Abstract
Fulvestrant is a selective estrogen receptor degrader that binds, blocks and degrades the estrogen receptor (ER), leading to complete inhibition of estrogen signaling through the ER. This review article further explains the mechanism of action of the drug and goes on to review the trials carried out to optimize its dosing. Multiple trials have been undertaken to compare fulvestrant with other endocrine treatments, and results have shown it to have similar efficacy to anastrozole, tamoxifen and exemestane at 250 mg every 28 days. However, when given at 500 mg every 28 days, with an extra loading dose on day 14, it has demonstrated an improved progression-free survival (PFS) compared to anastrozole. We look at how fulvestrant has been used in combination with CDK4/6 inhibitors such as palbociclib (PALOMA-3) and ribociclib (MONALEESA-3) and drugs targeting the PI3K/AKT/mTOR pathway such as pictilisib (FERGI) and buparlisib (BELLE-2 and BELLE-3). We then go on to describe a selection of the ongoing clinical trials looking at combination therapy involving fulvestrant. Finally, we review the effect of fulvestrant in patients who have developed resistance to aromatase inhibitors via ESR1 mutation, where it has been shown to offer a PFS benefit that is further improved by the addition of the CDK4/6 inhibitor palbociclib. Whilst fulvestrant is clearly an effective drug as monotherapy, we believe that its role in the treatment of ER-positive breast cancer may be best reserved for combination therapy, and whilst there are multiple trials currently in progress, it would appear that the combination with CDK4/6 inhibitors would offer the greatest promise in terms of balancing benefit with toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer has the highest incidence of any cancer in the world, with 1.7 million new cases recorded in 2012, accounting for 12% of all new cancer diagnoses. It is also the fifth highest cause of cancer death, with 521,827 deaths worldwide in 2012 (Cancer Research UK).
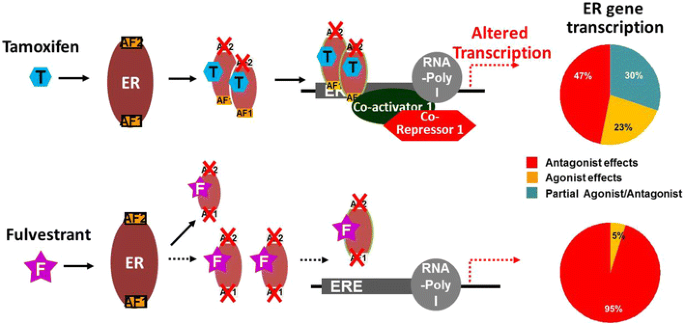
Approximately 80% of breast cancers express the estrogen receptor (ER), with their survival and proliferation driven by estrogen acting as the ligand and binding to the estrogen receptor, which is then translocated to the cancer cell nucleus. This in turn initiates a signaling cascade, resulting in the propagation of breast cancer cells. The ER is a nuclear receptor. Transcriptional activity is regulated by two activating functional domains: AF1 and AF2. The former, located in the N-terminal domain, acts independently of estrogen, becoming activated through phosphorylation. The latter, however, located in the ligand-binding domain, requires the presence of estrogen for activation [1].
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Mechanism of Action
Tamoxifen and fulvestrant are both anti-estrogens that counteract the effects of estrogen by binding directly to the ER, thereby working as an antagonist. Tamoxifen is a selective estrogen receptor modulator (SERM) that blocks E2-mediated activity of AF2, resulting in ER-antagonistic activity, although partial agonistic activity remains. Unlike tamoxifen, fulvestrant-induced conformational change of the ER disrupts both AF2- and AF1-related transcriptional activity [1].
Furthermore, the complex formed when fulvestrant binds to the ER is unstable, resulting in its accelerated degradation. Fulvestrant therefore acts as both a competitive antagonist and a selective estrogen receptor degrader (SERD), causing a reduction in cellular ER alpha levels [2]. In addition, it acts almost exclusively as an ER antagonist, whereas tamoxifen is also a partial agonist of ER [3] (Fig. 1).
Fulvestrant has a relatively high binding affinity to the ER, which is 89% that of estradiol [4]. It also impairs dimerization of the receptor, thereby blocking its nuclear localization [5], and the unstable complex formed results in accelerated degradation of the ER protein [6]. Thus, fulvestrant binds, blocks and degrades the ER, leading to complete inhibition of estrogen signaling through the ER [7].
Early Trials
One of the limiting factors in the dosing of fulvestrant is the practicality of administration. Fulvestrant has poor solubility and must be administered via intramuscular injection, thereby limiting the volume and dose that can be delivered. The initial dose, as used in the trials explained here, was defined as 250 mg every 28 days, and this dose was tested in a range of randomized phase III trials comparing fulvestrant with other, standard-of-care endocrine therapies in the first-line or subsequent settings.
