Abstract
Purpose of Review
This review discusses the trends of bacteraemia and their outcomes in tropical regions of Australia. Bacteraemia can frequently lead to severe sepsis and potentially life-threatening consequences. Epidemiology of bacteraemia is ever evolving.
Recent Findings
This review outlines the current patterns of bacteraemia in tropical regions of Australia, focusing on their outcomes and associated risk factors. The most frequently reported causes of bacteraemia were Staphylococcus aureus and Escherichia coli. There has been an increase in published incidence of Group A Streptococcus, methicillin-resistant Staphylococcus aureus and Burkholderia pseudomallei bacteraemia cases, while Streptococcus pneumoniae bacteraemia exhibited a declining trend. Factors specific to tropical environments and the higher representation of Indigenous populations in these areas were identified as contributing to the elevated incidence rates.
Summary
Bacteraemia was found to be an increasing healthcare burden to the Australian tropical regions. Ideally, linkage of existing data from healthcare settings could be utilised to obtain more accurate, comprehensive and up to date information of trends and patterns of bacteraemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacteraemia can frequently lead to severe sepsis and potentially life-threatening consequences. According to the Global Burden of Disease Study, bloodstream infections have caused more than 2 million deaths globally in 2019 [1]. Furthermore, bacteraemia is increasing globally and is predicted to increase in the future [2,3,4,5]. The drivers of increasing bacteraemia rates are manifold including changes in host characteristics, changes in pathogens and changes in healthcare systems and technologies [6, 7]. Environmental factors like temperature, rainfall, humidity also play a role [8, 9]. So, it is not surprising that there are regional differences in trends of bacteraemia and its outcomes. Knowledge on local pathogens causing bacteraemia and their temporal variations is helpful for individualising patient management with well selected empirical antibiotic treatment, and for early detection of outbreaks [6, 10].
This review describes the trends of bacteraemia and their outcomes in tropical regions of Australia. Many studies conducted in tropical Australia were focused on a single organism in a single setting. This review synthesises these studies and visualises the trends of common organisms in tropical Australia.
Tropical regions of Australia include Northern region of Western Australia, Northern Territory and Northern Queensland (Fig. 1). These regions have an average warm temperature all year round. In addition, these regions have a high proportion of Indigenous people. Northern Territory has the highest proportion of Indigenous people (30.3%) while Queensland and Western Australia have a proportion of 4.7% and 4.1% respectively [12]. Bacteraemia is recognized to correlate with comorbidities and low socioeconomic status, both of which are prevalent among Indigenous populations. Consequently, tropical regions face elevated risks of bacteraemia compared to other regions [13].
Tropical regions of Australia. The Australian Bureau of Meteorology climate classification by Martyman under CC BY-SA 3.0 [11]
Methodology
Search Strategy
Published literature was assessed through PubMed, EMBASE, Scopus and Web of Science from 1995 until November 2023 to identify studies on bacteraemia conducted in Australian tropical settings. The search terms used were ‘bacteraemia’, ‘bacteremia’, ‘blood stream infection’, ‘Australia’, ‘Northern Territory’, ‘Queensland’ and ‘Western Australia’. Furthermore, the common pathogens causing bacteraemia were searched by their pathogen name; ‘Staphylococcus aureus’, ‘methicillin resistant staphylococcus aureus’, ‘MRSA’, ‘Group A Streptococcus’, ‘Streptococcus pyogenes’, ‘Group B Streptococcus’, ‘Streptococcus pneumoniae’, ‘Escherichia coli’, ‘Klebsiella’, ‘Burkholderia pseudomallei’, ‘Salmonella’ and ‘nontyphoidal Salmonella’. Studies conducted before 1995 were excluded.
Analysis
We found a high variability in the units used to present incidence data in the studies reviewed. Therefore, we converted all findings to incidences calculated ‘per 100,000 population per year’ using either the population information reported on the article or using Australian Bureau of Statistics census data [14, 15]as shown in Table 1.
Results
In this section epidemiological trends, severe outcomes and risk factors of common organisms causing bacteraemia in tropical settings will be discussed.
