Abstract
Introduction
Although a number of pathophysiological aspects of childhood obesity have been reported, few information are available on obesity-related cardiac organ damage.
Aim
The present study was aimed at assessing the impact of anthropometric, blood pressure (BP) and metabolic variable on cardiac structure and function in youth.
Methods
In 78 subjects aged 5–16 years attending the outpatient clinic of cardiovascular risk (Valencia, Spain) anthropometric and metabolic variables, clinic and ambulatory BP and echocardiographic parameters were assessed. Subjects were also classified according to the presence of insulin resistance.
Results
Subjects mean age (± SD) amounted to 12.03 ± 2.4 years and males to 53.8%. Ten subjects were normoweight, 11 overweight, 39 obese, and 18 severely obese. No significant difference in office and ambulatory BP was detected among different bodyweight groups. A significant direct correlation was observed between left ventricular mass index (LVMI) and obesity markers [body mass index (BMI): r = 0.38, waist circumference (WC): r = 0.46, P < 0.04 for both]. Left ventricular hypertrophy, relative wall thickness and left atrial diameter were significantly related to BMI and WC. In contrast, office and ambulatory BP were unrelated to other variables, and differences in LVMI among different BP phenotypes were not significant. When partitioning the population by insulin resistance, LVMI, adjusted for confounders, was significantly greater in the insulin-resistant group.
Conclusions
In children and adolescents characterized by different body weight patterns, weight factors “per se” and the related insulin resistance state appear to represent the main determinants of LVMI and left ventricular hypertrophy, independently on BP values and BP phenotypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
A number of clinical studies have shown that in the adult population obesity is associated with profound cardiac structural alterations, the one most frequently detected being a pathological increase in left ventricular mass, frequently leading to the occurrence of left ventricular hypertrophy [1,2,3]. Evidence has been also provided that in the adult obese subjects hemodynamic, neurohumoral and anthropometric factors participate independently at the development and progression of the above mentioned cardiac structural changes [4,5,6].
Whether and to what extent the information collected in the overweight and obese adults are also shared by subjects in the pediatric age has been investigated in few studies, with the seminal information collected in the frame of the Bogalusa Heart Study [7]. Subsequent studies have attempted to clarify the relationships between left ventricular mass index (LVMI) and the obese state in patients in the pediatric age [8, 9]. However, the relative contribution of hemodynamic vs non-hemodynamic factors at the development of the above mentioned association remains at present unsettled, due to heterogeneity of the populations examined as well as to the presence of confounding factors [10]. A prospective/retrospective study very recently suggested the importance of body weight as determinant of left ventricular mass in a cohort of children [11].
The present study has been undertaken to determine the association of an overweight and an obese state with cardiac structural alterations and occurrence of left ventricular hypertrophy (LVH) in a group of children and adolescents. An additional aim was represented by the determination of the mechanistic role of ambulatory BP phenotypes versus anthropometric and metabolic factors, and specifically of the insulin resistance state frequently characterizing childhood obesity, in the development and progression of the cardiac organ damage in overweight and obese children and adolescents.
2 Methods
2.1 Population
White youths with normoweight, overweight or obesity of both sexes aged between 5 to 16 years were included in the study. They were recruited from those attending the outpatient clinic for cardiometabolic risk assessment at the Cardiovascular Risk Unit of the Hospital General of the University of Valencia, Spain. Concomitant disease were excluded by physical and instrumental examination, blood chemistry and urine analysis. Patients with secondary causes of hypertension and/or acute diseases were excluded from the sample. Obesity was diagnosed when body mass index (BMI) exceeded the 95th percentile for age and sex, and the extent of obesity was quantified using the least mean square method of Cole et al. [12]. An overweight state was defined in subjects with a BMI ranging from the 85th to 95th percentile of the BMI distribution in a normal age-matched reference population. Informed written consent was obtained from parents and participants before testing. The study protocol was reviewed and approved by the Ethics Committee of the General Hospital, University of Valencia and all the procedures of the investigation have been performed according to good clinical practice and to the Declaration of Helsinki. All participants provided written consent after being informed of the study nature and purpose.