Two parallel studies in patients progressing after prior endocrine treatment showed that fulvestrant at a dose of 250 mg every 4 weeks was as effective as anastrozole in postmenopausal women with advanced breast cancer progressing after prior endocrine treatment [8, 9]. In both trials, the median time to progression (TTP) for fulvestrant and anastrozole was comparable: 5.5 months versus 5.1 months (HR 0.98; 95% CI 0.8–1.21; p = 0.84) and 5.4 versus 3.4 months (HR 0.92; 95% CI 0.74–1.14; p = 0.43), respectively [8, 9]. A prospectively planned, combined analysis of the two studies also showed comparable outcome (HR 0.96; 95% CI 0.83–1.11; p = 0.61). In each of the studies, both drugs were well tolerated [10]. There was also no significant difference in the secondary endpoint of objective response rate (ORR), with 19.2% responding in the fulvestrant arm and 16.5% in the anastrozole arm (p = 0.31).
Another trial went on to compare fulvestrant with tamoxifen in patients who had not received prior endocrine therapy for metastatic disease and had not received adjuvant endocrine therapy within 12 months. Again, this trial showed no significant difference in the primary endpoint between the two investigatory arms, with a median TTP of 6.8 months for fulvestrant and 8.3 months for tamoxifen (HR 1.18; 95% CI 0.98–1.44; p = 0.088) [11]. The secondary endpoint, ORR, was also comparable between arms (OR 0.87; 95% CI 0.61–1.24; p = 0.45). However, exploratory survival analysis suggested a benefit for tamoxifen over fulvestrant (HR 1.29; 95% CI 1.01–1.64; p = 0.04) [11].
Finally, two randomized trials compared fulvestrant at the dose of 250 mg every 4 weeks to the steroidal aromatase inhibitor exemestane as single-agent therapy or in combination with the non-steroidal aromatase inhibitor anastrozole. In the EFECT study, there was no difference in TTP between fulvestrant and exemestane, with a median TTP of 3.7 months observed in both arms (HR 0.96; 95% CI 0.82–1.13; p = 0.65) [12]. Interestingly, this study used a loading dose regimen for fulvestrant, with 500 mg given on day 0, and then 250 mg given on days 14 and 28, before repeating every 28 days. The different regimens for fulvestrant administration will be discussed later in this review.
The SoFEA phase III study investigated fulvestrant plus anastrozole or placebo versus exemestane alone after progression on non-steroidal aromatase inhibitors in postmenopausal advanced cancer patients [13]. Again, the loading regimen previously described was used for the administration of fulvestrant. Once more, there was no significant difference among the three arms, with median progression-free survival (PFS) of 4.4, 4.8 and 3.4 months, respectively, for the three arms, demonstrating that double endocrine treatment is no more effective than fulvestrant alone or exemestane.
What is the Optimal Dose of Fulvestrant?
Originally, fulvestrant was prescribed as 250 mg every 28 days, and other than the EFECT study, the previously described randomized trials comparing fulvestrant to both steroidal and non-steroidal aromatase inhibitors and tamoxifen were carried out using this dosing scheme. However, there has been much debate about the best dose and optimal dosing schedule for fulvestrant, and several trials have sought to address this issue. These include neoadjuvant window-of-opportunity trials looking at the effect of fulvestrant therapy on biomarkers, as well as phase II and III clinical trials in the advanced breast cancer setting.
In a biomarker-driven preoperative window trial (NEWEST), researchers investigated the dose effect of fulvestrant on a range of biomarkers. The study included postmenopausal women with newly diagnosed ER-positive breast cancer. Women were given either 500 mg per month plus 500 mg on day 14 of month 1 or 250 mg per month as preoperative therapy. The primary endpoint for this study was the change in the Ki-67 labeling index from baseline to week 4. The study showed that the higher dose and intensified loading schedule was associated with significantly increased down-regulation of Ki-67 (−78.4% vs. −47.4%; p < 0.0001) [14].
In addition, the higher dose of fulvestrant was also associated with increased down-regulation of ER, with ER expression reduced by 25% with the 500-mg dose compared to a 13.5% reduction with the 250-mg dose. Changes in Ki-67 and ER expression were both measured at day 28. This demonstrates that fulvestrant is able to work more potently as an ER degrader with this dose scheduling. Importantly, these data show that not only does the increased dose have a greater effect on down-regulating cancer cell proliferation, but it also has a direct effect on the ER itself.
The synchronous FINDER 1 and FINDER 2 studies were designed to investigate the importance of different dosing schedules in relation to the efficacy and tolerability of fulvestrant in Japanese and Western populations, respectively [15, 16]. The approved dose (AD) of 250 mg/month, a loading dose (LD) of 500 mg on day 0, followed by 250-mg doses on days 14 and 28 and monthly thereafter, and a high dose (HD) of 500 mg on days 0, 14 and 28 and then monthly thereafter, were explored. Neither study found a statistically significant difference among the three doses, using overall response rate (ORR) as their primary outcomes, but these phase II studies were ultimately underpowered to demonstrate moderate differences.
