Abstract
Background
Pediatric obesity is a global emerging burden for society; among its health-related consequences there are hypertension (HTN) and left ventricular hypertrophy (LVH). Several anthropometric indices have been investigated for the early identification of cardiovascular risk in children. The aim of the present study was to assess whether tri-ponderal mass index (TMI) was associated with LVH in a cohort of Caucasian children and adolescents with obesity.
Methods
In this observational study, 63 children and adolescents with obesity aged 7-to-16 years were enrolled. During outpatient visits, adiposity, and cardio-metabolic indices (BMI z-score, WHR, TMI, ABSI) were collected. All subjects underwent a 24-hour ambulatory blood pressure monitoring (ABPM) and transthoracic echocardiography.
Results
Children and adolescents with obesity with LVH had significantly higher BMI z-score (p = 0.009), WHR (p = 0.006) and TMI (p = 0.026) compared to children without LVH. WC and WHR were the only indices significantly associated with left ventricular mass index (LVMI).
Conclusion
Left ventricular remodeling is associated with the cardio-metabolic risk markers WC and WHR, but not with the adiposity index TMI among children with obesity.
Similar content being viewed by others
Introduction
Obesity is the most prevalent chronic disease among children worldwide and it is a global significant burden for society [1]. Obesity can have many consequences on health, particularly Metabolic Syndrome (MetS) [2], described as a cluster of cardiovascular (CVD) risk factors such as abdominal obesity, hyperglycaemia, dyslipidaemia and hypertension (HTN) [3]. The known association between childhood BMI and adult cardio-metabolic diseases may reflect a common genetic predisposition, but could also be related to BMI persistence from childhood to adulthood [4].
HTN in children with obesity is a strong predictor of HTN in adulthood [5], and when it occurs during childhood or adolescence, it usually persists in adulthood even if Body Mass Index (BMI) is normalized into normal ranges [6]. To identify children at risk, along with office blood pressure (BP) measurement, 24-hour ambulatory BP monitoring (ABPM) is a useful diagnostic tool.
Observational studies confirm a greater left ventricular mass, left ventricular septal and posterior wall thickness, and left ventricular end-diastolic diameter in children with obesity when compared to lean subjects, even in subjects without hypertension [7,8,9]. The association of obesity and abnormal left ventricular geometry and function is debated; it is not clear whether it is the obesity itself to determine left ventricular alterations, or whether there is an intermediate player such as HTN or other subtle vascular changes [10].
Different anthropometric indices that are surrogates of body composition have been investigated for the early identification of CVD risks. BMI cannot accurately depict body composition in the pediatric population, as weight and height squared are not proportional during some growth phases [11]. Also BMI z-score, known as the standard indicator for screening paediatric obesity, showed to be only weakly associated with other measures of body fatness in paediatric age [12].
Therefore Peterson et al. proposed the Tri-ponderal Mass Index (TMI) as a replacement for BMI z-score in screening for body fat in children and adolescents [13]. Interestingly, TMI demonstrated a lower rate of misclassification than BMI in detecting body fat and HTN in overweight adolescents [13]. Notably TMI was proposed as a more reliable index among overweight and children with obesity [13,14,15]. Additionally, in our previous work we found TMI as being a good predictor of high blood pressure among males older than 10 years of age [16], although we assessed exclusively office blood pressure in an outpatient setting.
A Body Shape Index (ABSI) has been showed to have considerable associations with cardiometabolic risk markers in children and adolescents with obesity [16,17,18,19].
Up to date no studies have investigated the association between TMI or ABSI and left ventricular hypertrophy in pediatric age groups.
Conversely, evidence is emerging regarding the potential implication of the Waist-to-height ratio (WHR). WHR predicts abdominal fat mass and takes body size into account [20] and a value ≥ 0.55 is a proper cut-off for screening European children at high cardiometabolic risk [21, 22]. WHR has certain advantages over WC alone, since having a universal cut-off would help standardize practice, which may be independent of age, sex, height and race [21]. Moreover its utility in discriminating children with cardiac structural damage, mainly left ventricular hypertrophy (LVH) and left ventricular geometry (LVG), has been reported [23, 24].
The aim of this observational study was to assess whether TMI was associated with LVH in Caucasian children and adolescents affected by obesity. Secondarily, we sought to identify anthropometric, adiposity and glycometabolic indices that predicted left ventricular mass index (LVMI) in a population accurately screened using ABPM and echocardiography.
