Abstract
Background
Hamstrings neuromuscular function is a crucial component of functional movement, and changes after anterior cruciate ligament (ACL) injury contribute to risk factors for secondary injury and long-term sequelae. To effectively treat muscular impairments, an accurate understanding of hamstrings neuromuscular function in patients with ACL reconstruction (ACLR) is needed.
Objective
A systematic review and meta-analysis were undertaken to describe and quantify hamstrings neuromuscular function in individuals with ACLR compared to controls.
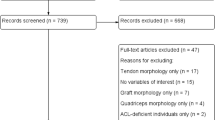
Methods
We searched PubMed, Web of Science, SPORTDiscus, CINAHL, and EBSCOhost databases in October of 2020 for studies evaluating the difference between hamstrings electromyography (EMG) between individuals with ACLR and controls. Two independent reviewers assessed each paper for inclusion and quality. Means and standard deviations were extracted from each included study to allow random-effect size (ES) meta-analysis calculations for comparison of results.
Results
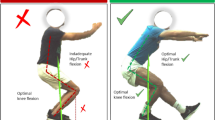
Thirty-four studies were included for final review. From these, 5 categories of neuromuscular outcomes were identified, and studies were grouped accordingly: (1) muscle activation levels (EMG amplitude), (2) co-activation, (3) onset timing, (4) electromechanical delay, and (5) time-to-peak activity. Moderate to strong evidence indicates that individuals with ACLR demonstrate higher hamstrings EMG amplitude (normalized to % maximum voluntary isometric contraction) and hamstrings-to-quadriceps co-activation during gait and stair ambulation compared to controls. In addition, there was moderate evidence of longer electromechanical delay during knee flexion and greater hamstrings-to-quadriceps co-activation during knee extension compared to controls.
Conclusions
Greater hamstrings EMG amplitude and co-activation during gait and ambulation tasks and longer electromechanical delay of the hamstrings in individuals with ACLR align with clinical impairments following ACLR and have implications for re-injury risk and long-term joint health, thus warranting attention in rehabilitation.







Similar content being viewed by others
References
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–70. https://doi.org/10.1177/0363546514542796.
Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–52. https://doi.org/10.1136/bjsports-2013-093398.
Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–43. https://doi.org/10.1177/0363546510384798.
Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–32. https://doi.org/10.1177/0363546516651845.
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–76. https://doi.org/10.1177/0363546515621554.
Harris KP, Driban JB, Sitler MR, Cattano NM, Balasubramanian E, Hootman JM. Tibiofemoral osteoarthritis after surgical or nonsurgical treatment of anterior cruciate ligament rupture: a systematic review. J Athl Train. 2017;52(6):507–17. https://doi.org/10.4085/1062-6050-49.3.89.
Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49(6):806–19. https://doi.org/10.4085/1062-6050-49.3.35.
Palmieri-Smith RM, McLean SG, Ashton-Miller JA, Wojtys EM. Association of quadriceps and hamstrings cocontraction patterns with knee joint loading. J Athl Train. 2009;44(3):256–63. https://doi.org/10.4085/1062-6050-44.3.256.
Blackburn T, Pietrosimone B, Goodwin JS, Johnston C, Spang JT. Co-activation during gait following anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2019;67:153–9. https://doi.org/10.1016/j.clinbiomech.2019.05.010.
Pietrosimone B, Pfeiffer SJ, Harkey MS, Wallace K, Hunt C, Blackburn JT, et al. Quadriceps weakness associates with greater T1rho relaxation time in the medial femoral articular cartilage 6 months following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2632–42. https://doi.org/10.1007/s00167-018-5290-y.
Pietrosimone B, Seeley MK, Johnston C, Pfeiffer SJ, Spang JT, Blackburn JT. Walking ground reaction force post-ACL reconstruction: analysis of time and symptoms. Med Sci Sports Exerc. 2019;51(2):246–54. https://doi.org/10.1249/MSS.0000000000001776.
Palmieri-Smith RM, Thomas AC. A neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev. 2009;37(3):147–53. https://doi.org/10.1097/JES.0b013e3181aa6669.
