discontinued treatment due to AEs, generally aligning with previous findings: in an analysis of SSAs to treat metastatic NETs, 8.6% discontinued treatment due to side effects [36, 37], while the ELECT study had a slightly lower rate of discontinuation due to AEs, at 1.7% [35, 36]. These results indicate that lanreotide depot is generally well tolerated in both clinical trials and a real-world setting, with patients typically experiencing mild or moderate AEs and few SAEs, as well as relatively low rates of discontinuation due to AEs.
Patient satisfaction and confidence with treatment were also assessed, in line with the FDA’s emphasis on patient autonomy and centricity [16]. Patient satisfaction questionnaires, such as the TSQM-9, allow patients receiving treatment to self-report on a range of factors, including convenience of the medication, symptom relief, and the ability of the medication to treat the condition. In our study, the majority of patients (> 80%) expressed satisfaction with their treatment, with 88.0% of patients specifically expressing satisfaction with the way the medication relieved their symptoms. As patients with GEP-NETs regularly experience a multitude of debilitating symptoms, including fatigue, diarrhea, abdominal discomfort, and trouble sleeping, alleviation of symptoms is a critical factor in patient satisfaction [38,39,40]. Confidence with the medication was also high; 88.0% of patients expressed that they felt somewhat, very, or extremely confident that taking lanreotide depot was good for them, and 84.3% felt that the good aspects of the medication outweighed the bad. The satisfaction scores obtained in our analysis align with the findings of previous studies, which generally report high rates of satisfaction in patients receiving lanreotide depot [41, 42]. Importantly, high patient satisfaction has been linked to better treatment adherence and persistence [43]. Therefore, the patient satisfaction results of our study indicate that real-world patients who receive lanreotide depot are likely to have good rates of adherence, which is a critical factor in ensuring the effectiveness of treatments in a real-world setting [44].
A relatively low proportion (26.3%) of patients in the study had received an octreotide scan at screening. Under European Society for Medical Oncology (ESMO) clinical practice guidelines, it is strongly recommended that patients with GEP-NETs undergo SSA radiolabeled imaging to assist with localization of both primary and metastatic tumors [45]. Historically, the primary imaging method has been somatostatin receptor scintigraphy (Octreoscan) [46], with 68Ga-labeled PET imaging increasingly used in recent years [47]. The low percentage of patients who had received an octreotide scan prior to entry in this study has several potential implications. Firstly, community-based treatment programs may not always have access to diagnostic techniques such as octreotide scans, or such scans may not be consistently utilized in clinical practice. In these cases, it may be difficult for tumors to be localized and treated effectively; where resources allow, imaging should be used to facilitate accurate GEP-NETs diagnosis. Secondly, it is also possible that octreotide scans were performed for more than 26.3% of patients and were simply underreported. With the increasing importance of real-world studies, it is crucial that data are reported as comprehensively and accurately as possible to ensure that studies’ findings closely reflect real-world clinical practice.
The inclusion of patients with diverse types of GEP-NETs, including GI, pancreatic, and unknown primary origin, was a key strength of this study. While the incidence of NETs is increasing overall, the percentage classified as tumors of unknown primary origin is decreasing, which may reflect advances in tumor identification techniques [1, 48]. Tumors of unknown primary origin are estimated to account for 10–22% of GEP-NETs [48, 49], which is slightly higher than the 9.1% of patients in our study. As the incidence and relative rate of GEP-NETs primary tumors changes over time, it is important to evaluate medications across a range of primary tumor sites to ensure that all patients receive effective care and disease management. In our study, lanreotide depot was shown to be effective in treating all included primary tumor types, indicating that our results are broadly applicable to the overall population of patients with GEP-NETs.
