Abstract
Purpose
Pulmonary Embolism (PE) is the third leading cause of cardiovascular death, following myocardial infarction and stroke. The latest European Society of Cardiology (ESC) guidelines on PE recommend short-term prognostic stratification based on right ventricular (RV) overload detected by transthoracic echocardiography (TTE) or contrast-enhanced chest CT. The aim of the study is to find out which of the signs of right ventricular dysfunction best predicts in-hospital mortality (IHM).
Methods
This is a monocentric, retrospective study including adult patients admitted from the emergency department with a c-e cCT confirmed diagnosis of PE between January 2018 and December 2022 who underwent a TTE within 48 h.
Results
509 patients (median age 76 years [IQR 67–84]) were included, with 7.1% IHM. At univariate analysis, RV/LV ratio > 1 (OR 2.23, 95% CI 1.1–4.5), TAPSE < 17 mm (OR 4.73, 95% CI 2.3–9.8), the D-shape (OR 3.73, 95% CI 1.71–8.14), and LVEF < 35% (OR 5.78, 95% CI 1.72–19.47) resulted significantly correlated with IHM. However, at multivariate analysis including also haemodynamic instability, PESI class > II, and abnormal hs-cTnI levels, only LVEF < 35% (OR 5.46, 95% CI 1.32–22.61) resulted an independent predictor of IHM.
Conclusion
Despite the recognised role of TTE in the early management of patients with circulatory shock and suspected PE, signs of RV dysfunction have been shown to be poor predictors of IHM, whereas severely reduced LVEF is an independent risk factor for in-hospital death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute pulmonary embolism (PE) is one of the most frequent cardiovascular emergencies and is associated with a high mortality rate if left untreated [1]. The development of a predictive model that defines the outcome of patients affected by PE is fundamental for therapeutic management and identification of the correct hospitalization setting, with an important impact on hospital costs [2]. The most recent European guideline on PE [3] recommends the integrated use of clinical parameters, laboratory tests, and instrumental investigations to stratify the risk of in-hospital and 30-day death, identifying five mortality-risk categories (high, intermediate-high, intermediate, intermediate-low, and low). Risk categories are defined by the presence of hemodynamic instability, Pulmonary Embolism Severity Index (PESI) class III-IV or sPESI ≥ 1 (simplified PESI), instrumental evidence of overload of the right ventricle (RV) (documented by echocardiography or computed tomography [CT] angiography), and abnormally high-sensitivity cardiac troponin levels (hs-cTn) [3]. Among patients with PE, between 27 and 55% of normotensive patients have echocardiographic evidence of RV dysfunction, which has a significant impact on the prognosis [4]. Echocardiographic signs of RV dysfunction are (i) dilated RV with basal RV/left ventricle (LV) ratio > 1.0, (ii) the McConnell sign (right ventricular free wall akinesia with sparing of the apex), (iii) the D-shape sign (flattened interventricular septum), (iv) distended inferior vena cava with diminished inspirational collapsibility, (v) tricuspid annular plane systolic excursion (TAPSE) < 16 mm, (vi) the 60/60 sign (a combination of pulmonary acceleration time inferior to 60 ms and tricuspid regurgitation (TR) jet gradient of 60 mmHg), and (vi) decreased peak systolic (S’) velocity of the tricuspid annulus (< 9.5 cm/s) [3]. However, although the ratio between the right and left ventricles [4] and the TAPSE index are the most studied signs for their prognostic value [5], the prognostic role of each sign of RV dysfunction is not clear [6,7,8]. Moreover, there is little evidence relating to the predictive capacity of other echocardiographic parameters commonly evaluated in the Emergency Department (ED) [9], such as the ejection fraction of the left ventricle and systolic pulmonary arterial pressure (sPAP) [10]. Finally, signs of RV dysfunction have a debated role in terms of sensitivity and specificity, considering high-sensitivity troponin [11, 12]. The main objective of our study was to evaluate the prognostic value of echocardiographic parameters in predicting in-hospital mortality (IHM) in patients admitted from the ED with a contrast-enhanced chest CT-confirmed diagnosis of PE.
