Abstract
Background and Objective
Hydroxychloroquine was widely used during the severe acute respiratory syndrome coronavirus 2 pandemic as an antiviral drug. Most previous pharmacokinetic/pharmacodynamic studies on hydroxychloroquine were conducted on healthy volunteers or patients receiving long-term therapy. There are no studies on the elimination of hydroxychloroquine after short-term treatments. Hydroxychloroquine is known to have a pro-arrhythmic effect through QT interval prolongation, but data in this setting are not conclusive. Our aims were to estimate the time needed for hydroxychloroquine concentrations (CHCQ) to drop to a safe concentration (500 ng/mL) after a short-term therapeutic cycle and to correlate the corrected QT interval with CHCQ.
Methods
We collected blood samples and electrocardiograms of patients who underwent short-term therapy with hydroxychloroquine during drug intake and after discontinuation. Hydroxychloroquine concentrations were determined by high-performance liquid chromatography–tandem mass spectrometry and analysed with a linear regression model to estimate the elimination time of the drug after its discontinuation. We conducted a multivariate analysis of the corrected QT interval correlation with CHCQ.
Results
Our data suggest that short-term hydroxychloroquine courses can generate significant CHCQ persisting above 500 ng/mL up to 16 days after discontinuation of treatment. Corrected QT interval prolongation significantly correlates with CHCQ.
Conclusions
The study confirms the long half-life of hydroxychloroquine and its effect on the corrected QT interval even after short-term courses of the drug. This can inform the clinician using hydroxychloroquine treatments that it would be safer to start or re-initiate treatments with corrected QT interval-prolonging potential 16 days after hydroxychloroquine discontinuation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hydroxychloroquine (HCQ) has a long elimination half-life after drug discontinuation and it has a QT prolongation effect during long-term treatment courses. |
Our study suggests that HCQ whole blood concentration could persist above 500 ng/mL up to 16 days after short-term treatment discontinuation and that HCQ concentration significantly correlates with corrected QT interval prolongation also in short-term treatment courses. |
We suggest to start (or re-introduce) QT-prolonging drugs 16 days after HCQ short-therapy discontinuation. |
1 Introduction
The antimalarial drug hydroxychloroquine (HCQ) is among those much-discussed drugs for the treatment and management of patients with coronavirus disease 2019 (COVID-19). The efficacy as well as the dosage of HCQ was highly debated during the start of the pandemic, when there were no reliable clinical data to endorse any specific therapies [1]. Hydroxychloroquine has been considered an ideal drug to treat severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, as it can inhibit the virus through its antiviral effects and mitigate the cytokine storm through its immunomodulatory effects [2], but subsequent studies did not confirm its efficacy and its use in COVID-19 treatment has fallen out of favor [3]. However, this drug is also known to potentially cause QTc interval prolongation, particularly when taken at high doses, for a long period of treatment, or in combination with other medications, such as azithromycin and lopinavir/ritonavir, [4,5,6,7,8,9,10,11,12,13,14,15] drugs that have been widely used as experimental or off-label treatments in the COVID-19 pandemic.
Most previous pharmacokinetic/pharmacodynamic studies were conducted on healthy volunteers or on patients with diseases different from COVID-19 [16,17,18]: it has been calculated that the HCQ terminal elimination half-life is more than 40 days, owing to its sequestration in deep tissue and the extremely large volume of distribution, rather than to low clearance [19]. Hydroxychloroquine accumulates in blood cells, in which its concentrations are much higher and less variable than in plasma, suggesting that whole blood is the optimal matrix to use for HCQ treatment monitoring [20].
Which HCQ whole blood concentration (CHCQ) could be considered safe is a matter of debate; a blood concentration of 200 ng/mL is sometimes suggested as a marker of patient non-adherence to treatment [21], whereas a CHCQ of 500 ng/mL was proposed as the minimum effective concentration that avoids flare-ups in systemic lupus erythematosus [22, 23] and is used as a marker of drug adherence [24]. It would be useful for clinicians to know when they can consider it safe to start or re-initiate other drugs with an effect on the QT interval after a brief HCQ treatment, information not already available in the scientific literature to the best of our knowledge. We used retrospective and prospective data on CHCQ and corrected QT interval (QTc) among the patients hospitalised for COVID-19 in Fondazione IRCCS Policlinico San Matteo between March and April 2020 to try to answer this clinical question.
