Abstract
The management of neonatal sepsis is challenging owing to complex developmental and environmental factors that contribute to inter-individual variability in the pharmacokinetics and pharmacodynamics of many antimicrobial agents. In this review, we describe (i) the changing epidemiology of early- and late-onset neonatal sepsis; (ii) the pharmacologic considerations that influence the safety and efficacy of antibacterials, antifungals, and immunomodulatory adjuvants; and (iii) the recommended dosing regimens for pharmacologic agents commonly used in the treatment and prevention of neonatal sepsis. Neonatal sepsis is marked by high morbidity and mortality, such that prompt initiation of antimicrobial therapy is essential following culture collection. Before culture results are available, combination therapy with ampicillin and an aminoglycoside is recommended. When meningitis is suspected, ampicillin and cefotaxime may be considered. Following identification of the causative organism and in vitro susceptibility testing, antimicrobial therapy may be narrowed to provide targeted coverage. Therapeutic drug monitoring should be considered for neonates receiving vancomycin or aminoglycoside therapies. For neonates with invasive fungal infections, the development of new antifungal agents has significantly improved therapeutic outcomes in recent years. Liposomal amphotericin B has been found to be safe and efficacious in patients with renal impairment or toxicity caused by conventional amphotericin B. Antifungal prophylaxis with fluconazole has also been reported to dramatically reduce rates of neonatal invasive fungal infections and to improve long-term neurodevelopmental outcomes among treated children. Additionally, several large multicenter studies are currently investigating the safety and efficacy of oral lactoferrin as an immunoprophylactic agent for the prevention of neonatal sepsis.

Similar content being viewed by others
References
Bizzarro MJ, Raskind C, Baltimore RS, Gallagher PG. Seventy-five years of neonatal sepsis at Yale: 1928–2003. Pediatrics. 2005;116(3):595–602.
Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004;292(19):2357–65.
Klein J. Bacterial sepsis and meningitis. Philadelphia: WB Saunders; 2001.
Cohen-Wolkowiez M, Moran C, Benjamin DK, Cotten CM, Clark RH, Benjamin DK Jr, et al. Early and late onset sepsis in late preterm infants. Pediatr Infect Dis J. 2009;28(12):1052–6.
Stoll BJ, Hansen NI, Sanchez PJ, Faix RG, Poindexter BB, Van Meurs KP, et al. Early onset neonatal sepsis: the burden of group B streptococcal and E. coli disease continues. Pediatrics. 2011;127(5):817–26.
Andrews WW, Schelonka R, Waites K, Stamm A, Cliver SP, Moser S. Genital tract methicillin-resistant Staphylococcus aureus: risk of vertical transmission in pregnant women. Obstet Gynecol. 2008;111(1):113–8.
Kaufman D, Fairchild KD. Clinical microbiology of bacterial and fungal sepsis in very-low-birth-weight infants. Clin Microbiol Rev. 2004;17(3):638–80.
Vergnano S, Menson E, Kennea N, Embleton N, Russell AB, Watts T, et al. Neonatal infections in England: the NeonIN surveillance network. Arch Dis Child Fetal Neonatal Ed. 2011;96(1):F9–14.
Nizet V, Klein JO. Bacterial sepsis and meningitis. In: Remington JS, Klein JO, Wilson CB, et al., editors. Infectious diseases of the fetus and newborn infant. 7th ed. Philadelphia: Elsevier Saunders; 2011. p. 222–75.
Johnson PJ. Neonatal pharmacology–pharmacokinetics. Neonatal Netw. 2011;30(1):54–61.
Yaffe S, Aranda JV. Neonatal and pediatric pharmacology: therapeutic principles in practice. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2010.
Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med. 2003;349(12):1157–67.
Friis-Hansen B. Body water compartments in children: changes during growth and related changes in body composition. Pediatrics. 1961;28:169–81.
Anderson GD, Lynn AM. Optimizing pediatric dosing: a developmental pharmacologic approach. Pharmacotherapy. 2009;29(6):680–90.