Materials and methods
This single-centre retrospective study was conducted in the Emergency Department (ED) of a tertiary-level university hospital located in a province with approximately 350,000 inhabitants, with more than 70,000 visits per year. The TRIPOD (transparent reporting of a multivariable prediction model for individual prognosis or diagnosis) statement has been followed in preparing this manuscript [13].
Patient selection
Inclusion criteria
All patients aged > 18 years admitted to the ED from 1st January 2018 to 31st December 2022 with a contrast-enhanced chest CT confirmed diagnosis of PE and who had undergone a comprehensive transthoracic echocardiography (TTE) performed by a Cardiologist within 48 h of diagnosis were included.
Exclusion criteria
All patients who did not undergo complete echocardiography within 48 h, pregnant women, and patients with incomplete data for score calculation ware excluded.
Clinical and laboratory parameters
For each patient, clinical and anamnestic data were obtained by querying the hospital computer system and re-evaluating ED assessment reports and inpatient medical records. Risk stratification was performed according to the 2019 ESC guidelines for PE [3] as follows: (i) high risk: haemodynamic instability; (ii) intermediate-high: haemodynamic stability, PESI class > II, RV dysfunction signs and abnormal hs-cTnI values; (iii) intermediate risk: haemodynamic stability, PESI class I or II, RV dysfunction signs and abnormal hs-cTnI values; (iv) intermediate-low risk: haemodynamic stability, PESI class I or II, and one or none between RV dysfunction signs and abnormal hs-cTnI; (v) low risk: haemodynamic stability, PESI class I or II, no signs of RV dysfunction and normal hs-cTnI. The presence of hemodynamic instability was defined according to the ESC guidelines on PE [3], and anamnestic and clinical data were collected to calculate the PESI score [13], including age (in years), sex, history of cancer, presence of heart failure, presence of chronic lung disease, heart rate (HR bpm, with cut-off ≥ 110), systolic blood pressure (SBP mmHg, with cut-off < 100), diastolic blood pressure (DBP, mmHg), respiratory rate (RR, with cutoff > 30 for a minute), body temperature (BT, with cutoff < 36°), mental state, and arterial haemoglobin saturation (SpO2%, with cutoff < 90%) presented at admission in the ED. Elevated cardiac troponin levels were determined using hs-cTn I, with a limit of detection of 2 ng/mL and abnormal values above 12 ng/mL for women and above 20 ng/mL for men.
Echocardiographic parameters
Echocardiographic data were retrieved retrospectively by a single investigator who was blinded to the other clinical data. The echocardiographic parameters evaluated were: (i) dilation of the RV defined as RV/LV > 1, (ii) presence of D-shape (flattened interventricular septum), (iii) reduced collapsibility of the inferior cava vein (< 50%), (iv) TAPSE (reported in millimetres [mm], defined as mildly reduced if < 21 mm and reduced if < 17 mm), (v) systolic pulmonary artery pressure (sPAP in mmHg, defined as increased if > 35 mmHg and severely increased if > 60 mmHg), and vi) left ventricular ejection fraction (LVEF) in %, defined as depressed if < 51% in men and < 54% in women, and severely depressed if < 35%. [14, 15]. Based on instrumental, clinical, and laboratory data, the in-hospital mortality risk class was calculated for each patient according to the ESC guidelines [3].
Statistics
Continuous data were described as median and interquartile range (IQR) and compared using the Mann–Whitney U-test amongst two different groups. Categorical data were reported as absolute numbers and percentages and compared using the Pearson chi-square test. Univariate and multivariate analyses were performed to test the predictive power of clinical and instrumental data for IHM. The independent predictive power of the echocardiographic elements was assessed by performing several multivariate analyses, each one including the elements of the 2019 ESC risk classification (haemodynamic instability, PESI class > II, and abnormal hs-ctni values) and one of the echocardiographic parameters assessed in the study. Statistical analyses were performed using SPSS v. 25 (Apache Software Foundation, Chicago, Illinois, USA) and MedCalc version 17.6 (MedCalc Software BVBA).
