Abstract
Purpose of Review
Normothermic machine perfusion (NMP) is a promising new tool in kidney transplantation to improve the outcome of marginal donor kidney transplantation. This review examines the current evidence for NMP in clinical practice and considers how the technology may be used in the future.
Recent Findings and Summary
There is emerging evidence to suggest that NMP has the potential to expand the donor pool of transplantable organs. The safety and feasibility of NMP have been established in a number of clinical studies but more research is needed to optimise the perfusion conditions. NMP shows promise as a viability assessment tool with particular focus on biomarkers and imaging techniques which provide real-time information to facilitate transplantation decision-making. Moreover, the exciting development of new potential therapeutics such as cell and gene-based therapies which are deliverable during NMP may also improve and recondition grafts prior to implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney transplantation is fundamental as a treatment for end-stage renal failure (ESRF); however, it is severely limited by the number of organs available. In order to meet this demand, there has been increased use of kidneys from donation after circulatory death (DCD) donors and from increasingly elderly and comorbid donor pools [1, 2]. These kidneys are more susceptible to the impacts of ischaemic reperfusion injury (IRI) and immunogenicity, the sequelae of which is delayed graft function (DGF), and higher rates of acute rejection and graft loss [3, 4]. Substantial work is currently being conducted on developing novel perfusion strategies to help mitigate these effects.
Normothermic machine perfusion (NMP) has emerged as a promising tool to assess, recondition and potentially treat kidneys for transplantation. This review will assess the current evidence for NMP and consider the future impact of the technology on clinical practice.
Why Normothermic Machine Perfusion?
The traditional method for the preservation of organs prior to transplantation is static cold storage (SCS), utilising the principles of hypothermia, in which organs are flushed with a preservation solution and then placed on ice for transport. The reduction in temperature reduces cellular metabolism by decreasing enzymatic activity and slowing the depletion of adenosine triphosphate (ATP) [5]. The preservation solutions themselves are designed to prevent intracellular acidosis, maintain cellular stability and flush the vasculature of the kidney [6]. Despite this, there is still inevitable cold ischaemic injury resulting in the loss of cell viability, with longer cold ischaemic times being directly proportional to DGF and graft loss [7]. This effect is exacerbated by the significant period of warm ischaemia particularly associated with DCD procurement.
Machine perfusion is not a new phenomenon, with hypothermic machines developed and utilised 60 years ago by Belzer et al. pre-dating the SCS techniques described above [8]. Its continual flow is able to prevent any build-up of unwanted metabolites and maintain cellular metabolism, albeit at a significantly reduced level [9]. The technique also promotes vasodilation within the microvasculature by reducing endothelin-1 levels, a potent vasoconstrictor, and increasing the levels of nitric oxide [10]. This technique has been adopted widely, with a plethora of studies and meta-analyses supporting its superiority over SCS in terms of reduced DGF and overall graft survival rates in DCD [11] and extended criteria donor (ECD) kidneys [12]. The addition of oxygen to these circuits in the experimental setting improves ATP synthesis and reduces the oxidative stress associated with IRI [13]. A study by Koetting et al. reported a significant improvement in renal function following oxygenated perfusion [14]. A randomised controlled trial (RCT) comparing oxygenated versus non-oxygenated perfusion did not demonstrate a significant difference in post-transplant graft function but did show a reduction in acute rejection, suggesting an immunoprotective effect [15]. A further trial by the same group comparing short-term hypothermic machine perfusion (HMP) following SCS against SCS alone was unable to show benefit in either function or graft survival [16].
From these preservation methods, NMP has emerged to utilise the beneficial effects of machine perfusion whilst negating the drawbacks with cold ischaemia. The ability to circulate a warm oxygenated perfusate through an organ to support rather than suppress cellular function could be critical for both reconditioning and viability assessment (Fig. 1).
Normothermic machine perfusion (NMP) involves the circulation of a red cell-based solution through the kidney at a near-normal body temperature and pressure. Oxygen, glucose and nutrients are provided to support aerobic metabolism. Renal function is restored to minimise ischaemic injury, and cell survival and repair mechanisms are upregulated to aid repair. NMP also provides the opportunity to assess the quality of a kidney
Experimental Studies
Early porcine models utilising an end-period of normothermic perfusion with oxygenated blood showed improved renal tubular function and increased ATP levels and displayed improved haemodynamic characteristics compared with SCS [17]. Protective heat shock protein 70 (HSP-70), critical for cell survival and repair, was also found to be upregulated during NMP [18].
In a porcine model of DCD transplantation, NMP was superior to SCS with regard to renal function and markers of renal injury such as serum neutrophil gelatinase-associated lipocalin (NGAL) [19]. NMP protocols have also been shown through transcriptional analysis of gene expression to upregulate pathways controlling cell survival, proliferation and protective stress responses [20]. It is important to consider that an environment that causes the upregulation of protective factors may also lead to the upregulation of unwanted detrimental inflammatory pathways.