2.2 Measurements
Anthropometric variables Body weight was recorded to the nearest 0.1 kg using a standard beam balance scale with the subjects wearing light indoor clothing and no shoes. Height was recorded to the nearest 0.5 cm using a standardized wall-mounted height board. Weight and body mass composition were evaluated with bioelectrical impedance analysis, using a Tanita TBF 410M over a horizontal and hard surface and to the nearest 0.1 kg, with the subject wearing light clothing and without shoes. BMI was calculated as weight (in kilograms) divided by height (in square meters) and patients were stratified on their obesity status according to both z-scores following World Health Organization (WHO) growth charts and Centers for Disease Control (CDC) percentiles [13]. According to WHO classification subjects with z-score between 1 and 2 were defined as overweight, subjects with z-scores between 2 and 3 were defined as obese and subjects with z-score > 3 were defined as severe obese [14]. According to CDC subjects were defined as overweight with BMI above 85th percentile for age and sex, obese with BMI above 95th percentile and further classified as class 1 obesity, i.e. BMI ≥ 95th percentile to < 120% of 95th percentile, class 2, i.e. BMI ≥ 25 kg/m2 120% to < 140% of 95th percentile or BMI ≥ 35 kg/m2 and class 3, i.e. BMI ≥ 140% of 95th percentile or BMI ≥ 40 kg/m2. Waist circumference (WC) was assessed in standing position at the end of expiration midpoint between the lowest margin last palpable ribs and top of iliac crest. Hip circumference was measured around the widest point of buttocks. Waist-to-hip ratio and waist-to-height ratio were consequently calculated.
Clinic BP measurements On the day of the study, trained clinical nurses measured sphygmomanometric office BP values of each subject three times consecutively in seated position, at 5 min intervals, using a mercury sphygmomanometer. This was done on the non-dominant arm, with a cuff and a bladder size adjusted to upper arm girth. Office systolic and diastolic BP values were taken as the average of 3 measurements. Office BP had to be at least 95th percentile of the BP distribution on at least 3 separate occasions to be considered as suggestive of a hypertensive state [15]. Using office BP, subjects were defined as normotensive when both systolic and diastolic BP were less than 90th percentile, age, sex, and height-specific. According to the 2016 European Society Hypertension (ESH) guidelines on pediatric hypertension, subjects were identified as hypertensive in presence of BP values above the 95th percentile for age and sex and normal-high pressure was defined ad BP between the 90th and 95th percentile [16, 17]. The hypertensive state was further classified, accordingly to its clinical severity, into grade 1 (95th percentile to the 99th percentile and 5 mmHg) and grade 2 (over 99th percentile plus 5 mmHg).
Ambulatory BP measurements Ambulatory BP recordings were obtained in daily life conditions over the 24 h period the day after office BP assessment. Recordings were initiated on regular school days between 08.30 a.m. and 09.00 a.m. On monitoring days, the participants did not engage in vigorous exercise. Cuff and bladder size were adjusted as for office BP. The oscillometric SpaceLabs 90207 and 90217 monitors (SpaceLabs Inc., Redmond, Washington, USA) were programmed to obtain BP readings at 20 min intervals from 06.00 am until 12.00 p.m. and at 30 min intervals from 12.00 p.m. until 06.00 am. Daytime was defined as the interval ranging from 10.00 a.m. to 08.00 p.m. and nighttime from 12.00 p.m. to 06.00 a.m. Measurements were automatically repeated when readings were outside the ranges of 70-220 mmHg systolic or 40-140 mmHg diastolic. Only recordings with more than 80% of successful measurements, defined as the percentage of valid measurements, were taken into account in the analysis. The averages of the valid readings for the whole 24 h period, the daytime and the nighttime subperiods, respectively, were calculated.
