Abstract
Background and Objective
Multiple myeloma is an incurable disease with a considerable illness and treatment burden, which negatively impacts patients’ quality of life. This study aimed to evaluate the implementation of multiple myeloma care in five Dutch hospitals, related to the three objectives of outcome-driven care, which are defined as (1) providing information for shared decision making in individual patient care, (2) supporting the learning capacity of healthcare professionals and healthcare institutions through benchmarking and (3) developing outcome-driven and patient-centred contracting by health insurers.
Methods
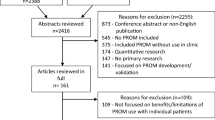
In this qualitative study, semi-structured interviews about experiences with patient-reported outcomes were conducted with patients, healthcare professionals and other stakeholders 2 years after implementation. Data were thematically analysed, and emerging topics were clustered around the three objectives of outcome-driven care.
Results
A total of 46 interviews were held (15 with patients, 16 with professionals and 15 with other stakeholders) that showed patients with multiple myeloma were willing to complete patient-reported outcomes, although integration of patient-reported outcomes in shared decision making fell short in clinical practice. Aggregated patient-reported outcomes were considered important for improving quality of care; however, data collection and data exchange are hindered by privacy legislation, limitations of IT systems and a lack of data standards. Patient-reported outcomes were expected to contribute to cost-effective multiple myeloma treatment, yet outcome-driven reimbursement is still lacking.
Conclusions
Outcome-driven multiple myeloma care using patient-reported outcomes is feasible, provided that (1) patient-reported outcomes and shared decision making are integrated into clinical practice, (2) legal and technical obstacles hindering data collection are removed and (3) health insurers adjust their reimbursement plans to facilitate outcome-driven care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although patients seem willing to complete patient-reported outcome questionnaires, using the outcomes in shared decision making is still limited. |
Removing legal and technical problems hindering data collection will facilitate using patient-reported outcomes in research and policymaking. |
Implementing patient-reported outcomes requires a multidisciplinary approach to achieve the objectives of patient-reported outcomes both at the patient level and at the aggregated level. |
1 Introduction
While multiple myeloma (MM) is an incurable plasma cell malignancy, the introduction of novel therapies [1] has increased the 5-year overall survival in patients with MM in the Netherlands, from 29% in 1996–2002 to 52% in 2010–16, and recent studies reported a further improvement in 5-year survival [1,2,3,4]. However, both the disease and the treatment cause a considerable burden of illness and have a negative effect on the patient’s health-related quality of life (HRQoL). Previous research on HRQoL in MM reported improvements in the overall HRQoL over time, although, during treatment, patients may still experience functional deteriorations [5] and an increase in symptoms because of adverse treatment effects [6,7,8,9,10].
To ensure that improved survival concurs with optimal HRQoL, the Dutch government, healthcare organisations, patient organisations and health insurers have agreed in 2018 to establish value-based and outcome-driven hospital care to improve the quality, affordability and accessibility of hospital care. Furthermore, they agreed that disease-specific outcome sets covering 50% of the total disease burden in Dutch hospitals would be defined within 4 years, i.e. by 2022 [11]. These outcome sets were expected to contribute to the three objectives of outcome-driven patient care: (1) providing information for shared decision making in individual patient care; (2) increasing and supporting the learning capacity of healthcare professionals through benchmarking; and (3) developing outcome-driven and patient-centred contracting by health insurance companies. To meet these objectives, clinical outcomes and HRQoL need to be measured in daily clinical practice and the measured outcomes need to be useful at the level of individual patients as well as at the level of aggregated data [11].
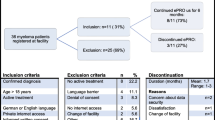
Although the agreement did not specify any particular diseases, an outcome set was also defined for MM because of the increase in treatment options and costs of treatments in MM. The outcome set consisted of clinical outcomes as well as patient-reported outcomes (PROs), which were to be measured by means of patient-reported outcome measures (PROMs) [12]. In 2019, the outcome set was implemented similarly in five Dutch hospitals (Electronic Supplementary Material [ESM]). The goal was to develop a national value-based MM registry containing real-world data, which could be used to improve the quality of MM care in the Netherlands.
However, in daily practice, bottlenecks were experienced during the implementation of PROs as well as with the logistics to collect PRO data at the aggregated level. Additionally, previous studies on implementing PROs in clinical practice reported barriers because of the lack of an implementation strategy [13, 14]. Some studies found that completing PROMs was considered a burden on patients and clinicians and that collecting PROs caused problems in the area of information and communication technology (ICT) [15,16,17]. It is to be expected that these problems may also occur in MM care, but specific literature on implementing PROs in daily clinical practice of MM care is limited [18]. However, the use of PROs is of increasing importance especially in MM care because of the high burden of disease and treatment that patients with MM experience.
The aim of the present study is to evaluate the implementation of PROs in MM over a 2-year period, in these five hospitals, in order to improve the use of PROs in individual patient care and on an aggregated level before further upscaling of PRO use in patients with MM throughout the Netherlands. In our evaluation, we considered the three objectives set out in the Dutch Agreement on outcome-driven hospital care.