Staphylococcus aureus Bacteraemia
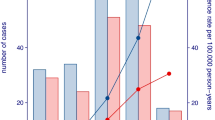
S. aureus was the commonest cause of bacteraemia in tropical Australia [17, 18, 20]. The annual incidence of S. aureus bacteraemia in tropical Australia ranged between 17 and 96 per 100,000 population during the period 2000 to 2019 according to the studies conducted in Northern Territory and Northern Queensland [16,17,18,19,20,21] (Table 1). The rates were lower in children which was around 10 to 20 cases per 100,000 population [22, 23]. High incidence of S. aureus bacteraemia was observed among the Indigenous patients compared to non-Indigenous [16, 19, 23, 31]. Many long-term studies conducted during 2000 to 2020 in tropical Australia revealed a decline in S. aureus bacteraemia [17, 20, 22]. This could be attributable to infection control measures in healthcare settings [20]. It is notable these findings run counter to the global trends. According to a systematic review, in the global setting, there were variable trends for S. aureus bacteraemia with no significant change in the incidence across the included countries from 2000 to 2020 [32].
Incidence rates of S. aureus bacteraemia in tropical Australia were found to be higher than that of the national rates. Annual incidence of S. aureus bacteraemia in Australia between 1999 and 2010 ranged from 11.2 to 35 per 100,000 population [31, 33], whereas the annual incidence of S. aureus bacteraemia in tropical Australia was as high as 96.6 per 100,000 population in some parts [17]. The latter study was conducted in the Northern Territory and described a high proportion of Indigenous people and numerous comorbidities.
Crude mortality rate of S. aureus bacteraemia in tropical Australia, ranged between 4 and 8% [16, 18]. Interestingly, a study conducted in Australia and New Zealand revealed a low mortality rate (7%) for Indigenous patients compared to non-Indigenous (17%) [31]. The probable explanation for this could be that Indigenous patients had a younger average age of acquisition of the infection [31].
MRSA Bacteraemia
The annual incidence of MRSA bacteraemia in tropical Australia ranged between 3.8 and 17 per 100,000 population within 2004 to 2015 [16, 18, 20,21,22] (Table 1). MRSA has different strains which can be differentiated based on resistance to non-methicillin antibiotics. Multiresistant MRSA (mrMRSA) exhibit resistance to multiple classes of antibiotics and are comparatively common in hospitals, whereas Non-multiresistant MRSA (nmMRSA) remain susceptible to some classes of antibiotics (cotrimoxazole, clindamycin and macrolides) and are comparatively common in the community.
Studies conducted in different tropical settings reported different trends of MRSA bacteraemia. The 10-year study conducted in Northern Queensland found that overall incidence of MRSA did not change significantly over the study period. However, mrMRSA significantly reduced during this period (P = 0.04) while nmMRSA increased, which was not statistically significant (P = 0.125) [20]. A paediatric study conducted in Northern Queensland from 2001 to 2010 revealed an increase in the number of MRSA bacteraemia during the study period [22].
Northern Australia, as noted by Murray et al. (2004), experienced a surge in community-onset MRSA bacteremia [21]. This increase in community-acquired MRSA infections has been noted throughout Australia. [33, 34]. A study conducted in 17 Australian hospitals revealed that 40% of the S. aureus bacteraemia episodes were hospital onset MRSA while 12% were of community onset [33]. Crowded living conditions, poor hygiene and heavy use of broad-spectrum antibiotics are proposed mechanisms by which there is increasing emergence of community acquired MRSA [35].
MRSA bacteraemia was found to be more prevalent among Indigenous people [19, 31]. Female sex and remote residence were significantly associated with resistant strains of MRSA compared to sensitive strains [16]. Mortality rates of MRSA ranged between 2% (MSSA) to 4.5% (MRSA) [16].