Clinical Studies
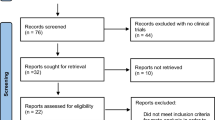
The first case of human renal transplantation following NMP was described in 2011, where one of a pair of DCD donor kidneys was allotransplanted successfully into a 55-year-old female with adult polycystic kidney disease [21•]. This demonstrated the feasibility of the technique and incidentally was associated with improved function compared to the control. Following on from this, a clinical trial of 18 ECD kidneys perfused for 1 h and subsequently transplanted was able to show a significant reduction in DGF [22]. The culmination of this work was a RCT designed to compare pre-implantation NMP versus SCS in DCD kidneys, with results due in 2022 [23].
A Canadian study by Mazilescu et al. presented 13 kidneys from deceased donors placed on NMP compared against historic controls perfused with anoxic HMP [24]. This study showed a reduced rate of DGF in the experimental group (p = 0.51) but ultimately recorded no differences in a 1-year outcome. The study confirmed the feasibility of NMP but was unable to define how best it should be used. This trend has been replicated in further clinical studies in the UK [25] and the Netherlands [26].
NMP vs Hypothermic Preservation
There is some experimental data that suggests a benefit with the use of NMP compared with HMP [27]. However, more recent porcine experimental models [28, 29] have shown HMP to be at least equivocal or superior in terms of physiological and histological outcomes. The Cochrane review by Tingle et al. [30] concluded a clear benefit found with HMP compared to SCS but there is a paucity of evidence to make any conclusions with regard to equivalence of inferiority with NMP.
To address this, there is a significant drive to further the evidence base of NMP, with further RCTs currently underway. Rijkse et al. [31] are comparing the use of NMP against HMP with a primary outcome of immediate graft function, and Lurje et al. are assessing the benefits of NMP over SCS (NCT05031052).
Optimisation of NMP
The promising results seen with NMP so far are hindered by the variability in the design of existing protocols including the perfusate composition, duration of perfusion and oxygenation. There is currently no consensus on these variables, and the ideal set-up may depend on the context for which the perfusion is indicated, be that reconditioning or viability assessment.
Perfusate Composition
The composition of the fluid used to perfuse the kidney is fundamental and has been primarily red blood cell (RBC) based alongside a number of other constituents in an attempt to replicate the physiological environment. A review by Elliot et al. [32] summarised the components commonly used in clinical practice for NMP and these are shown in Fig. 2.
Constituents required for normothermic machine perfusion: oxygen carrier, anticoagulant, anti-inflammatory agents, nutrients and multivitamins, diuretic, antibiotics, vasodilator and a colloid. (Figure adapted from Elliott et al. [32])
RBCs are used because they have an excellent oxygen-carrying ability, are relatively safe and promote normal endothelial physiological function [33]. However, there are a number of disadvantages associated with their use. There are increased rates of haemolysis in part due to contact with the perfusion equipment, with potentially detrimental effects to the kidney [34]; the deposition of iron within the kidney leads to an acute inflammatory response [35]; and the quality of the RBCs themselves is inversely proportional to the time since they were donated. The use of whole blood is of limited value with NMP due to platelet activation and the immune response of the resident leucocyte population; however, depletion of the leucocyte population has been shown to reduce tubulointerstitial damage [36].
There has been some work on the development of artificial oxygen carriers such as HBOC-201 (Hemopure), which is an effective substitute for RBC-based perfusate in porcine [37] and human models [38]. Brasile et al. [39] was able to successfully use an enriched medium supplemented with bovine haemoglobin to support kidneys and improve renal function compared to controls.
Different base solutions are used in each NMP experimental protocol, having been developed independently within each research group. Hosgood et al. [22] use Ringer’s solution to maintain circulating volume, whereas Kaths et al. [19] incorporate STEEN solution. STEEN solution, which has higher oncotic pressures, was initially developed for lung transplantation and is thought to be able to facilitate longer periods of perfusion. A similar approach was taken by the Oxford Research Group using a 5% albumin solution [40]. A novel approach to recirculate the urine in order to maintain circuit volume and homeostasis has also been proposed, with a particular aim of prolonged perfusion periods of up to 2 days [41•].
The perfusates are often supplemented with a vasodilator, glucose, insulin and steroids to replicate a physiological environment. The disparity between protocols has not been studied in great depth. A recent study by Poole et al. compared four separate perfusate protocols in a prolonged porcine perfusion model and found significant differences in outcomes with regards to injury markers and physiological parameters [42]. Further comparative studies are required to identify the optimal perfusate composition and tailor this to the indication for NMP.
Duration of Perfusion
There is increasing evidence that prolonging the duration of perfusion may allow the kidney to be reconditioned. This would also allow for the potential of this technology to eradicate the need for overnight transplantation. Increasing the duration of perfusion is challenging, with increased risks of both equipment failure, increased resources required to perfuse and the build-up of toxic metabolites.
Kaths et al. compared 1-, 8- and 16-h periods of NMP prior to reperfusion against a control, in an auto-transplantation porcine model [43]. Both of the longer perfusion durations showed better renal function and reduced tubular injury. A study by the same group looking at a DCD model showed NMP at 16 h was superior to both SCS and HMP [44]. In the hope of replicating this in a clinical setting, a study by Alwayn et al. has been approved to perfuse the kidneys up to 1, 3 and 6 h with a primary outcome of glomerular filtration rate at 6 month post-transplantation (NCT04693325).
