Abstract
Background
Hamstrings muscle morphology is determinant of muscle function (i.e. strength). Among individuals with ACL reconstruction (ACLR), less cross-sectional area (CSA) and volume in the ACLR-limb are associated with muscle weakness, and may contribute to lower rates of return to preinjury activity level and an increased risk for long-term sequelae.
Objectives
To effectively treat muscular impairments, an accurate understanding of differences in hamstrings morphology following ACLR is needed. A systematic review and meta-analysis were undertaken to describe the morphology of the hamstring muscle complex after ACLR.
Methods
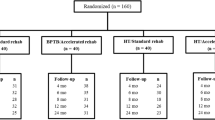
We searched five databases for studies evaluating the difference between hamstrings size and architecture in individuals with ACLR. Two independent reviewers assessed each paper for inclusion and quality. Means and standard deviations were extracted from each included study to allow fixed-effect size meta-analysis calculations for comparison of results.
Results
Twenty-four studies were included for final review. Eight categories of morphological outcomes were identified, and studies were grouped accordingly: (1) volume, (2) cross-sectional area (CSA), (3) muscle length, (4) muscle thickness, (5) fascicle length, (6) pennation angle, (7) fiber area, and (8) fiber type. Meta-analysis demonstrated lower hamstrings volume in the ACLR-limb in both contralateral and control group comparisons, and lower CSA, length, and thickness in the ACLR-limb in contralateral comparisons. The semitendinosus and gracilis were most profoundly impacted. Limited moderate evidence demonstrated greater biceps femoris pennation angle in the ACLR-limb.
Conclusions
Individuals with ACLR demonstrated large deficits in semitendinosus and gracilis muscle CSA and volume in the ACLR-limb compared contralaterally, with no differences observed in the biceps femoris or semimembranosus. Clinical implications regarding assessment and treatment of individuals with ACLR are discussed.






Similar content being viewed by others
References
MacWilliams BA, Wilson DR, DesJardins JD, Romero J, Chao EY. Hamstrings cocontraction reduces internal rotation, anterior translation, and anterior cruciate ligament load in weight-bearing flexion. J Orthop Res. 1999;17(6):817–22. https://doi.org/10.1002/jor.1100170605.
Norte GE, Goetschius JW, Slater LV, Hart JM. Influence of patient demographics and surgical characteristics on pass rates of return-to-activity tests in anterior cruciate ligament-reconstructed patients before physician clearance. Clin J Sport Med. 2020. https://doi.org/10.1097/JSM.0000000000000790 (Publish Ahead of Print).
Palmieri-Smith RM, Strickland M, Lepley LK. Hamstring muscle activity after primary anterior cruciate ligament reconstruction-a protective mechanism in those who do not sustain a secondary injury? a preliminary study. Sports Health. 2019;11(4):316–23. https://doi.org/10.1177/1941738119852630.
Sherman D, Birchmeier T, Kuenze CM, Garrison C, Hannon J, Bothwell J, et al. Thigh-muscle and patient-reported function early after anterior cruciate ligament reconstruction: clinical cutoffs unique to graft type and age. J Athl Train. 2020;55(8):826–33. https://doi.org/10.4085/1062-6050-370-19.
Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–51. https://doi.org/10.1136/bjsports-2015-095908.
Norte GE, Knaus KR, Kuenze C, Handsfield GG, Meyer CH, Blemker SS, et al. MRI-based assessment of lower-extremity muscle volumes in patients before and after ACL reconstruction. J Sport Rehabil. 2018;27(3):201–12. https://doi.org/10.1123/jsr.2016-0141.
Snow BJ, Wilcox JJ, Burks RT, Greis PE. Evaluation of muscle size and fatty infiltration with MRI nine to eleven years following hamstring harvest for ACL reconstruction. J Bone Jt Surg Am. 2012;94(14):1274–82. https://doi.org/10.2106/JBJS.K.00692.
Nomura Y, Kuramochi R, Fukubayashi T. Evaluation of hamstring muscle strength and morphology after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2015;25(3):301–7. https://doi.org/10.1111/sms.12205.