1.1 Aim
The primary objective of this study was to estimate the minimum interval needed for CHCQ to drop down to a cut-off safety concentration of 500 ng/mL [22, 23] after a short-term therapeutic cycle as those used in COVID-19 treatment. The secondary objective was to correlate the QTc with CHCQ in this particular clinical setting.
2 Materials and Methods
2.1 Patients
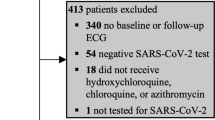
Patients were recruited for this study in two different settings. Group A comprised 12 patients who had been admitted in March and April 2020 in the wards of Fondazione IRCCS Policlinico San Matteo and had at least one CHCQ determined during admission.
Group B comprised 91 patients discharged from Fondazione IRCCS Policlinico San Matteo after COVID-19 infection and enrolled at their first scheduled follow-up visit, which allowed us to recover a residual volume of their blood (from samples already analysed for other clinical investigations) to measure CHCQ and obtain registration for an electrocardiogram (ECG).
Of the 91 patients in Group B, one had already a CHCQ determined during admission and was already enrolled in Group A; of the 12 patients in Group A, two had a double CHCQ determination (in 2 different days): the total group is therefore represented by 100 patients (65 were male, 65%, age 65 ± 13 years) with a total of 103 CHCQ determinations.
All patients had been admitted between March 2020 and April 2020 in Fondazione IRCCS Policlinico San Matteo for COVID-19 infection in internal medicine, pneumology, or infectious and tropical disease wards.
2.2 Chemicals and Reagents
A HCQ sulphate standard (≥95% pure) was provided by Cayman Chemical Company (Ann Arbor, MI, USA) and the internal standard hydroxychloroquine-D4 (HCQ-D4) sulphate (98% pure) was obtained from Toronto Research Chemicals (Toronto, ON, Canada). Water for liquid chromatography–mass spectrometry, ethyl ether and formic acid were acquired from Carlo Erba Reagents (Milan, Italy); sodium hydroxide pellets (98% pure) and methanol were from Merck Life Science (Milan, Italy) and Honeywell Research Chemicals (Milan, Italy), respectively.
2.3 Data Collection
Data from every enrolled patient were extracted from paper and electronic medical records and anonymised: data concerned baseline demographics, pharmacologic history especially about drugs administered as COVID-19 treatment having a prolonging effect on the QT interval (azithromycin, lopinavir/ritonavir, levofloxacin) and HCQ dose. Data were available also for other drugs used in acute COVID-19 care in that period (low-molecular-weight heparin, steroids, tocilizumab, remdesivir, ribavirin, ceftriaxone, piperacillin/tazobactam, doxycycline) but were a priori not used in this analysis, which is centred on QTc effects of HCQ treatment. Blood tests, including blood cell count, hepatic and kidney function, C-reactive protein and ECG registration were obtained at hospitalisation and/or at follow-up.
2.4 Blood Samples
We measured CHCQ in whole blood and not in plasma because HCQ accumulates in red blood cells, in which its concentrations are much higher and less variable than in plasma [22]; moreover, whole blood concentration better represents the amount of drug accumulated within the body’s tissues through time [19, 25]. Hydroxychloroquine concentrations were measured during hospitalisation (12 samples) and/or at the follow-up visit (91 samples).
2.5 Stock and Working Solutions
Hydroxychloroquine and HCQ-D4 stock solutions (10 mg/mL and 1 mg/mL, in CH3OH, respectively) were prepared by carefully weighing the corresponding standard powders. The working solutions were then obtained by serial dilution with methanol (1–0.01 mg/mL for HCQ and 50 ng/mL for HCQ-D4): calibrators and quality-control samples were prepared from different stock solutions, all stored at −20 °C: the working solutions were prepared fresh daily.
