Abstract
Sickle cell disease (SCD) is one of the most common inherited hemoglobinopathy disorders that affects millions of people worldwide. Reactivation of HBG (HBG1, HBG2) gene expression and induction of fetal hemoglobin (HbF) is an important therapeutic strategy for ameliorating the clinical symptoms and severity of SCD. Hydroxyurea is the only US FDA-approved drug with proven efficacy to induce HbF in SCD patients, yet serious complications have been associated with its use. Over the last three decades, numerous additional pharmacological agents that reactivate HBG transcription in vitro have been investigated, but few have proceeded to FDA approval, with the exception of arginine butyrate and decitabine; however, neither drug met the requirements for routine clinical use due to difficulties with oral delivery and inability to achieve therapeutic levels. Thus, novel approaches that produce sufficient efficacy, specificity, and sustainable HbF induction with low adverse effects are desirable. More recently, microRNAs (miRNAs) have gained attention for their diagnostic and therapeutic potential to treat various diseases ranging from cancer to Alzheimer’s disease via targeting oncogenes and their gene products. Thus, it is plausible that miRNAs that target HBG regulatory genes may be useful for inducing HbF as a treatment for SCD. Our laboratory and others have documented the association of miRNAs with HBG activation or suppression via silencing transcriptional repressors and activators, respectively, of HBG expression. Herein, we review progress made in understanding molecular mechanisms of miRNA-mediated HBG regulation and discuss the extent to which molecular targets of HBG might be suitable prospects for development of SCD clinical therapy. Lastly, we discuss challenges with the application of miRNA delivery in vivo and provide potential strategies for overcoming barriers in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Experimental data support the association of microRNAs (miRNAs) with HBG activation or suppression via silencing transcriptional repressors and activators, respectively, of HBG expression. |
The clinical utility of miRNAs involved in reactivation of HBG, potential off-target adverse effects, and specificity and sustainability for fetal hemoglobin (HbF) induction in vivo requires further investigation. |
Strategies for overcoming barriers in miRNA delivery are needed for the development of HbF-inducing therapeutics for SCD. |
1 Introduction
Sickle cell disease (SCD) is a group of common inherited hemoglobin disorders that affects millions of people worldwide, including more than 100,000 African Americans in the US [1]. Homozygous hemoglobin S (HbSS) and HbSβ0thalassemia or sickle cell anemia (SCA) are the most common and clinically severe phenotypes observed [1]. SCA is caused by a single amino acid base substitution (β6Glu > Val) in the β-globin gene (HBB), which produces abnormal sickle hemoglobin (HbS) [2, 3]. Disease severity and the clinical manifestations observed in SCD vary greatly in people with SCA, who experience more severe complications compared with other genotypes. These complications are often due to repetitive vaso-occlusive crises under hypoxic conditions that can lead to stroke, organ damage, and early death [4, 5].
Reactivation of HBG (HBG1, HBG2) gene expression and induction of fetal hemoglobin (HbF) is an important therapeutic strategy in SCD since an increase in the percentage of HbF inhibits polymerization of HbS molecules and ameliorates clinical severity. Historical data suggest that individuals with HbF levels >20% have fewer recurrent clinical events, such as crises or pulmonary complications and stroke [6]. A more recent clinical study by Estepp et al. supports the use of hydroxyurea (HU) in children with SCD, with the preferred dosing strategy targeting an HbF endpoint >20% to reduce clinical complications and hospitalizations [7]. Individuals with naturally occurring hereditary persistence of HbF variants have significantly higher HbF levels in the majority of their red blood cells (pancellular) producing benign clinical phenotypes. Thus, to achieve maximal clinical benefit, it is also critical that therapeutic agents produce a pancellular distribution of HbF.
To date, HU has been the only US FDA-approved drug with efficacy to induce HbF in SCA patients, yet serious complications have been associated with its use [8]. Over the last three decades, numerous additional pharmacological agents to reactivate HBG transcription have been investigated but few have proceeded to clinical trials, except arginine butyrate and decitabine; however, neither of these two drugs met requirements for routine clinical use due to difficulties with oral delivery and inability to achieve efficacious levels. Thus, therapeutic interventions that demonstrate sufficient efficacy, specificity, and sustainability for HbF induction with low adverse effects are desirable to mitigate the clinical complications observed in SCD patients.
Genetic mapping and genome-wide association studies discovered genetic loci in B-cell lymphoma/leukemia 11A (BCL11A), an Xnm1 variant upstream of hemoglobin subunit gamma 1 (HBG1), and the HBS1L-MYB intergenic region, which account for 20–50% of the common variation in HbF levels observed in SCA patients [9,10,11,12,13]. An investigation into the C > T genetic variant in XmnI (rs7482144), which is located at −158 upstream of the HBG1 gene, revealed a significant correlation of this variant with disease severity in adults with β-thalassemia [10]. In addition to the identification of genetic risk loci with HbF-modulating capabilities, a complex comprising of DNA-binding proteins, including GATA1, TAL1, E2A, LMO2, LRF/ZBTB7A, and LDB1 among others, have been shown to silence HBG transcription during hemoglobin switching by mediating DNA looping between the locus control region (LCR) and each globin promoter sequentially [14, 15]. Similarly, DNA hypomethylation and histone hyperacetylation of the HBG proximal promoter have been effective in inducing gene expression [16, 17] and have been associated with high levels of HbF [18]. Supporting studies reported that hemoglobin switching is controlled through the activity of epigenetic modulators such as BCL11A, KLF1, and HBS1L-MYB [19,20,21,22]. Collectively, these findings support molecular approaches to target genetic loci and/or their HBG-modifying transcripts and proteins to induce HbF to reduce the clinical complications of SCD.
Over the last decade, mounting evidence has highlighted the association of microRNAs (miRNAs) with HBG activation or suppression via transcriptional repressor proteins and transactivators, respectively, of HBG expression [23,24,25]. miRNAs are endogenous small RNAs that are naturally expressed at varying levels in mammalian tissues [26]. Since the emergence of the role of miRNAs in regulating distinct processes in mammalian cells, their applicability as a novel class of therapeutics for targeted gene expression in various human diseases, especially cancer, has been extensively explored and proven quite beneficial [27,28,29,30]. Moreover, due to their limited size, conservation among species, and capacity to disrupt expression of target genes, miRNAs are attractive therapeutic candidates for targeting gene expression in common mammalian diseases [31, 32].
Despite their high therapeutic potential, there are major concerns with the clinical utility of miRNAs due to off-target adverse effects. miRNAs function through imperfect base pairing to complementary regions of their target messenger RNA (mRNA) molecules and often produce downregulation of target gene expression, resulting in translational repression, mRNA cleavage, and deadenylation [33, 34]. However, the ability of a single miRNA to alter the expression of multiple genes and pathways, many of which may activate oncogenes or downregulate tumor suppressor genes [35], is an Achilles Heel when considering the development of miRNA-based interventions. Another concern is the lack of knowledge and uncertainty as to whether modulation of miRNAs will produce sufficient efficacy, specificity, and sustainability for HbF induction in vivo. In this review, we propose to discuss the involvement of miRNAs in HBG gene regulation and critically assess the extent to which direct or indirect targeting of HBG expression by miRNAs might be a suitable prospect for therapeutic development for SCD. Lastly, we discuss challenges with the application of miRNA delivery in vivo and provide strategies for overcoming barriers in miRNA delivery.
2 Background on MicroRNAs
In 1993, miRNAs were first discovered as the product of the heterochronic lin-4 gene in C. elegans [36, 37]. They are small (~22 nucleotides), endogenous nonprotein-coding RNA molecules that interact with the miRNA-induced silencing complex (mRISC) to silence gene-specific mRNA in the cytoplasm [38]. miRNAs facilitate mRNA degradation and gene silencing by base-pairing with complementary sequences in the 3′-untranslated regions (3′UTR) of target mRNA [26, 39]. According to the miRBase database, release 22 (accessed January 2022), more than 38,000 mature miRNAs have been discovered [40]. Each miRNA produced potentially regulates the expression of hundreds of genes. In addition, a single transcript can be targeted by more than one miRNA to alter the expression of genes in the same pathway [40, 41]. Therefore, miRNAs have been widely investigated since discovery, evidenced by more than 126,900 published studies on miRNAs indexed in PubMed.