MacWilliams BA, Wilson DR, DesJardins JD, Romero J, Chao EY. Hamstrings cocontraction reduces internal rotation, anterior translation, and anterior cruciate ligament load in weight-bearing flexion. J Orthop Res. 1999;17(6):817–22. https://doi.org/10.1002/jor.1100170605.
Palmieri-Smith RM, Strickland M, Lepley LK. Hamstring muscle activity after primary anterior cruciate ligament reconstruction-a protective mechanism in those who do not sustain a secondary injury? A preliminary study. Sports Health. 2019;11(4):316–23. https://doi.org/10.1177/1941738119852630.
Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71–9.
Basmajian JV, de Luca CJ. Muscles alive: their functions revealed by electromyography. 5th ed. Baltimore: Williams & Wilkins; 1985.
NIOSH. Selected topics in surface electromyography for use in the occupational setting: expert perspectives 1999. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 91-1001999.
Scheurer SA, Sherman DA, Glaviano NR, Ingersoll CD, Norte GE. Corticomotor function is associated with quadriceps rate of torque development in individuals with ACL surgery. Exp Brain Res. 2020;238(2):283–94. https://doi.org/10.1007/s00221-019-05713-w.
Norte GE, Hertel J, Saliba SA, Diduch DR, Hart JM. Quadriceps neuromuscular function in patients with anterior cruciate ligament reconstruction with or without knee osteoarthritis: a cross-sectional study. J Athl Train. 2018;53(5):475–85. https://doi.org/10.4085/1062-6050-102-17.
Kuenze C, Hertel J, Saliba S, Diduch DR, Weltman A, Hart JM. Clinical thresholds for quadriceps assessment after anterior cruciate ligament reconstruction. J Sport Rehabil. 2015;24(1):36–46. https://doi.org/10.1123/jsr.2013-0110.
Oiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthr Cartil. 2015;23(2):171–7. https://doi.org/10.1016/j.joca.2014.10.008.
Flaxman TE, Alkjaer T, Simonsen EB, Krogsgaard MR, Benoit DL. Predicting the functional roles of knee joint muscles from internal joint moments. Med Sci Sports Exerc. 2017;49(3):527–37. https://doi.org/10.1249/MSS.0000000000001125.
Flaxman TE, Smith AJ, Benoit DL. Sex-related differences in neuromuscular control: Implications for injury mechanisms or healthy stabilisation strategies? J Orthop Res. 2014;32(2):310–7. https://doi.org/10.1002/jor.22510.
Kim HJ, Lee JH, Ahn SE, Park MJ, Lee DH. Influence of anterior cruciate ligament tear on thigh muscle strength and hamstring-to-quadriceps ratio: a meta-analysis. PLoS ONE. 2016;11(1):e0146234. https://doi.org/10.1371/journal.pone.0146234.
Norte GE, Knaus KR, Kuenze C, Handsfield GG, Meyer CH, Blemker SS, et al. MRI-based assessment of lower-extremity muscle volumes in patients before and after ACL reconstruction. J Sport Rehabil. 2018;27(3):201–12. https://doi.org/10.1123/jsr.2016-0141.
Delahunt E, McGroarty M, De Vito G, Ditroilo M. Nordic hamstring exercise training alters knee joint kinematics and hamstring activation patterns in young men. Eur J Appl Physiol. 2016;116(4):663–72. https://doi.org/10.1007/s00421-015-3325-3.
Bencke J, Aagaard P, Zebis MK. Muscle activation during ACL injury risk movements in young female athletes: a narrative review. Front Physiol. 2018. https://doi.org/10.3389/fphys.2018.00445.
Hootman JM, Driban JB, Sitler MR, Harris KP, Cattano NM. Reliability and validity of three quality rating instruments for systematic reviews of observational studies. Res Synth Methods. 2011;2(2):110–8. https://doi.org/10.1002/jrsm.41.
Open-Source. Engauge digitizer software. In: Mitchell M, Muftakhidinov B, Winchen T, van Schaik B, Wilms A, Kensington et al., editors.: GitHub; 2015. p. Windows 10.
Briem K, Ragnarsdottir AM, Arnason SI, Sveinsson T. Altered medial versus lateral hamstring muscle activity during hop testing in female athletes 1–6 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):12–7. https://doi.org/10.1007/s00167-014-3333-6.