2 Methods
2.1 Study Population and Data Collection
In this evaluation study, three groups of participants involved in using PROs were recruited: (1) patients; (2) healthcare professionals; and (3) other stakeholders. Ethical approval was not required because the study was not subject to the Dutch Medical Research Involving Human Subjects Act (WMO) [MEC-2022-0001]. However, all participants provided informed consent to meet the requirements of the Dutch privacy legislation.
In the five participating hospitals, a total of 163 patients with MM received an invitation to complete PROs in the 2 years following the introduction of PROs. Each participating hospital selected five patients who would be eligible for an interview, aiming for a large variation within each sample. Only patients who had been invited to complete two or more PRO questionnaires (baseline and one follow-up) were selected, provided that their current medical condition was good enough to participate in an interview. The 25 eligible patients were invited by the hospital to participate in this study. After agreeing to participate and signing the informed consent, 15 patients were contacted by the research assistants to schedule the interview.
In each of the participating hospitals, healthcare professionals were invited to participate if they were involved in the implementation of the MM outcome set or if they treated patients with MM. Per hospital, we aimed to include at least one haematologist, one nurse involved in the treatment of patients with MM, and one manager or project manager involved in the implementation or coordination of PROs in MM care.
For the stakeholder group, we aimed to invite patient representatives, researchers and healthcare policymakers (including health insurers). We identified stakeholders based on their known expertise in the field of value-based healthcare (VBHC) or PROs in the Netherlands and additionally by snowballing from previous interviews.
Between March and May 2022, patients, healthcare professionals and stakeholders were interviewed individually in 30-minute interviews using a semi-structured topic list (see ESM). Because of the coronavirus disease 2019 pandemic restrictions at the start of this study, the interviews with the patients were conducted by telephone. The interviews with healthcare professionals and stakeholders were conducted individually using Microsoft teams [19]. All interviews were conducted by three research assistants (two Master’s students and one Bachelor’s student in Health Sciences), all of whom were trained in performing qualitative research and conducting in-depth interviews. Each research assistant was assigned to a specific participant group. The research assistants were supervised by the researchers. All interviews were audio-recorded, anonymised and transcribed verbatim in Dutch. The interview results were discussed collectively in regular research team meetings to share information with the research team. Each research assistant continued data collection until saturation was reached (see code manager in the ESM).
2.2 Data Analysis
According to the standard procedures of thematic analysis [20], all transcripts were read in detail per participant group by the researchers. All transcripts were coded separately per group using ATLAS-ti 22 [21] and subsequently compared and discussed, after which the transcripts of the participant groups were merged. The emerging dominant topics were discussed within the research team and clustered into themes related to the three objectives of outcome-driven patient care, as mentioned in the introduction [20] (Table 1).
3 Results
3.1 Participant Characteristics
In total, 15 patients, 16 healthcare professionals and 15 stakeholders were interviewed. Among the participants were nine male and six female patients. Their ages ranged from 52 to 87 years (mean age 69.86) years (Table 2).
The group of healthcare professionals consisted of six haematologists, four nurses and six PRO coordinators. Of the haematologists, two acted as team leaders for implementing PROs in their hospital, and four were not actively involved in PRO implementation. All the nurses and PRO coordinators were actively involved in the implementation of PROs in their hospitals (Table 4a of the ESM). The stakeholder group consisted of two patient representatives, seven researchers, five policymakers and two data analysts involved in data logistics of PROs (Table 4b of the ESM).
In the following sections, the results are presented in terms of the themes that emerged, which were categorised under the three objectives of outcome-driven care. These results are illustrated with quotes of the participants (more quotes in the ESM).
3.2 Providing Information for Shared Decision Making in Individual Patient Care
Most patients indicated to be willing to complete PROMs. These patients expressed their willingness to do anything that might help improve treatment, and a few mentioned that PROMs encouraged them to think about their health.
“… I’m willing to work on everything that I discuss with my specialist that is somehow related to my treatment. So if my specialist asks me to complete a questionnaire and the results may change my treatment, I’m happy to go along with that.” (patient 15)
Most patients indicated that completing the digital questionnaires (55 questions each time) was not too difficult and not too time consuming.
“I reckon no more than 10 minutes, it wasn’t so bad.” (patient 5)
A few patients commented that they were bothered by some of the questions, for example questions about thinking of death and questions about intimacy and sex life. Because of these questions, one patient ended participation after completing one questionnaire. Another patient expressed not to be willing to complete any questionnaire as he felt bothered by questionnaires too much in his life.
“… but when I’m asked how often I think of my own death, on how depressed I am and how my sex life is, I think to myself, I’m not answering those questions.” (patient 2)
Although most patients expressed their willingness to complete PROMs and to contribute to improving patient care, several patients indicated that they did not feel the need to discuss questionnaires with their physician and preferred disease and treatment symptoms or problems in daily functioning to emerge more naturally in a doctor-patient conversation, rather than going through a questionnaire.