Results
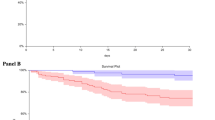
Overall, 783 patients were admitted to the ED with a final PE diagnosis during the study period. Of these, 274 were excluded because of the absence of an echocardiographic report performed within 48 h of admission to the ED, and 509 patients were finally included in this study. Included patients were male in 42.4% of cases, with a median age of 76 years (IQR 67–84), and 36 (7.1%) patients underwent IHM (Table 1). According to the ESC risk classification, 134 patients were identified at low risk (26.3%), 220 patients at intermediate-low risk (43.2%), 57 patients at intermediate risk (11.2%), 84 patients at intermediate-high risk (16.5%), and 14 high-risk patients (2.8%), with a mortality rate of 2.2%, 5%, 7%, 15.7%, and 33.3%, respectively (see Table 3). Patients who died were older with a median age of 84 years vs. 76 years (p 0.028), had a higher percentage of history of neoplasia (41.7% vs. 19.5%, p 0.002), and presented to the ED more frequently with an abnormal mental status (33% vs. 11.7%, p = 0.002), a HR > 110 bpm (44.4% vs. 12.3%, p = 0.001), a SpO2 < 90% (38.9% vs. 14.6%, p 0.001), and a PESI class > II (80% vs. 60%, p < 0.019). Moreover, patients who did not survive had higher hs-cTnI levels (median 125 [IQR 44–290] vs. 12 [IQR 5–74], p = 0.002). On echocardiography, patients who died in hospital had a higher incidence of RV/LV > 1 (38.9% vs. 22.2%, p = 0.002) and D-shape (32.4% vs. 11.3%, p < 0.001). There was no statistically significant difference in the percentage of mildly reduced TAPSE, while the percentage of reduced TAPSE was higher in patients who underwent IHM (38.9% vs. 11.8%, p < 0.001). While median LVEF values were similar between deceased and survivors (55% vs. 60%, p = 0.022), the percentage of patients with severely reduced LVEF was higher in patients who underwent IHM (11.1% vs. 2.1%, p = 0.001). The differences in sPAP values and inferior vena cava collapsibility between the deceased and surviving patients were not significant. (Table 2).
All assessed echocardiographic signs correlated significantly with the severity of PE according to the 2019 ESC risk classes, except for LVEF 35–55% and reduced inferior vena cava collapsibility (Table 3). On univariate analysis, the independent predictors of IHM were RV/LV ratio > 1 (OR 2.23, 95% CI 1.1–4.5), TAPSE < 17 mm (OR 4.73, 95% CI 2.3–9.8), the D-shape (OR 3.73, 95% CI 1.71–8.14), and LVEF < 35% (OR 5.78, 95% CI 1.72–19.47). Overall, except for reduced inferior vena cava collapsibility, the presence of any RV dysfunction was an independent predictor of mortality (OR 3.36, 95% CI 1.76–6.68). At multivariate analyses, only LVEF < 35% proved to be a significant independent predictor of IHM (OR 5.46, 95% CI 1.32–22.61) in the model, including hemodynamic instability (OR 3.99, 95% CI 1.15–14.4), PESI class > II (OR 1.59, 95% CI 0.61–4.15), and abnormal hs-cTnI values (OR 6.84, 95% CI 2.42–19.33) (Table 4). Excluding patients with hemodynamic instability, RV/LV > 1 and TAPSE < 17 mm did not correlate with IHM in univariate analysis, while D-shape (OR 2.55, 95% CI 1.03–6.3), the presence of any RV dysfunction other than reduced inferior vena cava collasibility (OR 2.58, 95% CI 1.23–5.41), and severely reduced LVEF (OR 6.1, 95% CI 1.53–24.25) predicted IHM.