Since discovery, development of miRNA-based therapeutics for a wide variety of diseases, ranging from cancer to Alzheimer’s disease, has erupted. More recently, studies have examined an association between miRNAs in peripheral blood of several diseases, including neurodegenerative disorders, Alzheimer’s disease, and cancer [42,43,44,45]. Several miRNAs are abundant in erythroid cells and function as critical regulators of hematopoiesis, including miR-15a/16, miR-144, miR-150, miR-191, and miR-221/222 [46]. Supporting studies reported expression of genes targeted by differentially expressed miRNAs in fetal versus adult erythroid progenitor cells, including the let-7 miRNA family [47, 48]. These findings justify further investigations into the therapeutic potential of miRNAs involved in HBG gene regulation during adult erythropoiesis.
3 Targeting of HBG Transcriptional Regulators by miRNAs, Activation of HBG Expression, and Induction of Fetal Hemoglobin
3.1 EKLF/KLF1
The first major transcription factor identified to play a key role in adult HBB gene activation during hemoglobin switching was Erythroid Krüppel-like factor (EKLF/KLF1) [49]. Subsequent studies provided further evidence that KLF1 is a major player in controlling HBG-to-HBB gene switching by activating BCL11A [21], which indirectly represses HBG transcription [50,51,52,53]. More recently, Li et al found that miR-326 suppressed KLF1 expression directly by targeting its 3′UTR and activated HBG expression in K562 cells and CD34+ hematopoietic progenitor cells (Fig. 1, Table 1) [54]. By overexpressing miR-326 in K562 cells, KLF1 protein reduced and HBG expression increased approximately 50%. Moreover, miR-326 expression was positively correlated with HbF levels in β-thalassemia patients, but it is unknown whether miR-326 induces HbF in CD34+ hematopoietic progenitor cells. Obeidi et al. showed that miR-451 upregulation correlated with the induction of several transcription factors, including KLF1, and promoted erythroid differentiation in murine embryonic stem cells [55]. It is unknown whether miR-451 upregulation silences HbF expression during erythroid differentiation in murine embryonic stem cells. A study by Pule et al. found that ex vivo HU treatment of differentiated primary erythroid cells from seven unrelated individuals and of K562 cells significantly downregulated KLF1, which corresponded nicely to decreased expression of BCL11A and increased HBG gene expression [56]. Several miRNAs, specifically miR-15a, miR-16, miR-26b and miR-151-3p, were induced following HU treatment in both cell models [56]. Published studies by our group found that miR-34a promoted cell differentiation by increasing expression of KLF1, glycophorin A, and the erythropoietin receptor while silencing STAT3 [57], a known repressor of HBG in K562 cells (Table 1) [58]. Additional investigations to understand the role of miRNAs in regulating HBG expression and inducing HbF through targeting KLF1 in vivo are needed.
Effect of miRNAs and transcription factors on fetal globin gene expression during hemoglobin switching. Shown is the HBB gene locus on chromosome 11, which consists of a locus control region with hypersensitive sites and the five developmentally regulated globin genes, including HBE (purple), fetal HBG1 and HBG2 (brown), HBD (blue), and adult HBB (orange). Silencing of HBG genes is mediated by transcriptional repressors, such as MYB, which activates KLF1, and which in turn activates the repressor BCL11A, which mediates transcriptional silencing of HBG. STAT3 inhibits HBG while KLF1 activates HBB. The HBG promoters become hypermethylated and silenced by DNA methylation. The DNMT3 proteins, DNMT3A and DNMT3B, are required for long-term methylation and silencing of the HBG gene promoters during adult erythropoiesis. MiR-29b, a DNMT3 inhibitor, also inhibits MYB expression, resulting in HBG activation. Several miRNAs have been shown to activate or inhibit HBG expression. miRNAs shown to inhibit (red line) or induce (green line) HBG expression via their target gene(s) are shown. DNMT DNA methyltransferase, BCL11A B-cell lymphoma 11A, HSs hypersensitive sites, KLF1 Krüppel-like factor 1, KLF3 Krüppel-like factor 3, LCR locus control region, miR microRNA, MYB MYB proto-oncogene, transcription factor
3.2 BCL11A
The BCL11A gene encoding a C2H2-type zinc finger protein is a major transcriptional repressor of HBG expression during adult erythropoiesis [19, 59]. Inherited genetic variants in BCL11A associated with HbF levels in hemoglobinopathy patients [60] provided the catalyst for laboratory studies confirming BCL11A as a major silencer of HBG gene expression. Table 1 highlights those miRNAs, including miR-451, which target BCL11A and influence HBG gene expression [25, 61, 62].
Other miRNAs besides miR-144 influence HbF levels via targeting BCL11A in vitro. For example, Gholampour et al. observed miR-30a expression correlated with higher HbF levels in erythroid precursors isolated from β-thalassemia intermedia patients [63]. Subsequent studies confirmed the role of miR-30a in silencing BCL11A in erythroid precursors and inducing HBG expression [63]. A similar study was conducted in the Democratic Republic of Congo in which 22 of 798 miRNAs were differentially expressed in peripheral blood of adult SCD patients receiving HU [64]. Interestingly, in that study several miRNAs, including miR-148b-3p, miR-32-5p, miR-340-5p, and miR-29c-3p were associated with silencing BCL11A (Fig. 1) [64]. Functional studies in K562 cells showed that healthy-donor exosomes and miR-138-5p regulated HBG expression by targeting BCL11A [43]. Lee et al. observed that suppression of let-7, which targets LIN28B, also reduced BCL11A expression and significantly induced HbF in adult human erythroblasts [65]. MiR-486-3p was also found to silence BCL11A and activate HBG in erythroid cells [66]. Future studies are needed to determine whether these miRNAs that target BCL11A will produce similar effects in preclinical sickle cell mouse models.
One of the earliest studies to implicate miRNAs in HbF induction by HU was published by Lopes et al. [67]. The authors observed a significant decrease in HIF1A expression, a marker of angiogenesis, and induction of miR-221, in human umbilical vein endothelial cell cultures following HU treatment in vitro [67]. Specifically, miR-210 and miR-486-3p were associated with increased HBG expression in HU responders [68]. A separate study by Sawant et al. further supported a role for miR-210 in erythroid differentiation and HbF induction in SCD patients receiving HU therapy [69].
3.3 c-MYB (MYB)
MYB is a well-characterized proto-oncogene [70] that plays an indirect role in silencing HBG transcription through targeting BCL11A and the repressor TR2/TR4 [52, 71]. MYB expression is high in immature hematopoietic cells but is downregulated during erythropoiesis [72]. Supporting studies showed that overexpression of MYB inhibited HBG expression in K562 cells [70], while silencing MYB induced HbF expression in primary human erythroid progenitors [73]. In human genetic studies, the association of MYB with HbF levels was demonstrated using quantitative trait loci studies and subsequent functional assays as previously described [10, 70, 73]. Later studies would provide evidence that MYB is a direct target of the tumor suppressor miR-15a/16 cluster (Table 1) [74]. Supporting data by Sankaran et al. showed that the higher expression of HbF observed in trisomy 13 subjects was due to increased expression of miR-15a and miR-16-1 [73]. In that study, miR-15a decreased MYB protein expression by inhibiting mRNA translation [73].
In contrast, Kouhkan et al. did not observe an effect of miR-16 on HBG expression in CD133+ stem cells [75]. Furthermore, miR-26b was shown to directly interact with the 3′UTR of MYB and induce HbF in both erythroid progenitors and K562 cells [56]. Our published findings also provide evidence that overexpression of miR-29b significantly decreased MYB protein expression in KU812 cells [24], which suggests that MYB may be a potential target of miR-29b (Fig. 1). A previously described study that was conducted in the Democratic Republic of Congo in which 22 of 798 differentially expressed miRNAs were identified in peripheral blood of adult SCD patients receiving HU further showed that miR-105-5p was associated with silencing MYB [64]. Collectively, these studies highlight the ability of multiple miRNAs to fine-tune expression of MYB and influence HBG expression and HbF levels.