Materials and methods
Subjects and design
This was an observational study conducted from September 2016 to February 2018 based on a cohort of consecutive Caucasian children and adolescents with obesity enrolled at the outpatient settings of the Paediatric Department of the San Paolo Hospital in Milan (Italy) as already described [9]. To be eligible to participate in the present study, individuals had to respect the following inclusion criteria:
-
1)
between 7-to-16 years of age;
-
2)
diagnosis of obesity according to World Health Organization criteria (BMI z scores for age and gender ≥ + 2 Standard Deviations) [25];
-
3)
agreement by the individual and their legal guardian to fully participate in the assessments;
-
4)
absence of secondary obesity, familiar dyslipidaemia with glucose metabolism alterations, diabetes mellitus, hypertension, pre-existing cardiovascular diseases and genetic or endocrine dysfunction.
After enrollment, all participants underwent a complete examination in the pediatric obesity outpatient clinic, including a medical visit, anthropometric assessments, repeated office BP measurements, echocardiogram, and 24-hour ABPM.
This study was approved by the hospitals’ Institutional Review Boards and all procedures were conducted in line with the Declaration of Helsinki. The study was conducted in accordance with the local medical ethical committee (protocol number 2015/ST/135).
At recruitment, all participants and their legal guardian provided written informed consent.
Anthropometric assessments and adiposity indices
After enrollment all children underwent physical examination, as previously described [9]. Anthropometric assessment, including body weight, height and waist circumference (WC) measurements, were performed by well-trained health professionals. BMI was calculated as:
BMI values were standardized into BMI z-scores, using WHO reference values [25].
To better assess cardio-metabolic risk, WHR index was calculated as [26]:
TMI was calculated according to the following formula:
ABSI was calculated as [27]:
Biochemical parameters and glycometabolic indices
Insulin and fasting blood glucose were determined by venous blood sampling after twelve hours of fasting. The glycometabolic indices Homeostatic Model Assessment Index– Insulin Resistance (HOMA-IR), HOMA of β-cell function (HOMA-β) and QUantitative Insulin-sensitivity Check Index (QUICKI) were calculated. These glycometabolic indices are used in clinical practice to detect children and adolescents at risk of type 2 diabetes mellitus calculated as previously described [9].
Blood pressure and 24-hour ABPM
Detailed description of procedure are described elsewhere [9]. In brief, office BP was measured by means of mercury sphygmomanometer and stethoscope according to European guidelines [28]. Systolic BP (SBP) and diastolic BP (DBP) values were the average of the last two mesaurments. The percentiles of SBP and DBP were calculated by reference normograms distributed by sex, age and height in accordance with the recommendations provided by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents and the European Society of Hypertension [28, 29].
The 24 h ABPM exam was collected by means of Custo screen 300 med (Sylcomed, Sylco S.r.l.) device. 24-hour, daytime and night-time mean SBP and DBP were recorded and evaluated according to American Heart Association (AHA) recommendations [30]. According to 24 h-ABPM results children were classified as normotensive, if mean 24-h BP values were normal, or hypertensive.
Echocardiography
Subjects affected by obesity underwent transthoracic echocardiography, as already described [9]. The exams were performed by the same operator. Transthoracic echocardiography was conducted to obtain left ventricular end-diastolic diameter, interventricular septum and posterior wall thickness, by averaging standard M-mode measurements in three different cardiac cycles according to the American Society of Echocardiography recommendations [31]. Left ventricular mass was estimated using the Devereux formula [32]. Left ventricular mass index (LVMI, g/m2) and relative wall thickness (RWT) were calculated according to the American Society of Echocardiography indications [31]. Age- and sex-corrected LVMI percentiles were used [33] and age-corrected RWT values above 0,390 were considered abnormal [34]. Left ventricular hypertrophy was defined as LVMI or RWT equals or greater than 95th percentile for age and sex [28].