Discussion
Pulmonary embolism is a life-threatening emergency, and rapid and accurate risk stratification with respect to mortality in the early stages is a fundamental step in patient management [3]. Our study underlined that patients who died in hospitals were older, had a higher prevalence of neoplasms, and were more likely to have hemodynamic instability. According to the ESC risk classification, IHM was progressive depending on the risk category, and 33% of high-risk patients underwent IHM [16]. Except for inferior vena cava collapsibility < 50%, all echocardiographic signs of RV dysfunction were more common in intermediate-high and high-risk patients; however, only RV/LV > 1, D-shape, and a TAPSE < 17 mm were associated with IHM. In addition, when considering the ESC risk classification, none of the individual echocardiographic signs of RV dysfunction included in a model with heamodinamic instability, PESI class > II, or abnormal hs-cTnI values were found to be significant independent predictors of IHM. Only the presence of severely reduced LVEF was independently associated with IHM. Acute RV dysfunction is a key factor contributing to hemodynamic collapse and death in acute PE [17]. If > 30–50% of the total cross-sectional area of the pulmonary arterial bed is occluded by the PE, the acute rise in pulmonary arterial pressure causes a sharp increase in pulmonary vascular resistance (PVR) that cannot be exceeded by RV contractile capacity. The increase in RV pressure causes increasing wall tension and myocyte elongation, with resultant RV dilatation that profoundly alters the contractile capabilities of the RV and impairs the Frank-Starling mechanism. Abnormal RV function impairs left ventricular (LV) function and impairs LV filling in early diastole. Cardiac output can be severely impaired by both ventricular desynchronization and reduced venous return from the pulmonary circulation, leading to circulatory collapse. Therefore, both cardiac status prior to acute PE in terms of RV contractility and LVEF appear to be critical in determining the ability of the heart to overcome the acute increase in PVR [3]. However, only RV imaging and function are recommended in the 2019 ESC guidelines for the risk stratification of PE patients [3]. Overall, signs of RV dysfunction are found in up to > 25% of patients with PE [18], and RV/LV > 1 and TAPSE < 17 mm are the most commonly reported parameters associated with IHM [5], but the positive predictive value of RV dysfunction for PE-related death overall appears to be < 10% [19]. Although previous studies have shown RV dilation to be an independent predictor of mortality [20, 21], with sensitivity and specificity for IHM of 72% and 58%, respectively [22], and reduced TAPSE has been shown to be an independent predictor of mortality [5, 23], the prognostic role of RV overload appears to be controversial. According to Cimini et al. [7], considering all patients with PE, an increased RV/LV ratio (risk ratio 1.61, 95% CI 1.90–2.39]) and a severely reduced TAPSE (risk ratio 2.29, 95% CI 1.45–3.59) correlated with short-term death; however, in hemodynamically stable patients, neither an abnormal TAPSE nor an increased RV/LV ratio showed a significant association with death when considered individually. While this finding is consistent with the present study, it contrasts with another recent systematic review that demonstrated the significant prognostic role of an increased RV/LV ratio in both hemodynamically unstable and stable patients with PE [6]. Such differences may be related to the different definitions of RV dysfunction used in different studies [7], and a definitive standardisation of RV dysfunction seems necessary. According to the ESC guidelines [3], and especially in hemodynamically stable patients, only a combination of different signs may be suitable for correct prognostic stratification [22]. Several authors investigated the role of different, complex measures of RV function, such as pulmonary vascular resistance [PVR], eccentricity index, fractional area change (FAC) of the RV, as well as global RV wall strain and free wall strain, in predicting IHM, with conflicting results; thus, their role in initial risk stratification needs to be further established [8, 24].