A systematic review by Fard et al. [45] summarises the current evidence with regards perfusate composition and duration.
Oxygenation
Most protocols for NMP use either pure O2 or carbogen (a mix of 95%O2/5%CO2) to maintain supraphysiological oxygen concentrations of approximately 75 Kilopascals (KPa), well above the normal physiological range, but thought to maintain homeostasis with a metabolically active organ. There is concern, however, that this high concentration of O2 could lead to the production of reactive oxygen species (ROS) and result in further IRI [46]. A study by Adams et al. using a porcine model of NMP indicated that reducing oxygen concentrations did not have a detrimental effect on kidney function or urine output [47]. Further experimental work is required to understand the optimal oxygen concentration in order to assess whether hyperoxia influences IRI.
Temperature
Having discussed both HMP and NMP, there is some evidence to suggest that there is an intermediary ground to be found. One study showed that porcine kidneys perfused at 20 °C had improved urine output and creatinine clearance compared with kidneys perfused with HMP or subjected to SCS [48]. However, this has been contradicted in a study in which NMP (37 °C) was superior with regards to tubular and renal function when compared to perfusion at 32 °C [49].
An interesting consideration is how quickly an organ should be warmed. A recent study by von Horn and Minor (2018) showed improved renal and mitochondrial function of kidneys that were gradually warmed from 8 °C when compared to NMP [50].
Technologies
The equipment used for most NMP studies is often salvaged cardiac bypass technology, and there is a significant need for the development of portable normothermic perfusion devices. Kidney Assist, a Dutch system, is the only commercially available device currently available for NMP; however, it is not portable. It will be used in the APOLLO trial by Rijkse et al. [31] as described above. The OrganOx group, known for their liver system, are currently trialling a new perfusion device with the University of Oxford, which will be utilised in a study looking at increasing perfusion times up to 24 h (ISRCTN13292277).
Viability Assessment
The ability for NMP to perfuse an organ at a near physiological state and the capacity for this to be performed at recipient centres provide a unique opportunity to assess the viability of a kidney prior to transplantation.
A recent study by Husain et al. showed that the kidneys declined at one centre were often accepted at another centre and subsequently transplanted [51]. A significant number of decisions to decline were related to concerns about organ or donor quality. Along with the poor predictive power of pre-transplant modelling based on donor/recipient demographics [52], more objective donor organ assessment is required to assist in predicting a successful transplant.
NMP has already facilitated utilisation of organs that would have otherwise been discarded. A group in Glasgow used NMP to assess two kidneys declined by all other centres due to severe kidney injury caused by rhabdomyolysis. Following NMP assessment, both kidneys were subsequently transplanted with excellent function 2 month post-transplant [53]. The same group also utilised NMP to facilitate a live donor transplantation of a kidney explanted due to renal artery stenosis and repair using arterial reconstruction [54].
An NMP quality assessment score was developed by the Cambridge team using the parameters of renal perfusate flow, overall macroscopic appearance and urine output, with the kidney given a score between 1 and 5; a score of 3 or less is considered safe for transplantation [55]. In this series, the kidneys scoring 3 had a DGF rate of 38% compared to 6% in those scoring 1. The assessment score has also been used to transplant DCD kidneys declined nationally due to poor in situ flushing and donor age [56]. Further studies aim to evaluate additional viability markers and/or techniques for a more systematic and detailed assessment.
Perfusate/Urinary Biomarkers
The assessment of molecules known to be associated with acute tubular injury have been used in numerous studies, which may be pertinent to NMP. NGAL released from the tubular epithelial cells is a marker of graft function following transplantation. Kidney injury molecule-1 [57] (KIM-1) released from the tubular epithelial cells is proportional to the rates of graft loss [58]. NGAL along with endothelin-1, a marker of renal damage, has been correlated with the Nicholson et al. NMP assessment score [59].
A study by Markgraf et al. looked at inulin clearance during NMP as a direct measure of function, which was correlated to both warm ischaemic time and perfusion parameters [60]. This is promising as it may be able to give a direct marker of functionality prior to transplantation.
Flavin mononucleotide (FMN) has also been studied, which during NMP was correlated with transplanted kidneys that developed DGF [59]. Other potential markers include lactate dehydrogenase, lactate, liver-type fatty-acid binding protein and aspartate aminotransferase [61•]. However, there remains no validated marker in larger clinical trials.
Radiological Assessment
The use of non-invasive imaging could be used to assess a kidney whilst it is being perfused. Contrast enhanced ultrasound scanning (CEUS) with a contrast ‘microbubble’ that is not nephrotoxic may be able to provide detailed assessment of kidney microvasculature [62].
Other potential radiological assessments include the use of magnetic resonance imaging [52] and near-infrared spectroscopy, which can measure changes in oxygen consumption and haemoglobin and provide an indirect measure of blood flow [63].
It is vital that any assessment technique be either point-of-care or readily available to the perfusion centre in order to provide near-immediate results to ensure expedient decisions can be made with regards to organ viability.