FINDER 1 found no significant difference among the three groups, with ORR of 11.1%, 17.6% and 10.6%, respectively [15]. FINDER 2 found a trend towards greater efficacy with the higher dose, but again, no significant difference was found among the three groups, with ORR of 8.5%, 5.9% and 15.2%, respectively [16]. Both trials were small, with 143 and 144 patients, respectively, and were essentially underpowered to demonstrate clinically small or moderate differences. In addition, both trials used ORR as the primary endpoint, which is considered suboptimal for comparing endocrine therapies. Tolerability, however, was similar throughout all arms within both studies.
The relevance of dose and schedule was further assessed in the CONFIRM trial, which included 736 postmenopausal patients (more than the two FINDER trials combined) who had already experienced progression on prior endocrine treatment. This phase III trial compared fulvestrant 250 mg/month with fulvestrant 500 mg/month with accelerated loading. The primary endpoint was PFS, with OS a secondary endpoint. Fulvestrant 500 mg was associated with a statistically significant increase in PFS compared to fulvestrant 250 mg (HR 0.80; 95% CI 0.68–0.94; p = 0.006), though interestingly, objective response rates were similar between the two arms (9.1% vs. 10.2%, respectively) [17]. Moreover, OS was also significantly better in the fulvestrant 500-mg arm, with a median OS of 26.4 months compared to 22.3 months in the 250-mg arm (HR 0.81; 95% CI 0.69–0.96; p = 0.02) [18]. Both dosing regimens were well tolerated.
Taken together, these data show that the higher dose of fulvestrant provides a statistically significant improvement in both PFS and OS, without an increase in toxicity, and so the higher dose has been adopted as the standard. Fulvestrant 500 mg/month with a loading dose is now the recommended dose.
Comparison Trials with Fulvestrant 500 mg
Having established an improved standard dose for fulvestrant, it has since been compared once more to aromatase inhibitors to see whether this improvement in PFS and OS compared to the lower dose could be translated into an improvement over to the established aromatase inhibitors, as opposed to the equivalence that was shown previously when the suboptimal fulvestrant dose of 250 mg was used.
The FIRST study was a phase II study of 205 patients, investigating the activity of fulvestrant 500 mg versus anastrozole 1 mg in patients without previous exposure to endocrine therapy in the advanced breast cancer setting. The primary endpoint was clinical benefit rate (CBR), defined as the proportion of patients experiencing an objective response or stable disease for 24 weeks or longer. CBR was similar for fulvestrant and anastrozole (72.5% vs. 67%, respectively), as was ORR (36% vs. 35.5%). However, TTP was significantly greater for fulvestrant at both the initial analysis [19] and the pre-planned follow-up analysis, with TTP at the latter time point of 23.4 months for fulvestrant and 13.1 months for anastrozole (HR 0.66; 95% CI 0.47–0.92; p = 0.01) [20]. Moreover, when (albeit unplanned) overall survival analysis was performed, it showed an OS of 54.1 months for fulvestrant and 48.4 months for anastrozole, an increase of 5.7 months (HR 0.70; 95% CI 0.5–0.98; p = 0.04) [21]. Once again, there was similar tolerance between the two drugs.
These findings were the basis for the FALCON phase III trial that included 462 postmenopausal women who had not previously received any form of endocrine therapy (adjuvant or metastatic). This trial was designed to confirm the efficacy of fulvestrant 500 mg compared to an aromatase inhibitor, anastrozole. A statistically significant improvement in the primary endpoint, PFS, was observed with fulvestrant relative to anastrozole (16.6 months in the fulvestrant arm vs. 13.8 months with anastrozole [HR = 0.797; 95% CI 0.637–0.999; p = 0.0486]), with similar adverse event rates [22].
Subgroup analysis suggested that patients without visceral disease might benefit most from receiving fulvestrant. PFS in this subgroup increased from 13.8 months in patients treated with anastrozole to 22.3 months for fulvestrant-treated patients (HR 0.59; 95% CI 0.42–0.84). This compares to similar efficacy in patients with visceral disease, with a PFS of 15.9 months for anastrozole and 13.8 months for fulvestrant (HR = 0.99). At the time of writing, the OS data are immature but have so far revealed no difference between the drugs [22]. At data cutoff, 67 (29%) of 230 patients in the fulvestrant group and 75 (32%) of 232 patients in the anastrozole group had died (HR 0.88, 95% CI 0.63–1.22, p = 0.4277).
Fulvestrant-Based Combination Therapy
Fulvestrant has been evaluated in various combinations, either with other endocrine agents or with novel targeted agents. Three studies have explored endocrine/endocrine combinations [23, 13, 24], with conflicting results. The SoFEA and FACT trials showed no benefit [23, 13], whereas the SWOG S0226 trial showed a slightly improved PFS of 15 months with the combination compared to 13.5 months with anastrozole alone (HR 0.8; 95% CI 0.68–0.94; p = 0.007) [24]. However, all of these studies used a suboptimal dosing regimen for fulvestrant, with 500 mg on day 1 but only 250 mg on day 15, and monthly from day 29 onwards. Moreover, the SWOG S0226 trial lacked a fulvestrant monotherapy arm.
Fulvestrant has since been combined with several different classes of targeted agents, namely CDK4/6 inhibitors, drugs targeting the PI3K/AKT/mTOR pathway and histone deacetylase (HDAC) inhibitors.