The results of this study should be interpreted in light of several limitations. While similar RWE studies have used comparable sample sizes [20, 21], the numbers of patients in each primary tumor type subgroup in the exploratory analysis were low. Patients in this study were recruited from the US Oncology Research sample, which may also have limited generalizability to other populations (e.g., patients in academic institutions, other geographic locations), and RWE does not always mirror clinical recommendations, which can make it difficult to accurately interpret all collected data. Additionally, this 2-year study only allowed for a relatively short timeframe to measure disease progression in GEP-NETs. For instance, although we were able to analyze the exploratory objective (PFS), too few patients experienced disease progression within the course of the study to calculate median duration for TTDP (the primary endpoint). Furthermore, while 75 of the 99 total patients did not experience disease progression within the 2-year study, only 15 patients were considered ‘at risk’ (i.e., had neither experienced disease progression nor been censored for any other reason) at 24 months, indicating that a large proportion of the study population was censored. In a longer study, more patients would likely experience disease progression prior to the end of the study, potentially resulting in fewer patients being censored at their final study visit. Indeed, the CLARINET OLE study found that the median PFS among patients treated with lanreotide depot was 38.5 months [28], suggesting that a longer prospective, observational study may be necessary to evaluate TTDP for patients in a community setting. Results for control of flushing and diarrhea from the current study have also not been reported, as a high proportion of patients presented without these symptoms at baseline (73.7% and 59.6%, respectively), which prevented meaningful analysis of these endpoints. Finally, the study did not include a comparator drug or placebo group against which lanreotide depot could be directly compared.
Conclusions
This study has demonstrated the effectiveness and tolerability of lanreotide depot in a real-world setting. Lanreotide depot was associated with prolonged PFS and OS in patients with GEP-NETs, in line with previous studies. Additionally, the medication was well tolerated, and the majority of patients reported satisfaction with their treatment. These results suggest that findings from stringent clinical trial populations are applicable to a more diverse group of patients in the community. Future RWE studies with an extended duration may be useful to explore the longer-term safety and effectiveness of lanreotide depot, especially in terms of TTDP and survival rate, in a real-world setting.
References
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–42.
Shah MH, Goldner WS, Benson AB, et al. Neuroendocrine and adrenal tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19(7):839–68.
Frilling A, Akerström G, Falconi M, et al. Neuroendocrine tumor disease: an evolving landscape. Endocr-Relat Cancer. 2012;19(5):R163–85.
Deroose CM, Hindié E, Kebebew E, et al. Molecular imaging of gastroenteropancreatic neuroendocrine tumors: current status and future directions. J Nucl Med. 2016;57(12):1949–56.
Öberg K. Management of functional neuroendocrine tumors of the pancreas. Gland Surg. 2018;7(1):20–7.
NCCN. NCCN Clinical Practice Guidelines in Oncology: neuroendocrine tumors. 2015.
Strosberg JR, Benson AB, Huynh L, et al. Clinical benefits of above-standard dose of octreotide LAR in patients with neuroendocrine tumors for control of carcinoid syndrome symptoms: a multicenter retrospective chart review study. Oncologist. 2014;19(9):930–6.
Wolin EM, Leyden J, Goldstein G, Kolarova T, Hollander R, Warner RRP. Patient-reported experience of diagnosis, management, and burden of neuroendocrine tumors: results from a large patient survey in the United States. Pancreas. 2017;46(5):639–47.
Kim KW, Krajewski KM, Nishino M, et al. Update on the management of gastroenteropancreatic neuroendocrine tumors with emphasis on the role of imaging. AJR Am J Roentgenol. 2013;201(4):811–24.
Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing but NET: a review of neuroendocrine tumors and carcinomas. Neoplasia. 2017;19(12):991–1002.
Raphael MJ, Chan DL, Law C, Singh S. Principles of diagnosis and management of neuroendocrine tumours. CMAJ. 2017;189(10):E398-e404.
Basuroy R, Bouvier C, Ramage JK, Sissons M, Srirajaskanthan R. Delays and routes to diagnosis of neuroendocrine tumours. BMC Cancer. 2018;18(1):1122.