“She shouldn’t check the answers to the questionnaire and say: hey, this isn’t going well, that is something that I should mention in conversation.” (patient 6)
Patients who did discuss their outcomes, did so with a nurse and indicated that complaints were addressed correctly and additional care was initiated. Most patients had no experience with discussing PROs with a healthcare professional. One of the patients indicated that she was disappointed that PROs had not been discussed with her by anyone while she experienced serious complaints that went unaddressed, even though she indicated this in the questionnaire.
“That my situation was a heavy burden and that I was sent home feeling that way. I fell into a dark hole and I stated this in the questionnaire but nothing was done with it.” (patient 7)
“… if she said, I can see in your questionnaire …, I noticed that you answered …, I would like to discuss something I read …, it would at least give me the impression my answers had been noticed.” (patient 1)
Patients indicated that although explicit discussion of PROs by their physician is not necessary, they do expect their healthcare professionals to take notice of PROs and consider PROs in their treatment decisions. However, most patients indicated that they do not exactly know how PROs are used by their healthcare professionals. Some patients indicated that they received information about how to complete questionnaires; however, most patients indicated not exactly knowing the purpose of PROs.
Maybe the purpose of the questionnaire could be explained [better]. Perhaps I was told what it was for, but it certainly didn’t stick.” (patient 11)
Some healthcare professionals expressed that informing patients about PROs is only one of the aspects discussed at the start of a care trajectory. In the information overload, this is easily forgotten.
“Yes, but that can be quite difficult because people are already given so much information, right? And then there’s also the questionnaire to keep in mind.” (healthcare professional)
Most healthcare professionals also confirmed that PROs are not discussed with patients. In two hospitals, PROs are discussed by nurses. Important barriers to discussing PROs during consultations that were mentioned were limited consultation time and a lack of dashboards with a clear presentation of the results. Additionally, one haematologist expressed that although they endorse the importance of PROs, they are focussed on discussing laboratory results, showing adverse treatment effects or disease progression. Therefore, some healthcare professionals, stakeholders and patients expressed the opinion that PROs are best discussed by nurses, as part of discussing overall psychosocial and physical well-being. However, some mentioned that discussing PROs in consultations with nurses is often insufficiently formalised by management and is therefore too non-committal, and too little attention is paid to ensure that it is done.
Another impediment is that PROMs need to be completed only three or four times a year, while the frequency of hospital visits is usually higher (some studies reported an average of 68–77 hospital visits in the first year after diagnosis [22, 23]). These differences in frequency complicate the integration and standardisation of PRO use in daily clinical practice.
“Look, if we were sure that a patient returns at set times, after three months, after nine months and that there are no appointments in between, then we would acquire a certain PROM routine. However, the patient may have ten more appointments in that time, where PROM doesn’t come into play at all. So, that makes it difficult to build up a routine.” (healthcare professional)
3.3 Increasing and Supporting the Learning Capacity of Healthcare Professionals Through Benchmarking
Participants in all three groups expressed the importance of data collection on an aggregated level for quality improvement of patient care. Several patients mentioned that improving quality of MM care is part of the reason why they are willing to complete PROs. Additionally, healthcare professionals indicated that aggregated PRO data provide useful information for benchmarking within and between hospitals. Comparing differences between treatments and discussing clinical outcomes and PROs between hospitals enables healthcare professionals to adjust treatments or to provide additional supportive care. In addition to benchmarking between hospitals, aggregated PROs provide a more comprehensive insight into topics that are not always addressed during consultation but which are important for patient-centred care, such as financial problems or sleeping problems due to some medications (e.g. dexamethasone).
“Does it show that we start pain medication too late, that there is not enough focus on malnutrition, that there are financial issues to consider? These are issues I never discuss, but if the outcomes show these issues in alarming numbers, we should add a social worker to the team during consultations to tackle them. We really don’t know enough about this.” (healthcare professional)
Some stakeholders added that collecting PROs in clinical practice provides important lessons from real-world data that could be compared to clinical trial data. One of the stakeholders indicated that PROs are less suited for benchmarking between institutions to measure quality of care. In his opinion, instead of focusing on differences between hospitals, the focus should be on using aggregated data as reference data to be able to interpret patients’ individual outcomes by comparing them to aggregated outcomes of other patients with MM.
… if the rest of the patient population experiences this [outcome] differently, and then the patient can reflect on this with the doctor, however, I don’t really support the use of PROs for benchmarks. (professor)
Participants mentioned that questionnaires to capture PROs were digitally integrated into electronic health records (EHRs). However, ICT is still considered an important barrier to using PRO data on an aggregated level to improve patient care. Some healthcare professionals and stakeholders stated that there is too little progression in the development of easy-to-use dashboards that present both individual outcomes as well as aggregated-level outcomes. Although this issue is in part due to complex ICT and data logistics, it is also caused by the low incidence rates of MM and the large amount of data that is needed to provide useful and reliable information to present in a dashboard. During the 2 years of PRO collection in patients with MM in five Dutch hospitals, two benchmark reports were provided. However, because of the many treatment options in several lines of treatment, the data were considered too immature to be used for reliable benchmarking between hospitals.