Group A Streptococcus (GAS) Bacteraemia
GAS bacteraemia is an invasive disease which frequently leads to life threatening consequences such as septicaemia and streptococcal toxic shock syndrome (STSS). Incidence of GAS bacteraemia among the general population in tropical Australia ranged between 7.45 and 20 per 100,000 population per year [17, 20, 24,25,26, 36] (Table 1). A high incidence rate for GAS bacteraemia was observed among Indigenous populations. Three large studies conducted in North Queensland and Northern Territory during 1996 to 2014 period revealed that the incidence among Indigenous population was 4–10 times higher compared to the total population incidence [24,25,26]. A paediatric study conducted in Northern Queensland from 2001 to 2010 revealed a relatively lower rate of incidence of GAS bacteraemia fluctuating between 0 and 7 per 100,000 population over the study period [22].
A significant rise in GAS bacteraemia was observed in Northern Territory during 1999 to 2019 period [17] while it was stable in Northern Queensland during 1996 to 2009 [36]. A steep rise in the reported incidence of invasive GAS (iGAS) disease across Australia was observed during 2018 to 2022 period from a large study [37]. This increase in reported case numbers could be due to increased case detection rate as a result of iGAS becoming a nationally notifiable disease during the period 2005 to 2021 in Australia [38]. Increasing incidence rates were observed in global literature as well [24, 39]. Likewise, Indigenous communities were at increased risk of infection with GAS globally [40, 41]. This can be explained by the strong relation of this pathogen to the social determinants of health, where Indigenous communities experience more socioeconomic disadvantages comparatively [26, 42].
Having chronic diseases like diabetes, chronic kidney disease, cardiac diseases and receiving dialysis were risk factors for GAS bacteraemia [26]. According to literature from tropical Australia, crude mortality rate of GAS bacteraemia ranged between 5.6 and 13.8% [24,25,26, 36]. Proportion of cases requiring ICU admissions varied from 15.0 to 23.6% while STSS was reported from 6.6 to 16.3% of these patients [25, 26]. Antimicrobial resistance was present in 19.2%, most commonly to tetracycline [26].
Group B Streptococcus (GBS) Bacteraemia
Group B Streptococcus frequently causes morbidity and mortality among vulnerable populations, such as pregnant mothers, newborns, and the elderly [36]. GBS bacteraemia can lead to sepsis, pneumonia and meningitis. Studies conducted in Northern Queensland from 1996 to 2020 revealed a rise in incidence from 4.3 to 11.4 per 100,000 per year [20, 27, 36]. The incidence of GBS bacteraemia was about 2.5 times higher among the Indigenous population compared to non-Indigenous population [27]. However, another high-risk group was the non-Indigenous older females [36]. One important observation throughout the studies was that GBS bacteraemia was deviating from being predominantly a neonatal and maternal infection to become a non-neonatal and non-pregnant infection [27, 36]. This change was observed in studies conducted globally [43,44,45,46,47]. Another interesting observation was that as age advanced, a switch from Indigenous cases to non-indigenous became apparent [27].
Presence of comorbidities was a risk factor for GBS bacteraemia [27]. Crude mortality rate was 3.6% [36] with an increased risk among males and immunosuppressed patients [27].
Streptococcus pneumoniae Bacteraemia
S. pneumoniae bacteraemia was found to be the commonest bacteraemia among children in tropical Australia [22]. Three recently conducted studies in tropical Australia between 2000 and 2019 revealed a reduction in reported S. pneumoniae bacteraemia [17, 20, 22] (Table 1). This decrease can largely be attributed to the successful pneumococcal vaccination programs in tropical Australia [20]. There was insufficient research on S. pneumoniae bacteraemia from tropical Australia to describe the associated risk factors and mortality.
Escherichia coli and Klebsiella pneumoniae Bacteraemia
E. coli was found to be the commonest gram-negative organism causing bacteraemia in Australian tropical regions [17, 18, 20]. The incidence of E. coli bacteraemia in the general population ranged between 19 and 48 per 100,000 per year during 2004 to 2020 in tropical Australia [17, 18, 20, 22]. There was conflicting evidence on trends of E. coli bacteraemia reported from tropical Australia. One study reported a 2.5 fold increase in the incidence of E. coli bacteraemia from 1999 to 2019 surpassing the number of S. aureus bacteraemia at the end of the study period [17]. But a more stable trend was observed in the paediatric population according to a study conducted in Northern Queensland from 2001 to 2010 [22]. However, an increas in incidence was observed globally for E. coli bacteraemia especially in European countries [48, 49].