Garcia-Carbonero R, Capdevila J, Crespo-Herrero G, et al. Incidence, patterns of care and prognostic factors for outcome of gastroenteropancreatic neuroendocrine tumors (GEP-NETs): results from the National Cancer Registry of Spain (RGETNE). Ann Oncol. 2010;21(9):1794–803.
Ipsen Biopharmaceuticals Inc. Highlights of US prescribing information: Somatuline Depot (lanreotide) injection, for subcutaneous use. Cambridge: Ipsen Biopharmaceuticals Inc; 2019.
Caplin ME, Pavel M, Ćwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224–33.
FDA. Framework for FDA's Real-World Evidence Program. 2018. Available at: https://www.fda.gov/media/120060/download.
Klink AJ, Feinberg B, Yu HT, et al. Patterns of care among real-world patients with metastatic neuroendocrine tumors. Oncologist. 2019;24(10):1331–9.
Huynh L, Cai B, Cheng M, et al. Analysis of real-world treatment patterns, healthcare resource utilization, and costs between octreotide and lanreotide among patients with neuroendocrine tumors. Pancreas. 2019;48(9):1126–35.
Bharmal M, Payne K, Atkinson MJ, Desrosiers M-P, Morisky DE, Gemmen E. Validation of an abbreviated Treatment Satisfaction Questionnaire for Medication (TSQM-9) among patients on antihypertensive medications. Health Qual Life Outcomes. 2009;7(1):36.
Jun E, Kim SC, Song KB, et al. Diagnostic value of chromogranin A in pancreatic neuroendocrine tumors depends on tumor size: a prospective observational study from a single institute. Surgery. 2017;162(1):120–30.
Ramage JK, Punia P, Faluyi O, et al. Observational study to assess quality of life in patients with pancreatic neuroendocrine tumors receiving treatment with everolimus: the OBLIQUE Study (UK Phase IV Trial). Neuroendocrinology. 2019;108(4):317–27.
US Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE). 2010.
SAS/ACCESS® 9.4 Interface to ADABAS: Reference. Cary: SAS Institute Inc; 2013.
Palazzo M, Lombard-Bohas C, Cadiot G, et al. Ki67 proliferation index, hepatic tumor load, and pretreatment tumor growth predict the antitumoral efficacy of lanreotide in patients with malignant digestive neuroendocrine tumors. Eur J Gastroenterol Hepatol. 2013;25(2):232–8.
Khan MS, El-Khouly F, Davies P, Toumpanakis C, Caplin ME. Long-term results of treatment of malignant carcinoid syndrome with prolonged release Lanreotide (Somatuline Autogel). Aliment Pharmacol Ther. 2011;34(2):235–42.
Faggiano A, Modica R, Lo Calzo F, et al. Lanreotide therapy vs active surveillance in MEN1-related pancreatic neuroendocrine tumors < 2 centimeters. J Clin Endocrinol Metab. 2020;105(1):78–84.
Faggiano A, Di Maio S, Mocerino C, et al. Therapeutic sequences in patients with grade 1–2 neuroendocrine tumors (NET): an observational multicenter study from the ELIOS group. Endocrine. 2019;66(2):417–24.
Caplin ME, Pavel M, Phan AT, et al. Lanreotide autogel/depot in advanced enteropancreatic neuroendocrine tumours: final results of the CLARINET open-label extension study. Endocrine. 2021;71(2):502–13.
Pavel M, Ćwikła JB, Lombard-Bohas C, et al. Efficacy and safety of high-dose lanreotide autogel in patients with progressive pancreatic or midgut neuroendocrine tumours: CLARINET FORTE phase 2 study results. Eur J Cancer. 2021;157:403–14.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Kulke MH, Siu LL, Tepper JE, et al. Future directions in the treatment of neuroendocrine tumors: consensus report of the National Cancer Institute Neuroendocrine Tumor clinical trials planning meeting. J Clin Oncol. 2011;29(7):934–43.