Ambrose PG, Bhavnani SM, Rubino CM, Louie A, Gumbo T, Forrest A, et al. Pharmacokinetics–pharmacodynamics of antimicrobial therapy: it’s not just for mice anymore. Clin Infect Dis. 2007;44(1):79–86.
Paap CM, Nahata MC. Clinical pharmacokinetics of antibacterial drugs in neonates. Clin Pharmacokinet. 1990;19(4):280–318.
Ljungberg B, Nilsson-Ehle I. Pharmacokinetics of antimicrobial agents in the elderly. Rev Infect Dis. 1987;9(2):250–64.
Neely MN, Reed MD. The pharmacokinetic–pharmacodynamic basis of optimal antibiotic dosing. In: Long S, Pickering L, Prober C, editors. Principles and practices of pediatric infectious diseases. 4th ed. Philadelphia: Elsevier Saunders; 2011.
Buxton ILO, Benet LZ. Pharmacokinetics: the dynamics of drug absorption, distribution, and elimination. In: Brunton L, Chabner B, Knollman B, editors. Goodman and Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill; 2011. p. 17–39.
van den Anker JN. Developmental pharmacology. Dev Disabil Res Rev. 2010;16(3):233–8.
Gupta M, Brans YW. Gastric retention in neonates. Pediatrics. 1978;62(1):26–9.
Koren G. Therapeutic drug monitoring principles in the neonate. National Academy of Clinical Biochemistry. Clin Chem. 1997;43(1):222–7.
Huang NN, High RH. Comparison of serum levels following the administration of oral and parenteral preparations of penicillin to infants and children of various age groups. J Pediatr. 1953;42(6):657–8.
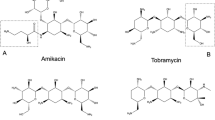
Touw DJ, Westerman EM, Sprij AJ. Therapeutic drug monitoring of aminoglycosides in neonates. Clin Pharmacokinet. 2009;48(2):71–88.
Kadambari S, Heath PT, Sharland M, Lewis S, Nichols A, Turner MA. Variation in gentamicin and vancomycin dosage and monitoring in UK neonatal units. J Antimicrob Chemother. 2011;66(11):2647–50.
Siber GR, Echeverria P, Smith AL, Paisley JW, Smith DH. Pharmacokinetics of gentamicin in children and adults. J Infect Dis. 1975;132(6):637–51.
Windorfer A, Kuenzer W, Urbanek R. The influence of age on the activity of acetylsalicylic acid-esterase and protein-salicylate binding. Eur J Clin Pharmacol. 1974;7(3):227–31.
Ehrnebo M, Agurell S, Jalling B, Boreus LO. Age differences in drug binding by plasma proteins: studies on human foetuses, neonates and adults. Eur J Clin Pharmacol. 1971;3(4):189–93.
Lees P, Shojaee Aliabadi F. Rational dosing of antimicrobial drugs: animals versus humans. Int J Antimicrob Agents. 2002;19(4):269–84.
Cuzzolin L. Drug metabolizing enzymes in the perinatal and neonatal period: differences in the expression and activity. Curr Drug Metab. 2013;14(2):167–73.
Lacroix D, Sonnier M, Moncion A, Cheron G, Cresteil T. Expression of CYP3A in the human liver—evidence that the shift between CYP3A7 and CYP3A4 occurs immediately after birth. Eur J Biochem. 1997;247(2):625–34.
de Wildt SN, Kearns GL, Leeder JS, van den Anker JN. Cytochrome P450 3A: ontogeny and drug disposition. Clin Pharmacokinet. 1999;37(6):485–505.
Rakhmanina NY, van den Anker JN. Pharmacological research in pediatrics: from neonates to adolescents. Adv Drug Deliv Rev. 2006;58(1):4–14.
Sonntag J, Prankel B, Waltz S. Serum creatinine concentration, urinary creatinine excretion and creatinine clearance during the first 9 weeks in preterm infants with a birth weight below 1500 g. Eur J Pediatr. 1996;155(9):815–9.
Rhodin MM, Anderson BJ, Peters AM, Coulthard MG, Wilkins B, Cole M, et al. Human renal function maturation: a quantitative description using weight and postmenstrual age. Pediatr Nephrol. 2009;24(1):67–76.