E. coli was noted to have a decrease in its susceptibility to gentamicin over the study period [20]. Crude mortality rate of E. coli bacteraemia was found to be around 10% [18].
Klebsiella spp. were found to be frequent pathogens causing gram negative bacteraemia in tropical Australia ranging between 3 and 18 per 100,000 per year during 1999 to 2019 [17, 18, 20, 22] (Table 1). A significant increase in the incidence of Klebsiella bacteraemia was reported from Northern Territory [17].
Burkholderia pseudomallei Bacteraemia
B. pseudomallei is an organism predominantly found in tropical and subtropical regions causing melioidosis. This has a strong seasonal preference, occurring in wet season [50]. Bacteraemia is a common consequence of melioidosis. In Northern Queensland and Northern Territory of Australia the incidence of B. pseudomallei bacteraemia ranged between 3 and 19 per 100,000 per year during 1998 to 2020 with an increase in incidence over that period [17, 18, 20, 28,29,30, 51] (Table 1). History of diabetes, excessive alcohol intake, immunosuppression, male sex, low socioeconomic status and wet season presentation were found to be associated with occurrence of B. pseudomallei bacteraemia [18, 28, 30].
Melioidosis leading to bacteraemia was significantly associated with ICU admission and mortality [30].
Non-typhoidal Salmonella (NTS) Bacteraemia
NTS is a common isolate among the immunocompromised patients and is the commonest gram negative cause of bacteraemia in sub-Saharan Africa where HIV prevalence is high [52]. There were few studies in tropical Australia that described NTS bacteraemia, with conflicting findings. There was an increasing trend over time in the incidence of NTS bacteraemia throughout all age groups, according to a study conducted in the Northern Territory [17]. But a paediatric study conducted within the same period in Northern Queensland revealed a declining trend [22]. There was an increase in the incidence of invasive nontyphoidal Salmonella (iNTS) in another study conducted in Queensland with high rates among males, infants, and elderly people [53].
Discussion
Bacteraemia is increasing worldwide. This review describes the recent trends of bacteraemia in Australian tropical regions, their outcomes and risk factors.
The common organisms causing bacteraemia did not change largely among the studies conducted in tropical regions of Australia over the past 2 decades. According to the reviewed studies, the major organisms causing bacteraemia were S. aureus, Group A Streptococcus, S. pneumoniae, E. coli and Klebsiella out of which, S. aureus and E. coli were the commonest [17, 18, 20]. Outside of Australia, S. aureus and E. coli dominated the temperate regions like Europe and North America, E. coli being the leading cause of bacteraemia in Europe and S. aureus being the leading cause of bacteraemia in North America [54].
MRSA bacteraemia has been increasing globally according to many of the studies reviewed. In addition, increasing incidence of community acquired MRSA was observed in tropical Australia. High rates of comorbidities and high number of people per household amongst other components of socioeconomic disadvantage in the Indigenous community could be possible explanations for this.
High incidence rate of GAS Bacteraemia was found to be an increasing burden to the health care system due to frequent life threatening complications and ICU admissions. Improving the socioeconomic status and preventive strategies for noncommunicable diseases especially among Indigenous people who are at high risk is a timely need in this regard. Declaring iGAS a nationally notifiable disease in Australia and the global efforts in development of a vaccine to prevent GAS infections are two affirmative initiatives currently [55].
An increasing global trend was reported for GBS infections as also reflected in this review [47, 56]. The switch from being a neonatal pathogen to an adult pathogen which was observed in tropical Australia could be due to the increasing incidence of comorbidities among older population. This trend was observed in global literature as well [47, 57]. As for many of the organisms discussed previously, an Indigenous predominance was observed for this organism too, which can be attributed to the high incidence of chronic illnesses like diabetes and obesity among Indigenous people [27, 58]. However, the fact that advanced age caused a tendency towards non-Indigenous cases reflected the probable increase in risk factors for GBS bacteraemia among non-Indigenous and the relatively younger age distribution among Indigenous Australians.