3.4 MiRNAs Involved in HBG Suppression
In contrast to miRNAs related to HbF induction, fewer have been associated with HBG gene suppression. To date, one miRNA has been shown to directly inhibit HBG mRNA, namely miR-96 [76]. Azzouzi et al. compared mRNA from reticulocytes of cord and adult blood and demonstrated miR-96 is highly expressed in adults [76]. When miR-96 was overexpressed in erythroid progenitors, HBG mRNA decreased 50% (Fig. 1). In luciferase-based studies, miR-96 directly inhibited HBG cDNA by targeting the open reading frame sequence [76]. In contrast, miR-223-3p suppressed HBG expression in β-thalassemia major exosomes by inhibiting the transcription factor LMO2 [77]. During erythropoiesis, miR-150 inhibits GATA1, which has been associated with HBG suppression in K562 cells [78]. Similarly, miR-23a and miR-27a enhance the expression of β-like globin genes by inhibiting KLF3 and SP1 binding to the β-like globin gene locus during erythroid differentiation [79]. A purified component of a natural Chinese medicine called emodin activates HBG expression in K562 cells through upregulation of c-KIT and downregulation of miR-221 and miR-222 [80].
miR-144 is one of the predominant miRNAs in peripheral blood erythrocytes that controls oxidative stress levels by suppressing NRF2 (nuclear factor erythroid 2-related factor) expression. A study by Sangokoya et al. showed that miR-144 was important in hemoglobin synthesis and SCD clinical severity [62]. Using prediction analysis of microarray to prioritize differentially expressed miRNAs, they further observed significantly higher expression levels of miR-144, miR-451, and miR-142-5p among erythrocytes isolated from adult SCD patients with severe anemia compared with normal erythrocytes [62]. In the same study, miR-144 directly targeted the 3′UTR of NRF2, a well-known transcription factor that modulates oxidative stress response, in K562 cells (Table 1) [62]. It is well documented that NRF2 directly activates HBG transcription while miR-144 targets NRF2 to silence HBG mRNA in normal CD34+ cells. Reversely, inhibiting miR-144 upregulates HBG in normal and sickle cell progenitors [25, 81]. Supporting studies from our group further showed that silencing of NRF2 by miR-144 significantly repressed HBG gene transcription twofold in normal erythroid progenitors while the miR-144 antagomir increased the percentage of F cells twofold in sickle erythroid progenitors [25].
3.5 HBG Regulation by DNA Methylation
DNA methylation is a critical epigenetic process that contributes to erythroid cell differentiation and hemoglobin switching mechanisms [82,83,84]. During developmentally regulated erythroid cell differentiation, the globin genes (5-′HBE, HBG1, HBG2, HBD, HBB-3′) in the HBB globin locus become sequentially demethylated and transcriptionally active. During adult erythropoiesis, the HBG gene promoter becomes hypermethylated and silenced by DNA methylation machinery, including DNMT3A, DNMT3B, DNMT1, and the MBD protein family [82, 85,86,87,88,89]. Thus, strategies to reverse HBG promoter hypermethylation and induce HbF have resulted in the development of pharmacologic DNMT inhibitors, particularly decitabine and 5-azacytidine, which reactivate HBG expression via hypomethylation of the CpG site within the HBG proximal promoter. Although decitabine and 5-azacytidine are potent HbF-inducing agents that impair de novo methylation activity, oral administration leads to rapid degradation by intestinal cytidine deaminases [90, 91] and there are concerns with possible adverse side effects [92], such as increased risk of hyperglycemia, neutropenia/leukopenia, and electrolyte imbalance. Thus, miRNAs, which are naturally found in the human body and that target genes involved in DNA methylation, resulting in an increase in HBG expression, may be an effective approach to address the clinical concerns raised by chemically induced DNA demethylation in general.
In our group, we took an alternative approach to discover miRNAs that target the DNA methylation machinery during hemoglobin switching. We initially conducted a genome-wide unbiased miRNA screen during switching in reticulocytes to identify miRNA expression patterns [25]. We collected blood samples from patients with confirmed HbSS genotype and contrasting HbF levels that ranged from 0.1% to 30.6%. SCD patients were separated into two groups based on their mean HbF levels: low HbF levels (average HbFLOW = 3.37 ± 1.02) versus high-HbF (average HbFHIGH = 23.48 ± 2.12). RNA was isolated from purified reticulocytes for microarray-based miRNA expression profiling. Following the miRNA screen, we identified an eightfold upregulation of miR-144 in the low-HbF group compared with those with high HbF levels [25]. We next discovered that miR-29b expression was associated with higher HbF levels [24], demonstrating the first evidence for a role of miR-29b as a DNA methyltransferase inhibitor to mediate HbF induction [24]. Subsequently, we observed that overexpression of miR-29b significantly increased the percentage of HbF-positive cells, while decreasing the expression of DNMT3A and MYB in human KU812 cells and primary erythroid progenitors (Fig. 1) [24].
These studies expand our previous findings showing that miR-29b has a complementary seed sequence with the 3′UTR of DNMT3A and DNMT3B, thereby inhibiting de novo DNMT synthesis in breast cancer cells [93]. Similar work by Walker et al. investigated the role of epigenetic mechanisms, specifically HBG promoter methylation levels and miRNA expression, on HbF induction in primary CD71+ erythrocytes of SCD patients before HU therapy and after reaching a maximum tolerated dose of HU therapy [94]. Their findings showed that expression of miR-26b and miR-151-3p known to target KLF1 were both associated with HbF levels at a maximum tolerated HU dose in SCD [94]. These findings highlight the importance for further investigation of the miR-29 family and other miRNAs in HBG regulation.
In support of these findings and the importance for targeting DNA methylation machinery, our group and others have shown that methyl CpG binding protein 2 (MeCP2) and/or other MBD proteins are involved in HBG regulation in adult erythroid progenitors [24, 95]. Considering epigenetic modifications, including acetylation and methylation, influence DNA looping of the LCR and access of transacting DNA-binding proteins at each globin promoter, it is plausible that targeting epigenetic pathways via miRNAs may enhance HBG gene transcription.
4 Overcoming Hurdles in miRNA Delivery
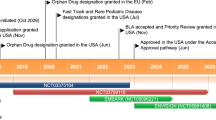
MiRNAs are attractive molecules for inhibiting repressors of HBG gene transcription and inducing HbF. In 2018, the FDA approved the first-of-its-kind targeted RNA interference (RNAi)-based therapy, ONPATTRO (patisiran) infusion, to treat peripheral nerve disease caused by hereditary transthyretin-mediated amyloidosis in adult patients [96]. Currently, 11 RNA-based therapeutics have been approved by the FDA and/or the European Medicines Agency [27]. These RNA-based therapies are delivered intravenously, intrathecally, or via subcutaneous administration to treat various diseases of the eye, muscle, or the central nervous system [27]. Recently, the FDA approved an emergency use authorization for the Moderna Vaccine (mRNA-1273) to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in individuals 12 years of age and older [97]. In addition to these RNA-based therapies, a substantial number of RNA therapeutics are in phase II or III clinical development, such as various anti-miRs and miRNA mimics [27], including a cholesterol-conjugated miR-29 mimic for skin keloid (NCT02603224, NCT03601052).
Despite the potential of RNA-based agents as therapeutic interventions, there are major concerns among the scientific community about the unwanted off-target effects mediated by miRNAs, or that straining the RNAi system may alter expression of multiple target genes [98,99,100]. However, miRNAs can potentially restore expression of proteins at physiological levels as previously documented [98,99,100], which is a major goal when considering the development of HbF-inducing therapeutics.
In addition to these concerns, critical hurdles involving delivery of miRNA-targeting agents remains a challenge for clinical translation [101]. Limitations to overcome delivery include, but are not limited to, poor in vivo stability and short half-life under physiological conditions, inappropriate biodistribution and degradation by ribonuclease enzymes, unfavorable immune response, and undesirable off-target effects, as previously described [101,102,103]. Thus, an appropriate carrier system and/or chemical modifications to overcome these limitations is critical to developing safe and effective miRNA-targeted therapeutics. Below, we briefly highlight promising platforms demonstrated to provide safe and targeted small-interfering RNA delivery in vivo.