Allegaert K, Anderson BJ, van den Anker JN, Vanhaesebrouck S, de Zegher F. Renal drug clearance in preterm neonates: relation to prenatal growth. Ther Drug Monitor. 2007;29(3):284–91.
Nierenberg DW. Drug inhibition of penicillin tubular secretion: concordance between in vitro and clinical findings. J Pharmacol Exp Ther. 1987;240(3):712–6.
Hayton WL. Maturation and growth of renal function: dosing renally cleared drugs in children. AAPS PharmSci. 2000;2(1):E3.
Gilman JT. Therapeutic drug monitoring in the neonate and paediatric age group. Problems and clinical pharmacokinetic implications. Clin Pharmacokinet. 1990;19(1):1–10.
de Hoog M, Mouton JW, van den Anker JN. New dosing strategies for antibacterial agents in the neonate. Semin Fetal Neonatal Med. 2005;10(2):185–94.
Waites KB, Sims PJ, Crouse DT, Geerts MH, Shoup RE, Hamrick WB, et al. Serum concentrations of erythromycin after intravenous infusion in preterm neonates treated for Ureaplasma urealyticum infection. Pediatr Infect Dis J. 1994;13(4):287–93.
Healy CM, Hulten KG, Palazzi DL, Campbell JR, Baker CJ. Emergence of new strains of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Clin Infect Dis. 2004;39(10):1460–6.
Dotis J, Iosifidis E, Ioannidou M, Roilides E. Use of linezolid in pediatrics: a critical review. Int J Infect Dis. 2010;14(8):e638–48.
Deville JG, Adler S, Azimi PH, Jantausch BA, Morfin MR, Beltran S, et al. Linezolid versus vancomycin in the treatment of known or suspected resistant gram-positive infections in neonates. Pediatr Infect Dis J. 2003;22(9 Suppl):S158–63.
Clissold SP, Todd PA, Campoli-Richards DM. Imipenem/cilastatin. A review of its antibacterial activity, pharmacokinetic properties and therapeutic efficacy. Drugs. 1987;33(3):183–241.
Blumer JL, Reed MD, Kearns GL, Jacobs RF, Gooch WM 3rd, Yogev R, et al. Sequential, single-dose pharmacokinetic evaluation of meropenem in hospitalized infants and children. Antimicrob Agents Chemother. 1995;39(8):1721–5.
Clark RH, Bloom BT, Spitzer AR, Gerstmann DR. Empiric use of ampicillin and cefotaxime, compared with ampicillin and gentamicin, for neonates at risk for sepsis is associated with an increased risk of neonatal death. Pediatrics. 2006;117(1):67–74.
Cotten CM, McDonald S, Stoll B, Goldberg RN, Poole K, Benjamin DK Jr. The association of third-generation cephalosporin use and invasive candidiasis in extremely low birth-weight infants. Pediatrics. 2006;118(2):717–22.
Mustafa MM, McCracken GH Jr. Antimicrobial agents in pediatrics. Infect Dis Clin N Am. 1989;3(3):491–506.
National Institute of Health and Clinical Excellence (NICE) Clinical Guideline. Antibiotics for early-onset neonatal infection: antibiotics for the prevention and treatment of early-onset neonatal infection. 2012. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0051825/. Accessed 1 Sept 2013
Schelonka RL, Chai MK, Yoder BA, Hensley D, Brockett RM, Ascher DP. Volume of blood required to detect common neonatal pathogens. J Pediatr. 1996;129(2):275–8.
Kellogg JA, Ferrentino FL, Goodstein MH, Liss J, Shapiro SL, Bankert DA. Frequency of low level bacteremia in infants from birth to two months of age. Pediatr Infect Dis J. 1997;16(4):381–5.
Polin RA. The “ins and outs” of neonatal sepsis. J Pediatr. 2003;143(1):3–4.
Kumar Y, Qunibi M, Neal TJ, Yoxall CW. Time to positivity of neonatal blood cultures. Arch Dis Child Fetal Neonatal Ed. 2001;85(3):F182–6.
Pichichero ME, Todd JK. Detection of neonatal bacteremia. J Pediatr. 1979;94(6):958–60.