Therapeutics
NMP is able to provide a unique environment not only to assess but also to treat kidneys. Any given intervention is able to bypass the systemic circulation eliminating any potential harm this may cause. NMP also replicates a near-physiological state of the kidney providing an optimal environment for the drug to act. There are a number of strategic treatments being assessed (Table 1).
Stem Cell Therapy
Mesenchymal stem cells (MSCs) are multipotent cells derived from adipose tissue, bone marrow or umbilical cord and have the ability to differentiate into mesodermal tissues [64]. They have the ability to promote regeneration and reduce inflammation within target tissues, which can be utilised to treat IRI.
A study by Pool et al. of the MSC and normothermic perfusion consortium (MePEP) perfused porcine kidney for 7 h with the introduction of either bone marrow derived or adipose-derived cultured MSCs [65]. They found lower markers of injury (e.g. NGAL) in the treatment group along with an increase in immunomodulatory cytokines. A further cell group, multipotent adult progenitor cells (MAPCs), has also been studied. These are derived from bone marrow and have both anti-inflammatory and immunomodulatory properties. Thompson et al. perfused paired human donor kidneys with MAPCs and found significant reduction in markers of tubular injury [66]. Brasile et al. perfused human kidneys with MSCs for 24 h and found increased ATP synthesis, reduced levels of proinflammatory cytokines, increased levels of growth factors and normalisation of metabolism and the cytoskeleton [67•].
The use of adipose-derived regenerative cells (ADRCs) containing a high proportion of adult MSCs mitigates against IRI [68] and uniquely can be collected as a point-of-care treatment during the transplantation process. They have been shown to differentiate into renal tubular cells [69] and excrete extracellular vesicles which can modify their response to treat IRI [70]. This aligned with NMP as a treatment platform creates a great synergy.
Gene Therapy
These therapies involve the transfer of genetic material to be taken up by the host cell in order to produce a beneficial effect. Small interfering RNA (siRNA) molecules have been used in transplantation with the hope of treating IRI. Yang et al. used a caspase-3 targeted siRNA administered to the kidney prior to NMP and found levels of caspase 3 and apoptosis were significantly reduced after NMP [71].
Biological Therapies
In order to protect the vascular endothelium during transplantation and prevent the series of reactions that promote IRI, biological therapies have been utilised. Brasile et al. used a non-blood-based NMP protocol and a nano-barrier membrane (NB-LVF4) to prevent immunomodulation of the endothelium. This delivered in a canine model which was found to be safe and was able to postpone acute rejection [72].
The receptor CD-47 is upregulated in IRI and has been shown to prevent tubular cell regeneration and proliferation [73]. Safe delivery of an antibody to this receptor was found to reduce IRI in a murine model and was subsequently perfused with porcine kidneys in NMP, with reduction in histological damage and oxidative stress observed [74].
Other Therapies
NMP can be used to treat kidneys poorly flushed in situ by removing micro-thrombi formation. DiRito et al. used a combination of tissue plasminogen factor (tPA) and plasminogen to treat declined human kidneys on NMP. This treatment was shown to clear the microcirculation of the kidney, improve intrarenal resistance and reduce levels of inflammatory cytokines [75]. A further porcine study mimicking a DCD retrieval with significant warm ischaemia used a combination of thrombolytics including Lys-plasminogen, antithrombin-III and alteplase to recondition organs [76]. The treated kidneys showed reduced vascular resistance and provided good function when transplanted.
Discussion
There is ever emerging evidence to suggest that NMP has the potential to expand the donor pool of transplantable organs. More work is required to strengthen the validity of the currently available viability assessment tools, with particular attention to biomarkers and imaging techniques which provide real-time information to facilitate transplantation decision-making. Moreover, the exciting development of new potential therapeutics that are deliverable during NMP will further not just the assessment of organs but also improve and recondition grafts prior to implantation.
The clinical deliverability and implementation of this technology will therefore become the next focus. In addition, the optimal perfusate constituents and conditions are not yet fully elucidated and will require effective collaboration between research groups to achieve clarity in this area.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Johnson RJ, Bradbury LL, Martin K, Neuberger J. Organ donation and transplantation in the UK-the last decade: a report from the UK national transplant registry. Transplantation. 2014;97 Suppl 1(SUPPL.1). https://doi.org/10.1097/01.TP.0000438215.16737.68
Aubert O, Kamar N, Vernerey D, et al. Long term outcomes of transplantation using kidneys from expanded criteria donors: prospective, population based cohort study. BMJ. 2015;16:18. https://doi.org/10.1136/bmj.h3557.
Saidi RF, Elias N, Kawai T, et al. Outcome of kidney transplantation using expanded criteria donors and donation after cardiac death kidneys: realities and costs. Am J Transplant. 2007;7(12):2769–74. https://doi.org/10.1111/j.1600-6143.2007.01993.x.
Hamed MO, Hamed MO, Chen Y, et al. Early graft loss after kidney transplantation: risk factors and consequences. Am J Transplant. 2015;15(6):1632–43. https://doi.org/10.1111/ajt.13162.