Statistical analysis
Continuous variables were expressed as median (interquartile range) as they were not normally distributed according to normality tests. Discrete variables were reported as frequency and percentage. Mann-Whitney U test and χ2 test were used as appropriate to compare characteristics of patients affected by obesity with and without left ventricular hypertrophy and of hypertensive and non-hypertensive patients with obesity (according to ABPM readings). Spearman correlation test was used to assess continuous variables correlations. Multiple testing adjustment was performed according to Bonferroni-Holm. Sex- and age-adjusted logistic multivariable analysis models were used to assess the association between BMI z-score, TMI, WC, WHR or ABSI with presence of left ventricular hypertrophy. McFadden pseudo-R2 was used as a measure of association. P values < 0.050 were considered statistically significant. Statistical analyses were performed using SPSS Statistics version 20 (IBM Corp., Armonk, NY).
Results
Table 1 shows anthropometric, adiposity and glycometabolic indices, office SBP and DBP, main echocardiography and ABPM parameters of patients affected by obesity. Sixty-three children and adolescents with obesity were enrolled. The median age of the patients was 11 years. Fourteen patients were diagnosed with LVH at echocardiography and 35% of patients were diagnosed as hypertensive at ABPM. Table 1 also illustrates gender differences. Twenty-one (49.2%) patients were females. The BMI z-score was not significantly different between the two groups. Twenty-five (78%) males and twenty-four females (77%) with obesity were diagnosed with LVH at echocardiography while 56% of males and 74% of females were diagnosed as hypertensive at ABPM.
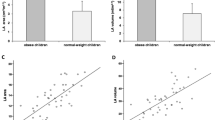
Patients were grouped according to presence of LVH at echocardiography. Table 2 compares the above-mentioned indices in patients with and without LVH. Children and adolescents with obesity with LVH had significantly higher BMI z-score, TMI and WHR. HOMA-β was significantly higher in patients with LVH. Mean 24-hour SBP and DBP did not differ significantly between patients with and without LVH (Table 2).
Anthropometric, adiposity and glycometabolic indices, office SBP and DBP, main echocardiography and ABPM parameters were compared in patients with and without hypertension at ABPM (Table 3). WC was significantly higher in patients with hypertension, as HOMA-IR and HOMA-β, while QUICKI was significantly lower in hypertensive patients. LVMI and prevalence of LVH did not differ significantly between hypertensive and non-hypertensive patients (Table 3).
Table4 shows a Spearman?s correlation heatmap. WHR was the only central adiposity index that significantly correlated with LVMI.
Table5 Shows sex- and age-adjusted association between adiposity indices and left ventricular hypertrophy.
Discussion
To the best of our knowledge, this is the first study evaluating the association between TMI and LVH in a group of children and adolescents with obesity. In the studied cohort, patients affected by obesity with LVH had significantly higher BMI z-score, WHR and TMI compared to the group without LVH. A higher TMI is therefore associated with LVH, though TMI, unlike WHR, did not correlated with left ventricular mass index.
It is well known that pediatric onset obesity is related to both target organ damage in the short term, and increased CVD risk and early mortality in adulthood [35, 36]. Therefore, prevention and treatment of obesity and its related detrimental health consequences is essential, starting from pediatric age. Several cardiovascular conditions may affect children with obesity, especially HTN [37] and LVH [8].
Although recent years have seen increased interest in assessing the presence of cardiovascular complications in children and adolescents with obesity, to date there are only few studies evaluating the association of adiposity indices with HTN and LVH.
TMI was originally proposed for its better stability across the age span in children and adolescent, obviating the need for z-scores calculation, and for its improved reliability in identifying body fat compared to BMI [13]. In line with this, Malavazos et al. demonstrated that TMI was superior to BMI as a body fat index [15]. Sun et al., in their systematic review, confirmed that TMI provided similar or better prediction of body adiposity compared to BMI in paediatric age. However, regarding cardio-metabolic outcomes, they found only few studies examining the correlation between TMI and blood pressure. They concluded that either TMI or BMI performed poorly in identifying high BP in children and adolescents, and that their ability varied in different populations [38]. Subsequently, few studies have argued in favour of TMI as a suitable index in discriminating cardio-metabolic risk factors [5, 11]. Alvim et al. showed a strong association between TMI values and CVD risk in a sample of 37.815 Brazilian adolescents (12–17 years old). In fact, adolescents classified as obese (TMI-for-age ≥ 95th percentile) had a higher prevalence of hypertension [11]. In another longitudinal cohort of 36.950 subjects (6–17 years old), the capacity of TMI slightly outperformed BMI in predicting pediatric HTN. The discriminating power of HTN was even stronger when considering the subgroup of subjects aged ≥ 16 years [39].