Rush JL, Norte GE, Lepley AS. Limb differences in hamstring muscle function and morphology after anterior cruciate ligament reconstruction. Phys Ther Sport. 2020;45:168–75. https://doi.org/10.1016/j.ptsp.2020.06.012.
Makihara Y, Nishino A, Fukubayashi T, Kanamori A. Decrease of knee flexion torque in patients with ACL reconstruction: combined analysis of the architecture and function of the knee flexor muscles. Knee Surg Sports Traumatol Arthrosc. 2006;14(4):310–7. https://doi.org/10.1007/s00167-005-0701-2.
Konishi Y, Fukubayashi T. Relationship between muscle volume and muscle torque of the hamstrings after anterior cruciate ligament reconstruction. J Sci Med Sport. 2010;13(1):101–5. https://doi.org/10.1016/j.jsams.2008.08.001.
Konrath JM, Vertullo CJ, Kennedy BA, Bush HS, Barrett RS, Lloyd DG. Morphologic characteristics and strength of the hamstring muscles remain altered at 2 years after use of a hamstring tendon graft in anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(10):2589–98. https://doi.org/10.1177/0363546516651441.
Tengman E, Brax Olofsson L, Stensdotter AK, Nilsson KG, Hager CK. Anterior cruciate ligament injury after more than 20 years. II. Concentric and eccentric knee muscle strength. Scand J Med Sci Sports. 2014;24(6):e501–9. https://doi.org/10.1111/sms.12215.
Janssen RP, van der Velden MJ, Pasmans HL, Sala HA. Regeneration of hamstring tendons after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):898–905. https://doi.org/10.1007/s00167-012-2125-0.
Viola RW, Sterett WI, Newfield D, Steadman JR, Torry MR. Internal and external tibial rotation strength after anterior cruciate ligament reconstruction using ipsilateral semitendinosus and gracilis tendon autografts. Am J Sports Med. 2000;28(4):552–5. https://doi.org/10.1177/03635465000280041801.
Tsifountoudis I, Bisbinas I, Kalaitzoglou I, Markopoulos G, Haritandi A, Dimitriadis A, et al. The natural history of donor hamstrings unit after anterior cruciate ligament reconstruction: a prospective MRI scan assessment. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1583–90. https://doi.org/10.1007/s00167-015-3732-3.
Timmins RG, Bourne MN, Shield AJ, Williams MD, Lorenzen C, Opar DA. Biceps femoris architecture and strength in athletes with a previous anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2016;48(3):337–45. https://doi.org/10.1249/MSS.0000000000000783.
Messer DJ, Shield AJ, Williams MD, Timmins RG, Bourne MN. Hamstring muscle activation and morphology are significantly altered 1–6 years after anterior cruciate ligament reconstruction with semitendinosus graft. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):733–41. https://doi.org/10.1007/s00167-019-05374-w.
Eriksson K, Hamberg P, Jansson E, Larsson H, Shalabi A, Wredmark T. Semitendinosus muscle in anterior cruciate ligament surgery: Morphology and function. Arthroscopy. 2001;17(8):808–17. https://doi.org/10.1016/s0749-8063(01)90003-9.
Hootman JM, Driban JB, Sitler MR, Harris KP, Cattano NM. Reliability and validity of three quality rating instruments for systematic reviews of observational studies. Res Synth Methods. 2011;2(2):110–8. https://doi.org/10.1002/jrsm.41.
Open-Source. Engauge digitizer software. In: Mitchell M, Muftakhidinov B, Winchen T, van Schaik B, Wilms A, Kensington, et al., editors.: GitHub; 2015. p. Windows 10.
Kellis E, Karagiannidis E, Patsika G. Patellar tendon and hamstring moment-arms and cross-sectional area in patients with anterior cruciate ligament reconstruction and controls. Comput Methods Biomech Biomed Engin. 2015;18(10):1083–9. https://doi.org/10.1080/10255842.2013.869323.