5 Progress in the Development of miRNA Delivery Systems
5.1 Lipid-Based Vectors
Over the last 2 decades, the development of cationic liposome/lipid-based systems has seen a rapid expansion after initial description by Felgner et al. in 1987, who described the first successful in vitro transfection with a cationic lipid [104]. Since that time, a large number of commercially available cationic liposome/lipid-based systems, such as Lipofectamine and TransIT TKO, Oligofectamine, Lipofectin, DOTAP and RNAifect, have been developed [105,106,107,108,109]. A major advantage for using liposomes is their flexible physicochemical and biophysical properties, which allows manipulation for different delivery considerations [110]. For instance, adding cholesterol modifiers and/or polymers, such as 1,2-Dioleoyl-sn-glycero-3-phosphoethanolamine (DOPE) and polyethylene glycol (PEG), to liposomes has reduced inflammatory responses and enhanced the stability of the liposomes and cellular uptake, allowing for more effective delivery and hepatic clearance in vivo [111]. Introducing helper cationic polymers in the formulation has been further shown to increase the siRNA entrapment inside the liposome core [112]. Adding functional lipid groups, such as –COOH or –NH2, at the distal terminal of polymers further assists with controlling pH and allows for easier linking with its target ligands [113]. Several cholesterol-conjugated small-interfering RNAs have advanced to clinical evaluation, such as RXI-109, SNALP®, and Atuplex, based on the ability to promote effective cellular uptake [114].
5.2 Nanoparticle-Based miRNA Delivery
To date, nanotechnology-based delivery systems are considered one of the most promising and exciting tools for precision medicine due to their ability to control the release of drugs and successful delivery in vivo [101, 115]. Nanoparticles are at the atomic or molecular level, with sizes ranging between 1 and 100 nm in diameter [116, 117]. Their small size is a major advantage, allowing them to move freely in the human body even when encapsulated or attached to therapeutic drugs that need to be delivered to target tissue sites [116, 117]. For instance, nanoparticle-based methods have been used to distinguish between healthy cells and cancer cells even when combined with chemotherapy and imaging modalities for cancer diagnosis [118,119,120]. Several small elements, such as gold, bismuth, and silver, have also been used as biomarkers for various molecular biology detection assays, and for magnetic, optical, and X-ray detection systems [121,122,123]. Other nanoparticle systems, such as the Rondel® platform, which uses the electrostatic force of attraction between negatively charged molecules and the positively charged linear polymer with alternate cyclodextrin molecules, has also been used to deliver small molecules [124].
5.3 Viral Vectors for miRNA Delivery
Viral-based delivery systems use retroviruses, lentiviruses, and adenoviruses or adeno-associated viruses (AVV) to deliver small molecules, including miRNAs, into somatic and germline cells [125, 126]. Viral vectors, especially AAV vectors, are more frequently utilized in delivering miRNAs due to the small size of miRNAs. This system enhances transfection efficiency and increased expression of miRNAs. A disadvantage of using viral vectors is their tendency to induce toxicity, inflammation, and immunogenicity caused by the inserted sequence [125, 127]. However, the development of the first-in-human lentiviral system targeting BCL11A (BCH-BB694 BCL11A shmiR) supported a phase I clinical trial for SCD patients (ClinicalTrials.gov identifier NCT03282656) [128, 129]. This open-label, nonrandomized, single-center, single-arm cohort study involved a single intravenous infusion of transduced CD34+ HSC cells containing a lentiviral vector encoding an shRNA targeting BCL11A mRNA embedded in an miRNA molecule that was evaluated in seven SCD patients [128]. Although adverse side effects (including pain, influenza, infection, priapism, and fever) were observed, individuals evaluated 6–24 months following infusion achieved robust and stable induction of HbF. Specifically, the median percentage of F cells among untransfused erythrocytes was 70.8%, which represented a substantial increase from baseline [128]. Of note, none of the patients evaluated had episodes of vaso-occlusive crises, stroke, or acute chest syndrome, which are common complications of SCD leading to emergency department visits and hospitalizations [130]. These findings warrant additional studies to determine the effect of vector-based targeting of other major HBG-modifying genes, such as BCL11A, MYB, KLF1, or other genes. However, there remains a considerable amount of concern with the clinical use of viral-based vectors due to their potential to increase risk of immunogenicity and insertional mutagenesis that needs to be addressed in future studies [131, 132].
6 Conclusions
For several years, miRNA-based targeted therapeutics have shown promise for the treatment of many diseases, by targeting multiple genes and pathways involved in oncogenesis and/or tumor suppression. Several genes, such as MYB, BCL11A, KLF1, and NRF2 are not only involved in oncogenesis or other biological processes but are also involved in HBG gene silencing. Supporting studies discussed in this review have shown the ability of various miRNAs to regulate HBG expression by activating or suppressing gene expression. Thus, identifying miRNAs associated with HBG activation or repression, such as MYB, BCL11A, KLF1, and NRF2, or other HBG repressor proteins, is critical for understanding the molecular mechanisms leading to HbF induction and reduced adverse effects in patients with SCD and other β-hemoglobinopathies.
Although there remains an unmet need to develop novel classes of drugs that are efficacious for HbF induction with limited adverse effects, utilizing miRNAs to target genes involved in HBG gene regulation shows promise. However, there are concerns with the implementation of miRNA-based interventions since they may alter the expression of genes involved in oncogenesis or tumor suppression. For instance, there are many miRNA signatures associated with cancer and progression but there is no consensus among multiple sera and tumor sample studies. As such, this is also a concern when considering how to ensure that multiple genes and their protein products are not altered when targeted by one or multiple miRNAs, resulting in unwarranted off-target adverse effects. Indeed, off-target and immunological effects remain an obstacle when considering the use of miRNAs as novel therapeutics. However, a major advantage for the use of miRNAs is that they can potentially restore expression of proteins, such as HbF, at physiological levels.
The challenge that remains with the utilization of miRNA molecules is the development of optimal drug delivery systems to prevent degradation in the blood. Recent developments in nanotechnology and drug delivery systems that target the tumor microenvironment may provide an alternative therapeutic approach with decreased toxicity. Thus, to overcome this hurdle, it is necessary for investigators to include studies utilizing in vivo rodent animal models to evaluate the carcinogenic potential of miRNAs. There is a significant need to reduce the cost of chemical induction of miRNAs and miRNA-based applications for targeted delivery in SCD. Another concern is the lack of knowledge and uncertainty as to whether modulation of miRNAs, both chronically and systemically, will produce sufficient efficacy, specificity, and sustainability for HbF induction in vivo. Nonetheless, the remarkably successful clinical trial and development of BCH-BB694 gene therapy (Bluebird Bio, Cambridge, MA, USA) highlights the potential for developing miRNA as a therapeutic approach to treat SCD. However, a principal factor to consider, in addition to HbF levels, is the distribution of HbF in red blood cells (F cells) to achieve clinical efficacy. Indeed, the potential to develop miRNAs that directly activate HBG by indirect pathways, such as epigenetic mechanisms and/or silencing the BCL11A, MYB, KLF1 genes, provide new strategies to develop small molecules to increase HbF during adult development for the successful treatment of SCD. In conclusion, investigations to define the role of miRNAs in globin gene regulation and their ability to promote robust and stable HbF induction within preclinical SCD animal models to justify future clinical trials are needed.
References
Weatherall DJ. The role of the inherited disorders of hemoglobin, the first “molecular diseases,” in the future of human genetics. Annu Rev Genomics Hum Genet. 2013;14:1–24. https://doi.org/10.1146/annurev-genom-091212-153500.
Rees DC, Gibson JS. Biomarkers in sickle cell disease. Br J Haematol. 2012;156(4):433–45. https://doi.org/10.1111/j.1365-2141.2011.08961.x.
Stuart MJ, Nagel RL. Sickle-cell disease. Lancet. 2004;364(9442):1343–60. https://doi.org/10.1016/S0140-6736(04)17192-4.
Gill FM, Sleeper LA, Weiner SJ, Brown AK, Bellevue R, et al. Clinical events in the first decade in a cohort of infants with sickle cell disease. Cooperative study of sickle cell disease. Blood. 1995;86(2):776–83.
Vichinsky EP, Styles LA, Colangelo LH, Wright EC, Castro O, et al. Acute chest syndrome in sickle cell disease: clinical presentation and course. Cooperative study of sickle cell disease. Blood. 1997;89(5):1787–92.
Powars DR, Weiss JN, Chan LS, Schroeder WA. Is there a threshold level of fetal hemoglobin that ameliorates morbidity in sickle cell anemia? Blood. 1984;63(4):921–6.
Estepp JH, Smeltzer MP, Kang G, Li C, Wang WC, et al. A clinically meaningful fetal hemoglobin threshold for children with sickle cell anemia during hydroxyurea therapy. Am J Hematol. 2017;92(12):1333–9. https://doi.org/10.1002/ajh.24906.