Cyclin-dependent kinases (CDKs) promote cell-cycle progression, with CDK4/6 playing a pivotal role in ER-positive breast cancer, regulating the G1-to-S-phase of the cell cycle. [25]. Several CDK4/6 inhibitors are now approved or currently in clinical development, including palbociclib, ribociclib and abemaciclib. Both palbociclib and ribociclib have been shown to substantially increase PFS in combination with the aromatase inhibitor letrozole in patients without prior endocrine treatment for metastatic breast cancer (PALOMA-2 study [26]; MONALEESA-2 study [27].
The PALOMA-3 study investigated fulvestrant with palbociclib or placebo in both pre- and postmenopausal patients who had progressed on previous endocrine treatment. The trial demonstrated a substantial increase in PFS, from 4.6 months in the placebo arm to 9.5 months in the palbociclib arm (HR = 0.46; 95% CI 0.36–0.59; p < 0.0001). In addition, ORR increased from 10.9% in patients receiving fulvestrant alone to 24.6% in those receiving the combination. Although the incidence of grade 3–4 adverse events increased from 22% to 73%, most of these events were uncomplicated myelosuppression (in particular neutropenia) and did not significantly affect patients’ quality of life. The risk of infection was low compared to chemotherapy across all studies with CDK4/6 inhibitors, affecting approximately 1% of patients. Interestingly, the added benefit of CDK4/6 inhibitors was seen irrespective of the degree of endocrine resistance, hormone receptor expression level or PIK3CA mutational status [28].
Other trials investigating the value of the CDK4/6 inhibitors are ongoing. The FLIPPER trial is a phase II study comparing fulvestrant and palbociclib with fulvestrant and placebo in the first-line metastatic setting. PARSIFAL is a phase II trial investigating the best endocrine therapy in combination with palbociclib, randomizing first-line patients to fulvestrant or letrozole. The MONALEESA-3 is a randomized placebo-controlled phase III study investigating the addition of ribociclib to fulvestrant. Finally, MONARCH 2 is also a randomized, placebo-controlled phase III study, but is investigating abemaciclib in combination with fulvestrant.
A second main target for combination endocrine therapy is the PI3K/AKT/mTOR pathway. Activation of the PI3K pathway has been shown to play a major role in promoting resistance to endocrine therapy [29]. This can be driven by either mutations in or up-regulation of the PIK3CA gene. Combination therapy with the mTOR inhibitor everolimus plus exemestane in the BOLERO-2 study demonstrated a significant benefit in PFS, but also showed substantially increased toxicity with the combination therapy. Trials with PI3K inhibitors were begun in the hope of improving on these results. Many of these studies used fulvestrant as the endocrine backbone. The efficacy of two different pan-PI3K inhibitors, pictilisib and buparlisib, has been assessed in combination with fulvestrant in three placebo-controlled randomized clinical trials: the phase II FERGI trial investigating pictilisib [30] and the phase III BELLE-2 and BELLE-3 trials investigating buparlisib (SABCS 2016).
The FERGI trial investigated the activity of the pan-PI3K inhibitor pictilisib in combination with fulvestrant in two parts. The first part included all patients with endocrine-resistant advanced breast cancer. The second part included only patients harbouring PI3K mutations. No significant PFS was seen in either stage of the study, with PFS of 6.6 months for pictilisib and 5.1 months for placebo in part 1 (HR = 0.74; 95% CI 0.52–1.06; p = 0.096) and PFS of 5.4 and 10 months, respectively, in part two (HR = 1.07; 95% CI 0.53–2.18; p = 0.84) [30]. There was also greater toxicity seen with pictilisib, potentially preventing it from being dosed sufficiently to provide efficacy. The investigators felt that a more specific inhibitor might allow more efficacious dosing.
BELLE-2 assessed the more pan-PI3K inhibitor buparlisib. The trial included women with hormone-resistant advanced breast cancer, stratified by the presence of PIK3CA mutations, as detected either in tumor tissue or from circulating tumor DNA (ctDNA). In the full study population, a small but significant increase in PFS from 5 to 6.9 months was seen with the addition of buparlisib to fulvestrant (HR = 0.78; p < 0.001). Interestingly, in the patients with a PIK3CA mutation, the relative benefit was larger, with an increase in median PFS from 3.2 to 7 months (HR = 0.56; p < 0.001). This was, however, associated with an increase in serious adverse effects seen with PI3K inhibition, including hyperglycaemia, hepatotoxicity and depression.
Also interestingly, no difference was seen in PFS between the full population and the PIK3CA-mutant patients in the arms receiving buparlisib, with the improved effect seemingly due to the fact that the PIK3CA-mutant patients progressed more rapidly than the full population when using fulvestrant monotherapy. This could imply that the presence of a PIK3CA mutation is an independent poor prognostic marker for single-agent endocrine therapy.