Previously, we found TMI is a good predictor of high BP among males older than 10 years of age [16], although we assessed exclusively office BP in an outpatient setting. In the present study, focused on a smaller cohort, we didn’t observe an association between TMI and HTN. It is important to note, though, that in the present cohort of subjects HTN was diagnosed using ABPM, obviating the known issue of masked HTN and white coat HTN, particularly common in the pediatric population [9]. We are unaware of previous studies on the association between adiposity indices and HTN diagnosed at ABPM.
HTN is the main cause of LVH in the general population, although it has already been described how in the obese pediatric population LVH can be found independently from HTN [10]. The present study confirms this finding in a population studied extensively with ABPM.
It has long been known in the literature that LVH is associated with obesity, mostly abdominal obesity [40]. As previously reported, TMI is a surrogate index of overall adiposity [13], and it is not a direct measure of visceral or abdominal fat. It is possible that we failed in demonstrating a correlation between TMI and LVMI, since TMI is a surrogate index of total fat and not of fat distribution. On the contrary, in the present work LVMI was significantly associated with WHR and WC. This is not surprising, as WHR and WC are well-known indicators of abdominal fat mass [21]. Recently, WHR showed similar ability in predicting LVH and left ventricular remodeling in a group of hypertensive children and adolescents compared to BMI or WC [23]. Moreover WHR had a better or similar predictive power compared to BMI in identifying eccentric hypertrophy (EH) and concentric hypertrophy (CH) in children aged 6-to-11 years [24], whilst WC performed worst. Hence, WHR has been proposed as a simple and convenient index for screening youth at high risk of target organ damage [23, 24].
As the WHR is an easy measure to perform and to interpret with a fixed cut-off of 0,55 for children, it seems suitable for use in medical practice [21]. Some authors suggested the use of TMI in conjunction with WHR to identify overweight adolescents at high cardio-metabolic risk [15], but further studies need to be conducted.
Finally, it is interesting to note that glycometabolic indices (HOMA- IR, HOMA-β and QUICKI) are strongly associated with the diagnosis of HTN at ABPM in children with obesity [9] but only weakly associated with LVH.
Our study has some limitations: first, a narrow sample size, although homogenous, may have limited the power of statistical tests. Secondly, we have investigated the role of adiposity indices which are surrogate indicators of body fat, whereas a body composition assessment would have been a direct measure of adiposity. It is possible that direct assessment of visceral adiposity distribution (with Dual Energy X-ray Absorptiometry, DEXA) is a better predictor of LVH in children with obesity, but this hypothesis needs to be tested in future studies. Thirdly, inter-observer agreement analysis is not available for auxological evaluation. The ABPM monitoring in every patient, on the other hand, represents the greatest strength of our study.
Conclusion
TMI, a surrogate indicator of total body fat, is higher in children and adolescents with obesity with LVH when compared to children and adolescents with obesity without LVH, although WC and WHR were significantly associated with LVMI.
Data availability
Not applicable.
References
Verduci E, Bronsky J, Embleton N, Gerasimidis K, Indrio F, Köglmeier J, et al. Role of dietary factors, Food habits, and lifestyle in childhood obesity development: a position paper from the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2021;72:769. https://doi.org/10.1097/MPG.0000000000003075.
Weihe P, Weihrauch-Blüher S. Metabolic syndrome in children and adolescents: diagnostic criteria, Therapeutic options and perspectives. Curr Obes Rep. 2019;8:472–9. https://doi.org/10.1007/s13679-019-00357-x.
Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome-a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80. https://doi.org/10.1111/j.1464-5491.2006.01858.x.
Vogelezang S, Bradfield JP, Ahluwalia TS, Curtin JA, Lakka TA, Grarup N, et al. Novel loci for childhood body mass index and shared heritability with adult cardiometabolic traits. PLoS Genet. 2020;16:e1008718. https://doi.org/10.1371/journal.pgen.1008718.
Cui Y, Zhang F, Wang H, Zhao L, Song R, Han M, et al. Temporal associations between Tri-ponderal Mass Index and Blood pressure in Chinese children: a Cross-lag Analysis. Nutrients. 2022;14:1783. https://doi.org/10.3390/nu14091783.
Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–46. https://doi.org/10.1542/peds.2006-2543.
de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20:1251–60. https://doi.org/10.1016/0735-1097(92)90385-z.
Alpert MA. Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci. 2001;321:225–36. https://doi.org/10.1097/00000441-200104000-00003.