Bae C, Henry SD, Guarrera JV. Is extracorporeal hypothermic machine perfusion of the liver better than the “good old icebox”? Curr Opin Organ Transplant. 2012;17(2):137–42. https://doi.org/10.1097/MOT.0B013E328351083D.
Chen Y, Shi J, Xia TC, Xu R, He X, Xia Y. Preservation solutions for kidney transplantation: history, advances and mechanisms. Cell Transplant. 2019;28(12):1472–89. https://doi.org/10.1177/0963689719872699.
Summers DM, Johnson RJ, Hudson A, Collett D, Watson CJ, Bradley JA. Effect of donor age and cold storage time on outcome in recipients of kidneys donated after circulatory death in the UK: a cohort study. Lancet. 2013;381(9868):727–34. https://doi.org/10.1016/S0140-6736(12)61685-7.
Belzer FO, Ashby BS, Gulyassy PF, Powell M. Successful seventeen-hour preservation and transplantation of human-cadaver kidney. N Engl J Med. 1968;278(11):608–10. https://doi.org/10.1056/NEJM196803142781108.
Lindell SL, Compagnon P, Mangino MJ, Southard JH. UW solution for hypothermic machine perfusion of warm ischemic kidneys. Transplantation. 2005;79(10):1358–61. https://doi.org/10.1097/01.TP.0000159143.45022.F6.
Moser MAJ, Ginther N, Luo Y, et al. Early experience with hypothermic machine perfusion of living donor kidneys—a retrospective study. Transpl Int. 2017;30:706–12. https://doi.org/10.1111/tri.12964.
Tingle SJ, Figueiredo RS, Moir JAG, et al. Hypothermic machine perfusion is superior to static cold storage in deceased donor kidney transplantation: a meta-analysis. Clin Transplant. 2020;34(4). https://doi.org/10.1111/CTR.13814
Jiao B, Liu S, Liu H, Cheng D, Cheng Y, Liu Y. Hypothermic machine perfusion reduces delayed graft function and improves one-year graft survival of kidneys from expanded criteria donors: a meta-analysis. PLoS One. 2013;8(12):e81826. https://doi.org/10.1371/journal.pone.0081826.
Jiao B, Liu S, Liu H, Buchs JB, Lazeyras F, Ruttimann R, Nastasi A, Morel P. Oxygenated hypothermic pulsatile perfusion versus cold static storage for kidneys from non-heart-beating donors tested by in-line ATP resynthesis to establish a strategy of preservation. Perfusion. 2011;26(2):159–65. https://doi.org/10.1177/0267659110387184.
Koetting M, Frotscher C, Minor T. Hypothermic reconditioning after cold storage improves postischemic graft function in isolated porcine kidneys. Transpl Int. 2010;23(5):538–42. https://doi.org/10.1111/j.1432-2277.2009.01014.x.
Jochmans I, Brat A, Davies L, et al. Oxygenated versus standard cold perfusion preservation in kidney transplantation (COMPARE): a randomised, double-blind, paired, phase 3 trial. Lancet. 2020;396(10263):1653–62. https://doi.org/10.1016/S0140-6736(20)32411-9.
Husen P, Boffa C, Jochmans I, et al. Oxygenated end-hypothermic machine perfusion in expanded criteria donor kidney transplant: a randomized clinical trial. JAMA Surg. 2021;156(6):517–25. https://doi.org/10.1001/jamasurg.2021.0949.
Bagul A, Hosgood SA, Kaushik M, Kay MD, Waller HL, Nicholson ML. Experimental renal preservation by normothermic resuscitation perfusion with autologous blood. Br J Surg. 2008;95(1):111–8. https://doi.org/10.1002/bjs.5909.
Hosgood SA, Patel M, Nicholson ML. The conditioning effect of ex vivo normothermic perfusion in an experimental kidney model. J Surg Res. 2013;182(1):153–60. https://doi.org/10.1016/j.jss.2012.08.001.
Kaths JM, Echeverri J, Chun YM, et al. Continuous normothermic ex vivo kidney perfusion improves graft function in donation after circulatory death pig kidney transplantation. Transplantation. 2017;101(4):754–63. https://doi.org/10.1097/TP.0000000000001343.
Hameed AM, Lu DB, Patrick E, et al. Brief normothermic machine perfusion rejuvenates discarded human kidneys. Transplantation Direct. 2019;5(11): e502. https://doi.org/10.1097/txd.0000000000000944.
• Hosgood SA, Nicholson ML. First in man renal transplantation after ex vivo normothermic perfusion. Transplantation. 2011;92(7):735–8. https://doi.org/10.1097/TP.0B013E31822D4E04. This is the first application of normothermic perfusion in clinical practice.
Nicholson ML, Hosgood SA. Renal transplantation after ex vivo normothermic perfusion: the first clinical study. Am J Transplant. 2013;13:1093–252. https://doi.org/10.1111/ajt.12179.
Hosgood SA, Saeb-Parsy K, Wilson C, Callaghan C, Collett D, Nicholson ML. Protocol of a randomised controlled, open-label trial of ex vivo normothermic perfusion versus static cold storage in donation after circulatory death renal transplantation. BMJ Open. 2017;7(1):e012237. https://doi.org/10.1136/bmjopen-2016-012237.
