Abstract
Aim
Dopamine is one of the major neurotransmitters of the central nervous system. Dopamine is involved in various cerebral and peripheral physiological functions and pathological conditions. The aim of this mini review is to overview the dopamine, PET radiotracers of dopaminergic system and their clinical applications.
Methods
Dopamine synthesis, dopamine receptors, role of dopamine in physiological functions and diseases, PET radiotracers of dopaminergic system and their clinical applications were reviewed.
Results
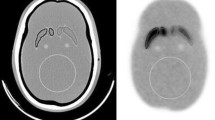
There is a large number of PET radiotracers to assess various elements of dopaminergic system such as F-18 fluorodopamine to assess dopamine transfer and storage in peripheral catecholamine-synthesizing cells, F-18 FDOPA to assess L-DOPA transfer via l-amino acid transporters, conversion of L-DOPA to dopamine by aromatic l-amino acid decarboxylase and storage of dopamine at vesicles, C-11 methylphenidat, C-11 dihydrotetrabenazine, and C-11 deprenyl to assess dopamine transport via dopamine transporters, dopamine transport into vesicles by vesicular monoamine transporter-2, and dopamine degredation by monoamine oxidase, respectively, in presynaptic dopaminergic nerve terminals in the brain and in certain peripheral cells and C-11 raclopride and C-11 SCH 23,390 to assess dopamine receptors at postsynaptic nerve terminals. Among these radiotracers, only F-18 FDOPA is widely and commercially available. The other radiotracers are available in limited centers, mainly for research purpose. Dopaminergic PET radiotracers help to detect or diagnose various diseases such as parkinsonian syndromes, huntington’s disease, dementias, schizophrenia, drug addictions, paragangliomas, pheochromocytoma, medullary thyroid carcinoma, gut carcinoids, gliomas and hyperinsulinemic hypoglycemia.
Conclusion
There is a large number of dopaminergic PET radiotracers which help to detect or diagnose diseases of the various systems in which dopaminergic system is involved.






Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Beaulieu JM, Espinoza S, Gainetdinov RR (2015) Dopamine receptors - IUPHAR Review 13. Br J Pharmacol 172:1–23
Vallone D, Picetti R, Borrelli E (2000) Structure and function of dopamine receptors. Neurosci Biobehav Rev 24:125–132
Franco R, Reyes-Resina I, Navarro G (2021) Dopamine in Health and Disease: much more than a neurotransmitter. Biomedicines 9:109
Chinta SJ, Andersen JK (2005) Dopaminergic neurons. Int J Biochem Cell Biol 37:942–946
Grant CE, Flis AL, Ryan BM (2022) Understanding the role of dopamine in cancer: past, present and future. Carcinogenesis 43:517–527
Kilbourn MR (2021) 11C- and 18F-Radiotracers for in vivo imaging of the dopamine system: past. Present Future Biomedicines 9:108. https://doi.org/10.3390/biomedicines9020108
Sarikaya I (2022) Biology of Cancer and PET Imaging: Pictorial Review. J Nucl Med Technol 50:81–89
Minn H, Kauhanen S, Seppänen M et al (2009) 18F-FDOPA: a multiple-target molecule. J Nucl Med 50:1915–1918
Morbelli S, Esposito G, Arbizu J et al (2020) EANM practice guideline/SNMMI procedure standard for dopaminergic imaging in parkinsonian syndromes 1.0. Eur J Nucl Med Mol Imaging 47:1885–1912
Taïeb D, Hicks RJ, Hindié E et al (2019) European Association of Nuclear Medicine Practice Guideline/Society of Nuclear Medicine and Molecular Imaging Procedure Standard 2019 for radionuclide imaging of phaeochromocytoma and paraganglioma. Eur J Nucl Med Mol Imaging 46:2112–2137
Giovanella L, Treglia G, Iakovou I et al (2020) EANM practice guideline for PET/CT imaging in medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging 47:61–77
Law I, Albert NL, Arbizu J et al (2019) Joint EANM/EANO/RANO practice guidelines/SNMMI procedure standards for imaging of gliomas using PET with radiolabelled amino acids and [18F]FDG: version 1.0. Eur J Nucl Med Mol Imaging 46:540–557