2.6 Sample Preparation
Hydroxychloroquine was detected in whole blood samples by a liquid–liquid extraction procedure combined with a high-performance liquid chromatography–tandem mass spectrometry assay. Three hundred microlitres of H2O, 150 μL of internal standard (HCQ-D4, 50 ng/mL), 20 μL of each working solution, 180 μL of whole blood (or 200 μL of patients’ whole blood) and 30 μL of NaOH (10 N) were progressively added to well-labelled conical glass tubes and extracted with 2 mL of ethyl ether. The mixtures were vortex mixed (10 s), shaken (10 min) and then centrifuged (10 min), at 4 °C, at 10,400g. Supernatants were removed from the top, dried under a gentle flow of nitrogen and then reconstituted in 100 μL of CH3OH:H2O=50:50 (v/v; 0.1% HCOOH). Ten microlitres were then directly injected into the chromatographic column.
2.7 Instrumentation and Chromatographic Conditions
The liquid chromatograph was an Accela high-performance liquid chromatography (Thermo Scientific, San Jose, CA, USA) system consisting of a quaternary pump, a degasser, a thermostatic column oven and an autosampler (kept at 10 °C). Xcalibur 2.07 and LCquan 2.5.6 software from Thermo Scientific were employed for the liquid chromatography-tandem mass spectrometry system control, data acquisition and data analysis. Calibration curves were generated using a weighted (1/×) linear regression curve in order to minimise the effect of deviation from the slope of the curve at lower concentrations. The analyte was separated on a Hypurity C18 150 × 4.6 mm (particle size: 5 mm) column, heated and maintained at 40 °C, at a flow rate of 700 μL/min. Elution was carried out in gradient mode, with acidified water (A, containing 0.1% HCOOH) and acidified CH3OH (B; containing 0.1% HCOOH), resulting in a total run time of 7 minutes per sample. A TSQ Quantum Access triple quadrupole mass spectrometer with an electrospray ionisation source, operating in positive ion mode, was used for the tandem mass spectrometry analysis. Quantification was performed using the following transitions: m/z 336.1 > 179.0; 247.0 and m/z 340.1 > 251.2 for HCQ and HCQ-D4, respectively. Ion spray voltage was set to 3500 V, with a capillary temperature of 300 °C. A typical chromatogram, indicating also the selected transitions and the collision energies for the analyte and ion spray, is reported in Fig. 1.
2.8 Validation Procedure
The developed method was fully validated for selectivity, lower limit of quantification (LLOQ), linearity, matrix effect, carry over, precision (within and between-run), accuracy (within and between-run) and stability, according to the guidelines for bioanalytical method validation defined by the European Medicines Agency (EMEA/CHMP/EWP/192217/2009 Rev.1). All samples (standards and quality controls) were prepared in HCQ free human whole blood.
Stability tests were performed for prepared samples only, stored in the autosampler at 10 °C for 24 hours. All collected samples from patients were analysed within a few hours.
2.9 QTc Measurement
Twelve-lead ECGs were collected from the clinical charts of the Group A patients (different electrocardiographs), while in Group B, ECGs were all registered with Cardioline ECG 200+ (Cardioline S.P.A., Trento, Italy). The QT interval was blinded, manually measured by a single expert cardiologist (AV) in D2 derivation (or in V2 or V5 if the T wave in D2 was flat or not measurable) and calculated with Bazett’s formula (as all ECGs showed a heart rate variability between 55 and 105 bpm) and the excess correction method for QRS values greater than 120 ms.
Only one patient showed atrial fibrillation in all measurements and, in this case, a medium value of the QTc interval was taken among the measured beats of the ECG. Patients having an ECG taken more than 5 days before or after the HCQ whole blood dosage were excluded from the CHCQ-QTc correlation analysis.
2.10 Statistical Analysis
Categorical variables were described as counts and percentages; quantitative variables as mean and standard deviation if normally distributed (Shapiro–Wilk test), with median and interquartile range otherwise. The normalised CHCQ for a total dose taken of 4000 mg was calculated as the whole blood concentration divided by the dose taken and multiplied by 4000 and entered as a dependent variable in a regression model with time from the last HCQ dose taken as the independent variable. Predicted values are presented with a 95% confidence interval (95% CI) of the prediction calculated from the standard error of the predicted expected value, or mean index, for the observation’s covariate pattern.