Subjects were further stratified on the basis of joint clinic and ambulatory blood pressure into different phenotypes: normotensive (normal clinic and ambulatory BP values), sustained hypertensive (both clinic and ambulatory BP values over the 95th percentile), white coat hypertensive (elevated office with normal ambulatory BP values) and masked hypertensive (normal office with elevated ambulatory BP values). According to the night-day pattern of the ambulatory BP monitoring we identified dippers, i.e. subjects in which mean systolic/diastolic night-time BP decreases at least 10%, and non-dippers, i.e. those in which the BP reduction night-time versus day-time is < 10% [16, 17].
Echocardiographic parameters All subjects underwent 2-dimensional and M-mode echocardiography. Loops of minimum 3 cycles were recorded and all measurements were taken 3 times, considering the average of the three values. The measurements were performed in standard positions and parasternal long axis (PLAX) and short axis views, apical 4 chambers, apical 2 chambers, apical 3 chambers were assessed. We determined in all subjects left ventricular end diastolic dimension, left ventricular end systolic dimension, end diastolic interventricular septum and posterior wall thickness, left atrial diameter in M-mode in PLAX. Major cardiac abnormalities were excluded. Left ventricular mass was assessed with M-mode measurements with Devereux formulae and LVMI was calculated with respect to height elevated to 2.7 [18]. LVH was defined as LVMI above the 95th percentile for age and sex as recommended by ESH guidelines [16]. Relative wall thickness (RWT) was calculated as (IVSd + LVPWd)/LVIDd. Concentric remodelling was defined as RWT above the accepted juvenile cut-off amounting to 0.38. Diastolic function was also assessed according to methods recommended by 2010 American Society of Echocardiography guidelines [19]. Pulsed-wave doppler analysis of mitral valve inflow velocities was measured in 4-C view by peak early diastolic velocity (E wave) and peak velocity during atrial contraction (A wave) and E/A ratio was calculated. E′ velocity was assessed by tissue doppler imaging from the lateral mitral valve annulus and the medial mitral valve attachment to the ventricular septum and E/E′ ratio was calculated. Left ventricular ejection fraction was calculated using biplane Simpson’s method in apical 2 chambers and apical 4 chambers views [19].
Metabolic profile Assessment of the metabolic profile was performed in the early morning under fasting conditions. Peripheral blood samples were obtained to measure uric acid, vitamin D, total and fractional cholesterol, triglycerides, glucose and insulin. Homeostatic model assessment (HOMA) index was calculated as the product of insulin (mU/ml) and glucose (mmol/l) divided by 22.5 [20].
2.3 Data Analysis
Data are expressed as means ± standard deviation (SD) and checked for normality using Shapiro-Wilks normality test and log-transformation. For multigroup comparisons depending on BP, BMI, waist circumference and LVMI, Levene's test has been performed to assess whether the variance is equal between groups. If the variance was heterogeneous, data have ben log-transformed before analysis. Regression models have been applied to analyse complex data. Comparisons between two groups have been assessed via t-test or non-parametric Mann–Whitney U-test. Two-way ANOVA has been used to determine the effects of different factors, in the case of independent categorical variables. ANCOVA analyses including variables such as BMI, age and gender as covariates have been also applied. The threshold of significance has been defined at P < 0.05. Correlation analyses with Bonferroni corrections have been also envisaged to determine the relationships between different parameters. SPSS and R software have been used for general statistical analyses.
3 Results
3.1 General Characteristics of the Study Population
Seventy-eight children and adolescents were included in the study. As shown in Table 1, when grouped accordingly to body weight categories, 10 were normoweight subjects, 11 overweight, 39 obese and 18 severe obese. Mean age amounted to 12.03± 2.44 years (means ± standard deviation) and males were 42 (53.8%). Study participants underwent 24 h ambulatory BP monitoring within one month from the echocardiographic assessment. Accordingly to the patterns of clinic and ambulatory BP values the study population was subdivided in different clinical BP phenotypes, i.e. normotension (n = 43, 55.1%), sustained hypertension (n = 7, 9.2%), white-coat hypertension (n = 10, 11.5%) and masked hypertension (n = 18, 24.2%). The general characteristics of the study population grouped by body weight categories are summarized in Tables 1 and 2. No significant difference in age, gender, height, and laboratory values between the 4 groups with different body weight values was detected. Also the distribution of the different BP phenotypes was superimposable in the study population subdivided accordingly to the four different body weight categories (Supplemental Table 1).