“Generally, you will end up with too little data, people don’t realise how much data you actually need so that you can make the data usable.” (researcher)
Another barrier to accelerating data collection is the fact that patients who are included in clinical trials also need to complete HRQoL questionnaires. In some hospitals, patients are asked to complete both sets of questionnaires, and in other hospitals, PRO collection is stopped for the duration of the trial. Although the PRO and HRQoL questionnaires are largely overlapping, the consent procedures of the clinical trial prohibit data exchange to use these data in the population-based registry. As a consequence, PROs of most patients in clinical trials are missing in the MM registry, which causes gaps in the data set and further delays in data collection.
“Multiple myeloma patients also participate in these studies, and they are asked to complete a questionnaire which is exactly the same. Which one will they choose to complete?” (healthcare professional)
Stakeholders mentioned that the current data management to collect data in MM on an aggregated level is complex, time consuming and expensive. This currently prevents expanding the number of hospitals collecting PROs. Patient-reported outcomes are retrieved digitally from EHRs or other data capture tools; however, the case-mix variables and clinical outcomes needed for benchmarking are mainly manually captured from the EHRs, which makes it expensive. Furthermore, some stakeholders mentioned that data integration of PROs and clinical outcomes is hindered because data sources use different ways of pseudonymising. Moreover, stakeholders stated that without individual patient consent, privacy legislation prohibits data integration from different data sources.
Although the aggregated-level data reports did not yet provide useful data for benchmarking or reference data to be used in consultations, some healthcare professionals stated that the reports did provide insights into the potential of a population-based MM registry. Others mentioned that they had no experience yet with discussing the PRO data locally. However, receiving these reports was expected to motivate the healthcare professionals to continue collecting PROs in daily practice. Ultimately, the objective is to arrive at valuable data for benchmarking to either reduce undesirable treatment or outcome variations or to discover best practices.
“So if we can show that scientific questions will be answered by means of systematic data collection …. Well, then that’s an incentive to use it during consultations.” (healthcare professional)
In addition to barriers in creating dashboards and reports to be used for benchmarking between institutions, stakeholders in particular indicated that the interpretation of aggregated level real-world PRO data is challenging and requires assessments of the quality of the data and a methodologically correct approach to drawing the right conclusions.
“In this [analyses of PROs], a number of statistical and technical measuring issues may arise, making its use more problematic.” (professor)
3.4 Outcome and Patient-Oriented Contracting by Health Insurers
Most health insurers promote shared decision making between healthcare professionals and patients in their hospital reimbursement plans. However, decision aids (in other malignancies) providing information on the advantages and disadvantages of different treatments are predominantly based on clinical outcomes that are easily captured with reimbursement data, not including PROs.
“In the end, health insurance companies opted to measure the outcomes based on claims data. Ultimately, I consider that to be a bit of an easy way out.” (health insurer)
One of the healthcare professionals mentioned that incentives are lacking to prioritise integrating PROs into daily routines. However, almost all participants stated that health insurers should not make PRO collection a mandatory reimbursement condition. They said that mandating PROs by health insurers is likely to provoke resistance among healthcare professionals in general. Furthermore, as implementing PROs also requires the registration of clinical outcomes and case-mix variables, healthcare professionals may be burdened by the additional registration of these variables. Other participants indicated that PROs should not be made mandatory because patients cannot be obliged to complete PROs and patients may not be able to complete questionnaires. However, some stakeholders indicated that patients should feel a moral obligation to do everything in their power to contribute to improving their health. This was also addressed by some patients.
“Yes, I do believe [PROs] are of great importance, so I consider completing them to be a moral obligation.” (professor)
“But I think it is in our own interest and that of others to do so.” (patient 3)
One participant mentioned that instead of making PROs mandatory, health insurers could encourage the completion of PROs by making them part of the reimbursement system, where collecting PROs is facilitated by additional reimbursements. When asked whether PROs are cost effective for healthcare costs, which would make it more interesting for health insurers to reimburse PRO use, most stakeholders mentioned that this is still unclear.
“I think we will find out in ten or twenty years.” (researcher)
Although most stakeholders acknowledged that efforts and costs of PRO implementation are high and that clear evidence that PROs will prove to be cost effective is still lacking, they expressed the expectation that using PROs will eventually prove cost effective. Some stakeholders argued that shared decision making based on PROs will enhance individual patient care and will lead to more cost-effective treatment plans. Additionally, most stakeholders mentioned that the evaluation of the aggregated PRO data in particular will contribute to improved overall quality of care and more insight into which treatments are most effective for which patients, which is expected to lead to more cost-effective treatment plans including a reduction in societal costs.
“That information will also lead to a systematic improvement in care as the process will be designed more effectively and more efficiently. As a result, this will be hugely beneficial for patients and also for cost reduction.” (advisor VBHC)
Finally, most patients who completed PROs stated that they were willing to keep doing so, even for a long time. Most participants of the healthcare professionals and stakeholders indicated that they expected PROs to become a regular part of MM care, provided that ICT and other bottlenecks are resolved and PROs are further integrated into daily practice, with less registration burden on patients. In addition to removing current bottlenecks, they also mentioned the introduction of apps and computer adaptive testing methods to reduce the registration burden.