The BELLE-3 study is another phase III placebo-controlled study of the combination of buparlisib and fulvestrant for patients who had progressed on or within 30 days of endocrine and mTOR inhibitor therapy given as the last therapy before study entry, and no more than one prior chemotherapy regimen for advanced disease The rationale was that mTOR1 inhibition elicits AKT phosphorylation via feedback activation. PI3K inhibitors then abrogate AKT phosphorylation elicited by mTORC1 inhibition [31, 32]. The primary endpoint of PFS was met with a PFS of 3.9 months in the buparlisib arm compared to 1.8 months in the placebo arm (HR 0.67; 95% CI 0.53–0.84; p < 0.001). Response rates were also greater with ORR in the buparlisib arm 7.6% compared to 2.1% in the placebo arm. There was, however, an increase in toxicity in the combination arm with grade 3/4 adverse events almost twice as frequent (62% vs. 34%). These were notably in the form of raised transaminases and mood disorders. This may represent a significant challenge to safely delivering this combination (Di Leo et al. [33]).
One of the main limitations of Pi3K inhibitors is tolerability, especially of pan-PI3K inhibitors; thus newer, more specific agents are being developed. Trials are under way to further explore the combination of fulvestrant with drugs targeting the PI3K/AKT/mTOR pathway. MANTA is a phase II study exploring its use in combination with two different mTOR inhibitors: everolimus, which is already licensed in combination with exemestane; and vistusertib, a novel mTOR inhibitor. Taselisib is selective for the PI3Kα isoform, and so the hope is that it will be less toxic than the previously described PI3K inhibitors, allowing more potent dosing. SANDPIPER is an ongoing study investigating the use of fulvestrant alongside taselisib in a placebo-controlled phase III trial. Similarly, the SOLAR-1 study is a phase III double-blind placebo-controlled study of another selective PI3K inhibitor, alpelisib, in combination with fulvestrant in two different cohorts, the first having PIK3CA mutations and the second a PIK3CA wild-type cohort.
ESR1 Mutations and Fulvestrant
There is increasing evidence implicating ESR1 mutations as an important driver of acquired resistance to endocrine treatment [34]. ESR1 mutations are rare in primary breast cancer but are more prevalent in metastatic cancers, especially in patients previously treated with aromatase inhibitors, implying that these mutations are acquired [35, 36, 37]. These mutations result in the ER becoming constitutively active, and have therefore been associated with resistance to aromatase inhibitors and tamoxifen [35, 36].
Fulvestrant is a selective estrogen receptor degrader. Thus it is potentially able to degrade the ER and consequently to stop the up-regulation of downstream proliferation even once it becomes constitutively active. This is supported by data from further analysis of tissue from the SoFEA trial showing that patients with ESR1 mutations had an improved PFS of 5.7 months with fulvestrant compared to 2.6 months with exemestane (HR = 0.52; 95% CI 0.30–0.92; p = 0.02) [38].
Spoerke et al. investigated hotspot mutations in ESR1 and PIK3CA in ctDNA from participants of the aforementioned FERGI trial. ESR1 mutations were observed in over a third of patients and were enriched in those with luminal A (41.4%) and PIK3CA-mutated (44.4%) tumors. It seems intuitive that luminal A cancers should have a greater frequency of ESR1 mutations, as they are likely to have been exposed to several lines of aromatase inhibitors over a longer time course than other breast cancer subtypes [39]. Despite the fact that the FERGI trial was a negative study, a post hoc analysis of patients with ESR1 mutations suggested an improvement in PFS from 3.7 months with placebo to 7.2 months with PI3K inhibition, suggesting that the PI3K/AKT/mTOR pathway is associated with resistance through ESR1 mutation [39].
Spoerke’s further tissue and ctDNA analysis of the FERGI trial provides no evidence that PFS with fulvestrant treatment is any different for patients with ESR1 mutations than for those with wild-type ESR1. This suggests that these mutations might not be associated with innate or acquired resistance to fulvestrant.
Fribbens et al. analysed samples taken from patients in the SoFEA and PALOMA-3 studies and analysed the impact of ESR1 mutations. In SoFEA, patients with ESR1 mutations had improved PFS with fulvestrant compared to exemestane (HR = 0.52), whereas those with wild-type ESR1 had similar PFS (HR = 1.07) [38]. In PALOMA-3, fulvestrant plus palbociclib improved PFS compared to fulvestrant plus placebo in both ESR1-mutant (HR = 0.43) and wild-type (HR = 0.49) patients [38].
Conclusions
Fulvestrant is an important endocrine therapy that has demonstrated substantial clinical benefit in many phase 3 trials, either alone or in combination with other agents. The trials involving fulvestrant are listed in Table 1. The majority of trials to date have explored its use in the metastatic setting, whereas there are limited data available for early breast cancer, partly because the requirement of intramuscular injection was considered less favorable in the adjuvant setting. Indeed, fulvestrant is not licensed for use in this setting. However, the development of oral SERDs might be able overcome this limitation, provided they can demonstrate improved efficacy over current treatment options. It will also be interesting to see whether oral availability will allow higher doses to be achieved, thereby potentially further increasing activity.