A multivariate regression model was fitted with QTc (measured in DII with Bazett’s formula) as dependent variables, while HCQ concentration, age, sex and use of other QT-lengthening drugs frequently used in patients with COVID-19 (azithromycin, levofloxacin, lopinavir/ritonavir) were independent variables. All analyses were performed with Stata version 16.1 (2019; StataCorp LLC, College Station, TX, USA).
2.11 Ethical and Consent Issues
The study has been conducted with respect to the principles of the World Medical Association’s Declaration of Helsinki (7th Edition, 2013) [26].
The Institutional Review Board of the Fondazione IRCCS Policlinico San Matteo (Comitato Etico della Provincia di Pavia) approved the study (Prot: 20200069934) for the patients enrolled at the post-COVID clinic (HCQ blood concentration determinations from 26 days after treatment end, Group B). The patients whose CHCQ has been determined during the hospital admission (Group A) gave consent to the retrospective data analysis in the current admission privacy consent form of Fondazione IRCCS Policlinico San Matteo. In the study database, single patient data were pseudo-anonymised.
3 Results
3.1 Validation Procedure
The linearity was observed within the dynamic range of 1–100 ng/mL with a coefficient of determination (R2) of 0.998 or better. The LLOQ was set at 1 ng/mL. Accuracy and precision (at low-quality, medium-quality, and high-quality control levels and at LLOQ) were within 15% and 20% (LLOQ), which met the requirement of the European Medicines Agency regulation. The matrix effect was evaluated and the findings indicated the absence of significant ion suppression or enhancement effects. Absence of carry-over was also assessed. Processed sample stability was verified after resting 24 h at 10 °C in the autosampler: five replicates of each quality control were prepared, immediately analysed and then tested again the next day. The mean concentration at each level was within ±15% of the nominal concentrations.
3.2 Patients’ Characteristics
Of the 100 enrolled patients, three were excluded because they were receiving HCQ treatment for rheumatic disease also before or after index admission (all three in Group B), and six more were excluded because at the CHCQ determination they had taken the drug for fewer than 3 days (one in Group A and five in Group B). The 91 remaining patients were mainly male (58, 64%); had an average age of 65 ± 13 years and had a total of 94 CHCQ determinations (11 in Group A and 83 in Group B) (Table 1).
3.3 C HCQ During and After Treatment
The time and dosage characteristics of the 94 observations are summarised in Table 2. The HCQ dose taken by the patient at the moment of the HCQ blood sample varied from 1400 mg to 10200 mg. We therefore decided to normalise the CHCQ for a total dose taken of 4000 mg (normalised CHCQ, ng/mL).
Figure 2 represents a scatter plot of 4000 mg normalised CHCQ with time from the last HCQ dose taken; the line represents a regression model estimating the normalised CHCQ in time, in an average patient who has taken a total HCQ dose of 4000 mg. The grey area represents the 95% CI of the predicted values of the regression model. The model has an R2 of 0.7504. The upper 95% CI of the prediction of the regression model crosses the line of the 500-ng/mL concentration at day 16 from HCQ treatment cessation.
Regression model curve of a normalised hydroxychloroquine whole blood concentration (nCHCQ) for a total dose taken of 4000 mg; the horizontal line represents the concentration of 500 ng/mL considered as a safety threshold; the upper 95% confidence interval (CI) of the model intercepts the line at 16 days from hydroxychloroquine treatment cessation. nCHCQ HCQ whole blood concentrations normalised for a total dose taken of 4000 mg
3.4 QTc and C HCQ
An ECG was available within 5 days of CHCQ measurement in 77 of the 94 observations. Corrected QT measurements (measured in DII with Bazett’s formula) were significantly different in Group A and Group B. Median QTc in our patients (77 observations) was 423.62 ± 34.59 ms, for Group A (seven observations) was 465.29 ± 41.49 ms and for Group B (70 observations) was 419.46 ± 31.22 ms. Corrected QT measurements correlate with CHCQ in a model that also includes age, sex and use of other QT-prolonging drugs frequently used for COVID-19 treatment (azithromycin, levofloxacin, lopinavir/ritonavir) with a p value of 0.010 and a R2 of 0.208. In the same model, age was significantly correlated with QTc (p = 0.013), whereas sex and concomitant treatment with QT-prolonging drugs were not (p = 0.108 and p = 0.524, respectively).