Vernaleken I, Kumakura Y, Cumming P et al (2006) Modulation of [18F]fluorodopa (FDOPA) kinetics in the brain of healthy volunteers after acute haloperidol challenge. NeuroImage 30:1332–1339
Garnett S, Firnau G, Nahmias C et al (1983) Striatal dopamine metabolism in living monkeys examined by positron emission tomography. Brain Res 280:169–171
Chondrogiannis S, Marzola MC, Al-Nahhas A, Venkatanarayana TD, Mazza A, Opocher G, Rubello D (2013) Normal biodistribution pattern and physiologic variants of 18F-DOPA PET imaging. Nucl Med Commun 34:1141–1149
Sarikaya I (2015) PET imaging in neurology: Alzheimer’s and Parkinson’s diseases. Nucl Med Commun 36:775–781
Carvey PM, Punati A, Newman MB (2006) Progressive dopamine neuron loss in Parkinson’s disease: the multiple hit hypothesis. Cell Transpl 15:239–250
Blesa J, Trigo-Damas I, Dileone M et al (2017) Compensatory mechanisms in Parkinson’s disease: circuits adaptations and role in disease modification. Exp Neurol 298:148–161
Ishiwata K, Kimura Y, Oda K et al (2010) Development of PET radiopharmaceuticals and their clinical applications at the Positron Medical Center. Geriatr Gerontol Int 10(Suppl 1):S180–S196
Dentresangle C, Veyre L, le Bars Pierre C et al (1999) Striatal D2 dopamine receptor status in Parkinson’s disease: an 18F DOPA and 11 C-raclopride PET study. Mov Disord 14:1025–1030
Turjanski N, Lees AJ, Brooks DJ (1997) In vivo studies on striatal dopamine D1 and D2 site binding in L-DOPA treated Parkinson’s disease patients with and without dyskinesias. Neurology 49:717–723
Antonini A, Schwarz J, Oertel WH et al (1997) Long-term changes of striatal dopamine D2 receptors in patients with Parkinson’s disease: a study with positron emission tomography and [11 C]raclopride. Mov Disord 12:33–38
Brooks DJ, Ibanez V, Sawle GV et al (1990) Differing patterns of striatal 18F-dopa uptake in Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy. Ann Neurol 28:547–555
Oh M, Lee N, Kim C et al (2021) Diagnostic accuracy of dual-phase 18F-FP-CIT PET imaging for detection and differential diagnosis of parkinsonism. Sci Rep 11:14992. https://doi.org/10.1038/s41598-021-94040-8
Van Laere K, Clerinx K, D’Hondt E, de Groot T et al (2010) Combined striatal binding and cerebral influx analysis of dynamic 11 C-raclopride PET improves early differentiation between multiple-system atrophy and Parkinson disease. J Nucl Med 51:588–595
la Fougère C, Pöpperl G, Levin J et al (2010) The value of the dopamine D2/3 receptor ligand 18F-desmethoxyfallypride for the differentiation of idiopathic and nonidiopathic parkinsonian syndromes. J Nucl Med 51:581–587
Criswell SR, Perlmutter JS, Videen TO et al (2011) Reduced uptake of [18F]FDOPA PET in asymptomatic welders with occupational manganese exposure. Neurology 76:1296–1301
Sarikaya I, Apaydin H, Topal U, Karaoglan O (2006) Cyanide-induced parkinsonism and F-18 FDG PET/CT findings. Clin Nucl Med 31:363–364
Wallert E, Letort E, van der Zant F et al (2022) Comparison of [18F]-FDOPA PET and [123I]-FP-CIT SPECT acquired in clinical practice for assessing nigrostriatal degeneration in patients with a clinically uncertain parkinsonian syndrome. EJNMMI Res 12:68
Eshuis SA, Jager PL, Maguire RP, Jonkman S, Dierckx RA, Leenders KL (2009) Direct comparison of FP-CIT SPECT and F-DOPA PET in patients with Parkinson’s disease and healthy controls. Eur J Nucl Med Mol Imaging 36:454–462
Sood A, Shukla J, Shree R, Vatsa R, Modi M, Mittal BR (2021) Comparative performance of 99mTc-TRODAT-1 SPECT/CT and 18F-FDOPA PET/CT imaging in patients with Parkinson’s Disease, Parkinson-Plus Syndrome, and essential tremor. Clin Nucl Med 46:95–102
Kerstens VS, Varrone A (2020) Dopamine transporter imaging in neurodegenerative movement disorders: PET vs. SPECT. Clin Transl Imaging 8:349–356