Agrawal RK, Patel RK, Shah V, Nainiwal L, Trivedi B. Hydroxyurea in sickle cell disease: drug review. Indian J Hematol Blood Transfus. 2014;30(2):91–6. https://doi.org/10.1007/s12288-013-0261-4.
Galarneau G, Palmer CD, Sankaran VG, Orkin SH, Hirschhorn JN, et al. Fine-mapping at three loci known to affect fetal hemoglobin levels explains additional genetic variation. Nat Genet. 2010;42(12):1049–51. https://doi.org/10.1038/ng.707.
Thein SL, Menzel S, Peng X, Best S, Jiang J, et al. Intergenic variants of HBS1L-MYB are responsible for a major quantitative trait locus on chromosome 6q23 influencing fetal hemoglobin levels in adults. Proc Natl Acad Sci USA. 2007;104(27):11346–51. https://doi.org/10.1073/pnas.0611393104.
Menzel S, Garner C, Gut I, Matsuda F, Yamaguchi M, et al. A QTL influencing F cell production maps to a gene encoding a zinc-finger protein on chromosome 2p15. Nat Genet. 2007;39(10):1197–9. https://doi.org/10.1038/ng2108.
Uda M, Galanello R, Sanna S, Lettre G, Sankaran VG, et al. Genome-wide association study shows BCL11A associated with persistent fetal hemoglobin and amelioration of the phenotype of beta-thalassemia. Proc Natl Acad Sci USA. 2008;105(5):1620–5. https://doi.org/10.1073/pnas.0711566105.
Lettre G, Sankaran VG, Bezerra MA, Araujo AS, Uda M, et al. DNA polymorphisms at the BCL11A, HBS1L-MYB, and beta-globin loci associate with fetal hemoglobin levels and pain crises in sickle cell disease. Proc Natl Acad Sci USA. 2008;105(33):11869–74. https://doi.org/10.1073/pnas.0804799105.
Love PE, Warzecha C, Li L. Ldb1 complexes: the new master regulators of erythroid gene transcription. Trends Genet. 2014;30(1):1–9. https://doi.org/10.1016/j.tig.2013.10.001.
Breda L, Motta I, Lourenco S, Gemmo C, Deng W, et al. Forced chromatin looping raises fetal hemoglobin in adult sickle cells to higher levels than pharmacologic inducers. Blood. 2016;128(8):1139–43. https://doi.org/10.1182/blood-2016-01-691089.
Ahmadvand M, Noruzinia M, Fard AD, Zohour MM, Tabatabaiefar MA, et al. The role of epigenetics in the induction of fetal hemoglobin: a combination therapy approach. Int J Hematol Oncol Stem Cell Res. 2014;8(1):9–14.
Zhao Q, Rank G, Tan YT, Li H, Moritz RL, et al. PRMT5-mediated methylation of histone H4R3 recruits DNMT3A, coupling histone and DNA methylation in gene silencing. Nat Struct Mol Biol. 2009;16(3):304–11. https://doi.org/10.1038/nsmb.1568.
Bao X, Zuo Y, Chen D, Zhao C. DNA methylation patterns of beta-globin cluster in beta-thalassemia patients. Clin Epigenetics. 2020;12(1):187. https://doi.org/10.1186/s13148-020-00987-2.
Sankaran VG, Menne TF, Xu J, Akie TE, Lettre G, et al. Human fetal hemoglobin expression is regulated by the developmental stage-specific repressor BCL11A. Science. 2008;322(5909):1839–42. https://doi.org/10.1126/science.1165409.
Stadhouders R, Aktuna S, Thongjuea S, Aghajanirefah A, Pourfarzad F, et al. HBS1L-MYB intergenic variants modulate fetal hemoglobin via long-range MYB enhancers. J Clin Invest. 2014;124(4):1699–710. https://doi.org/10.1172/JCI71520.
Zhou D, Liu K, Sun CW, Pawlik KM, Townes TM. KLF1 regulates BCL11A expression and gamma- to beta-globin gene switching. Nat Genet. 2010;42(9):742–4. https://doi.org/10.1038/ng.637.
Morrison TA, Wilcox I, Luo HY, Farrell JJ, Kurita R, et al. A long noncoding RNA from the HBS1L-MYB intergenic region on chr6q23 regulates human fetal hemoglobin expression. Blood Cells Mol Dis. 2018;69:1–9. https://doi.org/10.1016/j.bcmd.2017.11.003.
Verma HK, Ratre YK, Bhaskar L, Colombatti R. Erythrocyte microRNAs: a tiny magic bullet with great potential for sickle cell disease therapy. Ann Hematol. 2021;100(3):607–14. https://doi.org/10.1007/s00277-020-04390-y.
Starlard-Davenport A, Smith A, Vu L, Li B, Pace BS. MIR29B mediates epigenetic mechanisms of HBG gene activation. Br J Haematol. 2019;186(1):91–100. https://doi.org/10.1111/bjh.15870.
Li B, Zhu X, Ward CM, Starlard-Davenport A, Takezaki M, et al. MIR-144-mediated NRF2 gene silencing inhibits fetal hemoglobin expression in sickle cell disease. Exp Hematol. 2019;70:85-96.e5. https://doi.org/10.1016/j.exphem.2018.11.002.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116(2):281–97. https://doi.org/10.1016/s0092-8674(04)00045-5.
Winkle M, El-Daly SM, Fabbri M, Calin GA. Noncoding RNA therapeutics—challenges and potential solutions. Nat Rev Drug Discov. 2021;20(8):629–51. https://doi.org/10.1038/s41573-021-00219-z.
Fyfe I. MicroRNAs—diagnostic markers in Parkinson disease? Nat Rev Neurol. 2020;16(2):65. https://doi.org/10.1038/s41582-019-0305-y.
Bhatnagar B, Garzon R. Clinical applications of MicroRNAs in acute myeloid leukemia: a mini-review. Front Oncol. 2021;11: 679022. https://doi.org/10.3389/fonc.2021.679022.
Geisler L, Mohr R, Lambrecht J, Knorr J, Jann H, et al. The role of miRNA in the pathophysiology of neuroendocrine tumors. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22168569.
Mitra T, Elangovan S. Cervical cancer development, chemoresistance, and therapy: a snapshot of involvement of microRNA. Mol Cell Biochem. 2021;476(12):4363–85. https://doi.org/10.1007/s11010-021-04249-4.
Shi Y, Liu Z, Lin Q, Luo Q, Cen Y, et al. MiRNAs and cancer: key link in diagnosis and therapy. Genes (Basel). 2021;12(8):1289. https://doi.org/10.3390/genes12081289.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–33. https://doi.org/10.1016/j.cell.2009.01.002.
Fabian MR, Sonenberg N, Filipowicz W. Regulation of mRNA translation and stability by microRNAs. Annu Rev Biochem. 2010;79:351–79. https://doi.org/10.1146/annurev-biochem-060308-103103.
Cuciniello R, Filosa S, Crispi S. Novel approaches in cancer treatment: preclinical and clinical development of small non-coding RNA therapeutics. J Exp Clin Cancer Res. 2021;40(1):383. https://doi.org/10.1186/s13046-021-02193-1.
Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75(5):843–54. https://doi.org/10.1016/0092-8674(93)90529-y.
Wightman B, Ha I, Ruvkun G. Posttranscriptional regulation of the heterochronic gene lin-14 by lin-4 mediates temporal pattern formation in C. elegans. Cell. 1993;75(5):855–62. https://doi.org/10.1016/0092-8674(93)90530-4.
Saki N, Abroun S, Hajizamani S, Rahim F, Shahjahani M. Association of chromosomal translocation and MiRNA expression with the pathogenesis of multiple myeloma. Cell J. 2014;16(2):99–110.
Kim VN. Small RNAs: classification, biogenesis, and function. Mol Cells. 2005;19(1):1–15.
Kozomara A, Birgaoanu M, Griffiths-Jones S. miRBase: from microRNA sequences to function. Nucleic Acids Res. 2019;47(D1):D155–62. https://doi.org/10.1093/nar/gky1141.
Kozomara A, Griffiths-Jones S. miRBase: annotating high confidence microRNAs using deep sequencing data. Nucleic Acids Res. 2014;42(Database issue):D68-73. https://doi.org/10.1093/nar/gkt1181.