3.2 Echocardiographic Data
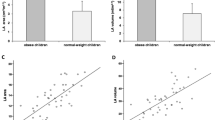
In the study population as a whole the presence of LVH was detected in 23 subjects (29.5%) according to the ESH definition [15, 16]. Concentric remodelling was detected in 16 individuals (20.5%) and concentric hypertrophy in 6 subjects (7.7%). When partitioning the whole study population by weight categories an increase in LVMI was observed with increasing BMI, particularly in the case of the severely obese group, although for this difference the P value did not achieve statistical significance (Table 3). The values of left atrial diameter were significantly greater in obese and severely obese subjects as compared to those found in normoweight individuals. A significant correlation was found between markers of body fat, such as BMI and waist circumference, and LVMI (Fig. 1). Furthermore, left atrial diameter values were significantly related to BMI, waist circumference (Fig. 1) and office heart rate (r = 0.293, P < 0.05). RWT was significantly (at least P < 0.05) correlated with BMI (r = 0.303), body weight (r = 0.371), waist circumference (r = 0.400), office systolic BP (r = 0.406), office heart rate (r = 0.271), diurnal ambulatory systolic BP (r = 0.253). No significant difference in the various echocardiographic parameters assessed in the present study was observed when partitioning the population in subgroups classified according to BP phenotypes, although a trend for an increase in LVMI was detected from the normotensive state to white-coat, masked and sustained hypertension (Supplemental Table 2). Partitioning the whole study population in subgroups according to the detection of an insulin resistance state, determined by a HOMA index value greater than the 3.6 a.u. pediatric cutoff value (21), a significant increase in LVMI as well as in the presence of LVH was found in insulin resistant subjects as compared to the non-insulin resistant counterparts (Fig. 2). In contrast relative wall thickness and left atrial diameter values were not significantly different in insulin- and non insulin resistant subjects. Insulin resistant subjects displayed significantly greater circulating plasma levels of glucose, insulin and triglycerides (Fig. 2).
Upper panels: relationships of body mass index (BMI, left panel), waist circumference (WC, right panel) and Left ventricular mass index (LVMI) in the study population. For each relationship r and P values are shown. Lower panels: between body mass index (BMI), left atrial diameter (LAD, left panel) and relative wall thickness in the same population. For each relationship r and P values are shown.
Mean ± SD values of HOMA index, plasma insulin, plasma triglycerides, plasma glucose, body mass index (BMI), waist circumference (WC), left ventricular mass index (LVMI) and percent values of detected left ventricular hypertrophy (LVH) in the population of the study classified accordingly to the absence (IR−) or presence (IR+) of insulin resistance (IR). Asterisks (*P < 0.05, **P < 0.01) refer to the level of statistical significance between the 2 groups.
4 Discussion
This single centre cross-sectional observational study was aimed at assessing in subjects in the pediatric age the main features of the association between anthropometric parameters, BP values, BP phenotypes and markers of cardiac organ damage, evaluated by echocardiography, in terms of structure and geometry. The main study findings can be summarized as follows. First, confirming recent findings [8, 9, 11, 22] markers of obesity such as body weight, BMI and waist circumference are strongly correlated LVMI in a pediatric population homogeneous in terms of biochemical profile and BP parameters. Second, the correlation was detected not only with left ventricular mass, but also with left atrial dimensions and RWT, i.e. parameters which, if affected, may favor with time the development of functional abnormalities leading to a ventricular diastolic dysfunction and cardiac failure as well [23]. Third, office BP, ambulatory BP and the different BP phenotypes appear to be also involved in favoring the development and progression of the cardiac structural alterations reported in childhood overweight and obesity, although the weaker correlation found between BP variables and echocardiographic parameters suggest a less relevant impact of haemodynamic mechanisms as compared to the anthropometric ones. Finally, not only a less or a more severe obese state but also the overweight condition, which is of more frequent clinical detection, appears to be associated with the structural alterations of the heart, suggesting therefore that even mild increases in body weight and body mass index may have an adverse impact on the left ventricle.