Red Book. 2012 Report of the committee on infectious diseases. Elk Grove: American Academy of Pediatrics; 2012.
El Desoky ES, Sheikh AA, Al Hammadi AY. Aminoglycoside and vancomycin serum concentration monitoring and mortality due to neonatal sepsis in Saudi Arabia. J Clin Pharm Ther. 2003;28(6):479–83.
de Hoog M, Schoemaker RC, Mouton JW, van den Anker JN. Vancomycin population pharmacokinetics in neonates. Clin Pharm Ther. 2000;67(4):360–7.
Rybak M, Lomaestro B, Rotschafer JC, Moellering R Jr, Craig W, Billeter M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2009;66(1):82–98.
Richardson MD. Changing patterns and trends in systemic fungal infections. J Antimicrob Chemother. 2005;56(Suppl 1):i5–11.
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110(2 Pt 1):285–91.
Langan EA, Agarwal RP, Subudhi CP, Judge MR. Aspergillus fumigatus: a potentially lethal ubiquitous fungus in extremely low birthweight neonates. Pediatr Dermatol. 2010;27(4):403–4.
Roilides E, Zaoutis TE, Walsh TJ. Invasive zygomycosis in neonates and children. Clin Microbiol Infect. 2009;15(Suppl 5):50–4.
Benjamin DK Jr, DeLong ER, Steinbach WJ, Cotton CM, Walsh TJ, Clark RH. Empirical therapy for neonatal candidemia in very low birth weight infants. Pediatrics. 2003;112(3 Pt 1):543–7.
Benjamin DK Jr, Stoll BJ, Gantz MG, Walsh MC, Sanchez PJ, Das A, et al. Neonatal candidiasis: epidemiology, risk factors, and clinical judgment. Pediatrics. 2010;126(4):e865–73.
Procianoy RS, Eneas MV, Silveira RC. Empiric guidelines for treatment of Candida infection in high-risk neonates. Eur J Pediatr. 2006;165(6):422–3.
van den Anker JN, van Popele NM, Sauer PJ. Antifungal agents in neonatal systemic candidiasis. Antimicrob Agents Chemother. 1995;39(7):1391–7.
Juster-Reicher A, Leibovitz E, Linder N, Amitay M, Flidel-Rimon O, Even-Tov S, et al. Liposomal amphotericin B (AmBisome) in the treatment of neonatal candidiasis in very low birth weight infants. Infection. 2000;28(4):223–6.
Baley JE, Meyers C, Kliegman RM, Jacobs MR, Blumer JL. Pharmacokinetics, outcome of treatment, and toxic effects of amphotericin B and 5-fluorocytosine in neonates. J Pediatr. 1990;116(5):791–7.
Grant SM, Clissold SP. Fluconazole. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in superficial and systemic mycoses. Drugs. 1990;39(6):877–916.
Fasano C, O’Keeffe J, Gibbs D. Fluconazole treatment of neonates and infants with severe fungal infections not treatable with conventional agents. Eur J Clin Microbiol Infect Dis. 1994;13(4):351–4.
Walsh TJ, Adamson PC, Seibel NL, Flynn PM, Neely MN, Schwartz C, et al. Pharmacokinetics, safety, and tolerability of caspofungin in children and adolescents. Antimicrob Agents Chemother. 2005;49(11):4536–45.
Hope WW, Seibel NL, Schwartz CL, Arrieta A, Flynn P, Shad A, et al. Population pharmacokinetics of micafungin in pediatric patients and implications for antifungal dosing. Antimicrob Agents Chemother. 2007;51(10):3714–9.
Smith PB, Walsh TJ, Hope W, Arrieta A, Takada A, Kovanda LL, et al. Pharmacokinetics of an elevated dosage of micafungin in premature neonates. Pediatr Infect Dis J. 2009;28(5):412–5.
Hope WW, Smith PB, Arrieta A, Buell DN, Roy M, Kaibara A, et al. Population pharmacokinetics of micafungin in neonates and young infants. Antimicrob Agents Chemother. 2010;54(6):2633–7.