4 Discussion
To the best of our knowledge, this is the first study investigating CHCQ after a short-term treatment such as those used in SARS-CoV-2 infection during the first pandemic surge. Recent studies have indeed evaluated the short-term treatment with HCQ and have indicated the HCQ doses needed to achieve an effective level against SARS-CoV-2 [25]; however, no data on drug elimination after treatment discontinuation are available.
Our data suggest that short-term courses of HCQ can generate significant blood concentrations of the drug, persisting above 500 ng/mL for up to 16 days after discontinuation of the treatment. These data could inform the clinician using this drug in a similar context, to estimate when it would be possible to start or re-initiate other treatment with QT-prolonging potential (such as antiarrhythmic drugs, antiepileptic drugs, neuroleptic drugs and some antibiotics).
Data on HCQ pharmacokinetics/pharmacodynamics are scarce and not conclusive, especially in short-term treatments such as those used in the COVID-19 epidemic. A single-dose terminal elimination phase has been studied in healthy volunteers [18] and the drug terminal elimination half-life in the whole blood was found to be about 50 days for oral treatment and 30 days for intravenous administration [19]. Elimination of HCQ has also been studied in patients receiving long-term treatment such as for malaria prevention and rheumatoid arthritis, demonstrating a very variable half-life starting from 43 h to more than 40 days [17].
Existing data suggest that the long persistence of HCQ concentrations in blood are due to the sequestration in deep tissues that leads to an extremely large volume of distribution, such as 5522 litres in blood, [19]. In fact, studies in animals show a high concentration of the drug in the lungs, kidney, liver and spleen [27]. The use of HCQ in the treatment of SARS-CoV-2 pneumonia found its indication, in addition to the antiviral effect [6], in the persistence of a high concentration of the drug in the lung [27].
The CHCQ found in our patients appear to have a clinical relevance because we found a significant correlation between CHCQ and the QTc interval in ECGs taken a short time apart from blood sampling. Hydroxychloroquine has been found to be associated with prolongation of the QTc interval in patients receiving long-term HCQ therapy [28], whereas data on short-term treatment are not conclusive [29, 30].
Corrected QT interval prolongation by HCQ has been related to the inhibitory effects of the 4-aminoquinoline antimalarials on hERG (human Ether-à-go-go-Related Gene) potassium channels and other cardiac ion channels, described in several recent in vitro studies [31–34]. Additionally, hERG channel inhibition by HCQ is stronger at lower extracellular K+ concentrations, [33] pointing to the need to correct or prevent hypokalaemia during and immediately after clinical therapy with this drug.
The direct correlation between the QTc interval and age seen in our data has already been described in the literature [35]. The correlation between CHCQ and QTc, apart from the above-described pharmacological effect, could be related to the higher acute inflammation levels during the admission period: inflammation is known to have a QT-prolonging effect [36], and indeed, we found a direct correlation also between C-reactive protein (CRP) and CHCQ in our data (R2 = 0.5598), which is obvious, as both CHCQ and CRP are much higher during the admission than at follow-up visits. We did not add CRP to the multivariate analysis because of this strong correlation between the CHCQ and the CRP variable and, with our data, we deem it not possible to eliminate this confounder from the analysis.
It is indeed well known that the QTc-prolonging effects of HCQ are mainly related to drug–drug interactions than to HCQ per se [6, 8]. In our analysis, CHCQ directly correlated with QTc prolongation, while therapy with other drugs with QTc-prolonging effects during hospitalisation [30, 35] did not statistically correlate with QTc values. This result may be explained by the fact that most of the ECGs of Group B were taken many days after discontinuation of these other drugs, meaning presumably after their complete elimination.