Mazilescu LI, Urbanellis P, Kim SJ, et al. Normothermic ex vivo kidney perfusion for human kidney transplantation: first North American results. Transplantation. 2022. https://doi.org/10.1097/TP.0000000000004098.
Chandak P, Phillips BL, Uwechue R, et al. Dissemination of a novel organ perfusion technique: ex vivo normothermic perfusion of deceased donor kidneys. Artif Organs. 2019;43(11):E308–19. https://doi.org/10.1111/AOR.13499.
Rijkse E, de Jonge J, Kimenai HJAN, et al. Safety and feasibility of 2 h of normothermic machine perfusion of donor kidneys in the Eurotransplant Senior Program. BJS Open. 2021;5(1):zraa024: https://doi.org/10.1093/bjsopen/zraa024
Hosgood SA, Barlow AD, Yates PJ, Snoeijs MGJ, van Heurn ELW, Nicholson ML. A pilot study assessing the feasibility of a short period of normothermic preservation in an experimental model of non-heart beating donor kidneys. J Surg Res. 2011;171(1):283–90. https://doi.org/10.1016/J.JSS.2010.01.027.
Vallant N, Wolfhagen N, Sandhu B, et al. A comparison of pulsatile hypothermic and normothermic ex vivo machine perfusion in a porcine kidney model. Transplantation. 2021;105(8):1760–70. https://doi.org/10.1097/TP.0000000000003599.
Blum MF, Liu Q, Soliman B, et al. Comparison of normothermic and hypothermic perfusion in porcine kidneys donated after cardiac death. J Surg Res. 2017;216:35–45. https://doi.org/10.1016/J.JSS.2017.04.008.
Tingle SJ, Figueiredo RS, Moir JA, Goodfellow M, Talbot D, Wilson CH. Machine perfusion preservation versus static cold storage for deceased donor kidney transplantation. Cochrane Database Syst Rev. 2019;3(3):CD011671. https://doi.org/10.1002/14651858.CD011671.pub2.
Rijkse E, Bouari S, Kimenai HJAN, et al. Additional normothermic machine perfusion versus hypothermic machine perfusion in suboptimal donor kidney transplantation: protocol of a randomized, controlled, open-label trial. Int J Surg Protoc. 2021;25(1):227–37. https://doi.org/10.29337/IJSP.165.
Elliott TR, Nicholson ML, Hosgood SA. Normothermic kidney perfusion: an overview of protocols and strategies. Am J Transplant. 2021;21(4):1382–90. https://doi.org/10.1111/AJT.16307.
Venema LH, van Leeuwen LL, Posma RA, et al. Impact of red blood cells on function and metabolism of porcine deceased donor kidneys during normothermic machine perfusion. Transplantation. 2022;106(6):1170–9. https://doi.org/10.1097/TP.0000000000003940.
Mamikonian LS, Mamo LB, Brian Smith P, Koo J, Lodge AJ, Turi JL. Cardiopulmonary bypass is associated with hemolysis and acute kidney injury in neonates, infants and children. Pediatr Crit Care Med. 2014;15(3):111–9. https://doi.org/10.1097/PCC.0000000000000047.
Hod EA. Red blood cell transfusion-induced inflammation: myth or reality. ISBT Sci Ser. 2015;10(Suppl 1):188. https://doi.org/10.1111/VOXS.12108.
Yang B, Hosgood SA, Harper SJF, Nicholson ML. Leucocyte depletion improves renal function in porcine kidney hemoreperfusion through reduction of myeloperoxidase+ cells, caspase-3, IL-1β, and tubular apoptosis1. J Surg Res. 2010;164(2):e315–24. https://doi.org/10.1016/J.JSS.2010.07.044.
Bhattacharjee RN, Patel SVB, Sun Q, et al. Renal protection against ischemia reperfusion injury: hemoglobin-based oxygen carrier-201 versus blood as an oxygen carrier in ex vivo subnormothermic machine perfusion. Transplantation. 2020;104(3):482–9. https://doi.org/10.1097/TP.0000000000002967.
Aburawi MM, Fontan FM, Karimian N, et al. Synthetic hemoglobin-based oxygen carriers are an acceptable alternative for packed red blood cells in normothermic kidney perfusion. Am J Transplant. 2019;19:2814–24. https://doi.org/10.1111/ajt.15375.
Brasile L, Stubenitsky BM, Booster MH, Arenada D, Haisch C, Kootstra G. Hypothermia – a limiting factor in using warm ischemically damaged kidneys. Am J Transplant. 2001;1(4):316–20. https://doi.org/10.1034/j.1600-6143.2001.10405.x.
Weissenbacher A, Lo Faro L, Boubriak O, et al. Twenty-four-hour normothermic perfusion of discarded human kidneys with urine recirculation. Am J Transplant. 2019;19(1):178–92. https://doi.org/10.1111/AJT.14932.