Hedges L, Olkin I. Statistical methods for meta-analysis. Orlando: Academic Press; 1985.
van Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review G. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976). 2003;28(12):1290–9. https://doi.org/10.1097/01.BRS.0000065484.95996.AF.
Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, LaStayo PC. Effects of early progressive eccentric exercise on muscle structure after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2007;89(3):559–70. https://doi.org/10.2106/JBJS.F.00385.
Irie K, Tomatsu T. Atrophy of semitendinosus and gracilis and flexor mechanism function after hamstring tendon harvest for anterior cruciate ligament reconstruction. Orthopedics. 2002;25(5):491–5. https://doi.org/10.3928/0147-7447-20020501-15.
Karagiannidis E, Kellis E, Galanis N, Vasilios B. Semitendinosus muscle architecture during maximum isometric contractions in individuals with anterior cruciate ligament reconstruction and controls. Muscles Ligaments Tendons J. 2017;7(1):147–51. https://doi.org/10.11138/mltj/2017.7.1.147.
Nishino A, Sanada A, Kanehisa H, Fukubayashi T. Knee-flexion torque and morphology of the semitendinosus after ACL reconstruction. Med Sci Sports Exerc. 2006;38(11):1895–900. https://doi.org/10.1249/01.mss.0000230344.71623.51.
Burks RT, Crim J, Fink BP, Boylan DN, Greis PE. The effects of semitendinosus and gracilis harvest in anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(10):1177–85. https://doi.org/10.1016/j.arthro.2005.07.005.
Setuain I, Izquierdo M, Idoate F, Bikandi E, Gorostiaga EM, Aagaard P, et al. Differential effects of 2 rehabilitation programs following anterior cruciate ligament reconstruction. J Sport Rehabil. 2017;26(6):544–55. https://doi.org/10.1123/jsr.2016-0065.
Williams GN, Snyder-Mackler L, Barrance PJ, Axe MJ, Buchanan TS. Muscle and tendon morphology after reconstruction of the anterior cruciate ligament with autologous semitendinosus-gracilis graft. J Bone Joint Surg Am. 2004;86(9):1936–46. https://doi.org/10.2106/00004623-200409000-00012.
Gandolfi M, Ricci M, Sambugaro E, Vale N, Dimitrova E, Meschieri A, et al. Changes in the sensorimotor system and semitendinosus muscle morphometry after arthroscopic anterior cruciate ligament reconstruction: a prospective cohort study with 1-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3770–9. https://doi.org/10.1007/s00167-018-5020-5.
Yoshii R, Konishi Y, Ando D, Ochiai S, Hagino T, Dobashi S. Effect of subcutaneous tissue on changes in thigh circumference following anterior cruciate ligament reconstruction. Int J Sports Med. 2019;40(8):544–50. https://doi.org/10.1055/a-0893-5838.
Arangio GA, Chen C, Kalady M, Reed JF 3rd. Thigh muscle size and strength after anterior cruciate ligament reconstruction and rehabilitation. J Orthop Sports Phys Ther. 1997;26(5):238–43. https://doi.org/10.2519/jospt.1997.26.5.238.
Rebai H, Barra V, Laborde A, Bonny JM, Poumarat G, Coudert J. Effects of two electrical stimulation frequencies in thigh muscle after knee surgery. Int J Sports Med. 2002;23(8):604–9. https://doi.org/10.1055/s-2002-35525.
Takeda Y, Kashiwaguchi S, Matsuura T, Higashida T, Minato A. Hamstring muscle function after tendon harvest for anterior cruciate ligament reconstruction: evaluation with T2 relaxation time of magnetic resonance imaging. Am J Sports Med. 2006;34(2):281–8. https://doi.org/10.1177/0363546505279574.
Flaxman TE, Alkjaer T, Simonsen EB, Krogsgaard MR, Benoit DL. Predicting the functional roles of knee joint muscles from internal joint moments. Med Sci Sports Exerc. 2017;49(3):527–37. https://doi.org/10.1249/MSS.0000000000001125.
Bourne MN, Opar DA, Williams MD, Shield AJ. Eccentric knee flexor strength and risk of hamstring injuries in rugby union: a prospective study. Am J Sports Med. 2015;43(11):2663–70. https://doi.org/10.1177/0363546515599633.