S. pneumoniae which is a common organism causing bacteraemia in children and older adults was found to be decreasing in Australian tropical settings [17, 20, 22]. The introduction of an additional pneumococcal vaccine booster for Indigenous children which was implemented in year 2001 could be the likely reason for this [17]. Vaccine related decline of invasive pneumococcal disease in both children and adults was prominent in global literature too [59, 60].
E.coli and Klebsiella spp. were found to be the commonest gram negative organisms causing bacteraemia [17]. Both these organisms were observed to be increasing in tropical Australia during 1999 and 2019 [17]. Incidence of bacteraemia due to both these organisms increased with age in the global literature [61, 62]. Therefore, general increase in life expectancy and associated increase in comorbidities could explain the observed increasing incidence.
We highlighted increasing patterns of B. pseudomallei in this review. Similarly, it has been observed to be on the rise in several other tropical countries [63, 64]. Bacteraemia due to B. pseudomallei caused high healthcare burden with high ICU admissions and high mortality rates. As this organism is commonly found in soil and mud, preventive strategies at the community level such as educating people on wearing protective gear while working in high risk environments, especially during the wet season could be beneficial [65].
According to global evidence, NTS is a major cause of bacteraemia in African regions due to its strong association with HIV infection [66,67,68]. NTS bacteraemia rates are comparatively low in tropical Australia but have been increasing [17, 53]. This can be explained by the strong association of this disease with socio-economic status, poverty, poor housing conditions, food insecurity, chronic diseases and co-infections which are prevalent among the Indigenous community that is disproportionately distributed in Australian tropical regions [53].
Although this review described most epidemiological aspects relevant to bacteraemia in tropical settings of Australia, there were some limitations. Scarcity of research evidence on some organisms made it difficult to generalise the findings to the whole tropical Australia. Some studies were conducted at different time periods, making comparison difficult.
Conclusion and Recommendations
In conclusion, bacteraemia was found to be an increasing healthcare burden to the Australian tropical regions. Environmental factors unique to tropical regions partly contributed to this. The fact that tropical regions had a disproportionately high Indigenous population also caused tropical regions more vulnerable for high incidence of blood stream infections. Indigenous Australians were found to have higher incidence of bacteraemia irrespective of the causative organism, reflecting the socioeconomic disadvantages experienced by them. Measures to reduce the socioeconomic inequalities in tropical Australian settings is urgently needed. Vaccination as a public health measure was highly successful with a consistent decline in S. pneumoniae bacteraemia. Likewise, the importance of notification with regard to disease control showed this measure by increased reported cases.
Although a number of studies were conducted in tropical regions describing bacteraemia, inconsistent findings amongst the studies was common. This was probably due to differing methodology, different locations and different time periods. Ideally, linkage of existing data from healthcare settings could be utilised to obtain more accurate, comprehensive and up to date information of trends and patterns of bacteraemia.
Data Availability
No datasets were generated or analysed during the current study.
References
**Ikuta KS, et al. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2022;400(10369):2221–48. Global Burden of Disease Study is the most comprehensive worldwide observational epidemiological study to date. It reports a very high global burden of bacteraemia.
Goto M, Al-Hasan M. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19(6):501–9.
Kontula KS, et al. Population-based study of bloodstream infection incidence and mortality rates, Finland, 2004–2018. Emerg Infect Dis. 2021;27(10):2560.
Søgaard M, et al. Temporal changes in the incidence and 30-day mortality associated with bacteremia in hospitalized patients from 1992 through 2006: a population-based cohort study. Clin Infect Dis. 2011;52(1):61–9.
Wilson J, et al. Trends among pathogens reported as causing bacteraemia in England, 2004–2008. Clin Microbiol Infect. 2011;17(3):451–8.
García-Rodríguez J, Mariño-Callejo A. The factors associated with the trend in incidence of Bacteraemia and associated mortality over 30 years. BMC Infect Dis. 2023;23(1):69.
De Kraker M, et al. The changing epidemiology of bacteraemias in Europe: trends from the European Antimicrobial Resistance Surveillance System. Clin Microbiol Infect. 2013;19(9):860–8.