Jakobson Mo S, Axelsson J, Jonasson L et al (2018) Dopamine transporter imaging with [18F]FE-PE2I PET and [123I]FP-CIT SPECT-a clinical comparison. EJNMMI Res 8:100. https://doi.org/10.1186/s13550-018-0450-0
Lee I, Kim JS, Park JY et al (2018) Head-to-head comparison of 18 F-FP-CIT and 123 I-FP-CIT for dopamine transporter imaging in patients with Parkinson’s disease: a preliminary study. Synapse 72:e22032. https://doi.org/10.1002/syn.22032
Li C, Chen M, Zhao X et al (2017) Chemical Exchange Saturation transfer MRI Signal loss of the Substantia Nigra as an imaging biomarker to evaluate the diagnosis and severity of Parkinson’s Disease. Front Neurosci 11:489
Shang S, Li D, Tian Y, Li R et al (2021) Hybrid PET-MRI for early detection of dopaminergic dysfunction and microstructural degradation involved in Parkinson’s disease. Commun Biol 4:1162
Chen S, Leung YM, Yeung KMA et al (2016) Comparative study of 18F-DOPA PET/MR and PET/CT in quantification accuracy and clinical applicability for Parkinson’s disease: A static and dynamic data analysis. Journal of Nuclear Medicine 57 (supplement 2) 1830
Arabi H, AkhavanAllaf A, Sanaat A, Shiri I, Zaidi H (2021) The promise of artificial intelligence and deep learning in PET and SPECT imaging. Phys Med 83:122–137
Boyle AJ, Gaudet VC, Black SE, Vasdev N, Rosa-Neto P, Zukotynski KA (2021) Artificial intelligence for molecular neuroimaging. Ann Transl Med 9:822
Palumbo B, Bianconi F, Nuvoli S et al (2021) Artificial intelligence techniques support nuclear medicine modalities to improve the diagnosis of Parkinson’s disease and parkinsonian syndromes. Clin Transl Imaging 9:19–35
Glaab E, Trezzi JP, Greuel A et al (2019) Integrative analysis of blood metabolomics and PET brain neuroimaging data for Parkinson’s disease. Neurobiol Dis 124:555–562
Choi H, Ha S, Im HJ et al (2017) Refining diagnosis of Parkinson’s disease with deep learning-based interpretation of dopamine transporter imaging. Neuroimage Clin 16:586–594
Wang J, Xue L, Jiang J et al (2024) Diagnostic performance of artificial intelligence-assisted PET imaging for Parkinson’s disease: a systematic review and meta-analysis. npj Digit med 7:17
Hwang D, Kim KY, Kang SK, Seo S et al (2018) Improving the Accuracy of simultaneously reconstructed activity and attenuation maps using deep learning. J Nucl Med 59:1624–1629
Sarikaya I, Sarikaya A, Elgazzar AH (2018) Current status of 18F-FDG PET brain imaging in patients with dementia. J Nucl Med Technol 46:362–367
McKeith I, O’Brien J, Walker Z et al (2007) Sensitivity and specificity of dopamine transporter imaging with 123I-FP-CIT SPECT in dementia with Lewy bodies: a phase III, multicentre study. Lancet Neurol 6:305–313
Thomas AJ, Attems J, Colloby SJ et al (2017) Autopsy validation of 123I-FP-CIT dopaminergic neuroimaging for the diagnosis of DLB. Neurology 88:276–283
Klein JC, Eggers C, Kalbe E et al (2010) Neurotransmitter changes in dementia with Lewy bodies and Parkinson disease dementia in vivo. Neurology 74:885–892
Xiasheng H, Xiaoyan Z, Hu Po (2002) 18F-DOPA PET imaging in the diagnosis of dementia with Lewy bodies. Chin J Nuclear Med 22:143–145
Lee YG, Jeon S, Baik K et al (2023) Substantia Nigral dopamine transporter uptake in dementia with Lewy bodies. NPJ Parkinsons Dis 9:88. https://doi.org/10.1038/s41531-023-00534-9
Rinne JO, Laine M, Kaasinen V et al (2002) Striatal dopamine transporter and extrapyramidal symptoms in frontotemporal dementia. Neurology 58:1489–1493
Schöll M, Carter SF, Westman E et al (2015) Early astrocytosis in autosomal dominant Alzheimer’s disease measured in vivo by multi-tracer positron emission tomography. Sci Rep 5:16404
Cybulska K, Perk L, Booij J, Laverman P, Rijpkema M (2020) Huntington’s disease: a review of the known PET imaging biomarkers and targeting Radiotracers. Molecules 25:482