In the present study, LVEF showed a significant impact on mortality, both in all patients and in hemodynamically stable ones. Severely reduced LVEF was found in 20% of patients in a high-risk class and only in less than 3% of patients in other classes, and it has consistently been demonstrated to be a predictor of mortality in both univariate and multivariate analyses. Severely reduced LVEF appears to be the only echocardiographic sign that correlates with a higher risk of death from EP, independent of hemodynamic status, PESI class, and hs-cTnI values. Patients with a history of heart failure with reduced EF have a higher risk of death than patients with heart failure with preserved EF [25]. Dahhan et al. [26] observed that LVEF < 40% was present in 20% of patients who died of EP and in 5% of patients who survived. The role of LV function on early and long-term mortality has been recognised by Khemasuwan et al., demonstrating that LVEF and LV end-diastolic diameter are significantly associated with ICU death, IHM, and long-term survival after adjustment for APACHE score, PESI score, and age and gender, respectively [8]. Furthermore, the ratio of sPAP to left ventricular systolic volume (LVSV) ≥ 1.0 mmHg/ml was found to be a predictor of IHM with an OR of 2.31 (95%CI 1.3–4.2, p-value = 0.005) [10], and reduced stroke volume is associated with both PE-associated IHM and cardiopulmonary decompensation in intermediate-risk patients (OR 1.37, IC 95% 1.23–1.52, p-value < 0.001) [27].
This study has several limitations. First, it is a retrospective study conducted in a single centre; second, it only included patients who underwent formal TTE, excluding patients who died before formal TTE or who refused hospital admission; third, it did not include all parameters of RV function mentioned in the ESC guidelines [3]. However, hyperacute formal TTE is rarely performed in the ED, and point-of-care ultrasound (POCUS) [28, 29] or focused cardiac ultrasound (FoCUS) [30, 31] are more easily implemented in this setting. In our opinion, the prognostic role of POCUS or FOCUS must be evaluated separately from the role of formal TTE, since these three examinations are performed with profoundly different echocardiographic instruments and by different experienced providers. Moreover, in the hyperacute phase with hemodynamic instability, in accordance with the 2019 ESC guidelines on PE, both dysfunction on computed tomography pulmonary angiography (CTPA) and POCUS/FoCUS are useful in determining the high risk in patients with PE or excluding the diagnosis of PE [3]. The 2019 ESC guidelines on PE reported that different TTE signs of RV overload, such as the McConnel sign and the “60/60 sign,” are present in only 12–20% of unselected patients with PE, and data from RV Doppler tissue imaging and wall strain assessment have very low sensitivity as stand-alone findings, as they were reported to be normal in hemodynamically stable patients despite the presence of PE [3]. Moreover, these data are not regularly collected by most echocardiographic laboratories; thus, the clinical utility of these latter findings remains unclear.
Conclusion
In conclusion, echocardiography remains a useful tool for determining the prognosis of patients with acute pulmonary embolism, especially when combined with the use of clinical scores and troponin dosing. Despite the recognised role of acute RV dysfunction in the pathogenesis of death in PE, the prognostic role of echocardiographic signs of RV dysfunction remains to be determined. In addition, reduced LVEF was found to be a significant independent predictor of IHM. Although further studies are needed to definitively clarify its role in acute pulmonary embolism, reduced LVEF may be a significant parameter to include in risk stratification of early mortality in patients with acute pulmonary embolism.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available, but are available from the corresponding author on reasonable request, upon approval by the local ethics committee.