Bulterys PL, et al. Climatic drivers of melioidosis in Laos and Cambodia: a 16-year case series analysis. Lancet Planet Health. 2018;2(8):e334–43.
Sinclair HA, et al. Epidemiology of Aeromonas Species Bloodstream Infection in Queensland, Australia: Association with Regional and Climate zones. Microorganisms. 2023;11(1):36.
Gradel KO, et al. Impact of appropriate empirical antibiotic treatment on recurrence and mortality in patients with bacteraemia: a population-based cohort study. BMC Infect Dis. 2017;17:1–9.
Martyman. The Australian Bureau of Meteorology climate classification. 2005. p. The Australian Bureau of Meteorology climate classification, a modification of Köppen’s classification. Data from bom.gov.au.
Australian Institute of Health and Welfare. Profile of First Nations People. 2023.
Einsiedel L, et al. Non-communicable diseases, infection and survival in a retrospective cohort of indigenous and non-indigenous adults in central Australia. BMJ open. 2013;3(7):e003070.
Australian Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians. 2021 [cited 2023 03/07]; https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/estimates-aboriginal-and-torres-strait-islander-australians/latest-release.
Australian. Bureau of Statistics.
Tong SY, et al. Community-associated strains of methicillin-resistant Staphylococcus aureus and methicillin-susceptible S. aureus in indigenous Northern Australia: epidemiology and outcomes. J Infect Dis. 2009;199(10):1461–70.
Douglas NM, et al. Trends in bacteremia over 2 decades in the top end of the northern territory of Australia. Open Forum Infectious diseases. Oxford University Press US; 2020.
Douglas MW, et al. Epidemiology of community-acquired and nosocomial bloodstream infections in tropical Australia: a 12-month prospective study. Volume 9. Tropical medicine & international health: TM & IH; 2004. pp. 795–804. 7.
Marquess J, et al. Spatial analysis of community-onset Staphylococcus aureus bacteremia in Queensland, Australia. Infect Control Hosp Epidemiol. 2013;34(3):291–8.
Porter S, Ketheesan N, Norton R. Bacteraemias in tropical Australia: changing trends over a 10-year period. Diagn Microbiol Infect Dis. 2013;75(3):266–70.
Murray RJ, et al. Community-onset methicillin-resistant Staphylococcus aureus bacteremia in Northern Australia. Int J Infect Dis. 2004;8(5):275–83.
Er J, et al. Paediatric bacteraemias in tropical Australia. J Paediatr Child Health. 2015;51(4):437–42.
Engelman D, et al. Invasive Staphylococcus aureus infections in children in tropical northern Australia. J Pediatr Infect Dis Soc. 2014;3(4):304–11.
Norton R, et al. Invasive group a streptococcal disease in North Queensland (1996–2001). Indian J Med Res. 2004;119:148–51.
Gear RJ, et al. Changes in the clinical and epidemiological features of group a streptococcal bacteraemia in a ustralia’s N orthern T erritory. Tropical Med Int Health. 2015;20(1):40–7.
*Nguyen AD et al. The efficacy and safety of a shortened duration of antimicrobial therapy for group A Streptococcus bacteremia International Journal of Infectious Diseases, 2023. 128: pp. 11–19. This is a 7 year long study conducted in far North Queensland on Group A Streptococcus (GAS) bacteremia. Although the key objective of this study was to determine if shorter courses of antibiotic therapy for GAS bacteremia are associated with excess mortality, this study also reports the latest incidence of GAS bacteraemia in general and for Indigenous population.
*Alizzi M et al. Group B streptococcal bacteraemia: changing trends in a tropical region of Australia Internal medicine journal, 2022. 52(5): pp. 800–807. This is a recent study on Group B streptococcal bacteraemia conducted in North Queensland which is a tropical region in Australia. This study highlights the important finding of a change in trend; a deviation from being a neonatal pathogen to a pathogen affecting older non-Indigenous patients.
Hanson J, et al. Melioidosis-a disease of socioeconomic disadvantage. PLoS Negl Trop Dis. 2021;15(6):e0009544.