Rinke A, Müller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656–63.
Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514–23.
Faivre S, Niccoli P, Castellano D, et al. Sunitinib in pancreatic neuroendocrine tumors: updated progression-free survival and final overall survival from a phase III randomized study. Ann Oncol. 2017;28(2):339–43.
Vinik AI, Wolin EM, Liyanage N, Gomez-Panzani E, Fisher GA. Evaluation of lanreotide depot/autogel efficacy and safety as a carcinoid syndrome treatment (ELECT): a randomized, double-blind, placebo-controlled trial. Endocr Pract. 2016;22(9):1068–80.
Michael M, Garcia-Carbonero R, Weber MM, Lombard-Bohas C, Toumpanakis C, Hicks RJ. The antiproliferative role of lanreotide in controlling growth of neuroendocrine tumors: a systematic review. Oncologist. 2017;22(3):272–85.
Aparicio T, Ducreux M, Baudin E, et al. Antitumour activity of somatostatin analogues in progressive metastatic neuroendocrine tumours. Eur J Cancer. 2001;37(8):1014–9.
Adams JR, Ray D, Willmon R, Pulgar S, Dasari A. Living with neuroendocrine tumors: assessment of quality of life through a mobile application. JCO Clin Cancer Inform. 2019;3:1–10.
Seo C, Horodniceanu E, Shah R, et al. Patient experience with somatostatin analog treatments for neuroendocrine tumors: insight from qualitative interviews. Support Care Cancer. 2020;30:6307–16.
Halperin DM, Huynh L, Beaumont JL, et al. Impact of carcinoid syndrome symptoms and long-term use of somatostatin analogs on quality of life in patients with carcinoid syndrome: a survey study. Medicine (Baltimore). 2018;97(47): e13390.
Ryan P, McBride A, Ray D, et al. Lanreotide vs octreotide LAR for patients with advanced gastroenteropancreatic neuroendocrine tumors: an observational time and motion analysis. J Oncol Pharm Pract. 2019;25(6):1425–33.
Ruszniewski P, Valle JW, Lombard-Bohas C, et al. Patient-reported outcomes with lanreotide Autogel/Depot for carcinoid syndrome: an international observational study. Dig Liver Dis. 2016;48(5):552–8.
Barbosa CD, Balp M-M, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48.
Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14.
Pavel M, Öberg K, Falconi M, et al. Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(7):844–60.
Díez M, Teulé A, Salazar R. Gastroenteropancreatic neuroendocrine tumors: diagnosis and treatment. Ann Gastroenterol. 2013;26(1):29–36.
Ambrosini V, Campana D, Tomassetti P, Fanti S. 68Ga-labelled peptides for diagnosis of gastroenteropancreatic NET. Eur J Nucl Med Mol Imaging. 2012;39(Suppl 1):S52-60.
Berner AM, Pipinikas C, Ryan A, et al. Diagnostic approaches to neuroendocrine neoplasms of unknown primary site. Neuroendocrinology. 2020;110(7–8):563–73.
Chauhan A, Farooqui Z, Murray LA, et al. Capecitabine and temozolomide in neuroendocrine tumor of unknown primary. J Oncol. 2018;2018:3519247.
Acknowledgements
Funding
This study received funding from Ipsen Biopharmaceuticals, Inc., Cambridge, MA, USA. The funder had the following involvement with the study: development of the study design, collection, analysis, and interpretation of data, the writing of this article, and the decision to submit it for publication. Ipsen Biopharmaceuticals, Inc. also provided funding for the journal’s Rapid Service Fee.
Medical Writing, Editorial, and Other Assistance
The authors thank all patients involved in the study, as well as their caregivers, care team, investigators, and research staff in participating institutions. The authors thank Kate Hanman, BSc, MSc (Costello Medical, UK), Jenna Hebert, PhD (Costello Medical, USA), and Isabel Haber, BS (Costello Medical, USA), for medical writing support and editorial assistance based on the authors’ input and direction, which was sponsored by Ipsen Biopharmaceuticals, Inc. in accordance with Good Publication Practice guidelines.