Our study also provides information on the role of metabolic factors in determining the relationships between overweight, obesity and cardiac structural alterations. In particular we found that the presence of an insulin resistance state represents the metabolic variable associated with an increased left ventricular mass and with the detection of LVH. Of additional interest is the finding that the insulin resistance state is associated with greater plasma triglyceride levels, which have been shown, at least in an adult obese population, to be independently related to left ventricular mass [24].
Our study was not designed at determining the precise mechanisms throughout which a pathological increase in body weight and body mass may trigger the development of the cardiac structural changes in subjects in pediatric age. We can speculate, however, that BP-dependent and BP-independent factors may participate [25]. Among the former, BP variability during the daytime and nighttime periods may play a relevant role, given the evidence that in adult overweight and obese subjects an increase in the short-term and long-term BP oscillations may be associated with a more pronounced cardiac organ damage [26]. Among the BP-independent factors a leading one is the hyperinsulinemic state, which is detectable in our insulin resistant young subjects, given the evidence that insulin may exert pro-hypertrophic effects at cardiac and vascular level [27, 28]. It may also include, however, the sympathetic nervous system, which (1) is activated in obese subjects at young and adult age, even when BP values are still in the normotensive range [29, 30], and (2) exerts directly and indirectly pro-hypertrophic cardiac effects [31]. These latter are confirmed by the evidence that adult patients with hypertension-related LVH display greater values of sympathetic nerve traffic and cardiac norepinephrine spillover as compared to age-matched hypertensive patients without evidence of cardiac organ damage [32, 33]. In should be noted that in the population of the present study, as well as in a previous study [30], obese and severe obese subjects display elevated heart rate values during daytime and the nighttime periods. Since heart rate is a marker, although indirect, of sympathetic cardiovascular drive [34], this finding may indicate that even at pediatric age the obese state is already characterized by a neuroadrenergic activation. Finally, elevated circulating blood levels of adipokines, leptin, such as those described in obese subjects, and activation of the renin-angiotensin system may be regarded as additional non-mutually exclusive factors favoring the development of the obesity-related cardiac structural alterations, given the evidence that both leptin, adipokines and angiotensin II exert marked prohypertrophic effects on the heart [35,36,37].
Our study has strengths and limitations. The strengths are represented by the fact that our study is the first to provide an extensive evaluation of young overweight an obese population, with simultaneous assessment of office BP, ambulatory BP, echocardiographic parameters and metabolic variables as well. The limitations include the relatively small sample size of the study population and the cross- sectional nature of the investigation which prevents to determine the hemodynamic, echocardiographic and metabolic changes and their interrelationships occurring during the follow-up. This was particularly the case for the determination of the main factor between BMI and HOMA index as responsible for the cardiac structural alterations observed in our subjects.
References
Cuspidi C, Rescaldani M, Sala C, Grassi G. Left ventricular hypertrophy and obesity—a systematic review and meta-analysis of echocardiographic studies. J Hypertens. 2014;32:16–25.
Abbasi SA, Hundley WG, Bluemke DA, Jerosch-Herold M, Blankstein R, Petersen SE, Rider OJ, Loma JC, Allison MA, Shah RV. Visceral adiposity and left ventricular remodeling: the multi-ethnic study of atherosclerosis. Nutr Metab Cardiovasc Dis. 2015;25:667–76.
Muiesan ML, Salvetti M, Di Castelnuovo A, Paini A, Assanelli D, Costanzo S, Badilini F, Vaglio M, Donati MB, Agabiti-Rosei E, de Gaetano G, Iacoviello L. Obesity and ECG left ventricular hypertrophy. J Hypertens. 2017;35:162–9.