Gassiep I, et al. Melioidosis Queensland: an analysis of clinical outcomes and genomic factors. PLoS Negl Trop Dis. 2023;17(10):e0011697. This is a latest study on Melioidosis conducted in Queensland, tropical Australia reporting the incidence of Melioidosis in tropical Australia. This study reported that 71% of melioidosis cases developed to bacteraemia.
*Prinsloo C et al. The Epidemiological, Clinical, and Microbiological Features of Patients with Burkholderia pseudomallei Bacteraemia—Implications for Clinical Management Tropical Medicine and Infectious Disease, 2023. 8(11): p. 481. This is a latest study on Melioidosis conducted in Queensland, tropical Australia reporting the incidence of Melioidosis in tropical Australia. This study reported that 70% of melioidosis cases developed to bacteraemia.
Tong SY, et al. Impact of ethnicity and socio-economic status on Staphylococcus aureus bacteremia incidence and mortality: a heavy burden in indigenous australians. BMC Infect Dis. 2012;12(1):1–9.
Hindy J-R et al. Incidence trends and epidemiology of Staphylococcus aureus bacteremia: a systematic review of population-based studies. Cureus, 2022. 14(5).
Collignon P, et al. Staphylococcus aureus bacteremia, Australia. Emerg Infect Dis. 2005;11(4):554.
Turnidge JD, et al. Staphylococcus aureus bacteraemia: a major cause of mortality in Australia and New Zealand. Med J Aust. 2009;191(7):368–73.
Maguire GP, et al. Emerging epidemic of community-acquired methicillin‐resistant Staphylococcus aureus infection in the Northern Territory. Med J Aust. 1996;164(12):721–3.
Harris P, et al. Bacteraemia caused by beta-haemolytic streptococci in North Queensland: changing trends over a 14-year period. Clin Microbiol Infect. 2011;17(8):1216–22.
Abo Y-N, et al. Increase in invasive group a streptococcal disease among Australian children coinciding with northern hemisphere surges. The Lancet Regional Health–Western Pacific; 2023.
Hla TK, et al. Getting to grips with invasive group a streptococcal infection surveillance in Australia: are we experiencing an epidemic? Med J Aust. 2023;219(6):242–5.
Barnett TC, Bowen AC, Carapetis JR. The fall and rise of Group A Streptococcus diseases. Epidemiol Infect. 2018;147:e4.
Boyd R, et al. High burden of invasive group a streptococcal disease in the Northern Territory of Australia. Epidemiol Infect. 2016;144(5):1018–27.
Whitehead B, Smith H, Nourse C. Invasive group a streptococcal disease in children in Queensland. Epidemiol Infect. 2011;139(4):623–8.
Carapetis J, et al. Clinical and epidemiological features of group a streptococcal bacteraemia in a region with hyperendemic superficial streptococcal infection. Epidemiol Infect. 1999;122(1):59–65.
Baldan R, et al. Group B streptococcal colonization in elderly women. BMC Infect Dis. 2021;21:1–8.
Farley MM, Strasbaugh LJ. Group B streptococcal disease in nonpregnant adults. Clin Infect Dis. 2001;33(4):556–61.
High KP, Edwards MS, Baker CJ. Group B streptococcal infections in elderly adults. Clin Infect Dis. 2005;41(6):839–47.
Slotved H, Hoffmann S. The epidemiology of invasive group B Streptococcus in Denmark from 2005 to 2018. Front Public Health 2020; 8: 40. 2020.
Watkins LKF, et al. Epidemiology of invasive group B streptococcal infections among nonpregnant adults in the United States, 2008–2016. JAMA Intern Med. 2019;179(4):479–88.
Blandy O, et al. Factors that impact on the burden of Escherichia coli bacteraemia: multivariable regression analysis of 2011–2015 data from West London. J Hosp Infect. 2019;101(2):120–8.
Schlackow I, et al. Increasing incidence of Escherichia coli bacteraemia is driven by an increase in antibiotic-resistant isolates: electronic database study in Oxfordshire 1999–2011. J Antimicrob Chemother. 2012;67(6):1514–24.
Hanson J, Smith S. Melioidosis in northern Australia. Microbiol Australia. 2022;43(3):120–4.