Cui M, Wang H, Yao X, Zhang D, Xie Y, et al. Circulating MicroRNAs in cancer: potential and challenge. Front Genet. 2019;10:626. https://doi.org/10.3389/fgene.2019.00626.
Cheng G. Circulating miRNAs: roles in cancer diagnosis, prognosis and therapy. Adv Drug Deliv Rev. 2015;81:75–93. https://doi.org/10.1016/j.addr.2014.09.001.
Kumar S, Reddy PH. Are circulating microRNAs peripheral biomarkers for Alzheimer’s disease? Biochim Biophys Acta. 2016;1862(9):1617–27. https://doi.org/10.1016/j.bbadis.2016.06.001.
van den Berg MMJ, Krauskopf J, Ramaekers JG, Kleinjans JCS, Prickaerts J, et al. Circulating microRNAs as potential biomarkers for psychiatric and neurodegenerative disorders. Prog Neurobiol. 2020;185: 101732. https://doi.org/10.1016/j.pneurobio.2019.101732.
Zhang L, Sankaran VG, Lodish HF. MicroRNAs in erythroid and megakaryocytic differentiation and megakaryocyte-erythroid progenitor lineage commitment. Leukemia. 2012;26(11):2310–6. https://doi.org/10.1038/leu.2012.137.
Lessard S, Beaudoin M, Orkin SH, Bauer DE, Lettre G. 14q32 and let-7 microRNAs regulate transcriptional networks in fetal and adult human erythroblasts. Hum Mol Genet. 2018;27(8):1411–20. https://doi.org/10.1093/hmg/ddy051.
Papasavva PL, Papaioannou NY, Patsali P, Kurita R, Nakamura Y, et al. Distinct miRNA signatures and networks discern fetal from adult erythroid differentiation and primary from immortalized erythroid cells. Int J Mol Sci. 2021;22(7):3626. https://doi.org/10.3390/ijms22073626.
Bieker JJ. Probing the onset and regulation of erythroid cell-specific gene expression. Mt Sinai J Med. 2005;72(5):333–8.
Miller IJ, Bieker JJ. A novel, erythroid cell-specific murine transcription factor that binds to the CACCC element and is related to the Kruppel family of nuclear proteins. Mol Cell Biol. 1993;13(5):2776–86. https://doi.org/10.1128/mcb.13.5.2776.
Shariati L, Khanahmad H, Salehi M, Hejazi Z, Rahimmanesh I, et al. Genetic disruption of the KLF1 gene to overexpress the gamma-globin gene using the CRISPR/Cas9 system. J Gene Med. 2016;18(10):294–301. https://doi.org/10.1002/jgm.2928.
Tallack MR, Perkins AC. Three fingers on the switch: Kruppel-like factor 1 regulation of gamma-globin to beta-globin gene switching. Curr Opin Hematol. 2013;20(3):193–200. https://doi.org/10.1097/MOH.0b013e32835f59ba.
Borg J, Papadopoulos P, Georgitsi M, Gutierrez L, Grech G, et al. Haploinsufficiency for the erythroid transcription factor KLF1 causes hereditary persistence of fetal hemoglobin. Nat Genet. 2010;42(9):801–5. https://doi.org/10.1038/ng.630.
Li Y, Liu D, Zhang X, Li Z, Ye Y, et al. miR-326 regulates HbF synthesis by targeting EKLF in human erythroid cells. Exp Hematol. 2018;63:33-40.e2. https://doi.org/10.1016/j.exphem.2018.03.004.
Obeidi N, Pourfathollah AA, Soleimani M, Nikougoftar Zarif M, Kouhkan F. The effect of Mir-451 upregulation on erythroid lineage differentiation of murine embryonic stem cells. Cell J. 2016;18(2):165–78. https://doi.org/10.22074/cellj.2016.4311.
Pule GD, Mowla S, Novitzky N, Wonkam A. Hydroxyurea down-regulates BCL11A, KLF-1 and MYB through miRNA-mediated actions to induce gamma-globin expression: implications for new therapeutic approaches of sickle cell disease. Clin Transl Med. 2016;5(1):15. https://doi.org/10.1186/s40169-016-0092-7.
Ward CM, Li B, Pace BS. Original Research: stable expression of miR-34a mediates fetal hemoglobin induction in K562 cells. Exp Biol Med (Maywood). 2016;241(7):719–29. https://doi.org/10.1177/1535370216636725.
Yao X, Kodeboyina S, Liu L, Dzandu J, Sangerman J, et al. Role of STAT3 and GATA-1 interactions in gamma-globin gene expression. Exp Hematol. 2009;37(8):889–900. https://doi.org/10.1016/j.exphem.2009.05.004.
Bauer DE, Kamran SC, Orkin SH. Reawakening fetal hemoglobin: prospects for new therapies for the beta-globin disorders. Blood. 2012;120(15):2945–53. https://doi.org/10.1182/blood-2012-06-292078.
Makani J, Menzel S, Nkya S, Cox SE, Drasar E, et al. Genetics of fetal hemoglobin in Tanzanian and British patients with sickle cell anemia. Blood. 2011;117(4):1390–2. https://doi.org/10.1182/blood-2010-08-302703.
Saki N, Abroun S, Soleimani M, Kavianpour M, Shahjahani M, et al. MicroRNA expression in beta-thalassemia and sickle cell disease: a role in the induction of fetal hemoglobin. Cell J. 2016;17(4):583–92. https://doi.org/10.22074/cellj.2016.3808.
Sangokoya C, Telen MJ, Chi JT. microRNA miR-144 modulates oxidative stress tolerance and associates with anemia severity in sickle cell disease. Blood. 2010;116(20):4338–48. https://doi.org/10.1182/blood-2009-04-214817.
Gholampour MA, Asadi M, Naderi M, Azarkeivan A, Soleimani M, et al. miR-30a regulates gamma-globin expression in erythoid precursors of intermedia thalassemia through targeting BCL11A. Mol Biol Rep. 2020;47(5):3909–18. https://doi.org/10.1007/s11033-020-05483-7.
Mnika K, Mazandu GK, Jonas M, Pule GD, Chimusa ER, et al. Hydroxyurea-induced miRNA expression in sickle cell disease patients in Africa. Front Genet. 2019;10:509. https://doi.org/10.3389/fgene.2019.00509.
Lee YT, de Vasconcellos JF, Yuan J, Byrnes C, Noh SJ, et al. LIN28B-mediated expression of fetal hemoglobin and production of fetal-like erythrocytes from adult human erythroblasts ex vivo. Blood. 2013;122(6):1034–41. https://doi.org/10.1182/blood-2012-12-472308.
Lulli V, Romania P, Morsilli O, Cianciulli P, Gabbianelli M, et al. MicroRNA-486-3p regulates gamma-globin expression in human erythroid cells by directly modulating BCL11A. PLoS ONE. 2013;8(4): e60436. https://doi.org/10.1371/journal.pone.0060436.
Lopes FC, Ferreira R, Albuquerque DM, Silveira AA, Costa R, et al. In vitro and in vivo anti-angiogenic effects of hydroxyurea. Microvasc Res. 2014;94:106–13. https://doi.org/10.1016/j.mvr.2014.05.009.
Hojjati MT, Azarkeivan A, Pourfathollah AA, Amirizadeh N. Comparison of MicroRNAs mediated in reactivation of the gamma-globin in beta-thalassemia patients, responders and non-responders to hydroxyurea. Hemoglobin. 2017;41(2):110–5. https://doi.org/10.1080/03630269.2017.1290651.
Sawant M, Chandrakala S, Colah R, Ghosh K, Nadkarni A. Does HbF induction by hydroxycarbamide work through MIR210 in sickle cell anaemia patients? Br J Haematol. 2016;173(5):801–3. https://doi.org/10.1111/bjh.13642.
Jiang J, Best S, Menzel S, Silver N, Lai MI, et al. cMYB is involved in the regulation of fetal hemoglobin production in adults. Blood. 2006;108(3):1077–83. https://doi.org/10.1182/blood-2006-01-008912.
Suzuki M, Yamamoto M, Engel JD. Fetal globin gene repressors as drug targets for molecular therapies to treat the beta-globinopathies. Mol Cell Biol. 2014;34(19):3560–9. https://doi.org/10.1128/MCB.00714-14.