The FALCON study suggests that fulvestrant is the most active single-agent endocrine therapy for postmenopausal women in the metastatic setting. It is clear that in terms of dosing and schedule, the higher dose of 500 mg on days 0, 14 and 28, and then every 28 days appears to be the most efficacious way to give the drug, balancing effectiveness and tolerability, as shown in the CONFIRM study. The remaining question is whether it is best used in monotherapy or in combination with other drugs. Combinations of fulvestrant and other endocrine treatments have not shown a clear advantage over single-agent therapy. However, fulvestrant might offer some advantages compared to other endocrine treatments as an endocrine backbone of combination therapy, most notably the ability to overcome ESR1 mutations that might be seen in patients who have relapsed on or after adjuvant aromatase inhibitors.
At present, most of the available evidence for the combination of fulvestrant and targeted biological therapies is for the CDK4/6 inhibitor palbociclib and PI3K inhibitors. The CDK4/6 inhibitors may offer the most promise, as the currently available PI3K inhibitors are associated with side effect profiles that limit their dosing to an extent that compromises their effectiveness. However, this is clearly an area of significant ongoing research, and additional combinations will hopefully be revealed over the coming years.
References
Moverare-Skrtic S, Borjesson AE, Farman HH, Sjogren K, Windahl SH, Lagerquist MK, Andersson A, Stubelius A, Carlsten H, Gustafsson JA, Ohlsson C. The estrogen receptor antagonist ICI 182,780 can act both as an agonist and an inverse agonist when estrogen receptor alpha AF-2 is modified. Proc Natl Acad Sci USA. 2014;111:1180–5.
Fan M, Rickert EL, Chen L, Aftab SA, Nephew KP, Weatherman RV. Characterization of molecular and structural determinants of selective estrogen receptor downregulators. Breast Cancer Res Treat. 2007;103:37–44.
Howell SJ, Johnston SR, Howell A. The use of selective estrogen receptor modulators and selective estrogen receptor down-regulators in breast cancer. Best Pract Res Clin Endocrinol Metab. 2004;18:47–66.
Wakeling AE, Bowler J. Steroidal pure antioestrogens. J Endocrinol. 1987;112:R7–10.
Fawell SE, White R, Hoare S, Sydenham M, Page M, Parker MG. Inhibition of estrogen receptor-DNA binding by the “pure” antiestrogen ICI 164,384 appears to be mediated by impaired receptor dimerization. Proc Natl Acad Sci USA. 1990;87:6883–7.
Nicholson RI, Gee JM, Manning DL, Wakeling AE, Montano MM, Katzenellenbogen BS. Responses to pure antiestrogens (ICI 164384, ICI 182780) in estrogen-sensitive and -resistant experimental and clinical breast cancer. Ann N Y Acad Sci. 1995;761:148–63.
Osborne CK, Wakeling A, Nicholson RI. Fulvestrant: an oestrogen receptor antagonist with a novel mechanism of action. Br J Cancer. 2004;90(Suppl 1):S2–6.
Howell A, Robertson JF, Quaresma Albano J, Aschermannova A, Mauriac L, Kleeberg UR, Vergote I, Erikstein B, Webster A, Morris C. Fulvestrant, formerly ICI 182,780, is as effective as anastrozole in postmenopausal women with advanced breast cancer progressing after prior endocrine treatment. J Clin Oncol. 2002;20:3396–403.
Osborne CK, Pippen J, Jones SE, Parker LM, Ellis M, Come S, Gertler SZ, May JT, Burton G, Dimery I, et al. Double-blind, randomized trial comparing the efficacy and tolerability of fulvestrant versus anastrozole in postmenopausal women with advanced breast cancer progressing on prior endocrine therapy: results of a North American trial. J Clin Oncol. 2002;20:3386–95.
Robertson JF, Osborne CK, Howell A, Jones SE, Mauriac L, Ellis M, Kleeberg UR, Come SE, Vergote I, Gertler S, et al. Fulvestrant versus anastrozole for the treatment of advanced breast carcinoma in postmenopausal women: a prospective combined analysis of two multicenter trials. Cancer. 2003;98:229–38.
Howell A, Robertson JF, Abram P, Lichinitser MR, Elledge R, Bajetta E, Watanabe T, Morris C, Webster A, Dimery I, Osborne CK. Comparison of fulvestrant versus tamoxifen for the treatment of advanced breast cancer in postmenopausal women previously untreated with endocrine therapy: a multinational, double-blind, randomized trial. J Clin Oncol. 2004;22:1605–13.
Chia S, Gradishar W, Mauriac L, Bines J, Amant F, Federico M, Fein L, Romieu G, Buzdar A, Robertson JF, et al. Double-blind, randomized placebo controlled trial of fulvestrant compared with exemestane after prior nonsteroidal aromatase inhibitor therapy in postmenopausal women with hormone receptor-positive, advanced breast cancer: results from EFECT. J Clin Oncol. 2008;26:1664–70.