Vizzuso S, Del Torto A, Fiore G, Milanta C, Locatelli G, D’Errico A, et al. Hypertension in a cohort of obese caucasian children and adolescents and its association with glycometabolic indices: a proposed screening tool. Nutr Metab Cardiovasc Dis. 2023;33(4):900–12. https://doi.org/10.1016/j.numecd.2023.01.001.
Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS. Childhood adiposity as a predictor of cardiac mass in adulthood: the Bogalusa Heart Study. Circulation. 2004;110:3488–92. https://doi.org/10.1161/01.CIR.0000149713.48317.27.
Alvim R, de O, Siqueira JH, Zaniqueli D, Paiva NS, Baldo MP, Bloch KV, et al. Reference values for the tri-ponderal mass index and its association with cardiovascular risk factors in Brazilian adolescents aged 12 to 17 years. Nutrition. 2022;99–100111656. https://doi.org/10.1016/j.nut.2022.111656.
Freedman DS, Butte NF, Taveras EM, Lundeen EA, Blanck HM, Goodman AB, et al. BMI z-Scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–2014. Obesity. 2017;25:739–46. https://doi.org/10.1002/oby.21782.
Peterson CM, Su H, Thomas DM, Heo M, Golnabi AH, Pietrobelli A, et al. Tri-ponderal Mass Index vs Body Mass Index in estimating body Fat during Adolescence. JAMA Pediatr. 2017;171:629. https://doi.org/10.1001/jamapediatrics.2017.0460.
Wang X, Ma J, Huang S, Dong B, Dong Y, Yang Z, et al. Use of Tri-ponderal Mass Index in Predicting Late adolescent overweight and obesity in children aged 7–18. Front Nutr. 2022;9:785863. https://doi.org/10.3389/fnut.2022.785863.
Malavazos AE, Capitanio G, Milani V, Ambrogi F, Matelloni IA, Basilico S, et al. Tri-ponderal Mass Index vs body Mass Index in discriminating central obesity and hypertension in adolescents with overweight. Nutr Metab Cardiovasc Dis. 2021;31:1613–21. https://doi.org/10.1016/j.numecd.2021.02.013.
Leone A, Vizzuso S, Brambilla P, Mameli C, Ravella S, De Amicis R, et al. Evaluation of Different Adiposity Indices and Association with metabolic syndrome risk in obese children: is there a winner? Int J Mol Sci. 2020;21:E4083. https://doi.org/10.3390/ijms21114083.
Duncan MJ, Mota J, Vale S, Santos MP, Ribeiro JC. Associations between body mass index, waist circumference and body shape index with resting blood pressure in Portuguese adolescents. Ann Hum Biol. 2013;40:163–7. https://doi.org/10.3109/03014460.2012.752861.
Mameli C, Krakauer NY, Krakauer JC, Bosetti A, Ferrari CM, Moiana N, et al. The association between a body shape index and cardiovascular risk in overweight and obese children and adolscents. PLoS ONE. 2018;13:e0190426. https://doi.org/10.1371/journal.pone.0190426.
Ge W, Yi L, Xiao C, Xiao Y, Liu J, Liang F, et al. Effectiveness of a body shape index in predicting pediatric high blood pressure. Pediatr Res. 2022;92:871–9. https://doi.org/10.1038/s41390-021-01844-5.
Martin-Calvo N, Moreno-Galarraga L, Martinez-Gonzalez MA. Association between Body Mass Index, Waist-to-height ratio and adiposity in children: a systematic review and Meta-analysis. Nutrients. 2016;8:512. https://doi.org/10.3390/nu8080512.
Muñoz-Hernando J, Escribano J, Ferré N, Closa-Monasterolo R, Grote V, Koletzko B, et al. Usefulness of the waist-to-height ratio for predicting cardiometabolic risk in children and its suggested boundary values. Clin Nutr. 2022;41:508–16. https://doi.org/10.1016/j.clnu.2021.12.008.
Lo K, Wong M, Khalechelvam P, Tam W. Waist-to-height ratio, body mass index and waist circumference for screening paediatric cardio-metabolic risk factors: a meta-analysis. Obes Rev. 2016;17:1258–75. https://doi.org/10.1111/obr.12456.