4.1 Limitations of the Study
Our study has several limitations. From a theoretical point of view, it is not the same to say that a CHCQ of 500 ng/mL is the lower limit of efficacy of HCQ or that it is also the limit over which adverse events begin; drug–drug interaction adverse events could be significant at lower or higher concentrations. Nevertheless, to our knowledge, no minimal toxicity concentrations are actually available for CHCQ.
In our data, there is a wide gap (approximately 1 log) between the CHCQ during admission (Group A) and those at the control visit (Group B) and there are very few HCQ measurements at the range 5–30 days, where quite probably CHCQ drops under 500 ng/mL. This deficiency of values coupled with an R2 = 0.75 brings a wide interval of days (95% CI) in which the curve could drop under the assumed safety threshold; nonetheless, to our knowledge, this is the first attempt to approximate the moment in which it is safe to add other drugs with a QT prolongation effect to the patients’ therapy.
Another data limitation is the normalisation of blood concentrations for the drug dose taken; this presumes a linear HCQ dose/CHCQ ratio persisting over a wide period of time; nevertheless, this is the best approximation given the quite different doses taken by patients, varying from 1400 to 10,200 mg at the time of blood sampling.
Moreover, we have only seven ECGs during HCQ treatment (within 5 days of the HCQ blood sample) and 70 after discontinuation of the drug. Only two patients underwent ECGs in two different timings, while other patients had only one ECG registration; however, to the best of our knowledge, this is the widest report available in the literature that attempts to correlate CHCQ to QTc in short-term treatment courses. Further studies with larger case series and more complex population pharmacokinetic models will be needed in order to definitively correlate QTc prolongation with CHCQ and to estimate thresholds of safety.
5 Conclusions
Our data confirm the long half-life of HCQ even in short-term courses of therapy, such as those that have been used for COVID-19 treatment. Indeed, HCQ therapy can lead to significant concentrations of the drug in the blood that could persist above a safety threshold of 500 ng/mL for up to 16 days after drug discontinuation. We also found a correlation between CHCQ and QTc prolongation that suggests the clinical relevance of the findings. These data could be of interest to the clinician, to estimate when it would be safe to start or re-introduce other treatments that prolong the QTc interval after HCQ treatment discontinuation.
References
Morrisette T, Lodise TP, Scheetz MH, et al. The pharmacokinetic and pharmacodynamic properties of hydroxychloroquine and dose selection for COVID-19: putting the cart before the horse. Infect Dis Ther. 2020;9:561–72.
Yao X, Ye F, Zhang M, et al. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin Infect Dis. 2020;71:732–9. https://doi.org/10.1093/cid/ciaa237.
Infectious Diseases Society of America (IDSA). IDSA guidelines on the treatment and management of patients with COVID-19. https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/. Accessed 9 Apr 2021.
Chatre C, Roubille F, Vernhet H, et al. Cardiac complications attributed to chloroquine and hydroxychloroquine: a systematic review of the literature. Drug Saf. 2018;41:919–31.
Molina JM, Delaugerre C, Le Goff J, et al. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe COVID-19 infection. Med Mal Infect. 2020;50:384.
Mercuro NJ, Yen CF, Shim DJ, et al. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1036–41. https://doi.org/10.1001/jamacardio.2020.1834.
Bessière F, Roccia H, Delinière A, et al. Assessment of QT intervals in a case series of patients with coronavirus disease 2019 (COVID-19) infection treated with hydroxychloroquine alone or in combination with azithromycin in an intensive care unit. JAMA Cardiol. 2020;5:1067–9.
Haghjoo M, Golipra R, Kheirkhah J, et al. Effect of COVID-19 medications on corrected QT interval and induction of torsade de pointes: results of a multicenter national survey. Int J Clin Pract. 2021;75: e14182. https://doi.org/10.1111/ijcp.14182.
Sánchez-Chapula J, Salinas-Stefanon E, Torres-Jácome J, Benavides-Haro DE, Navarro-Polanco RA. Blockade of currents by the antimalarial drug chloroquine in feline ventricular myocytes. J Pharmacol Exp Ther. 2001;297:437–45.
