Abstract
Environmental pollution in considered an established determinant of non-communicable illness, including cardiovascular diseases (CVDs). Air pollution is the result of a complex combination of chemical, physical, and biological agents, and represents one of the main causes of mortality and morbidity in the world population. It is responsible for 7.6% of global mortality. In this regard, it has been documented that it increases the risk of CVDs and major adverse cardiovascular and cerebrovascular events. In northern regions of China, long-term exposures to the particulate matter < 2.5 µm (PM2.5) increase in the risk of ischemic heart disease by almost two-folds. Similarly, the additional risk for stroke, increases by almost 10% for long-term exposure to PM2.5. The detrimental effects of air pollution on cardiovascular system are particularly manifest in vulnerable subjects, such as the elderly, patients with heart disease, and obese individuals. Therefore, nowadays, cardiovascular prevention strategies, in addition to controlling traditional risk factors, should also include measures to improve the environment. This goal can be achieved by the implementation of the health surveillance in occupational medicine and by the extensive application of the national and international legislative measures. In fact, the health surveillance represents a crucial preventive measure for workers exposed to health risks (chemical, physical agents, etc.) that may lead to occupational diseases after long-term exposure. On the other hand, since environmental pollution does not recognize well-defined boundaries, only the implementation of regulations among large territorial areas can be useful to improve the quality of environment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In recent years there are growing body of evidence that document that, in addition to conventional risk factors, the environment plays a key role in the determinism of cardiovascular diseases (CVD) and major adverse cardiovascular and cerebrovascular events (MACCE). In this regard, there is clear evidence that air pollution significantly contributes to the pathogenesis of CVD, while there is less convincing data for noise pollution and light pollution. It should be emphasized that the impact of environmental pollution as a risk determinant is amplified in vulnerable individuals, such as the elderly, patients with heart disease, and obese individuals. In the consideration of climate changes observed in the last years, this issue becomes particularly relevant in terms of public health. Therefore, nowadays, cardiovascular prevention strategies, in addition to controlling traditional risk factors, should also include measures to improve the environment as a whole. Since environmental pollution does not recognize well-defined boundaries, this goal can only be achieved through the implementation of regulations uniformly over large territorial areas, as well as through cooperation between various nations. Therefore, directives on pollution control issued by legislative bodies at both national and international levels are an important tool for primary and secondary cardiovascular (CV) prevention.
2 Air Pollution
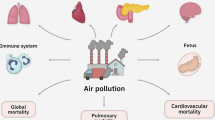
Air pollution is the result of a complex combination of chemical, physical, and biological agents, which varies depending on multiple factors such as geographic areas, weather conditions, population density, and degree of industrialization. Nowadays, it is considered one of the main causes of mortality and morbidity in the world population. In fact, the Global Burden of Disease has estimated that air pollution is responsible for 7.6% of global mortality [1]. In particular, the World Air Quality Report published in 2019 reports that 24% of deaths from stroke and 25% of deaths from ischemic heart disease can be attributed to air pollution [2, 3].
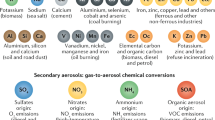
The main determinants of air pollution are represented by atmospheric particulate matter and gases. Atmospheric particulate matter refers to the combination of solid and liquid particles suspended in the air, with sizes ranging from a few nanometres to 100 μm. Depending on the particle size, particulate matter is classified as PM10, which consists of particles with sizes < 10 µm, and PM2.5, which consists of particles with diameters < 2.5 µm. Ultrafine particulate matter is characterized by particles < 0.1 µm (PM0.1); it is mainly generated by combustion processes, is prevalent in large urban and industrial areas, and is extremely harmful to health due to its ability to reach the deepest parts of the respiratory system.
Additional byproducts resulting from the use of fossil fuels, which significantly contribute to the deterioration of air quality, are nitrogen oxides (NOx). Upon contact with oxygen, Nox transforms into nitrogen dioxide (NO2), which is an irritant gas for the airways and, in turn, contributes to the formation of ozone and nitric acid.