Cheng H, Xi B, Liu J, Yan Y, Mi J. Performance of different adiposity measures for predicting left ventricular remodeling in Chinese hypertensive youth. Sci Rep. 2021;11:21943. https://doi.org/10.1038/s41598-021-00978-0.
Wang H, Zhao M, Magnussen CG, Xi B. Utility of three adiposity indices for identifying left ventricular hypertrophy and geometric remodeling in Chinese children. Front Endocrinol (Lausanne). 2021;12:762250. https://doi.org/10.3389/fendo.2021.762250.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7. https://doi.org/10.2471/blt.07.043497.
Yoo E-G. Waist-to-height ratio as a screening tool for obesity and cardiometabolic risk. Korean J Pediatr. 2016;59:425–31. https://doi.org/10.3345/kjp.2016.59.11.425.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE. 2012;7:e39504. https://doi.org/10.1371/journal.pone.0039504.
Lurbe I, Ferrer E. European Society of Hypertension Guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34(10):1887–920. https://doi.org/10.1097/HJH.0000000000001039.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice Guideline for Screening and Management of High Blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904. https://doi.org/10.1542/peds.2017-1904.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. https://doi.org/10.1016/j.echo.2005.10.005.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8. https://doi.org/10.1016/0002-9149(86)90771-x.
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR. Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr. 2009;22:709–14. https://doi.org/10.1016/j.echo.2009.03.003.
de Simone G, Daniels SR, Kimball TR, Roman MJ, Romano C, Chinali M, et al. Evaluation of concentric left ventricular geometry in humans: evidence for age-related systematic underestimation. Hypertension. 2005;45:64–8. https://doi.org/10.1161/01.HYP.0000150108.37527.57.
Cote AT, Harris KC, Panagiotopoulos C, Sandor GGS, Devlin AM. Childhood obesity and cardiovascular dysfunction. J Am Coll Cardiol. 2013;62:1309–19. https://doi.org/10.1016/j.jacc.2013.07.042.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond). 2011;35:891–8. https://doi.org/10.1038/ijo.2010.222.
Magge SN, Goodman E, Armstrong SC, COMMITTEE ON NUTRITION, SECTION ON ENDOCRINOLOGY, SECTION ON OBESITY. The metabolic syndrome in children and adolescents: shifting the focus to cardiometabolic risk factor clustering. Pediatrics. 2017;140:e20171603. https://doi.org/10.1542/peds.2017-1603.
Sun J, Yang R, Zhao M, Bovet P, Xi B. Tri-ponderal Mass Index as a Screening Tool for identifying body Fat and Cardiovascular Risk factors in children and adolescents: a systematic review. Front Endocrinol (Lausanne). 2021;12:694681. https://doi.org/10.3389/fendo.2021.694681.
Hu J, Zhong Y, Ge W, Lv H, Ding Z, Han D, et al. Comparisons of tri-ponderal mass index and body mass index in discriminating hypertension at three separate visits in adolescents: a retrospective cohort study. Front Nutr. 2022;9:1028861. https://doi.org/10.3389/fnut.2022.1028861.
Bastien M, Poirier P, Lemieux I, Després J-P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56:369–81. https://doi.org/10.1016/j.pcad.2013.10.016.
Acknowledgements
Not applicable.
Funding
The present publication was supported by the Department of Health Sciences of the University of Milan, Milan, Italy, which received funding from the PRIN2022 (Title project “An app to shed the light on the window of opportunity of the first 1000 days of life”; coordinator University of Foggia, Italy; funded by Italian Ministry of Education, University and Research).
Author information
Authors and Affiliations
Contributions
Conceptualization, E.V.; methodology, S.V., A.D.T.; validation, E.V.; formal analysis, A.D.T, S.V.; investigation, S.V, A.D.T., G.F.; data curation, S.V., A.D.T., G.F., S.C.; writing—original draft preparation, S.V., A.D.T., G.F.; writing—review and editing, E.V.; visualization, E.V.; supervision, G.Z. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki, and all the procedures involving human participants were approved by the human research ethics committees of the University of Milan and the hospitals’ Institutional Review Boards.
Consent to participate
Written informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vizzuso, S., Torto, A.D., Fiore, G. et al. Tri-ponderal mass index and left ventricular hypertrophy in a cohort of caucasian children and adolescents with obesity. Ital J Pediatr 50, 75 (2024). https://doi.org/10.1186/s13052-024-01634-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-024-01634-9