“Yes, I do hope so. A lot needs to be achieved in order for it [PROs] to become embedded in daily practice.” (healthcare professional)
4 Discussion
This study aimed to evaluate the implementation of PROs in MM care in five Dutch hospitals, related to the three objectives of outcome-driven care. The results of our study showed that patients with MM seem willing to complete PROMs; however, the integration of PROs in individual patient care and shared decision making, which matches the expectations of both patients and healthcare professionals, is complex and requires team effort. Participants considered PROs to be important for providing aggregated reference data to support dashboards used for shared decision making, quality improvement and research. However, data collection and the development of dashboards are complex and expensive and are hindered by privacy legislation and a lack of standards in registration. Furthermore, PROs are expected to contribute to more patient-centred and cost-effective treatment; however, integration of PROs in healthcare policy is still lacking, as are incentives to use PROs in reimbursement plans.
To improve the use of PROs in individual patient care, PROs should be integrated into shared decision making between patients and healthcare professionals [24]. This will provide healthcare professionals with a more comprehensive insight into the patients’ HRQoL, which is especially important in patients who are often highly burdened by disease and treatment effects. Additionally, clear information about the importance of PROs and actively addressing them during consultation will encourage patients to keep completing PROMs [25]. To achieve this goal, addressing PROs could best be integrated into care pathways as a specific task of nurses, as addressing quality-of-life aspects fits well into the comprehensive holistic approach of nurse consultations [26,27,28]. However, engagement of hospital management is often too non-committal [14, 29,30,31]. Patient-reported outcome integration is complex, especially in patients with MM with complex and unpredictable pathways and large numbers of hospital visits without the need to complete PROMs during each visit. It therefore requires committed leadership to develop PRO workflows and dashboards that support shared decision making. Another crucial factor for achieving integration of PROs in clinical practice is the clinical leadership of haematologists, who should convince their teams of the importance of PROs.
Although local dashboards for both healthcare professionals and patients may provide patients’ individual PRO outcomes, the availability of aggregated reference data will considerably improve local dashboard information by showing patients their health status compared to the mean outcomes of other patients with MM. Additionally, analyses of aggregated data will be useful to evaluate the quality of MM care through benchmark meetings, providing insights into what matters most to patients and what improvements are required in clinical practice [32,33,34]. To provide reliable aggregated outcome information, large amounts of data are needed. However, because of legal and technical bottlenecks, data logistics is too complex and expensive. It will require the joint efforts of hospitals, EHR providers and data-platform providers to resolve IT problems that obstruct the process of data collection. This process towards Findable, Accessible, Interoperable and Reusable (FAIR) data could be guided by data managers who are experts in capturing and modelling EHR data, for example those of the Dutch cancer registry [35,36,37,38]. Nevertheless, patients must be able to rely on the safe, anonymised and non-traceable use of their medical data, which are therefore protected by privacy legislation [39]. However, a strict interpretation of privacy laws may not serve the best interests of patients, as it limits the optimal use of available health data from different sources, hindering both individual care and innovations at the population level [40]. Therefore, governmental institutions, healthcare organisations and patient organisations should provide clear policies on data integration and standardised pseudonymisation. If these problems pertain, they will hinder upscaling of the use of PROMs to other hospitals, and it will take even longer before the value of using PROMs will become evident.
Standardisation of PROs and PROMs in clinical trials and clinical practice will facilitate data exchange and further integration of PRO use into clinical practice and will prevent registration burden or data gaps. Furthermore, international standardisation of PROs will accelerate the collection of real-world data and may help facilitate the initiation of trials, providing that legal, technical and methodological requirements are met.
Finally, patient-centred outcome information, including PROs that are integrated with healthcare utilisation data, will provide better insight into both the efficacy and the cost effectiveness of treatments, which is important to determine the actual value of a treatment. This information will support decision making on whether treatments should be reimbursed in health insurance plans. However, health insurers lack interest in PROs and outcome-driven payment [41, 42]. Transparency on which treatments provide the highest value for patients becomes increasingly important especially in patients with MM, owing to the introduction of expensive new and prolonged treatments. This transparency will not only improve current MM care, but it will also ensure that MM care remains affordable and future treatments become available to patients with MM. Therefore, especially in MM, health insurers should prioritise outcome-driven care and facilitate PRO use and shared decision making in clinical practice to ensure that the quality and accessibility of MM treatments are guaranteed [43].
These results emphasise the importance of resolving bottlenecks both at the local and the aggregated level. They also show that the objectives of outcome-driven care are mutually dependent and that improvements at all levels by all stakeholders are needed to facilitate the continuation and upscaling of outcome-driven MM care (Fig. 1).
4.1 Strengths and Weaknesses
In this study, a broad variety of different participants was included, all of whom highlighted their experiences with PROs from different perspectives. Furthermore, this study evaluated PRO use in various local settings, and by referring to national policy, a broader picture was sketched of interdependencies and solutions to improve PRO use. However, selection bias cannot be ruled out, as most participants had an active role in PRO completion, implementation or research and may therefore have a more positive attitude towards PROs. Even so, despite their possibly more positive attitude, they addressed several bottlenecks that need to be resolved to achieve feasible and affordable outcome-driven MM care. It could also be considered a limitation that the topic lists used in the interviews in the stakeholder group were not specified for each specific group of stakeholders. Further research, especially research on the role of policymakers and health insurers, is needed to obtain more insight into these stakeholders’ perspectives on and experiences with PROs.