Feng P, Huang Y, Wang S, Yu G, Li G, Lei H, Qin S, Huang W. Analysis of the association between obesity indices and left ventricular mass. Cardiology. 2018;141:183–9.
Crea P, Zito C, Cusmà Piccione M, Arcidiacono S, Todaro MC, Oreto L, Navarra G, Carerj S. The role of echocardiography in the evaluation of cafdiac organ damage in heypertensive obese patient. High Blood Press Cardiovasc Prev. 2015;22:23–7.
Vest AR, Patel AR. The heavy heart. Circ Heart Fail. 2017;10: e004092.
Berenson GS, Srinivasan SR, Bao W, Newman Third WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;38:1650–6.
Rodicio MM, Domenech de Miguel V, Jimenez MG, Gigarran Guldris S, Montserrat Lopez Franco M, Gestal AE, Couce M, Leis Trabazo MR. Early cardiac abnormalities in obese children and their relationship with adiposity. Nutrition. 2018;46:83–9.
Genovesi S, Tassistro E, Giussani M, Lieti G, Patti I, Orlando A, Montemerlo M, Antolini L, Parati G. Association of obesity phenotypes with left ventricular mass index and left ventricular hypertrophy in children and adolescents. Front Endocrinol. 2022;13:1006588.
Urbina EM, Mendizabal B, Becjìker RC, Daniels SR, Falkner BE, Hamdani G, Hanevold C, Hopoper SR, Ingelfinger JR, Lanade M, Martin LJ, Meyers K, Mitsnefes M, Rosner B, Samuels J, Flynn JT. Association of blood pressure level with left ventricular mass in adolescents. Hypertension. 2019;74:590–6.
Fabi M, Meli M, Leardini D, Andreozzi L, Maltoni G, Bitelli M, Pierantoni L, Zarbo C, Dondi A, Bertulli C, Bernardini L, Passion A, Lanari M. Body mass index is the strongest predictor of systemic hypertension and cardiac mass in a cohort of children. Nutrients. 2023;15:5079.
Cole TJ, Belizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. Br Med J. 2000;7244:1240–3.
WHO Multicentre Growth Reference Study Group. WHO child growth standards based on length/height, weight and age. Acta Paediatr. 2006;450:76–85.
De Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Flynn JT, Kaelber DC, Baker-Smith C, Blowey D, Carroll AE, Daniels SR, de Ferranti S, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140: e20171904.
Lurbe E, Agabiti-Rosei EA, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, Invitti C, Litwin M, Mancia G, Pall D, Rascher W, Redon J, Schaefer F, Seeman T, Sinha M, Stabouli S, Webb NJ, Wuhl E, Zanchetti A. European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887–920.
Stabouli S, Redon J, Lurbe E. Redefining hypertension in children and adolescents: a review of the evidence considered by the European Society of Hypertension and American Academy of Pediatrics guidelines. J Hypertens. 2020;38:196–200.
Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977;55:613–8.
Lai WW, Geva T, Shirali GS, Frommelt PC, Humes RA, Brook MM, Pignatelli RH, Rychlik J. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr. 2006;19:1413–30.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Tresaco B, Bueno G, Pineda I, Moreno LA, Garagorri JM, Bueno M. Homeostatic model assessment (HOMA) index cutoff values to identify the metabolic syndrome in children. J Physiol Biochem. 2005;61:381–8.
Trandafir LM, Cojocaru LM, Moscalu M, Leon Costantin MM, Miorn I, Mastaleru A, Teslariu M, Fotea S, Frasinariu O. Predictive markers of early cardiovascular impairment and insulin resistance in obese pediatric patients. Diagnostics. 2021;11:735.
Tadic M, Cuspidi C. Obesity and heart failure with preserved ejection fraction. A paradox or something else? Heart Fail Rev. 2019;24:379–85.