Ortiz A, Capo-Lugo CE, Venegas-Rios HL. Biomechanical deficiencies in women with semitendinosus-gracilis anterior cruciate ligament reconstruction during drop jumps. PM R. 2014;6(12):1097–106. https://doi.org/10.1016/j.pmrj.2014.07.003.
Telianidis S, Perraton L, Clark RA, Pua Y-H, Fortin K, Bryant AL. Diminished sub-maximal quadriceps force control in anterior cruciate ligament reconstructed patients is related to quadriceps and hamstring muscle dyskinesia. J Electromyogr Kinesiol. 2014;24(4):513–9.
Rudroff T. Functional capability is enhanced with semitendinosus than patellar tendon ACL repair. Med Sci Sports Exerc. 2003;35(9):1486–92. https://doi.org/10.1249/01.MSS.0000084425.07852.7D.
Swanik CB, Lephart SM, Giraldo JL, Demont RG, Fu FH. Reactive muscle firing of anterior cruciate ligament-injured females during functional activities. J Athl Train. 1999;34(2):121–9.
Wojtys EM, Huston LJ. Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Am J Sports Med. 2000;28(3):336–44. https://doi.org/10.1177/03635465000280030901.
Demont RG, Lephart SM, Giraldo JL, Swanik CB, Fu FH. Muscle preactivity of anterior cruciate ligament-deficient and -reconstructed females during functional activities. J Athl Train. 1999;34(2):115–20.
Ciccotti MG, Kerlan RK, Perry J, Pink M. An electromyographic analysis of the knee during functional activities. II. The anterior cruciate ligament-deficient and -reconstructed profiles. Am J Sports Med. 1994;22(5):651–8. https://doi.org/10.1177/036354659402200513.
Ortiz A, Olson S, Trudelle-Jackson E, Rosario M, Venegas HL. Landing mechanics during side hopping and crossover hopping maneuvers in noninjured women and women with anterior cruciate ligament reconstruction. PM R. 2011;3(1):13–20. https://doi.org/10.1016/j.pmrj.2010.10.018.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: L. Erlbaum Associates; 1988.
Higgins JPT, Green S, Cochrane C. Cochrane handbook for systematic reviews of interventions. Chichester, Hoboken: Wiley-Blackwell; 2008.
Pamukoff DN, Pietrosimone BG, Ryan ED, Lee DR, Blackburn JT. Quadriceps function and hamstrings co-activation after anterior cruciate ligament reconstruction. J Athl Train. 2017;52(5):422–8. https://doi.org/10.4085/1062-6050-52.3.05.
Jordan MJ, Aagaard P, Herzog W. Asymmetry and thigh muscle coactivity in fatigued anterior cruciate ligament-reconstructed elite skiers. Med Sci Sports Exerc. 2017;49(1):11–20. https://doi.org/10.1249/MSS.0000000000001076.
Bryant AL, Newton RU, Steele J. Successful feed-forward strategies following ACL injury and reconstruction. J Electromyogr Kinesiol. 2009;19(5):988–97. https://doi.org/10.1016/j.jelekin.2008.06.001.
Bryant AL, Pua YH, Clark RA. Morphology of knee extension torque-time curves following anterior cruciate ligament injury and reconstruction. J Bone Jt Surg Am. 2009;91(6):1424–31. https://doi.org/10.2106/JBJS.H.01335.
Kasovic M, Mejovsek M, Matkovic B, Jankovic S, Tudor A. Electromyographic analysis of the knee using fixed-activation threshold after anterior cruciate ligament reconstruction. Int Orthop. 2011;35(5):681–7. https://doi.org/10.1007/s00264-010-1050-4.
Rush JL, Norte GE, Lepley AS. Limb differences in hamstring muscle function and morphology after anterior cruciate ligament reconstruction. Phys Ther Sport. 2020;45:168–75. https://doi.org/10.1016/j.ptsp.2020.06.012.
Ristanis S, Tsepis E, Giotis D, Stergiou N, Cerulli G, Georgoulis AD. Electromechanical delay of the knee flexor muscles is impaired after harvesting hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(11):2179–86. https://doi.org/10.1177/0363546509340771.
Árnason S, Birnir B, Guðmundsson T, Guðnason G, Briem K. Medial hamstring muscle activation patterns are affected 1–6 years after ACL reconstruction using hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1024–9.