Turjanski N, Weeks R, Dolan R et al (1995) Striatal D1 and D2 receptor binding in patients with Huntington’s disease and other choreas. A PET study. Brain. 1995;118:689–96
Sedvall G, Karlsson P, Lundin A et al (1994) Dopamine D1 receptor number—asensitive PET marker for early brain degeneration in Huntington’s disease. Eur Arch Psychiatry Clin Neurosci 243:249–255
Andrews TC, Weeks RA, Turjanski N et al (1999) Huntington’s disease progression. PET and clinical observations. Brain 122:2353–2363
Pavese N, Andrews TC, Brooks DJ et al (2003) Progressive striatal and cortical dopamine receptor dysfunction in Huntington’s disease: a PET study. Brain 126:1127–1135
Ginovart N, Lundin A, Farde L et al (1997) PET study of the pre- and post-synaptic dopaminergic markers for the neurodegenerative process in Huntington’s disease. Brain 120:503–514
Everix L, Staelens S, Bertoglio D (2023) Positron Emission Tomography (PET) imaging biomarkers in Huntington’s Disease. In: Thomas EA, Parkin GM (eds) Biomarkers for Huntington’s Disease. Contemporary clinical neuroscience. Springer, Cham. https://doi.org/10.1007/978-3-031-32815-2_6
Pagano G, Niccolini F, Politis M (2016) Current status of PET imaging in Huntington’s disease. Eur J Nucl Med Mol Imaging 43:1171–1182
Fusar-Poli P, Meyer-Lindenberg A (2013) Striatal presynaptic dopamine in schizophrenia, part I: meta-analysis of dopamine active transporter (DAT) density. Schizophr Bull 39:22–32
Fusar-Poli P, Meyer-Lindenberg A (2013) Striatal presynaptic dopamine in schizophrenia, part II: meta-analysis of [(18)F/(11)C]-DOPA PET studies. Schizophr Bull 39:33–42
Plavén-Sigray P, Ikonen Victorsson P, Santillo A et al (2022) Thalamic dopamine D2-receptor availability in schizophrenia: a study on antipsychotic-naive patients with first-episode psychosis and a meta-analysis. Mol Psychiatry 27:1233–1240
Agid O, Mamo D, Ginovart N et al (2007) Striatal vs extrastriatal dopamine D2 receptors in antipsychotic Response—A double-blind PET study in Schizophrenia. Neuropsychopharmacol 32:1209–1215
Abi-Dargham A, Gil R, Krystal J et al (1998) Increased striatal dopamine transmission in schizophrenia: confirmation in a second cohort. Am J Psychiatry 155:761–767
Weinstein JJ, van de Giessen E, Rosengard RJ et al (2018) PET imaging of dopamine-D2 receptor internalization in schizophrenia. Mol Psychiatry 23:1506–1511
Okubo Y, Suhara T, Suzuki K et al (1997) Decreased prefrontal dopamine D1 receptors in schizophrenia revealed by PET. Nature 385:634–636
Wu JC, Bell K, Najafi A et al (1997) Decreasing striatal 6-FDOPA uptake with increasing duration of cocaine withdrawal. Neuropsychopharmacology 17:402–409
Heinz A, Siessmeier T, Wrase J et al (2005) Correlation of alcohol craving with striatal dopamine synthesis capacity and D2/3 receptor availability: a combined [18F]DOPA and [18F]DMFP PET study in detoxified alcoholic patients. Am J Psychiatry 1515–1520
McCann UD, Wong DF, Yokoi F et al (1998) Reduced striatal dopamine transporter density in abstinent methamphetamine and methcathinone users: evidence from positron emission tomography studies with [11 C]WIN-35,428. J Neurosci 18:8417–8422
Sekine Y, Iyo M, Ouchi Y et al (2001) Methamphetamine-related psychiatric symptoms and reduced brain dopamine transporters studied with PET. Am J Psychiatry 158:1206–1214
Shi J, Zhao LY, Copersino ML et al (2008) PET imaging of dopamine transporter and drug craving during methadone maintenance treatment and after prolonged abstinence in heroin users. Eur J Pharmacol 579:160–166
Wang GJ, Volkow ND, Fowler JS et al (1997) Dopamine D2 receptor availability in opiate-dependent subjects before and after naloxone-precipitated withdrawal. Neuropsychopharmacology 16:174–182