Bianchi E, Zini R, Salati S, Tenedini E, Norfo R, et al. c-myb supports erythropoiesis through the transactivation of KLF1 and LMO2 expression. Blood. 2010;116(22):e99-110. https://doi.org/10.1182/blood-2009-08-238311.
Sankaran VG, Menne TF, Scepanovic D, Vergilio JA, Ji P, et al. MicroRNA-15a and -16-1 act via MYB to elevate fetal hemoglobin expression in human trisomy 13. Proc Natl Acad Sci USA. 2011;108(4):1519–24. https://doi.org/10.1073/pnas.1018384108.
Chung EY, Dews M, Cozma D, Yu D, Wentzel EA, et al. c-Myb oncoprotein is an essential target of the dleu2 tumor suppressor microRNA cluster. Cancer Biol Ther. 2008;7(11):1758–64. https://doi.org/10.4161/cbt.7.11.6722.
Kouhkan F, Soleimani M, Daliri M, Behmanesh M, Mobarra N, et al. miR-451 up-regulation, induce erythroid differentiation of CD133+cells independent of cytokine cocktails. Iran J Basic Med Sci. 2013;16(6):756–63.
Azzouzi I, Moest H, Winkler J, Fauchere JC, Gerber AP, et al. MicroRNA-96 directly inhibits gamma-globin expression in human erythropoiesis. PLoS ONE. 2011;6(7): e22838. https://doi.org/10.1371/journal.pone.0022838.
Sun KT, Huang YN, Palanisamy K, Chang SS, Wang IK, et al. Reciprocal regulation of gamma-globin expression by exo-miRNAs: Relevance to gamma-globin silencing in beta-thalassemia major. Sci Rep. 2017;7(1):202. https://doi.org/10.1038/s41598-017-00150-7.
Zolea F, Battaglia AM, Chiarella E, Malanga D, De Marco C, et al. Ferritin heavy subunit silencing blocks the erythroid commitment of K562 cells via miR-150 up-regulation and GATA-1 repression. Int J Mol Sci. 2017;18(10):2167. https://doi.org/10.3390/ijms18102167.
Ma Y, Wang B, Jiang F, Wang D, Liu H, et al. A feedback loop consisting of microRNA 23a/27a and the beta-like globin suppressors KLF3 and SP1 regulates globin gene expression. Mol Cell Biol. 2013;33(20):3994–4007. https://doi.org/10.1128/MCB.00623-13.
Ma YN, Chen MT, Wu ZK, Zhao HL, Yu HC, et al. Emodin can induce K562 cells to erythroid differentiation and improve the expression of globin genes. Mol Cell Biochem. 2013;382(1–2):127–36. https://doi.org/10.1007/s11010-013-1726-3.
Zhu X, Li B, Pace BS. NRF2 mediates gamma-globin gene regulation and fetal hemoglobin induction in human erythroid progenitors. Haematologica. 2017;102(8):e285–8. https://doi.org/10.3324/haematol.2016.160788.
Ruiz MA, Rivers A, Ibanez V, Vaitkus K, Mahmud N, et al. Hydroxymethylcytosine and demethylation of the gamma-globin gene promoter during erythroid differentiation. Epigenetics. 2015;10(5):397–407. https://doi.org/10.1080/15592294.2015.1039220.
Ginder GD. Epigenetic regulation of fetal globin gene expression in adult erythroid cells. Transl Res. 2015;165(1):115–25. https://doi.org/10.1016/j.trsl.2014.05.002.
Mabaera R, Richardson CA, Johnson K, Hsu M, Fiering S, et al. Developmental- and differentiation-specific patterns of human gamma- and beta-globin promoter DNA methylation. Blood. 2007;110(4):1343–52. https://doi.org/10.1182/blood-2007-01-068635.
Lavelle D, Saunthararajah Y, Vaitkus K, Singh M, Banzon V, et al. S110, a novel decitabine dinucleotide, increases fetal hemoglobin levels in baboons (P. anubis). J Transl Med. 2010;8:92. https://doi.org/10.1186/1479-5876-8-92.
Molokie R, Lavelle D, Gowhari M, Pacini M, Krauz L, et al. Oral tetrahydrouridine and decitabine for non-cytotoxic epigenetic gene regulation in sickle cell disease: a randomized phase 1 study. PLoS Med. 2017;14(9): e1002382. https://doi.org/10.1371/journal.pmed.1002382.
Singal R, Wang SZ, Sargent T, Zhu SZ, Ginder GD. Methylation of promoter proximal-transcribed sequences of an embryonic globin gene inhibits transcription in primary erythroid cells and promotes formation of a cell type-specific methyl cytosine binding complex. J Biol Chem. 2002;277(3):1897–905. https://doi.org/10.1074/jbc.M105580200.
Ginder GD, Gnanapragasam MN, Mian OY. The role of the epigenetic signal, DNA methylation, in gene regulation during erythroid development. Curr Top Dev Biol. 2008;82:85–116. https://doi.org/10.1016/S0070-2153(07)00004-X.
Forrester WC, Thompson C, Elder JT, Groudine M. A developmentally stable chromatin structure in the human beta-globin gene cluster. Proc Natl Acad Sci USA. 1986;83(5):1359–63. https://doi.org/10.1073/pnas.83.5.1359.
Camiener GW, Smith CG. Studies of the enzymatic deamination of cytosine arabinoside. I. Enzyme distribution and species specificity. Biochem Pharmacol. 1965;14(10):1405–16. https://doi.org/10.1016/0006-2952(65)90175-9.
Ebrahem Q, Mahfouz RZ, Ng KP, Saunthararajah Y. High cytidine deaminase expression in the liver provides sanctuary for cancer cells from decitabine treatment effects. Oncotarget. 2012;3(10):1137–45. https://doi.org/10.18632/oncotarget.597.
Gao C, Wang J, Li Y, Zhao H, Li R, et al. Incidence and risk of hematologic toxicities with hypomethylating agents in the treatment of myelodysplastic syndromes and acute myeloid leukopenia: a systematic review and meta-analysis. Medicine (Baltimore). 2018;97(34): e11860. https://doi.org/10.1097/MD.0000000000011860.
Starlard-Davenport A, Kutanzi K, Tryndyak V, Word B, Lyn-Cook B. Restoration of the methylation status of hypermethylated gene promoters by microRNA-29b in human breast cancer: a novel epigenetic therapeutic approach. J Carcinog. 2013;12:15. https://doi.org/10.4103/1477-3163.115720.
Walker AL, Steward S, Howard TA, Mortier N, Smeltzer M, et al. Epigenetic and molecular profiles of erythroid cells after hydroxyurea treatment in sickle cell anemia. Blood. 2011;118(20):5664–70. https://doi.org/10.1182/blood-2011-07-368746.
Rivers A, Molokie R, Lavelle D. A new target for fetal hemoglobin reactivation. Haematologica. 2019;104(12):2325–7. https://doi.org/10.3324/haematol.2019.230904.
US FDA. FDA approves first-of-its kind targeted RNA-based therapy to treat a rare disease. Silver Spring: US FDA; 2018.
US FDA. Moderna COVID-19 Vaccine/mRNA-1273 Emergency Use Authorization (EUA) for an Unapproved Product Review Memorandum. Sliver Spring: US FDA; 2020.
Lam JK, Chow MY, Zhang Y, Leung SW. siRNA versus miRNA as therapeutics for gene silencing. Mol Ther Nucleic Acids. 2015;4: e252. https://doi.org/10.1038/mtna.2015.23.
Rupaimoole R, Slack FJ. MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat Rev Drug Discov. 2017;16(3):203–22. https://doi.org/10.1038/nrd.2016.246.
Mishra S, Yadav T, Rani V. Exploring miRNA based approaches in cancer diagnostics and therapeutics. Crit Rev Oncol Hematol. 2016;98:12–23. https://doi.org/10.1016/j.critrevonc.2015.10.003.
Charbe NB, Amnerkar ND, Ramesh B, Tambuwala MM, Bakshi HA, et al. Small interfering RNA for cancer treatment: overcoming hurdles in delivery. Acta Pharm Sin B. 2020;10(11):2075–109. https://doi.org/10.1016/j.apsb.2020.10.005.
Zhang Y, Wang Z, Gemeinhart RA. Progress in microRNA delivery. J Control Release. 2013;172(3):962–74. https://doi.org/10.1016/j.jconrel.2013.09.015.