3 Mortality and Morbidity in Cardiovascular Diseases (CVDs)
Numerous studies and meta-analyses have demonstrated that both short-term and long-term exposures to high levels of PM2.5, PM10, and NOx are associated with increased mortality and hospital admissions for CVDs [3]. It is interesting to note that although statistically significant, the risk of cardiovascular mortality and hospitalization is moderately increased for short-term exposures to particulate matter and nitrogen oxides. Conversely, for long-term exposures to PM2.5 and NOx, the risk is significantly higher. Specifically, for every 10 μg/m3 increase in PM2.5, there is an additional risk of mortality and hospitalization for CVDs ranging from 11 to 20%, and for every 10 μg/m3 increase in NOx, there is an additional risk ranging from 3 to 23% [3].
4 Ischemic Heart Disease and Myocardial Infarction
Short-term exposures to PM2.5 and NOx have been shown to increase the risk of mortality and hospitalizations for ischemic heart disease. The additional risk for PM2.5 exposures ranges from 2.5 to 3.36, and for NOx, it ranges from 0.88 to 1.42. This phenomenon is particularly evident in China, where higher concentrations of PM2.5 have been documented in northern regions compared to southern regions. This is associated with a 1.8% increase in the risk of ischemic heart disease [4].
Similar associations have been observed between concentrations of PM2.5, PM10, and NOx, and hospitalization and mortality for myocardial infarction. For short-term exposures to 10 μg/m3 of PM2.5, PM10, and NOx, the additional risk ranges from 1.2 to 2.4, from 0.5 to 1.1, and from 1.1, respectively.
5 Stroke
The most convincing evidence of the link between environmental pollution and CVDs has been documented for stroke. Both short-term and long-term exposures to PM2.5, PM10, and NOx increase the risk, hospitalizations, and mortality for both ischemic and haemorrhagic stroke. However, this data underestimates the burden of disability resulting from cerebrovascular events caused by pollution. Exposures to 10 μg/m3 of PM2.5 result in an additional risk increase in stroke incidence ranging from 11 to 14%, and in stroke mortality ranging from 11 to 26%. No association has been found between pollution and stroke subtype.
Closely linked to the risk of cerebrovascular events induced by pollution is the risk of atrial fibrillation. A meta-analysis has shown that for every 10 μg/m3 increase in PM2.5, the risk of atrial fibrillation increases by 24% [5].
6 Arterial Hypertension
Air pollution has a significant impact on blood pressure regulation. A meta-analysis evaluating a total of 17 studies that analysed the effects of air pollutants, both short-term (6 studies) and long-term (11 studies), It has been documented that both short-term and long-term exposures to PM2.5, PM10, and NOx lead to an increased incidence of arterial hypertension [6]. As above mentioned, the air pollution is mainly generated by the combustion processes. Interestingly, not only the industrial activity, but also the burning of natural sources can generate atmospheric particulate matters. At this regard, recently, it has been reported that during the Athens 2021 wildfires the air concentration of PM2.5 increased by 54.68%. This was associated, in 20 patients under the antihypertensive treatment, with an increase of 2.1 mmHg of systolic blood pressure (SBP). The multivariate regression analysis documented that the change of PM2.5 air concentration before and during wildfires was independently associated with the variation of SBP. Despite the very small sample size of this study, these results highlight the detrimental effect of the “climate changes” can have, in the next future, on the CV risk [7].
7 Pathogenetic Aspects
The pathogenetic mechanisms underlying the strong association between air pollution and CV risk are multifactorial and complex. The primary driver of this complex association is oxidative stress triggered by the inhalation of air pollutants. Excess oxygen free radicals initiate a cascade reaction that leads to the oxidation of lipids, proteins, DNA, and the activation of an inflammatory state. This results in alterations in cardiomyocytes, endothelial cells, and smooth muscle cells, ultimately compromising cardiac and vascular function [8]. Long-term exposure to PM2.5 has been shown to impair antioxidant capacity and reduce cardiac contractility in mice [9]. Furthermore, studies on volunteers have documented that PM exposure triggers a pulmonary and systemic inflammatory response, manifested by increased circulating levels of C-reactive protein and interleukin-6, leading to an increased thrombotic risk and alterations in mechanisms controlling blood pressure [10]. The main pathogenetic mechanisms responsible for the CV risk associated with air pollution are depicted in Fig. 1.