4.2 Implications for Further Research and Clinical Practice
Our study focussed on a single disease, MM. As a consequence, we did not consider the complexity caused by multiple PROs and PROMs at the hospital level or even at the level of individual patients with multimorbidity. However, it would be very interesting and relevant for further research, for example to identify the advantages and disadvantages of generic non-disease-specific PROs and PROMs. Additionally, the analyses and methodologically correct interpretations of PROs need continuous attention, as using PROs will become more important in decision making on the effectiveness and cost effectiveness of treatments. Furthermore, although limited research is available on the cost effectiveness of PROs [44, 45], more cost-effectiveness analyses of implementing and using PROs are needed [46].
In this study, we focused on PROs in hospitals. However, it is to be expected that home administration of MM treatment and e-health in follow-up care will become more common practice, which will create new challenges to integrate PROs into new care pathways, especially if these pathways involve other healthcare providers.
Finally, this study evaluated the implementation and use of PROs in MM care over a 2-year period. Most participants indicated that based on their current knowledge, they expect outcome-driven MM care and the use of PROs to be feasible. However, this evaluation study needs to be repeated in a few years to be able to determine whether using PROs in clinical practice will contribute to improving the quality of care in MM in the long run.
5 Conclusions
Further upscaling of outcome-driven MM care using PROs seems possible, provided that PROs and shared decision making are integrated into clinical practice through more engaged leadership and clear directives indicating who should address PROs in daily practice. Furthermore, higher priority should be given to removing legal and technical obstacles that hinder the collection of aggregated real-world data. Finally, the importance of PROs should be explicated in reimbursement plans, and health insurers should take responsibility to facilitate the implementation of outcome-driven hospital care.
References
Dinmohamed A. Belangrijke cijfers over hematologische kankersoorten. Utrecht, The Netherlands: 2019:11.
Cavo M, Beksac M, Pantani L, et al. Autologous haematopoietic stem-cell transplantation versus bortezomib-melphalan-prednisone, with or without bortezomib-lenalidomide-dexamethasone consolidation therapy, and lenalidomide maintenance for newly diagnosed multiple myeloma (EMN02/HO95): a multicentre, randomised, open-label, phase 3 study. Lancet Haematol. 2020;7(6):e456–68. https://doi.org/10.1016/s2352-3026(20)30099-5.
Oliva S, Bruinink DHO, Rihova L, et al. Minimal residual disease assessment by multiparameter flow cytometry in transplant-eligible myeloma in the EMN02/HOVON 95 MM trial. Blood Cancer J. 2021;11(6):106. https://doi.org/10.1038/s41408-021-00498-0.
Gaballa MR, Ma J, Tanner MR, et al. Real-world long-term outcomes in multiple myeloma with VRD induction, Mel200-conditioned auto-HCT, and lenalidomide maintenance. Leuk Lymphoma. 2022;63(3):710–21. https://doi.org/10.1080/10428194.2021.1992763.
Johnsen AT, Tholstrup D, Petersen MA, et al. Health related quality of life in a nationally representative sample of haematological patients. Eur J Haematol. 2009;83(2):139–48. https://doi.org/10.1111/j.1600-0609.2009.01250.x.
Mols F, Oerlemans s, Vos AH, et al. Health-related quality of life and disease-specific complaints among multiple myeloma patients up to 10 yr after diagnosis: results from a population-based study using the PROFILES registry. Eur J Haematol. 2012;89(4):311–9. https://doi.org/10.1111/j.1600-0609.2012.01831.x.
Jordan K, Proskorovsky I, Lewis P, et al. Effect of general symptom level, specific adverse events, treatment patterns, and patient characteristics on health-related quality of life in patients with multiple myeloma: results of a European, multicenter cohort study. Support Care Cancer. 2014;22(2):417–26. https://doi.org/10.1007/s00520-013-1991-4.
Ludwig H, Pönisch W, Knop S, et al. Quality of life in patients with relapsed/refractory multiple myeloma during ixazomib-thalidomide-dexamethasone induction and ixazomib maintenance therapy and comparison to the general population. Leuk Lymphoma. 2020;61(2):377–86. https://doi.org/10.1080/10428194.2019.1666381.
Kiely F, Cran A, Finnerty D, et al. Self-reported quality of life and symptom burden in ambulatory patients with multiple myeloma on disease-modifying treatment. Am J Hosp Palliat Care. 2017;34(7):671–6. https://doi.org/10.1177/1049909116646337.
Bennink MC, Stege CAM, Lissenberg-Witte BI, et al. Impact of comorbidities on health-related quality of life in nontransplant eligible patients with newly diagnosed multiple myeloma. Hemasphere. 2022;6(7): e744. https://doi.org/10.1097/hs9.0000000000000744.