Pappas PG, Rex JH, Sobel JD, Filler SG, Dismukes WE, Walsh TJ, et al. Guidelines for treatment of candidiasis. Clin Infect Dis. 2004;38(2):161–89.
Azizia M, Lloyd J, Allen M, Klein N, Peebles D. Immune status in very preterm neonates. Pediatrics. 2012;129(4):e967–74.
Ballow M, Cates KL, Rowe JC, Goetz C, Desbonnet C. Development of the immune system in very low birth weight (less than 1500 g) premature infants: concentrations of plasma immunoglobulins and patterns of infections. Pediatr Res. 1986;20(9):899–904.
Locksmith G, Duff P. Infection, antibiotics, and preterm delivery. Semin Perinatol. 2001;25(5):295–309.
Hill HR. Intravenous immunoglobulin use in the neonate: role in prophylaxis and therapy of infection. Pediatr Infect Dis J. 1993;12(7):549–58 (quiz 59).
Ohlsson A, Lacy JB. Intravenous immunoglobulin for suspected or subsequently proven infection in neonates. Cochrane Database Syst Rev. 2004;(1):CD001239.
Ohlsson A, Lacy JB. Intravenous immunoglobulin for preventing infection in preterm and/or low-birth-weight infants. Cochrane Database Syst Rev. 2004;(1):CD000361.
Baley JE. Neonatal sepsis: the potential for immunotherapy. Clin Perinatol. 1988;15(4):755–71.
Christensen RD, Brown MS, Hall DC, Lassiter HA, Hill HR. Effect on neutrophil kinetics and serum opsonic capacity of intravenous administration of immune globulin to neonates with clinical signs of early-onset sepsis. J Pediatr. 1991;118(4 Pt 1):606–14.
Mohan PV, Tarnow-Mordi W, Stenson B, Brocklehurst P, Haque K, Cavendish V, et al. Can polyclonal intravenous immunoglobulin limit cytokine mediated cerebral damage and chronic lung disease in preterm infants? Arch Dis Child Fetal Neonatal Ed. 2004;89(1):F5–8.
Alejandria MM, Lansang MA, Dans LF, Mantaring JB. Intravenous immunoglobulin for treating sepsis and septic shock. Cochrane Database Syst Rev. 2002;(1):CD001090.
Brocklehurst P, Farrell B, King A, Juszczak E, Darlow B, Haque K, et al. Treatment of neonatal sepsis with intravenous immune globulin. N Engl J Med. 2011;365(13):1201–11.
al-Mulla ZS, Christensen RD. Neutropenia in the neonate. Clin Perinatol. 1995;22(3):711–39.
Rodwell RL, Taylor KM, Tudehope DI, Gray PH. Hematologic scoring system in early diagnosis of sepsis in neutropenic newborns. Pediatr Infect Dis J. 1993;12(5):372–6.
Davies EG. The immunology of neonates and children and its relation to susceptibility to infection. London: Springer; 2008.
Sachs UJ, Reiter A, Walter T, Bein G, Woessmann W. Safety and efficacy of therapeutic early onset granulocyte transfusions in pediatric patients with neutropenia and severe infections. Transfusion. 2006;46(11):1909–14.
Pammi M, Brocklehurst P. Granulocyte transfusions for neonates with confirmed or suspected sepsis and neutropenia. Cochrane Database Syst Rev. 2011;(10):CD003956.
Saez-Llorens X, McCracken GH Jr. Bacterial meningitis in children. Lancet. 2003;361(9375):2139–48.
Goldmann DA, Durbin WA Jr, Freeman J. Nosocomial infections in a neonatal intensive care unit. J Infect Dis. 1981;144(5):449–59.
Sande MA, Tauber MG, Scheld WM, McCracken GH Jr. Pathophysiology of bacterial meningitis: summary of the workshop. Pediatr Infect Dis J. 1989;8(12):929–33.
Saravolatz LD, Manzor O, VanderVelde N, Pawlak J, Belian B. Broad-range bacterial polymerase chain reaction for early detection of bacterial meningitis. Clin Infect Dis. 2003;36(1):40–5.
Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267–84.