Borsini F, Crumb W, Pace S, et al. In vitro cardiovascular effects of dihydroartemisin-piperaquine combination compared with other antimalarials. Antimicrob Agents Chemother. 2012;56:3261. https://doi.org/10.1128/AAC.05688-11.
Vicente J, Zusterzeel R, Johannesen L, et al. Assessment of multi-ion channel block in a phase I randomized study design: results of the CiPA Phase I ECG Biomarker Validation Study. Clin Pharmacol Ther. 2019;105:943–53. https://doi.org/10.1002/CPT.1303.
Becker ML, Snijders D, van Gemeren CW, et al. QTc prolongation in COVID-19 patients using chloroquine. Cardiovasc Toxicol. 2021;21:314–21. https://doi.org/10.1007/S12012-020-09621-2.
Chorin E, Dai M, Shulman E, et al. The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. nature.com
Roden DM, Harrington RA, Poppas A, Russo AM. Considerations for drug interactions on QTc interval in exploratory COVID-19 treatment. J Am Coll Cardiol. 2020;75:2623. https://doi.org/10.1016/J.JACC.2020.04.016.
Gérard A, Romani S, Fresse A, et al. “Off-label” use of hydroxychloroquine, azithromycin, lopinavir-ritonavir and chloroquine in COVID-19: a survey of cardiac adverse drug reactions by the French Network of Pharmacovigilance Centers. Therapie. 2020;75:371–9. https://doi.org/10.1016/J.THERAP.2020.05.002.
Petri M, Elkhalifa M, Li J, et al. Hydroxychloroquine blood levels predict hydroxychloroquine retinopathy. Arthritis Rheumatol. 2020;72:448–53. https://doi.org/10.1002/art.41121.
Carmichael SJ, Charles B, Tett SE. Population pharmacokinetics of hydroxychloroquine in patients with rheumatoid arthritis. Ther Drug Monit. 2003;25:671–81. https://doi.org/10.1097/00007691-200312000-00005.
Tett S, Cutler D, Day R, Brown K. Bioavailability of hydroxychloroquine tablets in healthy volunteers. Br J Clin Pharmacol. 1989;27:771–9. https://doi.org/10.1111/j.1365-2125.1989.tb03439.x.
Tett S, Cutler D, Day R, Brown K. A dose-ranging study of the pharmacokinetics of hydroxy-chloroquine following intravenous administration to healthy volunteers. Br J Clin Pharmacol. 1988;26:303–13. https://doi.org/10.1111/j.1365-2125.1988.tb05281.x.
Brocks DR, Skeith KJ, Johnston C, et al. Hematologic disposition of hydroxychloroquine enantiomers. J Clin Pharmacol. 1994;34:1088–97. https://doi.org/10.1002/j.1552-4604.1994.tb01986.x.
Costedoat-Chalumeau N, Amoura Z, Hulot JS, et al. Very low blood hydroxychloroquine concentration as an objective marker of poor adherence to treatment of systemic lupus erythematosus. Ann Rheum Dis. 2007;66:821–4. https://doi.org/10.1136/ard.2006.067835.
Mok CC, Penn HJ, Chan KL, et al. Hydroxychloroquine serum concentrations and flares of systemic lupus erythematosus: a longitudinal cohort analysis. Arthritis Care Res. 2016;68:1295–302. https://doi.org/10.1002/acr.22837.
Costedoat-Chalumeau N, Amoura Z, Hulot JS, et al. Low blood concentration of hydroxychloroquine is a marker for and predictor of disease exacerbations in patients with systemic lupus erythematosus. Arthritis Rheum. 2006;54:3284–90. https://doi.org/10.1002/art.22156.
Durcan L, Clarke WA, Magder LS, Petri M. Hydroxychloroquine blood levels in systemic lupus erythematosus: clarifying dosing controversies and improving adherence. J Rheumatol. 2015;42:2092–7. https://doi.org/10.3899/jrheum.150379.