• Weissenbacher A, Messner F, Gasteiger S, Soleiman A, Öfner D, Schneeberger S. Forty-eight hours of normothermic kidney preservation applying urine recirculation. Artif Organs. 2022;00:1–5. https://doi.org/10.1111/aor.14160. This is the longest reported period of normothermic kidney perfusion and uses a novel technique of urine recirculation to maintain normal homeostasis.
Pool MBF, Hamelink TL, van Goor H, van den Heuvel MC, Leuvenink HGD, Moers C. Prolonged ex-vivo normothermic kidney perfusion: the impact of perfusate composition. PLoS One. 2021;16(5):e0251595. https://doi.org/10.1371/journal.pone.0251595.
Kaths JM, Echeverri J, Linares I, et al. Normothermic ex vivo kidney perfusion following static cold storage – brief, intermediate, or prolonged perfusion for optimal renal graft reconditioning? Am J Transplant. 2017;17(10):2580–90. https://doi.org/10.1111/ajt.14294.
Urbanellis P, Hamar M, Kaths JM, et al. Normothermic ex vivo kidney perfusion improves early DCD graft function compared with hypothermic machine perfusion and static cold storage. Transplantation. 2020;104(5):947–55. https://doi.org/10.1097/TP.0000000000003066.
Fard A, Pearson R, Lathan R, Mark PB, Clancy MJ. Perfusate composition and duration of ex-vivo normothermic perfusion in kidney transplantation: a systematic review. Transpl Int. 2022;11(35):10236. https://doi.org/10.3389/ti.2022.10236.
Watson CJE, Kosmoliaptsis V, Randle LV, et al. Normothermic perfusion in the assessment and preservation of declined livers before transplantation: hyperoxia and vasoplegia-important lessons from the first 12 cases. Transplantation. 2017;101(5):1084–98. https://doi.org/10.1097/TP.0000000000001661.
Adams TD, Hosgood SA, Nicholson ML. Physiological effects of altering oxygenation during kidney normothermic machine perfusion. Am J Physiol Renal Physiol. 2019;316:823–9. https://doi.org/10.1152/ajprenal.00178.2018.
Hoyer DP, Gallinat A, Swoboda S, et al. Subnormothermic machine perfusion for preservation of porcine kidneys in a donation after circulatory death model. Transpl Int. 2014;27(10):1097–106. https://doi.org/10.1111/tri.12389.
Adams TD, Patel M, Hosgood SA, Nicholson ML. Lowering perfusate temperature from 37°C to 32°C diminishes function in a porcine model of ex vivo kidney perfusion. Transplant Direct. 2017;3(3):e140. https://doi.org/10.1097/TXD.0000000000000655.
von Horn C, Minor T. Improved approach for normothermic machine perfusion of cold stored kidney grafts. Am J Transl Res. 2018;10(6):1921–9.
Husain SA, King KL, Pastan S, et al. Association between declined offers of deceased donor kidney allograft and outcomes in kidney transplant candidates. JAMA Netw Open. 2019;2(8):e1910312. https://doi.org/10.1001/jamanetworkopen.2019.10312.
Moeckli B, Sun P, Lazeyras F, et al. Evaluation of donor kidneys prior to transplantation: an update of current and emerging methods. Transpl Int. 2019;32(5):459–69. https://doi.org/10.1111/TRI.13430.
Pearson R, Asher J, Jackson A, Mark PB, Shumeyko V, Clancy MJ. Viability assessment and utilization of declined donor kidneys with rhabdomyolysis using ex vivo normothermic perfusion without preimplantation biopsy. Am J Transplant. 2021;21:1317–21. https://doi.org/10.1111/ajt.16329.
Pearson R, Wubetu J, Jackson A, Kingsmore D. Living donor kidney transplant following nephrectomy for renal artery stenosis with arterial reconstruction and viability assessment using ex vivo normothermic perfusion. BMJ Case Reports CP. 2021;14(11):e245273. https://doi.org/10.1136/BCR-2021-245273.
Hosgood SA, Barlow AD, Hunter JP, Nicholson ML. Ex vivo normothermic perfusion for quality assessment of marginal donor kidney transplants. Br J Surg. 2015;102(11):1433–40. https://doi.org/10.1002/BJS.9894.
Hosgood SA, Thompson E, Moore T, Wilson CH, Nicholson ML. Normothermic machine perfusion for the assessment and transplantation of declined human kidneys from donation after circulatory death donors. Br J Surg. 2018;105(4):388–94. https://doi.org/10.1002/bjs.10733.
Cantaluppi V, Dellepiane S, Tamagnone M, et al. Neutrophil gelatinase associated lipocalin is an early and accurate biomarker of graft function and tissue regeneration in kidney transplantation from extended criteria donors. PLoS One. 2015;10(6):e0129279. https://doi.org/10.1371/JOURNAL.PONE.0129279.
van Timmeren MM, Vaidya VS, van Ree RM, et al. High urinary excretion of kidney injury molecule-1 is an independent predictor of graft loss in renal transplant recipients. Transplantation. 2007;84(12):1625–30. https://doi.org/10.1097/01.TP.0000295982.78039.EF.