El Bashir H, Laundy M, Booy R. Diagnosis and treatment of bacterial meningitis. Arch Dis Child. 2003;88(7):615–20.
Quagliarello VJ, Scheld WM. Treatment of bacterial meningitis. N Engl J Med. 1997;336(10):708–16.
Renier D, Flandin C, Hirsch E, Hirsch JF. Brain abscesses in neonates. A study of 30 cases. J Neurosurg. 1988;69(6):877–82.
Graham DR, Band JD. Citrobacter diversus brain abscess and meningitis in neonates. JAMA. 1981;245(19):1923–5.
Schrag SJ, Zywicki S, Farley MM, Reingold AL, Harrison LH, Lefkowitz LB, et al. Group B streptococcal disease in the era of intrapartum antibiotic prophylaxis. N Engl J Med. 2000;342(1):15–20.
Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep. 2002;51(RR-11):1–22.
Van Dyke MK, Phares CR, Lynfield R, Thomas AR, Arnold KE, Craig AS, et al. Evaluation of universal antenatal screening for group B streptococcus. N Engl J Med. 2009;360(25):2626–36.
Verani JR, McGee L, Schrag SJ. Prevention of perinatal group B streptococcal disease—revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010;59(RR-10):1–36.
Jordan HT, Farley MM, Craig A, Mohle-Boetani J, Harrison LH, Petit S, et al. Revisiting the need for vaccine prevention of late-onset neonatal group B streptococcal disease: a multistate, population-based analysis. Pediatr Infect Dis J. 2008;27(12):1057–64.
Baker CJ, Edwards MS. Group B streptococcal conjugate vaccines. Arch Dis Child. 2003;88(5):375–8.
Benjamin DK Jr, Stoll BJ, Fanaroff AA, McDonald SA, Oh W, Higgins RD, et al. Neonatal candidiasis among extremely low birth weight infants: risk factors, mortality rates, and neurodevelopmental outcomes at 18 to 22 months. Pediatrics. 2006;117(1):84–92.
Kaufman DA, Manzoni P. Strategies to prevent invasive candidal infection in extremely preterm infants. Clin Perinatol. 2010;37(3):611–28.
Manzoni P, Jacqz-Aigrain E, Rizzollo S, Franco C, Stronati M, Mostert M, et al. Antifungal prophylaxis in neonates. Early Hum Dev. 2011;87(Suppl 1):S59–60.
Speer CP. Inflammatory mechanisms in neonatal chronic lung disease. Eur J Pediatr. 1999;158(Suppl 1):S18–22.
ELFIN Trial Investigators Group. Lactoferrin immunoprophylaxis for very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2013;98(1):F2–4.
Ochoa TJ, Cleary TG. Effect of lactoferrin on enteric pathogens. Biochimie. 2009;91(1):30–4.
Valenti P, Antonini G. Lactoferrin: an important host defence against microbial and viral attack. Cell Mol Life Sci. 2005;62(22):2576–87.
Legrand D, Pierce A, Elass E, Carpentier M, Mariller C, Mazurier J. Lactoferrin structure and functions. Adv Exp Med Biol. 2008;606:163–94.
Scott PH. Plasma lactoferrin levels in newborn preterm infants: effect of infection. Ann Clin Biochem. 1989;26(Pt 5):412–5.
Manzoni P, Rinaldi M, Cattani S, Pugni L, Romeo MG, Messner H, et al. Bovine lactoferrin supplementation for prevention of late-onset sepsis in very low-birth-weight neonates: a randomized trial. JAMA. 2009;302(13):1421–8.
Venkatesh MP, Abrams SA. Oral lactoferrin for the prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst Rev. 2010;(5):CD007137.
Modi N, Dore CJ, Saraswatula A, Richards M, Bamford KB, Coello R, et al. A case definition for national and international neonatal bloodstream infection surveillance. Arch Dis Child Fetal Neonatal Ed. 2009;94(1):F8–12.
Isaacs CE, Kashyap S, Heird WC, Thormar H. Antiviral and antibacterial lipids in human milk and infant formula feeds. Arch Dis Child. 1990;65(8):861–4.