Johnston SR, Kilburn LS, Ellis P, Dodwell D, Cameron D, Hayward L, Im YH, Braybrooke JP, Brunt AM, Cheung KL, et al. Fulvestrant plus anastrozole or placebo versus exemestane alone after progression on non-steroidal aromatase inhibitors in postmenopausal patients with hormone-receptor-positive locally advanced or metastatic breast cancer (SoFEA): a composite, multicentre, phase 3 randomised trial. Lancet Oncol. 2013;14:989–98.
Kuter I, Gee JM, Hegg R, Singer CF, Badwe RA, Lowe ES, Emeribe UA, Anderson E, Sapunar F, Finlay P, et al. Dose-dependent change in biomarkers during neoadjuvant endocrine therapy with fulvestrant: results from NEWEST, a randomized Phase II study. Breast Cancer Res Treat. 2012;133:237–46.
Ohno S, Rai Y, Iwata H, Yamamoto N, Yoshida M, Iwase H, Masuda N, Nakamura S, Taniguchi H, Kamigaki S, Noguchi S. Three dose regimens of fulvestrant in postmenopausal Japanese women with advanced breast cancer: results from a double-blind, phase II comparative study (FINDER1). Ann Oncol Off J Euro Soc Med Oncol/ESMO. 2010;21:2342–7.
Pritchard KI, Rolski J, Papai Z, Mauriac L, Cardoso F, Chang J, Panasci L, Ianuli C, Kahan Z, Fukase K, et al. Results of a phase II study comparing three dosing regimens of fulvestrant in postmenopausal women with advanced breast cancer (FINDER2). Breast Cancer Res Treat. 2010;123:453–61.
Di Leo A, Jerusalem G, Petruzelka L, Torres R, Bondarenko IN, Khasanov R, Verhoeven D, Pedrini JL, Smirnova I, Lichinitser MR, et al. Results of the CONFIRM phase III trial comparing fulvestrant 250 mg with fulvestrant 500 mg in postmenopausal women with estrogen receptor-positive advanced breast cancer. J Clin Oncol. 2010;28:4594–600.
Di Leo A, Jerusalem G, Petruzelka L, Torres R, Bondarenko IN, Khasanov R, Verhoeven D, Pedrini JL, Smirnova I, Lichinitser MR, et al. Final overall survival: fulvestrant 500 mg vs 250 mg in the randomized CONFIRM trial. J Natl Cancer Inst. 2014;106:djt337.
Robertson JF, Llombart-Cussac A, Rolski J, Feltl D, Dewar J, Macpherson E, Lindemann J, Ellis MJ. Activity of fulvestrant 500 mg versus anastrozole 1 mg as first-line treatment for advanced breast cancer: results from the FIRST study. J Clin Oncol. 2009;27:4530–5.
Robertson JF, Lindemann JP, Llombart-Cussac A, Rolski J, Feltl D, Dewar J, Emerson L, Dean A, Ellis MJ. Fulvestrant 500 mg versus anastrozole 1 mg for the first-line treatment of advanced breast cancer: follow-up analysis from the randomized ‘FIRST’ study. Breast Cancer Res Treat. 2012;136:503–11.
Ellis MJ, Llombart-Cussac A, Feltl D, Dewar JA, Jasiowka M, Hewson N, Rukazenkov Y, Robertson JF. Fulvestrant 500 mg versus anastrozole 1 mg for the first-line treatment of advanced breast cancer: overall survival analysis from the Phase II FIRST study. J Clin Oncol. 2015;33:3781–7.
Robertson JF, Bondarenko IM, Trishkina E, Dvorkin M, Panasci L, Manikhas A, Shparyk Y, Cardona-Huerta S, Cheung KL, Philco-Salas MJ, et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): an international, randomised, double-blind, phase 3 trial. Lancet. 2016;388:2997–3005.
Bergh J, Jonsson PE, Lidbrink EK, Trudeau M, Eiermann W, Brattstrom D, Lindemann JP, Wiklund F, Henriksson R. FACT: an open-label randomized phase III study of fulvestrant and anastrozole in combination compared with anastrozole alone as first-line therapy for patients with receptor-positive postmenopausal breast cancer. J Clin Oncol. 2012;30:1919–25.
Mehta RS, Barlow WE, Albain KS, Vandenberg TA, Dakhil SR, Tirumali NR, Lew DL, Hayes DF, Gralow JR, Livingston RB, Hortobagyi GN. Combination anastrozole and fulvestrant in metastatic breast cancer. N Engl J Med. 2012;367:435–44.
O’Leary B, Finn RS, Turner NC. Treating cancer with selective CDK4/6 inhibitors. Nat Rev Clin Oncol. 2016;13:417–30.
Finn RS, Crown JP, Ettl J, Schmidt M, Bondarenko IM, Lang I, Pinter T, Boer K, Patel R, Randolph S, et al. Efficacy and safety of palbociclib in combination with letrozole as first-line treatment of ER-positive, HER2-negative, advanced breast cancer: expanded analyses of subgroups from the randomized pivotal trial PALOMA-1/TRIO-18. Breast Cancer Res Bcr. 2016;18:67.