Author Contributions
Substantial contributions to study conception/design, or acquisition/analysis/interpretation of data: Scott Paulson, David Ray, Sharan Aranha, Amy Scales, Yunfei Wang, Eric Liu; drafting of the publication, or revising it critically for important intellectual content: Scott Paulson, David Ray, Sharan Aranha, Amy Scales, Yunfei Wang, Eric Liu; final approval of the publication: Scott Paulson, David Ray, Sharan Aranha, Amy Scales, Yunfei Wang, Eric Liu; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: Scott Paulson, David Ray, Sharan Aranha, Amy Scales, Yunfei Wang, Eric Liu.
Disclosures
Scott Paulson: Stock or other ownership interests in Actinium, Aptose, and Alexion Pharmaceuticals; honoraria from Cardinal Health; consulting or advisory role in Advanced Accelerator Applications, Amgen, Bristol Myers Squibb, Eisai, Exelixis, Incyte, Ipsen, Pfizer, QED Therapeutics; research funding from Astra Zeneca, Bristol Myers Squibb, Deciphera, Exelixis, G1 Therapeutics, Hutchinson, Incyte, Ipsen, Lilly, Taiho Pharmaceutical; David Ray: Former employee, shareholder of Ipsen Biopharmaceuticals, current employee of Karyopharm Therapeutics Inc.; Sharan Aranha: Employee, McKesson, US Oncology Research; Amy Scales: Employee, McKesson, US Oncology Research; Yunfei Wang: Employee, McKesson, US Oncology Research; Eric Liu: Speaker for Curium, Ipsen, TerSera; consulting fees from AAA.
Compliance with Ethics Guidelines
This study was non interventional and therefore fell outside the scope of the European Union (EU) Directive 2001/20/EC and the EU Directive 2005/28/EC. As required by applicable local regulations, all legal regulatory aspects were covered, and approval was obtained from the appropriate regulatory bodies prior to study initiation. This study adhered to all local regulatory requirements applicable to non-interventional studies. Before initiating the study, written and dated approval/favorable opinion were obtained from the Independent Ethics Committee (IEC)/Institutional Review Board (IRB).
This study complied with the EU Directive 95/46/EC of the European Parliament, and of the Council of 24 October 1995 on the protection of individuals with regards to the processing of personal data and on the free movement of such data. This study also followed the recommendations from the International Society for Pharmacoepidemiology (ISPE), Good Pharmacoepidemiological Practice (GPP) Guidelines, April 2007.
Participants were given a full explanation, in lay terms, of the nature and purpose of this data collection at the enrollment visit. All assessments and procedures were conducted in accordance with routine medical practice, and therefore participation in the study did not convey any additional risk or burden for patients. However, participants were provided with information on the benefits and risks of their medical treatment. Participants were required to provide written informed consent to confirm that they allowed their medical data to be collected, analyzed, and shared with regulatory authorities. Informed consent was obtained prior to participant enrollment and prior to any data collection. Sufficient time was allowed for participants to discuss any questions with investigators.
Data Availability
Where patient data can be anonymized, Ipsen will share all individual participant data that underlie the results reported in this article with qualified researchers who provide a valid research question. Study documents, such as the study protocol and clinical study report, are not always available. Proposals should be submitted to DataSharing@Ipsen.com and will be assessed by a scientific review board. Data are available beginning 6 months and ending 5 years after publication; after this time, only raw data may be available.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Paulson, S., Ray, D., Aranha, S. et al. Lanreotide Depot to Treat Gastroenteropancreatic Neuroendocrine Tumors in a US Community Oncology Setting: A Prospective, Observational Study. Oncol Ther 10, 463–479 (2022). https://doi.org/10.1007/s40487-022-00208-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-022-00208-1