References
Essien EO, Rali P, Mathai SC (2019) Pulmonary embolism. Med Clin North Am 103(3):549–564. https://doi.org/10.1016/j.mcna.2018.12.013
Motte S, Mélot C, Di Pierdomenico L, Martins D, Leclercq P, Pirson M (2016) Predictors of costs from the hospital perspective of primary pulmonary embolism. Eur Respir J 47(1):203–211. https://doi.org/10.1183/13993003.00281-2015
Konstantinides SV, Meyer G, Becattini C et al (2020) 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 41(4):543–603. https://doi.org/10.1093/eurheartj/ehz405
Kreit JW (2004) The impact of right ventricular dysfunction on the prognosis and therapy of normotensive patients with pulmonary embolism. Chest 125(4):1539–1545. https://doi.org/10.1378/chest.125.4.1539
Pruszczyk P, Goliszek S, Lichodziejewska B et al (2014) Prognostic value of echocardiography in normotensive patients with acute pulmonary embolism. JACC Cardiovasc Imaging 7(6):553–560. https://doi.org/10.1016/j.jcmg.2013.11.004
Prosperi-Porta G, Ronksley P, Kiamanesh O, Solverson K, Motazedian P, Weatherald J (2022) Prognostic value of echocardiography-derived right ventricular dysfunction in haemodynamically stable pulmonary embolism: a systematic review and meta-analysis. Eur Respir Rev 31(166):220120. https://doi.org/10.1183/16000617.0120-2022
Cimini LA, Candeloro M, Pływaczewska M et al (2023) Prognostic role of different findings at echocardiography in acute pulmonary embolism: a critical review and meta-analysis. ERJ Open Res 9(2):00641–02022. https://doi.org/10.1183/23120541.00641-2022
Khemasuwan D, Yingchoncharoen T, Tunsupon P et al (2015) Right ventricular echocardiographic parameters are associated with mortality after acute pulmonary embolism. J Am Soc Echocardiogr 28(3):355–362. https://doi.org/10.1016/j.echo.2014.11.012
D’Andrea A, Del Giudice C, Fabiani D et al (2023) The incremental role of multiorgan point-of-care ultrasounds in the emergency setting. Int J Environ Res Public Health 20(3):2088. https://doi.org/10.3390/ijerph20032088
Dahhan T, Siddiqui I, Tapson VF et al (2016) Clinical and echocardiographic predictors of mortality in acute pulmonary embolism. Cardiovasc Ultrasound 14(1):44. https://doi.org/10.1186/s12947-016-0087-y
Weekes AJ, Johnson AK, Troha D, Thacker G, Chanler-Berat J, Runyon M (2017) Prognostic value of right ventricular dysfunction markers for serious adverse events in acute normotensive pulmonary embolism. J Emerg Med 52(2):137–150. https://doi.org/10.1016/j.jemermed.2016.09.002
Becattini C, Maraziti G, Vinson DR et al (2021) Right ventricle assessment in patients with pulmonary embolism at low risk for death based on clinical models: an individual patient data meta-analysis. Eur Heart J 42(33):3190–3199. https://doi.org/10.1093/eurheartj/ehab329
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594. https://doi.org/10.1136/bmj.g7594
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1-39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Alerhand S, Sundaram T, Gottlieb M (2021) What are the echocardiographic findings of acute right ventricular strain that suggest pulmonary embolism? Anaesth Crit Care Pain Med 40(2):100852. https://doi.org/10.1016/j.accpm.2021.100852
Elias A, Mallett S, Daoud-Elias M, Poggi JN, Clarke M (2016) Prognostic models in acute pulmonary embolism: a systematic review and meta-analysis. BMJ Open 6(4):e010324. https://doi.org/10.1136/bmjopen-2015-010324
Konstantinides SV (2014) 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 35(45):3145–3146. https://doi.org/10.1093/eurheartj/ehu393
Kurnicka K, Lichodziejewska B, Goliszek S et al (2016) Echocardiographic pattern of acute pulmonary embolism: analysis of 511 consecutive patients. J Am Soc Echocardiogr 29(9):907–913. https://doi.org/10.1016/j.echo.2016.05.016
Coutance G, Cauderlier E, Ehtisham J, Hamon M, Hamon M (2011) The prognostic value of markers of right ventricular dysfunction in pulmonary embolism: a meta-analysis. Crit Care 15(2):R103. https://doi.org/10.1186/cc10119
Becattini C, Agnelli G, Lankeit M et al (2016) Acute pulmonary embolism: mortality prediction by the 2014 European Society of Cardiology risk stratification model. Eur Respir J 48(3):780–786. https://doi.org/10.1183/13993003.00024-2016