Ministerie van Volksgezondheid Welzijn en Sport. Bestuurlijk akkoord medisch specialistische zorg 2019-2022: Kennis- en exploitatiecentrum Officiele Overheidspublicaties; 2019 [cited 2022]. Available from: https://open.overheid.nl/Details/ronl-28f77d2c-bff3-4907-9bf6-45aa6078309a/1#panel-gegevens
Oerlemans S, Bennink MC, Levin MD, et al. Development of a patient centered outcome set for patients with multiple myeloma to be used in clinical practice. Hemasphere. 2020;4(3): e366. https://doi.org/10.1097/hs9.0000000000000366.
Cheng HWB, Lam KO. Supportive and palliative care in hemato-oncology: how best to achieve seamless integration and subspecialty development? Ann Hematol. 2021;100(3):601–6. https://doi.org/10.1007/s00277-020-04386-8.
Boyce MB, Browne JP, Greenhalgh J. The experiences of professionals with using information from patient-reported outcome measures to improve the quality of healthcare: a systematic review of qualitative research. BMJ Qual Saf. 2014;23(6):508–18. https://doi.org/10.1136/bmjqs-2013-002524.
Graupner C, Breuking SO, Mul S, et al. Patient-reported outcome measures in oncology: a qualitative study of the healthcare professional’s perspective. Support Care Cancer. 2021;29(9):5253–61. https://doi.org/10.1007/s00520-021-06052-9.
Nguyen H, Butow P, Dhillon H, et al. A review of the barriers to using Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs) in routine cancer care. J Med Radiat Sci. 2021;68(2):186–95. https://doi.org/10.1002/jmrs.421.
van Muilekom MM, Teela L, van Oers HA, et al. Patients’ and parents’ perspective on the implementation of patient reported outcome measures in pediatric clinical practice using the KLIK PROM portal. Qual Life Res. 2022;31(1):241–54. https://doi.org/10.1007/s11136-021-02950-x.
Terpos E, Mikhael J, Hajek R, et al. Management of patients with multiple myeloma beyond the clinical-trial setting: understanding the balance between efficacy, safety and tolerability, and quality of life. Blood Cancer J. 2021;11(2):40. https://doi.org/10.1038/s41408-021-00432-4.
Microsoft. Microsoft Teams, version 1.4.00.22472 ed. https://www.microsoft.com/nl-nl/microsoft-teams/group-chat-software: Microsoft; 2021.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
ATLAS.ti Scientific Software Development GmbH. ATLAS.ti 22 Windows. 2022.
Teitelbaum A, BA-Mancini A, Huang H, et al. Health care costs and resource utilization, including patient burden, associated with novel-agent-based treatment versus other therapies for multiple myeloma: findings using real-world claims data. Oncologist. 2013;18(1):37–45. https://doi.org/10.1634/theoncologist.2012-0113.
Mian HS, Fiala MA, Wildes TM. Burden of treatment among older adults with newly diagnosed multiple myeloma. Clin Lymphoma Myeloma Leuk. 2021;21(2):e152–9. https://doi.org/10.1016/j.clml.2020.09.010.
Di Maio M, Basch E, Denis F, et al. The role of patient-reported outcome measures in the continuum of cancer clinical care: ESMO clinical practice guideline. Ann Oncol. 2022. https://doi.org/10.1016/j.annonc.2022.04.007.
Snyder CF, Aaronson NK, Choucair AK, et al. Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Qual Life Res. 2012;21(8):1305–14. https://doi.org/10.1007/s11136-011-0054-x.
Conway A, O’Donnell C, Yates P. The effectiveness of the nurse care coordinator role on patient-reported and health service outcomes: a systematic review. Eval Health Prof. 2019;42(3):263–96. https://doi.org/10.1177/0163278717734610.
Cheng X, Wei S, Zhang H, et al. Nurse-led interventions on quality of life for patients with cancer: a meta-analysis. Medicine (Baltimore). 2018;97(34):e12037. https://doi.org/10.1097/md.0000000000012037.
Monterosso L, Platt V, Bulsara M, et al. Systematic review and meta-analysis of patient reported outcomes for nurse-led models of survivorship care for adult cancer patients. Cancer Treat Rev. 2019;73:62–72. https://doi.org/10.1016/j.ctrv.2018.12.007.
Greenhalgh J. Understanding the complexities of collecting and using PRO data in a primary care context. BMJ Qual Saf. 2022;31(3):175–8. https://doi.org/10.1136/bmjqs-2021-013315.
Stover AM, Haverman L, van Oers HA, et al. Using an implementation science approach to implement and evaluate patient-reported outcome measures (PROM) initiatives in routine care settings. Qual Life Res. 2021;30(11):3015–33. https://doi.org/10.1007/s11136-020-02564-9.
Lavallee DC, Chenok KE, Love RM, et al. Incorporating patient-reported outcomes into health care to engage patients and enhance care. Health Aff (Millwood). 2016;35(4):575–82. https://doi.org/10.1377/hlthaff.2015.1362.