Hosgood SA, Nicholson ML. An assessment of urinary biomarkers in a series of declined human kidneys measured during ex vivo normothermic kidney perfusion. Transplantation. 2017;101(9):2120–5. https://doi.org/10.1097/TP.0000000000001504.
Markgraf W, Mühle R, Lilienthal J, et al. Inulin clearance during ex vivo normothermic machine perfusion as a marker of renal function. ASAIO J. 2021. https://doi.org/10.1097/MAT.0000000000001624.
• Hamelink TL, Ogurlu B, de Beule J, et al. Renal normothermic machine perfusion: the road toward clinical implementation of a promising pretransplant organ assessment tool. Transplantation. 2022;106(2):268–79. https://doi.org/10.1097/TP.0000000000003817. Comprehensive review detailing different techniques of kidney assessment.
Rafailidis V, Huang DY, Yusuf GT, Sidhu PS. General principles and overview of vascular contrast-enhanced ultrasonography. Ultrasonography. 2020;39(1):22–42. https://doi.org/10.14366/USG.19022.
Ferrari M, Mottola L, Quaresima V. Principles, techniques, and limitations of near infrared spectroscopy. Can J Appl Physiol. 2004;29(4):463–87. https://doi.org/10.1139/h04-031.
Bochon B, Kozubska M, Surygała G, et al. Mesenchymal stem cells—potential applications in kidney diseases. Int J Mol Sci. 2019;20(10):2462. https://doi.org/10.3390/ijms20102462.
Pool MBF, Vos J, Eijken M, et al. Treating ischemically damaged porcine kidneys with human bone marrow- and adipose tissue-derived mesenchymal stromal cells during ex vivo normothermic machine perfusion. Stem Cells Dev. 2020;29(20):1320–30. https://doi.org/10.1089/SCD.2020.0024.
Thompson ER, Bates L, Ibrahim IK, et al. Novel delivery of cellular therapy to reduce ischemia reperfusion injury in kidney transplantation. Am J Transplant. 2021;21(4):1402–14. https://doi.org/10.1111/AJT.16100.
• Brasile L, Henry N, Orlando G, Stubenitsky B. Potentiating renal regeneration using mesenchymal stem cells. Transplantation. 2019;103(2):307–13. https://doi.org/10.1097/TP.0000000000002455. This study is the first to demonstrate signs of regeneration after 24h of perfusion with the administration of a cell based therapy.
Storti G, Favi E, Albanesi F, Kim BS, Cervelli V. Adipose-derived stem/stromal cells in kidney transplantation: status quo and future perspectives. Int J Mol Sci. 2021;22(20):11188. https://doi.org/10.3390/ijms222011188.
Li K, Han Q, Yan X, Liao L, Zhao RC. Not a process of simple vicariousness, the differentiation of human adipose-derived mesenchymal stem cells to renal tubular epithelial cells plays an important role in acute kidney injury repairing. Stem Cells Dev. 2010;19(8):1267–75. https://doi.org/10.1089/scd.2009.0196.
Bruno S, Grange C, Deregibus MC, et al. Mesenchymal stem cell-derived microvesicles protect against acute tubular injury. J Am Soc Nephrol. 2009;20(5):1053–67. https://doi.org/10.1681/ASN.2008070798.
Yang B, Hosgood SA, Nicholson ML. Naked small interfering RNA of caspase-3 in preservation solution and autologous blood perfusate protects isolated ischemic porcine kidneys. Transplantation. 2011;91(5):501–7. https://doi.org/10.1097/TP.0B013E318207949F.
Brasile L, Glowacki P, Castracane J, Stubenitsky BM. Pretransplant kidney-specific treatment to eliminate the need for systemic immunosuppression. Transplantation. 2010;90(12):1294–8. https://doi.org/10.1097/TP.0b013e3181ffba97.
Rogers NM, Zhang ZJ, Wang JJ, Thomson AW, Isenberg JS. CD47 regulates renal tubular epithelial cell self-renewal and proliferation following renal ischemia reperfusion. Kidney Int. 2016;90(2):334–47. https://doi.org/10.1016/J.KINT.2016.03.034.
Hameed AM, Lu DB, Burns H, et al. Pharmacologic targeting of renal ischemia-reperfusion injury using a normothermic machine perfusion platform. Sci Rep. 2020;10(1):1–17. https://doi.org/10.1038/s41598-020-63687-0.
DiRito JR, Hosgood SA, Reschke M, et al. Lysis of cold-storage-induced microvascular obstructions for ex vivo revitalization of marginal human kidneys. Am J Transplant. 2021;21:161–73. https://doi.org/10.1111/ajt.16148.
Olausson ME, Antony D, Travnikova G, et al. Novel ex-vivo thrombolytic reconditioning of kidneys retrieved 4 to 5 hours after circulatory death. Transplantation. 2021. https://doi.org/10.1097/TP.0000000000004037.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Kidney Transplantation
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Norton, W.G., Pearson, R., Devlin, J. et al. Normothermic Machine Perfusion in Renal Transplantation. Curr Transpl Rep 9, 308–317 (2022). https://doi.org/10.1007/s40472-022-00378-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-022-00378-x