Sanchez O, Trinquart L, Planquette B et al (2013) Echocardiography and pulmonary embolism severity index have independent prognostic roles in pulmonary embolism. Eur Respir J 42(3):681–688. https://doi.org/10.1183/09031936.00097512
Frémont B, Pacouret G, Jacobi D, Puglisi R, Charbonnier B, de Labriolle A (2008) Prognostic value of echocardiographic right/left ventricular end-diastolic diameter ratio in patients with acute pulmonary embolism: results from a monocenter registry of 1416 patients. Chest 133(2):358–362. https://doi.org/10.1378/chest.07-1231
Lobo JL, Holley A, Tapson V et al (2014) Prognostic significance of tricuspid annular displacement in normotensive patients with acute symptomatic pulmonary embolism. J Thromb Haemost 12(7):1020–1027. https://doi.org/10.1111/jth.12589
Pruszczyk P, Kurnicka K, Ciurzyński M et al (2020) Defining right ventricular dysfunction by echocardiography in normotensive patients with pulmonary embolism. Pol Arch Intern Med 130(9):741–747. https://doi.org/10.20452/pamw.15459
Lee K, Kwon O, Lee EJ et al (2019) Prognostic value of echocardiographic parameters for right ventricular function in patients with acute non-massive pulmonary embolism. Heart Vessels 34(7):1187–1195. https://doi.org/10.1007/s00380-019-01340-1
Obradovic S, Dzudovic B, Subotic B et al (2020) Predictive value of heart failure with reduced versus preserved ejection fraction for outcome in pulmonary embolism [published correction appears in ESC Heart Fail 2022 Jun;9(3):2058]. ESC Heart Fail 7(6):4061–4070. https://doi.org/10.1002/ehf2.13015
Kamran H, Hariri EH, Iskandar JP et al (2021) Simultaneous pulmonary artery pressure and left ventricle stroke volume assessment predicts adverse events in patients with pulmonary embolism. J Am Heart Assoc 10(18):e019849. https://doi.org/10.1161/JAHA.120.019849
Prosperi-Porta G, Solverson K, Fine N, Humphreys CJ, Ferland A, Weatherald J (2020) Echocardiography-derived stroke volume index is associated with adverse in-hospital outcomes in intermediate-risk acute pulmonary embolism: a retrospective cohort study. Chest 158(3):1132–1142. https://doi.org/10.1016/j.chest.2020.02.066
Yoshida T, Yoshida T, Noma H, Nomura T, Suzuki A, Mihara T (2023) Diagnostic accuracy of point-of-care ultrasound for shock: a systematic review and meta-analysis. Crit Care 27(1):200. https://doi.org/10.1186/s13054-023-04495-6
Spampinato D, Luppi F, Cristofaro E et al (2023) Diagnostic accuracy of Point Of Care UltraSound (POCUS) in clinical practice: a retrospective, emergency department based study. J Clin Ultrasound. https://doi.org/10.1002/jcu.23619
Via G, Hussain A, Wells M et al (2014) International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr 27(7):683.e1-683.e33. https://doi.org/10.1016/j.echo.2014.05.001
Funding
Open access funding provided by Università degli Studi di Ferrara within the CRUI-CARE Agreement. RDG was supported by FAR (Fondo Ateneo Ricerca) and FIR (Fondo Incentivazione Ricerca) funds from the University of Ferrara, Italy.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Andrea Portoraro, Francesco Luppi, Marcello Benedetto, Luca D’Angelo, Giorgio Galizia, Irma Sofia Fabbri, and Teresa Pagano; analysis was performed by Michele Domenico Spampinato, Giulia Passarini, and Rita Pavasini. The first draft of the manuscript was written by Michele Domenico Spampinat; the manuscript was critically reviewed by Matteo Guarino, Angelina Passaro, Rita Pavasini, Soccorsa M. Sofia and Roberto De Giorgio, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was conducted in accordance with the principles of the Declaration of Helsinki and has been approved by the local ethics committee (CE AVEC:549/2022/Oss/AOUFe.).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Spampinato, M.D., Portoraro, A., Sofia, S.M. et al. The role of echocardiography in pulmonary embolism for the prediction of in-hospital mortality: a retrospective study. J Ultrasound (2024). https://doi.org/10.1007/s40477-024-00874-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40477-024-00874-z