Coats-Thomas MS, Miranda DL, Badger GJ, Fleming BC. Effects of ACL reconstruction surgery on muscle activity of the lower limb during a jump-cut maneuver in males and females. J Orthop Res. 2013;31(12):1890–6. https://doi.org/10.1002/jor.22470.
Cordeiro N, Cortes N, Fernandes O, Diniz A, Pezarat-Correia P. Dynamic knee stability and ballistic knee movement after ACL reconstruction: an application on instep soccer kick. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1100–6. https://doi.org/10.1007/s00167-014-2894-8.
Freddolini M, Battaglioli A, Chiechi F, Placella G, Georgoulis A, Cerulli G, et al. Electromechanical delay of the knee flexor muscles after anterior cruciate ligament reconstruction using semitendinosus tendon. Sports Biomech. 2015;14(4):384–93. https://doi.org/10.1080/14763141.2015.1086425.
Hall M, Stevermer CA, Gillette JC. Muscle activity amplitudes and co-contraction during stair ambulation following anterior cruciate ligament reconstruction. J Electromyogr Kinesiol. 2015;25(2):298–304. https://doi.org/10.1016/j.jelekin.2015.01.007.
Harput G, Howard JS, Mattacola C. Comparison of muscle activation levels between healthy individuals and persons who have undergone anterior cruciate ligament reconstruction during different phases of weight-bearing exercises. J Orthop Sports Phys Ther. 2016;46(11):984–92. https://doi.org/10.2519/jospt.2016.5896.
Heller BM, Pincivero DM. The effects of ACL injury on lower extremity activation during closed kinetic chain exercise. J Sports Med Phys Fit. 2003;43(2):180–8.
Perraton L, Clark R, Crossley K, Pua YH, Whitehead T, Morris H, et al. Impaired voluntary quadriceps force control following anterior cruciate ligament reconstruction: relationship with knee function. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1424–31. https://doi.org/10.1007/s00167-015-3937-5.
Pincheira PA, Silvestre R, Armijo-Olivo S, Guzman-Venegas R. Ankle perturbation generates bilateral alteration of knee muscle onset times after unilateral anterior cruciate ligament reconstruction. PeerJ. 2018;6(7):e5310. https://doi.org/10.7717/peerj.5310.
Flaxman TE, Alkjaer T, Smale KB, Simonsen EB, Krogsgaard MR, Benoit DL. Differences in EMG-moment relationships between ACL-injured and uninjured adults during a weight-bearing multidirectional force control task. J Orthop Res. 2019;37(1):113–23. https://doi.org/10.1002/jor.24145.
Lepley LK, Thomas AC, McLean SG, Palmieri-Smith RM. Fatigue’s lack of effect on thigh-muscle activity in anterior cruciate ligament-reconstructed patients during a dynamic-landing task. J Sport Rehabil. 2013;22(2):83–92. https://doi.org/10.1123/jsr.22.2.83.
San Martín-Mohr C, Cristi-Sánchez I, Pincheira PA, Reyes A, Berral FJ, Oyarzo C. Knee sensorimotor control following anterior cruciate ligament reconstruction: a comparison between reconstruction techniques. PLoS ONE. 2018;13(11):e0205658. https://doi.org/10.1371/journal.pone.0205658.
Smeets A, Verschueren S, Staes F, Vandenneucker H, Claes S, Vanrenterghem J. Athletes with an ACL reconstruction show a different neuromuscular response to environmental challenges compared to uninjured athletes. Gait Posture. 2021;83:44–51. https://doi.org/10.1016/j.gaitpost.2020.09.032.
Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM. Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16(1):2–14. https://doi.org/10.1007/s00167-007-0427-4.
Pereira HM, Nowotny AH, Santos AB, Cardoso JR. Electromyographic activity of knee stabilizer muscles during six different balance board stimuli after anterior cruciate ligament surgery. Electromyogr Clin Neurophysiol. 2009;49(2–3):117–24.
Mantashloo Z, Letafatkar A, Moradi M. Vertical ground reaction force and knee muscle activation asymmetries in patients with ACL reconstruction compared to healthy individuals. Knee Surgery Sports Traumatol Arthrosc. 2020;28(6):2009–14. https://doi.org/10.1007/s00167-019-05743-5.