Zahr N, Urien S, Llopis B, et al. Pharmacokinetics and pharmacodynamics of hydroxychloroquine in hospitalized patients with COVID-19. Therapie. 2021;76:295–395. https://doi.org/10.1016/j.therap.2021.01.056.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
McChesney EW. Animal toxicity and pharmacokinetics of hydroxychloroquine sulfate. Am J Med. 1983;75:11–8. https://doi.org/10.1016/0002-9343(83)91265-2.
Hooks M, Bart B, Vardeny O, et al. Effects of hydroxychloroquine treatment on QT interval. Hear Rhythm. 2020;17:1930–5. https://doi.org/10.1016/j.hrthm.2020.06.029.
Vicentini A, Masiello L, D’Amore S, et al. QTc interval and mortality in a population of SARS-2-CoV infected patients. Circ Arrhythm Electrophysiol. 2020;13:e008890.
Saleh M, Gabriels J, Chang D, et al. Effect of chloroquine, hydroxychloroquine, and azithromycin on the corrected QT interval in patients with SARS-CoV-2 infection. Circ Arrhythmia Electrophysiol. 2020;13:496–504. https://doi.org/10.1161/CIRCEP.120.008662.
Delaunois A, Abernathy M, Anderson WD, et al. Applying the CiPA approach to evaluate cardiac proarrhythmia risk of some antimalarials used off-label in the first wave of COVID-19. Clin Transl Sci. 2021;14:1133–46. https://doi.org/10.1111/CTS.13011.
Thomet U, Amuzescu B, Knott T, et al. Assessment of proarrhythmogenic risk for chloroquine and hydroxychloroquine using the CiPA concept. Eur J Pharmacol. 2021;913: 714632. https://doi.org/10.1016/J.EJPHAR.2021.174632.
TeBay C, McArthur JR, Mangala M, et al. Pathophysiological metabolic changes associated with disease modify the proarrhythmic risk profile of drugs with potential to prolong repolarisation. Br J Pharmacol. 2021. https://doi.org/10.1111/BPH.15757.
Jordaan P, Dumotier B, Traebert M, et al. Cardiotoxic potential of hydroxychloroquine, chloroquine and azithromycin in adult human primary cardiomyocytes. Toxicol Sci. 2021;180:356–68. https://doi.org/10.1093/TOXSCI/KFAA194.
Tomaselli Muensterman E, Tisdale JE. Predictive analytics for identification of patients at risk for QT interval prolongation: a systematic review. Pharmacotherapy. 2018;38:813–21.
Lazzerini PE, Laghi-Pasini F, Bertolozzi I, et al. Systemic inflammation as a novel QT-prolonging risk factor in patients with torsades de pointes. Heart. 2017;103:1821–9. https://doi.org/10.1136/heartjnl-2016-311079.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This article was funded by research grants of Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Conflicts of interest/competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval
The study has been conducted in respect of the principles of the World Medical Association’s Declaration of Helsinki (7th Edition, 2013). The Institutional Review Board of the Fondazione IRCCS Policlinico San Matteo (Comitato Etico della Provincia di Pavia) approved the study (Prot: 20200069934) for the patients enrolled at the post-COVID clinic (hydroxychloroquine blood concentration determinations from 26 days after treatment end, Group B).
Consent to Participate
The patients whose hydroxychloroquine blood concentrations were determined during the hospital admission (Group A) gave consent to a retrospective data analysis in the current admission privacy consent form of Fondazione IRCCS Policlinico San Matteo. In the study database, single patient data were pseudo-anonymised.
Consent for publication
The authors own the data and all consent fully for publication.
Availability of data and material
Raw data are available on request.
Code availability
Not applicable.
Author contributions
SDG, FF and MM conceived the study. SDG and FF wrote and revised the paper. AB, AF, EC, RC, US, CS and AN contributed to the data collection and analysis. AV read all the electrocardiograms and determined corrected QT intervals. ADS conducted the statistical analysis. ADS coordinated the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
De Gregori, S., Falaschi, F., Ballesio, A. et al. Hydroxychloroquine Blood Concentrations Can Be Clinically Relevant Also After Drug Discontinuation. Drugs R D 22, 155–163 (2022). https://doi.org/10.1007/s40268-022-00387-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-022-00387-2