Pollard CW, Opar DA, Williams MD, Bourne MN, Timmins RG. Razor hamstring curl and Nordic hamstring exercise architectural adaptations: Impact of exercise selection and intensity. Scand J Med Sci Sports. 2019;29(5):706–15. https://doi.org/10.1111/sms.13381.
Bourne MN, Williams MD, Opar DA, Al Najjar A, Kerr GK, Shield AJ. Impact of exercise selection on hamstring muscle activation. Br J Sports Med. 2017;51(13):1021–8. https://doi.org/10.1136/bjsports-2015-095739.
Bourne MN, Timmins RG, Opar DA, Pizzari T, Ruddy JD, Sims C, et al. An evidence-based framework for strengthening exercises to prevent hamstring injury. Sports Med. 2018;48(2):251–67. https://doi.org/10.1007/s40279-017-0796-x.
Abe T, Loenneke JP, Thiebaud RS. Ultrasound assessment of hamstring muscle size using posterior thigh muscle thickness. Clin Physiol Funct Imaging. 2016;36(3):206–10. https://doi.org/10.1111/cpf.12214.
Palmer TB, Akehi K, Thiele RM, Smith DB, Thompson BJ. Reliability of panoramic ultrasound imaging in simultaneously examining muscle size and quality of the hamstring muscles in young, healthy males and females. Ultrasound Med Biol. 2015;41(3):675–84. https://doi.org/10.1016/j.ultrasmedbio.2014.10.011.
Opar DA, Serpell BG. Is there a potential relationship between prior hamstring strain injury and increased risk for future anterior cruciate ligament injury? Arch Phys Med Rehabil. 2014;95(2):401–5.
Timmins RG, Bourne MN, Shield AJ, Williams MD, Lorenzen C, Opar DA. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med. 2016;50(24):1524–35. https://doi.org/10.1136/bjsports-2015-095362.
Timmins RG, Ruddy JD, Presland J, Maniar N, Shield AJ, Williams MD, et al. Architectural changes of the biceps femoris long head after concentric or eccentric training. Med Sci Sports Exerc. 2016;48(3):499–508. https://doi.org/10.1249/MSS.0000000000000795.
Lisee C, Lepley AS, Birchmeier T, O’Hagan K, Kuenze C. Quadriceps strength and volitional activation after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Sports Health. 2019;11(2):163–79. https://doi.org/10.1177/1941738118822739.
Hiemstra LA, Webber S, MacDonald PB, Kriellaars DJ. Contralateral limb strength deficits after anterior cruciate ligament reconstruction using a hamstring tendon graft. Clin Biomech (Bristol, Avon). 2007;22(5):543–50. https://doi.org/10.1016/j.clinbiomech.2007.01.009.
Kuenze C, Pietrosimone B, Lisee C, Rutherford M, Birchmeier T, Lepley A, et al. Demographic and surgical factors affect quadriceps strength after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):921–30. https://doi.org/10.1007/s00167-018-5215-9.
Acknowledgements
The authors would like to acknowledge all participants that contributed to the original research reviewed in this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflicts of Interest
David Sherman, Justin Rush, Neal Glaviano and Grant Norte declare that they have no conflicts of interest relevant to the content of this review.
Standards of reporting
PRISMA
Ethics approval
This is a systematic review. The University of Toledo Institutional Review Board for Biomedical Research has confirmed that no ethical approval is required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Authors' contributions
All authors (DAS, JLR, NRG, and GEN) have contributed equally and demonstrated significant involvement in the planning and carrying out of this review and manuscript. Material preparation and data extraction were performed by David Sherman. Methodological quality review was performed by David Sherman and Justin Rush. Data analysis was performed by David Sherman. The first draft of the manuscript was written by David Sherman and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sherman, D.A., Rush, J.L., Glaviano, N.R. et al. Hamstrings Muscle Morphology After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Med 51, 1733–1750 (2021). https://doi.org/10.1007/s40279-021-01431-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01431-y