Fayanju OM, Mayo TL, Spinks TE, et al. Value-based breast cancer care: a multidisciplinary approach for defining patient-centered outcomes. Ann Surg Oncol. 2016;23(8):2385–90. https://doi.org/10.1245/s10434-016-5184-5.
Javid SH, Lawrence SO, Lavallee DC. Prioritizing patient-reported outcomes in breast cancer surgery quality improvement. Breast J. 2017;23(2):127–37. https://doi.org/10.1111/tbj.12707.
Pryor DI, Martin JM, Millar JL, et al. Evaluation of hypofractionated radiation therapy use and patient-reported outcomes in men with nonmetastatic prostate cancer in Australia and New Zealand. JAMA Netw Open. 2021;4(11):e2129647. https://doi.org/10.1001/jamanetworkopen.2021.29647.
Willems SM, Abeln S, Feenstra KA, et al. The potential use of big data in oncology. Oral Oncol. 2019;98:8–12. https://doi.org/10.1016/j.oraloncology.2019.09.003.
van den Hurk CJG, Mols F, Eicher M, et al. A narrative review on the collection and use of electronic patient-reported outcomes in cancer survivorship care with emphasis on symptom monitoring. Curr Oncol. 2022;29(6):4370–85. https://doi.org/10.3390/curroncol29060349.
Jansen T, Geleijnse G, Van Maaren M, et al. Machine learning explainability in breast cancer survival. Stud Health Technol Inform. 2020;270:307–11. https://doi.org/10.3233/shti200172.
Smits D, Van Beusekom B, Martin F, et al. An improved infrastructure for privacy-preserving analysis of patient data. Stud Health Technol Inform. 2022;295:144–7. https://doi.org/10.3233/shti220682.
Kayaalp M. Patient privacy in the era of big data. Balkan Med J. 2018;35(1):8–17. https://doi.org/10.4274/balkanmedj.2017.0966.
Price WN 2nd, Cohen IG. Privacy in the age of medical big data. Nat Med. 2019;25(1):37–43. https://doi.org/10.1038/s41591-018-0272-7.
Neubert A, Brito Fernandes O, Lucevic A, et al. Understanding the use of patient-reported data by health care insurers: a scoping review. PLoS ONE. 2020;15(12):e0244546. https://doi.org/10.1371/journal.pone.0244546.
Hanmer J, Cizik AM, Gulek BG, et al. A scoping review of US insurers’ use of patient-reported outcomes. Am J Manag Care. 2022;28(6):e232–8. https://doi.org/10.37765/ajmc.2022.89162.
Theroux H, Williams A, Liu M, et al. Multiple myeloma cost of care under the oncology care model: the influence of high-cost therapies. JCO Oncol Pract. 2020;16(10):e1078–84. https://doi.org/10.1200/jop.19.00569.
Nixon N, Spackman E, Clement F, et al. Cost-effectiveness of symptom monitoring with patient-reported outcomes during routine cancer treatment. J Cancer Policy. 2018;15:32–6.
Lizee T, Basch E, Tremoliers P, et al. Cost-effectiveness of web-based patient-reported outcome surveillance in patients with lung cancer. J Thorac Oncol. 2019;14(6):1012–20. https://doi.org/10.1016/j.jtho.2019.02.005.
Blommestein HM, Zweegman S. Cost-effectiveness: maximizing impact by meticulous data. Blood. 2022;140(6):525–6. https://doi.org/10.1182/blood.2022016958.
Acknowledgements
We thank our research assistants Maartje van Wijk, Cindy Wong and Melanie Jongeneel for interviewing, transcribing and coding. We are grateful to the participating hospitals for their contribution to this research. Finally, we thank Annabelle Payne for translating the quotations used in this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study received funding from the National Health Care Institute (Zorginstituut Nederland), OP1240.
Conflict of interest
PS received research grants from Amgen, Celgene, Janssen and Skyline Dx, honoraria from Amgen, BMS/Celgene, Janssen, Karyopharm and Seagen, and is the Chairman of the European Myeloma Network and Co-Chairman of HOVON Myeloma Working Group. JH is an independent consultant. AB is on the advisory boards and has received honoraria from Amgen, Janssen, BMS and Sanofi. CB, MM, MK, LT, EJ, MG and DL have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Ethics approval was not required (MEC-2022-0001).
Consent to participate
Written consent was obtained from all patients, verbal consent was obtained from all other participants prior to the interview.
Consent for publication
All participants provided verbal consent for publication.
Availability of data and material
The datasets generated and analysed during the current study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Author contributions
CB, MdM, DL, PS and JH contributed to the conception and design. CB, MvdK, AB, LT, EdJ and MG participated in the data collection. CB, MdM and JH performed the analysis and drafted the first version of the manuscript. All authors critically read, revised and approved the final version of the manuscript.
Consent for publication
Written consent was obtained from all patients, verbal consent was obtained from all other participants prior to the interview. All participants provided verbal consent for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bennink, C., de Mul, M., van der Klift, M. et al. Improving Outcome-Driven Care in Multiple Myeloma Using Patient-Reported Outcomes: A Qualitative Evaluation Study. Patient 16, 255–264 (2023). https://doi.org/10.1007/s40271-023-00616-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-023-00616-z