Pietri P, Georgiopoulos G, Tsiachris D, Kordalis A, Vlachopoulos C, Vyssoulis G, Stefanadis C. Triglycerides are related to left ventricular mass in hypertensive patients independently of other cardiometabolic risk factors: the effect of gender. Sci Rep. 2020;10:13253.
Talib A, Roebroek YGM, Paulus GF, van Loo K, Winkens B, Bouvy D, van Heurn ELW. Left ventricular geometrical changes in severely obese adolescents: prevalence, determinants, and clinical implications. Pediatr Cardiol. 2021;42:331–9.
Nardin C, Rattazzi M, Pauletto P. Blood pressure variability and therapeutic implications in hypertension and cardiovascular disease. High Blood Press Cardiovasc Prev. 2019;26:353–9.
Seravalle G, Grassi G. Sympathetic nervous system, hypertension, obesity and metabolic syndrome. High Blood Press Cardiovasc Prev. 2016;23:175–9.
Paternostro G, Pagano D, Gnecchi Ruscone T, Bonser R, Camici PG. Insulin resistance in patients with cardiac hypertrophy. Cardiovasc Res. 1999;42:246–53.
Grassi G, Seravalle G, Cattaneo BM, Bolla G, Lanfranchi A, Colombo M, Giannattasio C, Brunani A, Cavagnini F, Mancia G. Sympathetic activation in obese normotensive subjects. Hypertension. 1995;25:560–3.
Campos JO, Barros MAV, Oliveira TLPSA, Nobre IG, De Morais AS, Santos MAM, Leandro CG, Costa-Silva JH. Cardiac autonomic dysfunction in school age children with overweight and obesity. Nutr Met Cardiovasc Dis. 2022;32:2410–7.
Simpson P. Norepinephrine-stimulated hypertrophy of cultured rat myocardial cells is an alpha-1-adrenergic response. J Clin Invest. 1983;72:732–8.
Schlaich MP, Kaye DM, Lambert E, Sommerville M, Socratous F, Esler MD. Relation between cardiac sympathetic activity and hypertensive left ventricular hypertrophy. Circulation. 2003;108:560–5.
Greenwood JP, Scott EM, Stoker JB, Mary ASG. Hypertensive left ventricular hypertrophy: relation to peripheral sympathetic drive. J Am Coll Cardiol. 2001;38:1711–7.
Seravalle G, Facchetti R, Cappellini C, Annaloro A, Gelfi E, Grassi G. Elevated heart rate as sympathetic biomarker in human obesity. Nutr Metab Cardiovasc Dis. 2022;32:2367–74.
Perego L, Pizzocri P, Corradi D, Maisano F, Paganelli M, Fiorina P, Barbieri M, Morabito A, Paolisso G, Folli F, Pontiroli AE. Circulating leptin correlates with left ventricular mass in morbid (grade III) obesity before and after weight loss induced by bariatric surgery: a potential role for leptin in mediating human left ventricular hypertrophy. J Clin Endocrinol Metab. 2005;90:4087–93.
von Jeinsen B, Ritzen L, Vietheer J, Unbehaun C, Weferling M, Liebetrau C, Hamm CW, Rolf A, Keller T. The adipokine fatty-acid binding protein 4 and cardiac remodeling. Cardiovasc Diabetol. 2020;29:117.
Yamazaki T, Komuro I, Kudoh S, Zou Y, Shiojima I, Mizuno T, Takano H, Hiroi Y, Ueki K, Tobe K. Angiotensin II partly mediates mechanical stress-induced cardiac hypertrophy. Circ Res. 1995;77:258–65.
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors declare that they have no conflict of interest. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Compliance with ethical standards
The Ethics committee approved the protocol of this study. All procedures performed in the present study are in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Annaloro, A., Invernizzi, C., Aguilar, F. et al. Association Between Elevated Body Mass Index and Cardiac Organ Damage in Children and Adolescents: Evidence and Mechanisms. High Blood Press Cardiovasc Prev 31, 167–175 (2024). https://doi.org/10.1007/s40292-024-00633-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-024-00633-5