Currie BJ, et al. The Darwin prospective melioidosis study: a 30-year prospective, observational investigation. Lancet Infect Dis. 2021;21(12):1737–46.
Acheson D, Hohmann EL. Nontyphoidal salmonellosis. Clin Infect Dis. 2001;32(2):263–9.
Parisi A, et al. Increasing incidence of invasive nontyphoidal Salmonella infections in Queensland, Australia, 2007–2016. PLoS Negl Trop Dis. 2019;13(3):e0007187.
Biedenbach DJ, Moet GJ, Jones RN. Occurrence and antimicrobial resistance pattern comparisons among bloodstream infection isolates from the SENTRY Antimicrobial Surveillance Program (1997–2002). Diagn Microbiol Infect Dis. 2004;50(1):59–69.
Dale JB, Walker MJ. Update on group a streptococcal vaccine development. Curr Opin Infect Dis. 2020;33(3):244–50.
Trivalle C, et al. Group B streptococcal bacteraemia in the elderly. J Med Microbiol. 1998;47(7):649–52.
Phares CR, et al. Epidemiology of invasive group B streptococcal disease in the United States, 1999–2005. JAMA. 2008;299(17):2056–65.
Jackson LA, et al. Risk factors for group B streptococcal disease in adults. Ann Intern Med. 1995;123(6):415–20.
Lynch JP, Zhanel GG. Streptococcus pneumoniae: epidemiology, risk factors, and strategies for prevention. In seminars in respiratory and critical care medicine. © Thieme Medical; 2009.
Feldman C, Anderson R. Recent advances in the epidemiology and prevention of Streptococcus pneumoniae infections. F1000Research, 2020. 9.
Bonten M, et al. Epidemiology of Escherichia coli bacteremia: a systematic literature review. Clin Infect Dis. 2021;72(7):1211–9.
Sawatwong P, et al. High burden of extended-spectrum β-lactamase–producing Escherichia coli and klebsiella pneumoniae bacteremia in older adults: a seven-year study in two rural Thai provinces. Am J Trop Med Hyg. 2019;100(4):943.
Ribolzi O, et al. Land use and soil type determine the presence of the pathogen Burkholderia pseudomallei in tropical rivers. Environ Sci Pollut Res. 2016;23:7828–39.
Sathkumara HD, et al. Clinical, Bacteriologic, and Geographic Stratification of Melioidosis Emerges from the Sri Lankan National Surveillance Program. Am J Trop Med Hyg. 2018;98(2):607–15.
Mohapatra P, Mishra B. Prevention of melioidosis. J Family Med Prim care. 2022;11(9):4981–6.
Gilchrist JJ, MacLennan CA. Invasive nontyphoidal Salmonella disease in Africa. EcoSal Plus, 2019. 8(2).
Gordon MA, et al. Epidemics of invasive Salmonella enterica serovar enteritidis and S. Enterica Serovar typhimurium infection associated with multidrug resistance among adults and children in Malawi. Clin Infect Diseases: Official Publication Infect Dis Soc Am. 2008;46(7):963–9.
MacLennan CA, et al. Dysregulated humoral immunity to nontyphoidal Salmonella in HIV-infected African adults. Science. 2010;328(5977):508–12.
Acknowledgements
We thank Mr Stephen Anderson, the Research and Learning Librarian at James Cook University Townsville, Bebegu Yumba campus.The first author is funded by the Australian Institute of Tropical Health and Medicine and James Cook University, Australia PhD programme. We thank Dr. Rojelio Mejia for reviewing the paper.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
HR and EM conceived the idea and design; created the manuscript outline. HR, EM, DE, OA, AP contributed to the method. HR wrote the introduction, methods section, results section, discussion and prepared the Table 1. EM, DE, OA and AP made critical comments, suggested final edits and revisions and supervised the writing. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ratnayake, H.E., Eisen, D.P., Adegboye, O.A. et al. Bacteraemia in Tropical Australia: A Review. Curr Trop Med Rep (2024). https://doi.org/10.1007/s40475-024-00326-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s40475-024-00326-y