Cristiani R, Mikkelsen C, Forssblad M, Engström B, Stålman A. Only one patient out of five achieves symmetrical knee function 6 months after primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3461–70. https://doi.org/10.1007/s00167-019-05396-4.
Knutson LM, Soderberg GL, Ballantyne BT, Clarke WR. A study of various normalization procedures for within day electromyographic data. J Electromyogr Kinesiol. 1994;4(1):47–59. https://doi.org/10.1016/1050-6411(94)90026-4.
Withrow TJ, Huston LJ, Wojtys EM, Ashton-Miller JA. Effect of varying hamstring tension on anterior cruciate ligament strain during in vitro impulsive knee flexion and compression loading. J Bone Jt Surg Am. 2008;90(4):815–23. https://doi.org/10.2106/JBJS.F.01352.
Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–51. https://doi.org/10.1136/bjsports-2015-095908.
Khandha A, Manal K, Wellsandt E, Capin J, Snyder-Mackler L, Buchanan TS. Gait mechanics in those with/without medial compartment knee osteoarthritis 5 years after anterior cruciate ligament reconstruction. J Orthop Res. 2017;35(3):625–33. https://doi.org/10.1002/jor.23261.
Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–57. https://doi.org/10.1177/0363546514526139.
Ward S, Pearce AJ, Pietrosimone B, Bennell K, Clark R, Bryant AL. Neuromuscular deficits after peripheral joint injury: a neurophysiological hypothesis. Muscle Nerve. 2015;51(3):327–32. https://doi.org/10.1002/mus.24463.
Nyland J, Gamble C, Franklin T, Caborn DNM. Permanent knee sensorimotor system changes following ACL injury and surgery. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1461–74. https://doi.org/10.1007/s00167-017-4432-y.
Weinhandl JT, Earl-Boehm JE, Ebersole KT, Huddleston WE, Armstrong BS, O’Connor KM. Anticipatory effects on anterior cruciate ligament loading during sidestep cutting. Clin Biomech (Bristol, Avon). 2013;28(6):655–63. https://doi.org/10.1016/j.clinbiomech.2013.06.001.
van Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review G. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976). 2003;28(12):1290–9. https://doi.org/10.1097/01.BRS.0000065484.95996.AF.
Kuenze C, Pietrosimone B, Lisee C, Rutherford M, Birchmeier T, Lepley A, et al. Demographic and surgical factors affect quadriceps strength after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):921–30. https://doi.org/10.1007/s00167-018-5215-9.
Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD. The influence of graft choice on isokinetic muscle strength 4–24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):768–80. https://doi.org/10.1007/s00167-010-1357-0.
Harput G, Soylu AR, Ertan H, Ergun N, Mattacola CG. Effect of gender on the quadriceps-to-hamstrings coactivation ratio during different exercises. J Sport Rehabil. 2014;23(1):36–43. https://doi.org/10.1123/jsr.2012-0120.
Blackburn JT, Bell DR, Norcross MF, Hudson JD, Engstrom LA. Comparison of hamstring neuromechanical properties between healthy males and females and the influence of musculotendinous stiffness. J Electromyogr Kinesiol. 2009;19(5):e362–9. https://doi.org/10.1016/j.jelekin.2008.08.005.
Acknowledgements
The authors would like to acknowledge all participants who contributed to the original research reviewed in this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
David Sherman, Neal Glaviano and Grant Norte declare that they have no conflicts of interest relevant to the content of this review.
Standards of reporting
PRISMA.
Ethics approval
This is a systematic review. The University of Toledo Institutional Review Board for Biomedical Research has confirmed that no ethical approval is required.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
All authors (DAS, NRG, and GEN) have contributed equally and demonstrated significant involvement in the planning and carrying out of this review and manuscript. Material preparation and data extraction were performed by DAS. Methodological quality review was performed by DAS and NRG. Data analysis was performed by DAS. The first draft of the manuscript was written by DAS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sherman, D.A., Glaviano, N.R. & Norte, G.E. Hamstrings Neuromuscular Function After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Med 51, 1751–1769 (2021). https://doi.org/10.1007/s40279-021-01433-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01433-w