Fehr C, Yakushev I, Hohmann N et al (2008) Association of low striatal dopamine d2 receptor availability with nicotine dependence similar to that seen with other drugs of abuse. Am J Psychiatry 165:507–514
Dagher A, Bleicher C, Aston JA et al (2001) Reduced dopamine D1 receptor binding in the ventral striatum of cigarette smokers. Synapse 42:48–53
Volkow ND, Fowler JS, Gatley SJ et al (1996) PET evaluation of the dopamine system of the human brain. J Nucl Med 37:1242–1256
Carrasquillo JA, Chen CC, Jha A et al (2021) Imaging of Pheochromocytoma and Paraganglioma. J Nucl Med. 2021;62:1033–1042
Treglia G, Cocciolillo F, de Waure C et al (2012) Diagnostic performance of 18F-dihydroxyphenylalanine positron emission tomography in patients with paraganglioma: a meta-analysis. Eur J Nucl Med Mol Imaging 39:1144–1153
Piccardo A, Morana G, Puntoni M et al (2020) Diagnosis, treatment response, and prognosis: the role of 18F-DOPA PET/CT in children affected by Neuroblastoma in comparison with 123I-mIBG scan: the first prospective study. J Nucl Med 61:367–374
PiccardoA, Lopci E, Conte M et al (2012) Comparison of 18F-dopa PET/CT and 123I MIBG scintigraphy in stage 3 and 4 neuroblastoma: a pilot study. Eur J Nucl Med Mol Imaging 39:57–71
Kim Yong-il, Lee DY, Kim D-H et al (2019) Diagnostic Value of Early F-18-FDOPA PET-CT for Initial Staging of Neuroblastoma: A Comparison Study with Delay F-18-FDOPA PET-CT and I-123-MIBG Scintigraphy/SPECT-CT Journal of Nuclear Medicine 60 (supplement 1):157
Schiepers C, Chen W, Cloughesy T et al (2007) 18F-FDOPA kinetics in brain tumors. J Nucl Med 48:1651–1661
Somme F, Bender L, Namer IJ et al (2020) Usefulness of 18F-FDOPA PET for the management of primary brain tumors: a systematic review of the literature. Cancer Imaging 20:70. https://doi.org/10.1186/s40644-020-00348-5
Evangelista L, Cuppari L, Bellu L et al (2019) Comparison between 18F-Dopa and 18F-Fet PET/CT in patients with suspicious recurrent high Grade Glioma: A literature review and our experience. Curr Radiopharm 12:220–228
Xiao J, Jin Y, Nie J et al (2019) Diagnostic and grading accuracy of 18F-FDOPA PET and PET/CT in patients with gliomas: a systematic review and meta-analysis. BMC Cancer 19:767
Herrmann K, Czernin J, Cloughesy T et al (2014) Comparison of visual and semiquantitative analysis of 18F-FDOPA-PET/CT for recurrence detection in glioblastoma patients. Neuro-Oncol 16:603–609
Hoegerle S, Altehoefer C, Ghanem N et al (2001) 18F-DOPA positron emission tomography for tumour detection in patients with medullary thyroid carcinoma and elevated calcitonin levels. Eur J Nucl Med 28:64–71
Golubić AT, Pasini Nemir E, Žuvić M et al (2017) The value of 18F-DOPA PET/CT in patients with medullary thyroid carcinoma and increased calcitonin values. Nucl Med Commun 38:636–641
Soussan M, Nataf V, Kerrou K et al (2012) Added value of early 18F-FDOPAPET/CT acquisition time in medullary thyroid cancer. Nucl Med Commun 33:775–779
Kjærulff MLG, Dias AH, Iversen P et al (2022) Early acquisition of [18F]FDOPA PET/CT imaging in patients with recurrent or residual medullary thyroid cancer is safe—and slightly better! Eur J Hybrid Imaging 6:20
Schillaci O (2014) 18F-DOPA and other radiopharmaceuticals for imaging unknown primary neuroendocrine tumors. J Nucl Med 55:357–359
States LJ, Davis JC, Hamel SM et al (2021) 18F-6-Fluoro-l-Dopa PET/CT Imaging of Congenital Hyperinsulinism. J Nucl Med 62(Suppl 2):51S–56S
Imperiale A, Sebag F, Vix M et al (2015) 18F-FDOPA PET/CT imaging of insulinoma revisited. Eur J Nucl Med Mol Imaging 42:409–418
Leroy-Freschini B, Amodru V, Addeo P et al (2019) Early 18F-FDOPA PET/CT imaging after carbidopa premedication as a valuable diagnostic option in patients with insulinoma. Eur J Nucl Med Mol Imaging 46:686–695
Author information
Authors and Affiliations
Contributions
Dr Sarikaya wrote the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.