Continuum in cardio- and cerebrovascular diseases induced by air pollution. Air pollutants activate different pathogenic mechanisms that results in many forms of target organ damage, which, in turn, participate to the development of cardiovascular risk factors, that account for the occurrence of cardio- and cerebrovascular diseases. CV Cardiovascular, PM2.5 Particulate Matter with diameter < 2.5 μm, PM10 Particulate Matter with diameter < 10 μm, NO2 Nitrogen Dioxide, O3 Ozone, SO2 Sulfur Dioxide, CO Carbon Monoxide
8 Noise and Light Pollution
There is less strong evidence regarding the impact of noise and light pollution on the increased CV risk. The Danish Nurse Cohort study has documented an association between traffic-related noise pollution and increased stroke incidence [11]. Additionally, it has been reported that noise pollution from railway, air, and road traffic increases CV mortality [12]. Another determinant of environmental pollution is light pollution. There is convincing evidence that light pollution, especially in the elderly population, disrupts blood pressure regulation. Excessive nocturnal illumination (> 5 Lux) has been shown to induce increases in nocturnal systolic blood pressure ranging from 3 to 4 mmHg [13]. Further studies have demonstrated that light pollution in elderly individuals is associated with an Increased risk of hospitalizations (HR 1.11, 95% CI 1.03–1.18) and mortality (HR 1.10, 95% CI 1.00–1.22) due to ischemic heart disease [14].
9 Role of Health Surveillance in the Prevention and Early Identification of CVDs
It has been observed that environmental pollution can have significant etiopathogenic implications for CVDs. Since mass screening of the entire population is not feasible, a substantial contribution to the prevention and early identification of pollution-related CVDs can be achieved through health surveillance, autonomously regulated in each country.
In occupational medicine, health surveillance aims to prevent occupational diseases and work-related illnesses, prevent health conditions from deteriorating due to work-related factors, and contribute to preventing workplace injuries. Health surveillance is a crucial preventive measure for workers exposed to health risks (chemical, physical agents, etc.) that may lead to occupational diseases after varying periods of exposure.
In essence, health surveillance assesses the health effects of such exposure, with the goal of adapting preventive measures to individual workers' specific circumstances and verifying the effectiveness of adopted measures, ensuring that exposed individuals do not experience health issues.
The purpose of health surveillance includes: (A) Assessing specific fitness for work; (B) Identifying categories of workers with genetic or acquired hypersusceptibility; (C) Evaluating co-exposures to cumulative and/or synergistic occupational risks on the same target organ; (D) Detecting clinical or preclinical anomalies for early diagnosis; (E) Preventing worsening of workers' health (secondary prevention); (F) Evaluating the efficacy of preventive measures in the workplace; (G) Reinforcing correct work-related measures and behaviours.
Regarding CVDs, there have been few studies investigating the relationship between exposure to environmental pollution and disruptions in the cardiovascular system. Some scientific studies have focused on specific worker categories: an observational study published in 2007 involving 54,000 transport sector workers (more exposed to pollutants) found an increased risk of cardiac pathologies compared to the general population, with a 49% increased risk for truck drivers, 32% for port workers, and 34% for small transporters [15]. Consistently, a report on highway police officers associated particulate matter exposure with heart rate alterations and increased inflammatory markers. Exposure to particulate matter has also been identified as a cause of premature death in two major studies on environmental pollution [16]. Diesel emissions can increase the risk of developing blood clots and stroke. Experimental studies and epidemiological data revealed that the risk more than doubled after 2 hours of exposure to high levels of particulate matter [17, 18].