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, Campone M, Blackwell KL, Andre F, Winer EP, et al. Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med. 2016;375:1738–48.
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, Colleoni M, DeMichele A, Loi S, Verma S, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17:425–39.
Van Tine BA, Crowder RJ, Ellis MJ. ER and PI3K independently modulate endocrine resistance in ER-positive breast cancer. Cancer Discov. 2011;1:287–8.
Krop IE, Mayer IA, Ganju V, Dickler M, Johnston S, Morales S, Yardley DA, Melichar B, Forero-Torres A, Lee SC, et al. Pictilisib for oestrogen receptor-positive, aromatase inhibitor-resistant, advanced or metastatic breast cancer (FERGI): a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2016;17:811–21.
O’Reilly KE, Rojo F, She QB, Solit D, Mills GB, Smith D, Lane H, Hofmann F, Hicklin DJ, Ludwig DL, et al. mTOR inhibition induces upstream receptor tyrosine kinase signaling and activates Akt. Can Res. 2006;66:1500–8.
Sun SY, Rosenberg LM, Wang X, Zhou Z, Yue P, Fu H, Khuri FR. Activation of Akt and eIF4E survival pathways by rapamycin-mediated mammalian target of rapamycin inhibition. Can Res. 2005;65:7052–8.
Di Leo A, Seok Lee K, Ciruelos E. BELLE-3: a phase III study of buparlisib + fulvestrant in postmenopausal women with HR+, HER2–, aromatase inhibitor-treated, locally advanced or metastatic breast cancer, who progressed on or after mTOR inhibitor-based treatment. San Antonio Breast Cancer Symposium. 2016;Abstract S4-07.
Jeselsohn R, Buchwalter G, De Angelis C, Brown M, Schiff R. ESR1 mutations-a mechanism for acquired endocrine resistance in breast cancer. Nat Rev Clin Oncol. 2015;12:573–83.
Jeselsohn R, Yelensky R, Buchwalter G, Frampton G, Meric-Bernstam F, Gonzalez-Angulo AM, Ferrer-Lozano J, Perez-Fidalgo JA, Cristofanilli M, Gomez H, et al. Emergence of constitutively active estrogen receptor-alpha mutations in pretreated advanced estrogen receptor-positive breast cancer. Clin Cancer Res Off J Am Assoc Cancer Res. 2014;20:1757–67.
Robinson DR, Wu YM, Vats P, Su F, Lonigro RJ, Cao X, Kalyana-Sundaram S, Wang R, Ning Y, Hodges L, et al. Activating ESR1 mutations in hormone-resistant metastatic breast cancer. Nat Genet. 2013;45:1446–51.
Schiavon G, Hrebien S, Garcia-Murillas I, Cutts RJ, Pearson A, Tarazona N, Fenwick K, Kozarewa I, Lopez-Knowles E, Ribas R, et al. Analysis of ESR1 mutation in circulating tumor DNA demonstrates evolution during therapy for metastatic breast cancer. Sc Translat Med. 2015;7:313ra182.
Fribbens C, O’Leary B, Kilburn L, Hrebien S, Garcia-Murillas I, Beaney M, Cristofanilli M, Andre F, Loi S, Loibl S, et al. Plasma ESR1 mutations and the treatment of estrogen receptor-positive advanced breast cancer. J Clin Oncol. 2016;34:2961–8.
Spoerke JM, Gendreau S, Walter K, Qiu J, Wilson TR, Savage H, Aimi J, Derynck MK, Chen M, Chan IT, et al. Heterogeneity and clinical significance of ESR1 mutations in ER-positive metastatic breast cancer patients receiving fulvestrant. Nat Commun. 2016;7:11579.
Fasching PA, Jerusalem GHM, Pivot X, et al. Phase III study of ribociclib (LEE011) plus fulvestrant for the treatment of postmenopausal patients with hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–) advanced breast cancer (aBC) who have received no or only one line of prior endocrine treatment (ET): MONALEESA-3. J Clin Oncol. 2016;34(Suppl):Abstract TPS624.
Baselga J, Im S-A, Iwata H, et al. PIK3CA status in circulating tumor DNA (ctDNA) predicts efficacy of buparlisib (BUP) plus fulvestrant (FULV) in postmenopausal women with endocrine-resistant HR+/HER2– advanced breast cancer (BC): first results from the randomized, phase III BELLE-2 trial. San Antonio Breast Cancer Symposium. 2015;Abstract S6-01.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from comments received were made by the author based on their scientific and editorial merit.
Disclosures
Peter Schmid has received grants from AstraZeneca, Roche/Genentech, Novartis, OncoGenex, Medivation and Astellas, and has and received personal fees from AstraZeneca, Novartis, Pfizer, Boehringer, Bayer, Puma, Eisai, Celgene and Merck. Mark R. Nathan has nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/EA18F06030674CE1.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nathan, M.R., Schmid, P. A Review of Fulvestrant in Breast Cancer. Oncol Ther 5, 17–29 (2017). https://doi.org/10.1007/s40487-017-0046-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-017-0046-2