Winberg J, Wessner G. Does breast milk protect against septicaemia in the newborn? Lancet. 1971;1(7709):1091–4.
Ashraf RN, Jalil F, Zaman S, Karlberg J, Khan SR, Lindblad BS, et al. Breast feeding and protection against neonatal sepsis in a high risk population. Arch Dis Child. 1991;66(4):488–90.
Hanson LA, Korotkova M. The role of breastfeeding in prevention of neonatal infection. Semin Neonatol SN. 2002;7(4):275–81.
Goldman AS. The immune system of human milk: antimicrobial, antiinflammatory and immunomodulating properties. Pediatr Infect Dis J. 1993;12(8):664–71.
Wold A, Adlerberth I. Pathological consequences of commensalism. In: Nataro J, Blaser MJ, Cunningham-Rundless S, editors. Persistent bacterial infections. Washington: ASM Press; 2000.
Hanson L, Dahlman-Hoglund A, Karlsson M, et al. Normal microbial flora of the gut and the immune system. In: Hanson L, Yoken RH, editors. Probiotics, other nutritional factors, and intestinal microflora. Philadelphia: Lippincott-Raven; 1999. p. 217–28.
Hasselbalch H, Jeppesen DL, Engelmann MD, Michaelsen KF, Nielsen MB. Decreased thymus size in formula-fed infants compared with breastfed infants. Acta Paediatr. 1996;85(9):1029–32.
Lam BC, Lee J, Lau YL. Hand hygiene practices in a neonatal intensive care unit: a multimodal intervention and impact on nosocomial infection. Pediatrics. 2004;114(5):e565–71.
Etienne KA, Subudhi CP, Chadwick PR, Settle P, Moise J, Magill SS, et al. Investigation of a cluster of cutaneous aspergillosis in a neonatal intensive care unit. J Hosp Infect. 2011;79(4):344–8.
Weston D. Infection prevention and control: theory and practice for healthcare professionals. West Sussex: Wiley; 2008.
Edwards MS, Baker CJ. Bacterial infections in the neonate. In: Long S, Pickering L, Prober C, editors. Principles and practices of pediatric infectious diseases. 4th ed. Philadelphia: Elsevier Saunders; 2011.
DiCenzo R, Forrest A, Slish JC, Cole C, Guillet R. A gentamicin pharmacokinetic population model and once-daily dosing algorithm for neonates. Pharmacotherapy. 2003;23(5):585–91.
Yoshioka H, Takimoto M, Riley HD Jr. Pharmacokinetics of ampicillin in the newborn infant. J Infect Dis. 1974;129(4):461–4.
Rodvold KA, Everett JA, Pryka RD, Kraus DM. Pharmacokinetics and administration regimens of vancomycin in neonates, infants and children. Clin Pharmacokinet. 1997;33(1):32–51.
Wurthwein G, Groll AH, Hempel G, Adler-Shohet FC, Lieberman JM, Walsh TJ. Population pharmacokinetics of amphotericin B lipid complex in neonates. Antimicrob Agents Chemother. 2005;49(12):5092–8.
Piper L, Smith PB, Hornik CP, Cheifetz IM, Barrett JS, Moorthy G, et al. Fluconazole loading dose pharmacokinetics and safety in infants. Pediatr Infect Dis J. 2011;30(5):375–8.
Wade KC, Wu D, Kaufman DA, Ward RM, Benjamin DK Jr, Sullivan JE, et al. Population pharmacokinetics of fluconazole in young infants. Antimicrob Agents Chemother. 2008;52(11):4043–9.
Doby EH, Benjamin DK Jr, Blaschke AJ, Ward RM, Pavia AT, Martin PL, et al. Therapeutic monitoring of voriconazole in children less than three years of age: a case report and summary of voriconazole concentrations for ten children. Pediatr Infect Dis J. 2012;31(6):632–5.
Conflict of interest
None. No sources of funding were used to support the writing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stockmann, C., Spigarelli, M.G., Campbell, S.C. et al. Considerations in the Pharmacologic Treatment and Prevention of Neonatal Sepsis. Pediatr Drugs 16, 67–81 (2014). https://doi.org/10.1007/s40272-013-0057-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-013-0057-x