Given these considerations, it is evident that gaining more information about the effects of environmental pollution, especially on CVDs, is crucial for developing both socioeconomic interventions and public health measures.
Reiterating the potential role of health surveillance, it appears necessary to reconfigure both the risk assessment system (not of medical relevance) and the visit protocol. Particularly noted is the absence of guidelines or specific indications for this specific risk factor in subjects exposed to environmental pollutants. Preventive medical examinations should encompass clinical, instrumental, and laboratory assessments aimed at monitoring not only the potential effects of environmental pollutants but also the presence of biochemical alterations that may have a co-causal or synergistic role in the onset of CV diseases.
To identify symptoms early during the medical visit, the use of structured and standardized questionnaires and rating scales can be employed as tools to identify characteristic symptoms of exposure to pollutants or simultaneous exposure to cigarette smoke. In this regard, the use of questionnaires to assess smoking habits, such as the “Cigarette Dependence Scale” [19], could be useful. This scale exists in two forms: a longer version with 12 questions (CDS-12) and a shorter version with 5 questions (CDS-5). These provide a quantitative, continuous, and unidimensional measure of dependence, with particular attention to the compulsion to smoke, abstinence, locus of control, time management, and the abandonment of other activities. It is always important to remember the role of the competent physician as a point of reference capable of providing support, listening, and assistance to actively counteract such habits. Further investigation into possible indicators is also advisable. Various scientific publications consider Elemental Carbon (EC) to be a reliable indicator of exposure to pollutants, if feasible, seek related work. EC refers to the fraction of atmospheric particulate matter that contains only carbon, not bound to other elements, and its various allotropic forms. It is a fundamental part of particulate matter and can absorb organic compounds such as polycyclic aromatic hydrocarbons (PAHs), oxidized PAHs, nitro-PAHs, and small amounts of sulfates, nitrates, metals, and other trace elements (Table 1).
Thus, health surveillance of workers, especially those exposed to environmental pollutants, can represent a fundamental preventive tool for the development of economic, social, and health policies concerning the entire population. Therefore, it is advisable to: (A) Reconsider occupational risk factors, including environmental pollution as a co-factor in the genesis of cardiovascular diseases, especially for certain categories of workers, (B) Modify and implement the health protocol, including among the standard examinations: (1) Specific questionnaires, including those related to smoking habits; (2) Hematochemical tests, including blood glucose and lipid profile; (3) Electrocardiogram (ECG) and potentially echocardiogram.
Clearly, there is a need for further scientific investigation with the collection of an adequate amount of data for statistical and epidemiological purposes.
10 Legislative Interventions in Italy
There is irrefutable evidence that environmental pollution significantly contributes to the development of CV risk [20], and that decisive action on the environment is necessary to achieve acceptable goals in terms of cardiovascular prevention [21]. This goal can only be achieved through national legislative measures. In this context, in 2010, the Italian government implemented a decree-law (No. 155, dated August 13 in 2010), the Italian government enacted Legislative Decree No. 155, which incorporated the directives of the European Community from 2008 regarding strategies for improving air quality (Table 1). This decree establishes threshold values and emission reduction recommendations for various air pollutants. It sets limit values for ambient air concentrations of sulfur-dioxide, nitrogen-dioxide, benzene, carbon-monoxide, lead, and PM10. Additionally, critical levels for sulfur-dioxide and nitrogen-oxides, alert thresholds for sulfur-dioxide and nitrogen-dioxide, and various objectives and targets for PM2.5, arsenic, cadmium, nickel, and benzo(a)pyrene are defined.
Furthermore, in Italy, Law No. 132 of June 28, 2016, established the "National Network System for Environmental Protection and Regulation of the Higher Institute for Environmental Protection and Research." This system aims to ensure the effectiveness and uniformity of public control over environmental quality in support of environmental sustainability policies and public health prevention.