Chen Y, Gao DY, Huang L. In vivo delivery of miRNAs for cancer therapy: challenges and strategies. Adv Drug Deliv Rev. 2015;81:128–41. https://doi.org/10.1016/j.addr.2014.05.009.
Felgner PL, Gadek TR, Holm M, Roman R, Chan HW, et al. Lipofection: a highly efficient, lipid-mediated DNA-transfection procedure. Proc Natl Acad Sci USA. 1987;84(21):7413–7. https://doi.org/10.1073/pnas.84.21.7413.
Omidi Y, Hollins AJ, Benboubetra M, Drayton R, Benter IF, et al. Toxicogenomics of non-viral vectors for gene therapy: a microarray study of lipofectin- and oligofectamine-induced gene expression changes in human epithelial cells. J Drug Target. 2003;11(6):311–23. https://doi.org/10.1080/10611860310001636908.
Khan MA, Jabeen R, Mohammad O. Prophylactic role of liposomized chloroquine against murine cryptococcosis less susceptible to fluconazole. Pharm Res. 2004;21(12):2207–12. https://doi.org/10.1007/s11095-004-7672-8.
Judge A, McClintock K, Phelps JR, Maclachlan I. Hypersensitivity and loss of disease site targeting caused by antibody responses to PEGylated liposomes. Mol Ther. 2006;13(2):328–37. https://doi.org/10.1016/j.ymthe.2005.09.014.
Morrissey DV, Lockridge JA, Shaw L, Blanchard K, Jensen K, et al. Potent and persistent in vivo anti-HBV activity of chemically modified siRNAs. Nat Biotechnol. 2005;23(8):1002–7. https://doi.org/10.1038/nbt1122.
Pirollo KF, Rait A, Zhou Q, Hwang SH, Dagata JA, et al. Materializing the potential of small interfering RNA via a tumor-targeting nanodelivery system. Cancer Res. 2007;67(7):2938–43. https://doi.org/10.1158/0008-5472.CAN-06-4535.
Sercombe L, Veerati T, Moheimani F, Wu SY, Sood AK, et al. Advances and challenges of liposome assisted drug delivery. Front Pharmacol. 2015;6:286. https://doi.org/10.3389/fphar.2015.00286.
Wasungu L, Hoekstra D. Cationic lipids, lipoplexes and intracellular delivery of genes. J Control Release. 2006;116(2):255–64. https://doi.org/10.1016/j.jconrel.2006.06.024.
Li SD, Chen YC, Hackett MJ, Huang L. Tumor-targeted delivery of siRNA by self-assembled nanoparticles. Mol Ther. 2008;16(1):163–9. https://doi.org/10.1038/sj.mt.6300323.
Tagami T, Nakamura K, Shimizu T, Ishida T, Kiwada H. Effect of siRNA in PEG-coated siRNA-lipoplex on anti-PEG IgM production. J Control Release. 2009;137(3):234–40. https://doi.org/10.1016/j.jconrel.2009.04.006.
Byrne M, Tzekov R, Wang Y, Rodgers A, Cardia J, et al. Novel hydrophobically modified asymmetric RNAi compounds (sd-rxRNA) demonstrate robust efficacy in the eye. J Ocul Pharmacol Ther. 2013;29(10):855–64. https://doi.org/10.1089/jop.2013.0148.
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MDP, et al. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnol. 2018;16(1):71. https://doi.org/10.1186/s12951-018-0392-8.
Murthy SK. Nanoparticles in modern medicine: state of the art and future challenges. Int J Nanomed. 2007;2(2):129–41.
Chang EH, Harford JB, Eaton MA, Boisseau PM, Dube A, et al. Nanomedicine: past, present and future—a global perspective. Biochem Biophys Res Commun. 2015;468(3):511–7. https://doi.org/10.1016/j.bbrc.2015.10.136.
Haba Y, Kojima C, Harada A, Ura T, Horinaka H, et al. Preparation of poly(ethylene glycol)-modified poly(amido amine) dendrimers encapsulating gold nanoparticles and their heat-generating ability. Langmuir. 2007;23(10):5243–6. https://doi.org/10.1021/la0700826.
Cao S, Lin C, Li X, Liang Y, Saw PE. TME-responsive multistage nanoplatform for siRNA delivery and effective cancer therapy. Int J Nanomed. 2021;16:5909–21. https://doi.org/10.2147/IJN.S322901.
Qin X, Wu C, Niu D, Qin L, Wang X, et al. Peroxisome inspired hybrid enzyme nanogels for chemodynamic and photodynamic therapy. Nat Commun. 2021;12(1):5243. https://doi.org/10.1038/s41467-021-25561-z.
Lee N, Choi SH, Hyeon T. Nano-sized CT contrast agents. Adv Mater. 2013;25(19):2641–60. https://doi.org/10.1002/adma.201300081.
Curry T, Kopelman R, Shilo M, Popovtzer R. Multifunctional theranostic gold nanoparticles for targeted CT imaging and photothermal therapy. Contrast Media Mol Imaging. 2014;9(1):53–61. https://doi.org/10.1002/cmmi.1563.
Zhu L, Torchilin VP. Stimulus-responsive nanopreparations for tumor targeting. Integr Biol (Camb). 2013;5(1):96–107. https://doi.org/10.1039/c2ib20135f.
Heidel JD, Schluep T. Cyclodextrin-containing polymers: versatile platforms of drug delivery materials. J Drug Deliv. 2012;2012: 262731. https://doi.org/10.1155/2012/262731.
Nayerossadat N, Maedeh T, Ali PA. Viral and nonviral delivery systems for gene delivery. Adv Biomed Res. 2012;1:27. https://doi.org/10.4103/2277-9175.98152.
Yang N. An overview of viral and nonviral delivery systems for microRNA. Int J Pharm Investig. 2015;5(4):179–81. https://doi.org/10.4103/2230-973X.167646.
Goswami R, Subramanian G, Silayeva L, Newkirk I, Doctor D, et al. Gene therapy leaves a vicious cycle. Front Oncol. 2019;9:297. https://doi.org/10.3389/fonc.2019.00297.
Esrick EB, Lehmann LE, Biffi A, Achebe M, Brendel C, et al. Post-transcriptional genetic silencing of BCL11A to treat sickle cell disease. N Engl J Med. 2021;384(3):205–15. https://doi.org/10.1056/NEJMoa2029392.
Brendel C, Guda S, Renella R, Bauer DE, Canver MC, et al. Lineage-specific BCL11A knockdown circumvents toxicities and reverses sickle phenotype. J Clin Invest. 2016;126(10):3868–78. https://doi.org/10.1172/JCI87885.
Uwaezuoke SN, Ayuk AC, Ndu IK, Eneh CI, Mbanefo NR, et al. Vaso-occlusive crisis in sickle cell disease: current paradigm on pain management. J Pain Res. 2018;11:3141–50. https://doi.org/10.2147/JPR.S185582.
Ehlert EM, Eggers R, Niclou SP, Verhaagen J. Cellular toxicity following application of adeno-associated viral vector-mediated RNA interference in the nervous system. BMC Neurosci. 2010;11:20. https://doi.org/10.1186/1471-2202-11-20.
Davidson BL, McCray PB Jr. Current prospects for RNA interference-based therapies. Nat Rev Genet. 2011;12(5):329–40. https://doi.org/10.1038/nrg2968.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this manuscript was supported in part by: NIH/National Heart, Lung, and Blood Institute grant HL144641-01A1 to Athena Starlard-Davenport. NIH/National Heart, Lung, and Blood Institute grant HL149365-01A1 to Betty S. Pace.
Conflicts of interest/Competing interest
Athena Starlard-Davenport, Qingqing Gu, and Betty S. Pace declare that there are no conflicts of interests with respect to the research, authorship, and/or publication of this article.
Ethics approval and consent
Not applicable.
Author contributions
AS-D, QG, and BSP reviewed the literature, designed the review sections, and conducted a final review of the paper. AS-D designed the figures and tables and wrote several drafts of the paper.
Data availability
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Starlard-Davenport, A., Gu, Q. & Pace, B.S. Targeting Genetic Modifiers of HBG Gene Expression in Sickle Cell Disease: The miRNA Option. Mol Diagn Ther 26, 497–509 (2022). https://doi.org/10.1007/s40291-022-00589-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-022-00589-z