A report published in 2020 by the National System for Environmental Protection, based on 296 sampling points, revealed that 1.7% of the cases exceeded the annual average PM2.5 limit of 25 μg/m3 set by law. However, this data is not entirely reassuring since the same monitoring indicated that in 77.7% of the cases, the annual average PM2.5 value exceeded the limits recommended by the World Health Organization (WHO), which are 10 μg/m3. In the remaining 20.6% of cases, the PM2.5 concentrations were within the WHO reference values. The regions with the highest PM2.5 concentrations in Italy were Lombardy and Veneto, while Sardinia had the lowest concentration.
It is important to note the discrepancy between the PM2.5 limits imposed by Italian law and the WHO recommendations. The global goal of achieving PM2.5 values of 10 μg/m3 by 2030 is considered a priority by the United Nations for environmental protection.
References
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, Feigin V, Freedman G, Hubbell B, Jobling A, Kan H, Knibbs L, Liu Y, Martin R, Morawska L, Pope CA 3rd, Shin H, Straif K, Shaddick G, Thomas M, van Dingenen R, van Donkelaar A, Vos T, Murray CJL, Forouzanfar MH. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–18. https://doi.org/10.1016/S0140-6736(17)30505-6. (Erratum in: Lancet. 2017 Jun 17;389(10087):e15. Erratum in: Lancet. 2018 Apr 21;391(10130):1576).
IQAir. World Air Quality Report 2019: region and city PM2.5 ranking. 2019.
de Bont J, Jaganathan S, Dahlquist M, Persson Å, Stafoggia M, Ljungman P. Ambient air pollution and cardiovascular diseases: an umbrella review of systematic reviews and meta-analyses. J Intern Med. 2022;291(6):779–800. https://doi.org/10.1111/joim.13467.
Zhang S, Routledge MN. The contribution of PM2.5 to cardiovascular disease in China. Environ Sci Pollut Res Int. 2020;27(30):37502–13. https://doi.org/10.1007/s11356-020-09996-3.
Yue C, Yang F, Wang L, Li F, Chen Y. Association between fine particulate matter and atrial fibrillation in implantable cardioverter defibrillator patients: a systematic review and meta-analysis. J Interv Card Electrophysiol. 2020;59(3):595–601. https://doi.org/10.1007/s10840-020-00864-1.
Cai Y, Zhang B, Ke W, Feng B, Lin H, Xiao J, Zeng W, Li X, Tao J, Yang Z, Ma W, Liu T. Associations of short-term and long-term exposure to ambient air pollutants with hypertension: a systematic review and meta-analysis. Hypertension. 2016;68(1):62–70. https://doi.org/10.1161/HYPERTENSIONAHA.116.07218.
Andreadis EA, Vourkas GI, Varelas G, Angelopoulos ET, Gerasopoulos E, Mihalopoulos N, Thomopoulos C. Air pollution and home blood pressure: the 2021 Athens wildfires. High Blood Press Cardiovasc Prev. 2022;29(6):619–24. https://doi.org/10.1007/s40292-022-00547-0.
Hamanaka RB, Mutlu GM. Particulate matter air pollution: effects on the cardiovascular system. Front Endocrinol (Lausanne). 2018;16(9):680. https://doi.org/10.3389/fendo.2018.00680.
Wold LE, Ying Z, Hutchinson KR, Velten M, Gorr MW, Velten C, Youtz DJ, Wang A, Lucchesi PA, Sun Q, Rajagopalan S. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ Heart Fail. 2012;5(4):452–61. https://doi.org/10.1161/CIRCHEARTFAILURE.112.966580.
Lucking AJ, Lundbäck M, Barath SL, Mills NL, Sidhu MK, Langrish JP, Boon NA, Pourazar J, Badimon JJ, Gerlofs-Nijland ME, Cassee FR, Boman C, Donaldson K, Sandstrom T, Newby DE, Blomberg A. Particle traps prevent adverse vascular and prothrombotic effects of diesel engine exhaust inhalation in men. Circulation. 2011;123(16):1721–8. https://doi.org/10.1161/CIRCULATIONAHA.110.987263.
Cole-Hunter T, Dehlendorff C, Amini H, Mehta A, Lim YH, Jørgensen JT, Li S, So R, Mortensen LH, Westendorp R, Hoffmann B, Bräuner EV, Ketzel M, Hertel O, Brandt J, Jensen SS, Christensen JH, Geels C, Frohn LM, Backalarz C, Simonsen MK, Loft S, Andersen ZJ. Long-term exposure to road traffic noise and stroke incidence: a Danish Nurse Cohort study. Environ Health. 2021;20(1):115. https://doi.org/10.1186/s12940-021-00802-2.
Vienneau D, Saucy A, Schäffer B, Flückiger B, Tangermann L, Stafoggia M, Wunderli JM, Röösli M, SNC study group. Transportation noise exposure and cardiovascular mortality: 15-years of follow-up in a nationwide prospective cohort in Switzerland. Environ Int. 2022;158: 106974. https://doi.org/10.1016/j.envint.2021.106974.
Obayashi K, Saeki K, Iwamoto J, Ikada Y, Kurumatani N. Association between light exposure at night and nighttime blood pressure in the elderly independent of nocturnal urinary melatonin excretion. Chronobiol Int. 2014;31(6):779–86. https://doi.org/10.3109/07420528.2014.900501.
Sun S, Cao W, Ge Y, Ran J, Sun F, Zeng Q, Guo M, Huang J, Lee RS, Tian L, Wellenius GA. Outdoor light at night and risk of coronary heart disease among older adults: a prospective cohort study. Eur Heart J. 2021;42(8):822–30. https://doi.org/10.1093/eurheartj/ehaa846.
Laden F, Hart JE, Smith TJ, Davis ME, Garshick E. Cause-specific mortality in the unionized U.S. trucking industry. Environ Health Perspect. 2007;115(8):1192–6. https://doi.org/10.1289/ehp.10027.
Riediker M, Cascio WE, Griggs TR, Herbst MC, Bromberg PA, Neas L, Williams RW, Devlin RB. Particulate matter exposure in cars is associated with cardiovascular effects in healthy young men. Am J Respir Crit Care Med. 2004;169(8):934–40. https://doi.org/10.1164/rccm.200310-1463OC.
Nemmar A, Hoet PH, Dinsdale D, Vermylen J, Hoylaerts MF, Nemery B. Diesel exhaust particles in lung acutely enhance experimental peripheral thrombosis. Circulation. 2003;107(8):1202–8. https://doi.org/10.1161/01.cir.0000053568.13058.67.
Münzel Yamazaki S, Nitta H, Ono M, Green J, Fukuhara S. Intracerebral haemorrhage associated with hourly concentration of ambient particulate matter: case-crossover analysis. Occup Environ Med. 2007;64(1):17–24. https://doi.org/10.1136/oem.2005.021097.
Etter JF, Le Houezec J, Perneger TV. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology. 2003;28(2):359–70. https://doi.org/10.1038/sj.npp.1300030.
Hahad TO, Sørensen M, Lelieveld J, Duerr GD, Nieuwenhuijsen M, Daiber A. Environmental risk factors and cardiovascular diseases: a comprehensive expert review. Cardiovasc Res. 2022;118(14):2880–902. https://doi.org/10.1093/cvr/cvab316.
Capua I, Piccolo E. Evolving landscapes driving cardiovascular diseases require a Circular Health approach. Eur Heart J. 2023;44(2):77–9. https://doi.org/10.1093/eurheartj/ehac593.
Acknowledgements
The authors are grateful to Federica De Luise for her assistance with manuscript preparation.
Funding
Open access funding provided by Università degli Studi di Napoli Federico II within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None
Conflict of interest
None of the authors report a conflict of interest to disclose on the content of the present manuscript.
Author contributions
Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content and they agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ghazihosseini, S., De Rosa, C., Trimarco, V. et al. The Environmental Pollution and Cardiovascular Risk: The Role of Health Surveillance and Legislative Interventions in Cardiovascular Prevention. High Blood Press Cardiovasc Prev 30, 533–538 (2023). https://doi.org/10.1007/s40292-023-00612-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-023-00612-2